Impacts of COVID-19 Pandemic on the Mental Health of Working Adults in the Czech Republic: Analysis of Self-Report Psychological Data in a One Year Perspective
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
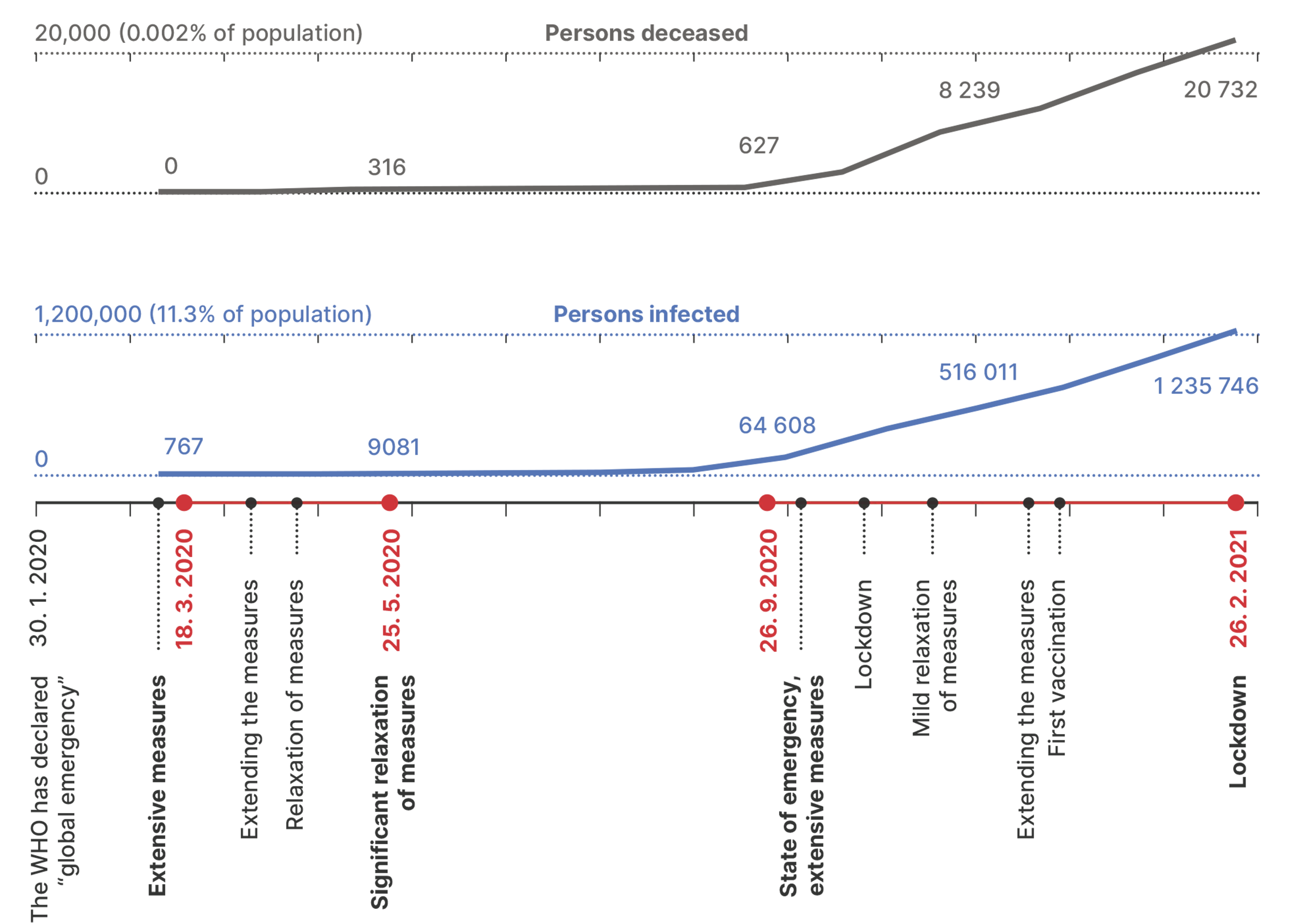
2.3. Procedure
2.4. Data Analysis
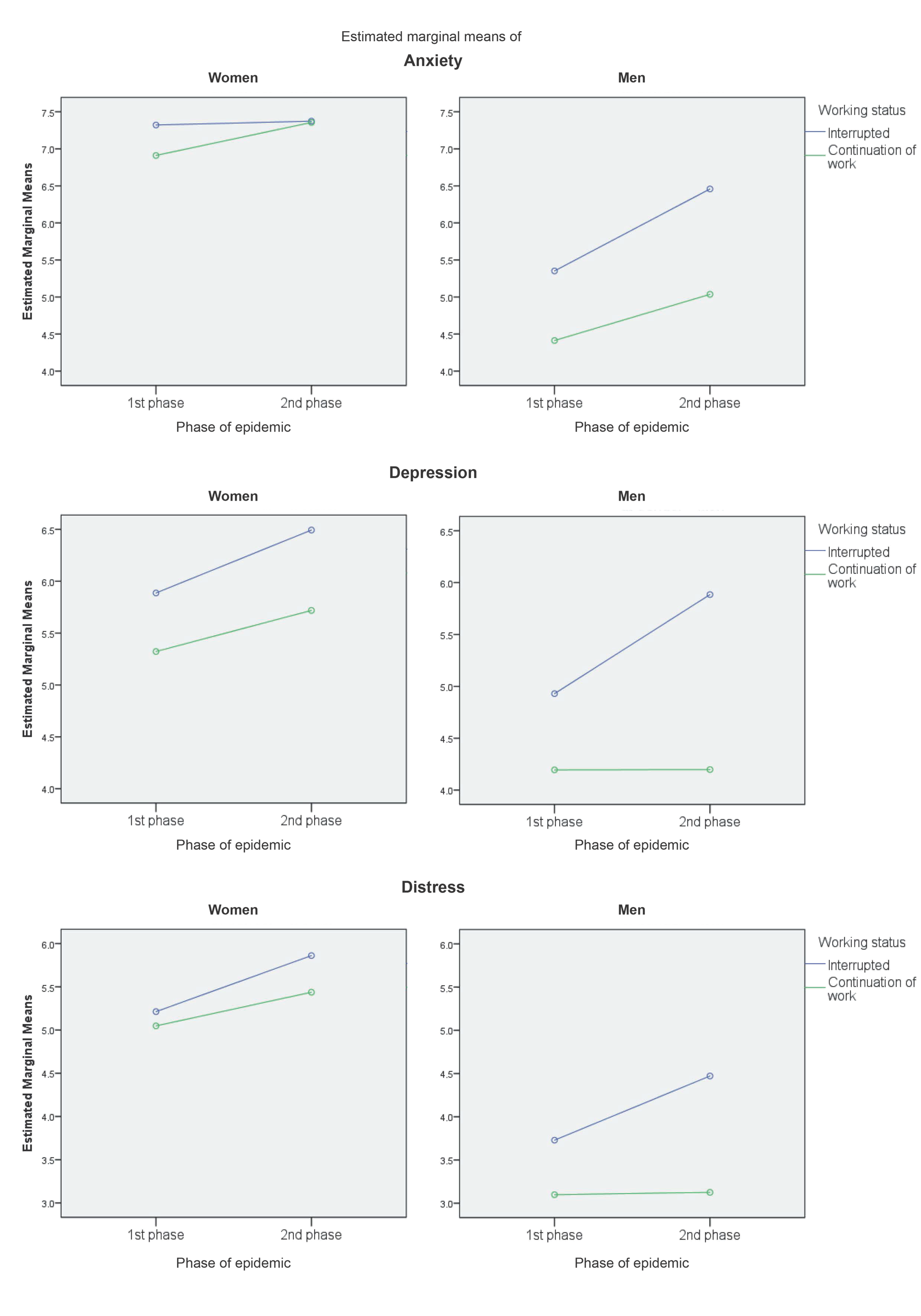
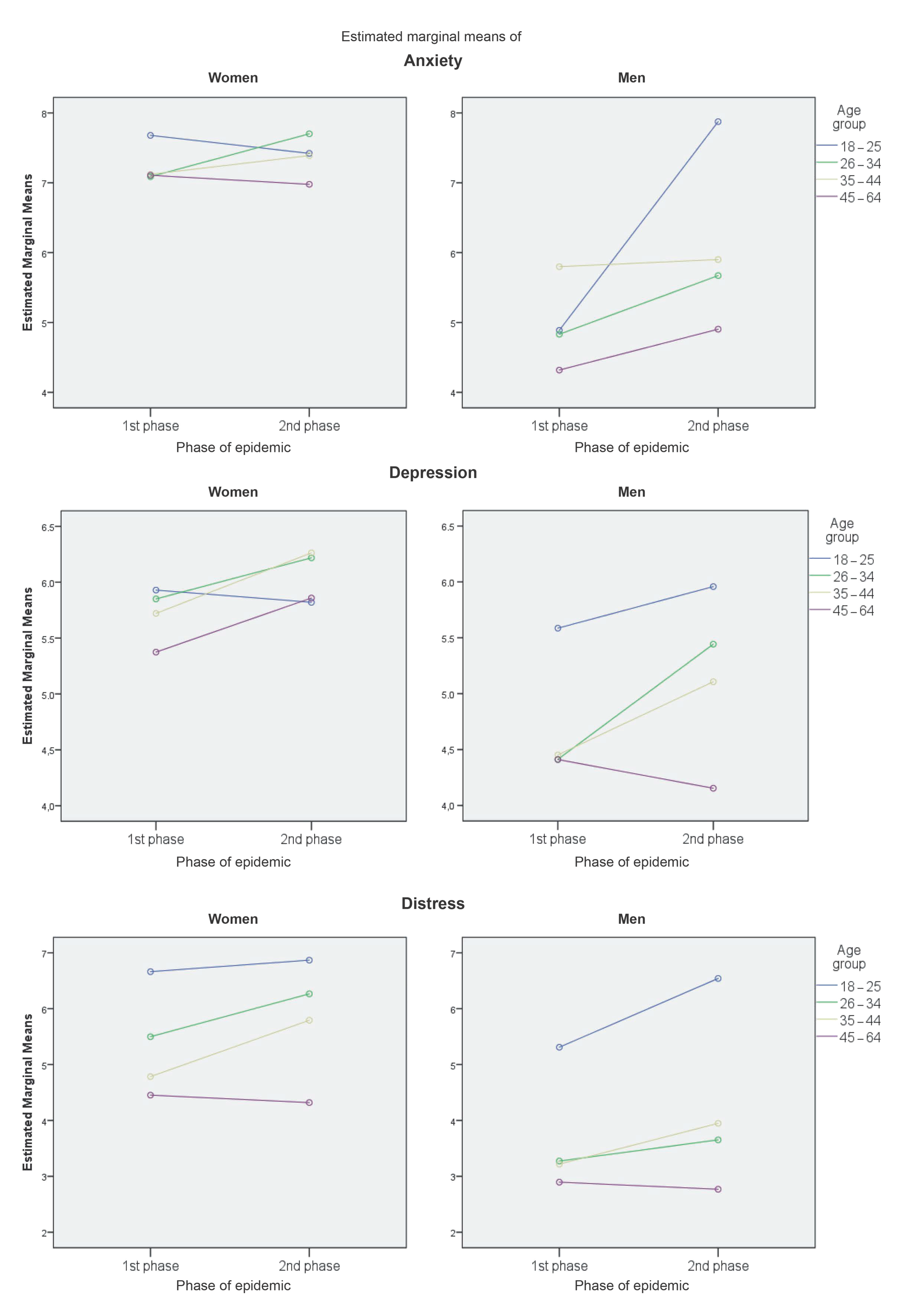
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethical Statement
References
- Van der Westhuizen, C.; Wyatt, G.; Williams, J.K.; Stein, D.J.; Sorsdahl, K. Validation of the Self Reporting Questionnaire 20-Item (SRQ-20) for Use in a Low- and Middle-Income Country Emergency Centre Setting. Int. J. Ment. Health Addict. 2016, 14, 37–48. [Google Scholar] [CrossRef] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Prati, G.; Mancini, A.D. The Psychological Impact of COVID-19 Pandemic Lockdowns: A Review and Meta-Analysis of Longitudinal Studies and Natural Experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Röthke, N.; Günthner, L.; Stoffers-Winterling, J.; Tüscher, O.; Coenen, M.; Rehfuess, E.; Schwarzer, G.; Binder, H.; Schmucker, C.; et al. Mental Burden and Its Risk and Protective Factors during the Early Phase of the SARS-CoV-2 Pandemic: Systematic Review and Meta-Analyses. Glob. Health 2021, 17, 34. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain. Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Holman, E.A.; Thompson, R.R.; Garfin, D.R.; Silver, R.C. The Unfolding COVID-19 Pandemic: A Probability-Based, Nationally Representative Study of Mental Health in the United States. Sci. Adv. 2020, 6, eabd5390. [Google Scholar] [CrossRef]
- Fisher, J.R.; Tran, T.D.; Hammarberg, K.; Sastry, J.; Nguyen, H.; Rowe, H.; Kirkman, M. Mental Health of People in Australia in the First Month of COVID-19 Restrictions: A National Survey. Med. J. Aust. 2020, 213, 458–464. [Google Scholar] [PubMed]
- Al Dhaheri, A.S.; Bataineh, M.F.; Mohamad, M.N.; Ajab, A.; Al Marzouqi, A.; Jarrar, A.H.; Habib-Mourad, C.; Abu Jamous, D.O.; Ali, H.I.; Al Sabbah, H.; et al. Impact of COVID-19 on Mental Health and Quality of Life: Is There Any Effect? A Cross-Sectional Study of the MENA Region. PLoS ONE 2021, 16, e0249107. [Google Scholar] [CrossRef]
- McCracken, L.M.; Badinlou, F.; Buhrman, M.; Brocki, K.C. Psychological Impact of COVID-19 in the Swedish Population: Depression, Anxiety, and Insomnia and Their Associations to Risk and Vulnerability Factors. Eur. Psychiatry 2020, 63. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Talevi, D.; Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; di Bernardo, A.; Capelli, F.; Pacitti, F. Mental Health Outcomes of the CoViD-19 Pandemic. Riv. Psichiatr. 2020, 55, 137–144. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of Stress, Anxiety, Depression among the General Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Gilan, D.; Röthke, N.; Blessin, M.; Kunzler, A.; Stoffers-Winterling, J.; Müssig, M.; Yuen, K.S.L.; Tüscher, O.; Thrul, J.; Kreuter, F.; et al. Psychomorbidity, Resilience, and Exacerbating and Protective Factors During the SARS-CoV-2 Pandemic: A Systematic Literature Review and Results from the German COSMO-PANEL. Dtsch. Aerzteblatt Online 2020, 117, 625–632. [Google Scholar] [CrossRef]
- Szabó, C.; Pukánszky, J.; Kemény, L. Psychological Effects of the COVID-19 Pandemic on Hungarian Adults. Int. J. Environ. Res. Public. Health 2020, 17, 9565. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The Psychological Impact of COVID-19 on the Mental Health in the General Population. QJM Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Trnka, R.; Lorencova, R. Fear, Anger, and Media-Induced Trauma during the Outbreak of COVID-19 in the Czech Republic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 546–549. [Google Scholar] [CrossRef]
- Kniffin, K.M.; Narayanan, J.; Anseel, F.; Antonakis, J.; Ashford, S.P.; Bakker, A.B.; Bamberger, P.; Bapuji, H.; Bhave, D.P.; Choi, V.K.; et al. COVID-19 and the Workplace: Implications, Issues, and Insights for Future Research and Action. Am. Psychol. 2021, 76, 63–77. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The Effect of Age, Gender, Income, Work, and Physical Activity on Mental Health during Coronavirus Disease (COVID-19) Lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Alamri, H.S.; Algarni, A.; Shehata, S.F.; Al Bshabshe, A.; Alshehri, N.N.; ALAsiri, A.M.; Hussain, A.H.; Alalmay, A.Y.; Alshehri, E.A.; Alqarni, Y.; et al. Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic. Int. J. Environ. Res. Public. Health 2020, 17, 9183. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Larson, L.R.; Sharaievska, I.; Rigolon, A.; McAnirlin, O.; Mullenbach, L.; Cloutier, S.; Vu, T.M.; Thomsen, J.; Reigner, N.; et al. Psychological Impacts from COVID-19 among University Students: Risk Factors across Seven States in the United States. PLoS ONE 2021, 16, e0245327. [Google Scholar] [CrossRef]
- Jacques-Aviñó, C.; López-Jiménez, T.; Medina-Perucha, L.; de Bont, J.; Gonçalves, A.Q.; Duarte-Salles, T.; Berenguera, A. Gender-Based Approach on the Social Impact and Mental Health in Spain during COVID-19 Lockdown: A Cross-Sectional Study. BMJ Open 2020, 10, e044617. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain. Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Banna, M.H.A.; Sayeed, A.; Kundu, S.; Christopher, E.; Hasan, M.T.; Begum, M.R.; Kormoker, T.; Dola, S.T.I.; Hassan, M.M.; Chowdhury, S.; et al. The Impact of the COVID-19 Pandemic on the Mental Health of the Adult Population in Bangladesh: A Nationwide Cross-Sectional Study. Int. J. Environ. Health Res. 2020, 1–12. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental Health and Well-Being during the COVID-19 Pandemic: Longitudinal Analyses of Adults in the UK COVID-19 Mental Health & Wellbeing Study. Br. J. Psychiatry 2020, 218, 326–333. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under Lockdown: Comparisons of Students’ Social Networks and Mental Health before and during the COVID-19 Crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- Birditt, K.S.; Turkelson, A.; Fingerman, K.L.; Polenick, C.A.; Oya, A. Age Differences in Stress, Life Changes, and Social Ties During the COVID-19 Pandemic: Implications for Psychological Well-Being. Gerontologist 2021, 61, 205–216. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental Health before and during the COVID-19 Pandemic: A Longitudinal Probability Sample Survey of the UK Population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Tsoukalis-Chaikalis, N.; Demsia, S.F.; Chaniotis, D.; Chaniotis, F. Systematic Mapping Study of The Covid-19 Psychological Impact. Health Sci. J. 2021, 15, 1–7. [Google Scholar]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydın, G.; Chong, Y.Y.; et al. Impact of COVID-19 Pandemic on Mental Health: An International Study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef]
- Savolainen, I.; Oksa, R.; Savela, N.; Celuch, M.; Oksanen, A. COVID-19 Anxiety—A Longitudinal Survey Study of Psychological and Situational Risks among Finnish Workers. Int. J. Environ. Res. Public. Health 2021, 18, 794. [Google Scholar] [CrossRef]
- Zavlis, O.; Butter, S.; Bennett, K.; Hartman, T.K.; Hyland, P.; Mason, L.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Levita, L.; et al. How Does the COVID-19 Pandemic Impact on Population Mental Health? A Network Analysis of COVID Influences on Depression, Anxiety and Traumatic Stress in the UK Population; Cambridge University Press: Cambridge, UK, 2021; pp. 1–9. [Google Scholar]
- Shah, S.M.A.; Mohammad, D.; Qureshi, M.F.H.; Abbas, M.Z.; Aleem, S. Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment. Health J. 2021, 57, 101–110. [Google Scholar] [CrossRef]
- Veldhuis, C.B.; Nesoff, E.D.; McKowen, A.L.W.; Rice, D.R.; Ghoneima, H.; Wootton, A.R.; Papautsky, E.L.; Arigo, D.; Goldberg, S.; Anderson, J.C. Addressing the Critical Need for Long-Term Mental Health Data during the COVID-19 Pandemic: Changes in Mental Health from April to September 2020. Prev. Med. 2021, 146, 106465. [Google Scholar] [CrossRef]
- Ritchie, H.; Ortiz-Ospina, E.; Beltekian, D.; Mathieu, E.; Hasell, J.; Macdonald, B.; Giattino, C.; Appel, C.; Rodés-Guirao, L.; Roser, M. Coronavirus Pandemic (COVID-19). Our World Data. 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 1 June 2021).
- COVID-19 v ČR. COVID-19 in the Czech Republic. Available online: https://onemocneni-aktualne.mzcr.cz/covid-19/widget (accessed on 29 August 2021).
- Dickinson, E.R.; Adelson, J.L.; Owen, J. Gender Balance, Representativeness, and Statistical Power in Sexuality Research Using Undergraduate Student Samples. Arch. Sex. Behav. 2012, 41, 325–327. [Google Scholar] [CrossRef]
- McCray, J.A.; King, A.R.; Bailly, M.D. General Versus Gender-Specific Attributes of the Psychology Major. J. Gen. Psychol. 2005, 132, 139–150. [Google Scholar] [CrossRef]
- Cosco, T.D.; Doyle, F.; Ward, M.; McGee, H. Latent Structure of the Hospital Anxiety And Depression Scale: A 10-Year Systematic Review. J. Psychosom. Res. 2012, 72, 180–184. [Google Scholar] [CrossRef]
- Bužgová, R.; Hajnová, E.; Feltl, D.; Stolička, M. Faktory ovlivňující úzkost a depresi u pacientů v konečném stadiu nemoci při hospitalizaci. Ceská Slov. Psychiatr. 2014, 110, 7. [Google Scholar]
- Harding, T.W.; Climent, C.E.; Diop, M.; Giel, R.; Ibrahim, H.H.; Murthy, R.S.; Suleiman, M.A.; Wig, N.N. The WHO Collaborative Study on Strategies for Extending Mental Health Care, II: The Development of New Research Methods. Am. J. Psychiatry 1983, 140, 1474–1480. [Google Scholar] [CrossRef]
- A User’s Guide to the Self Reporting Questionnaire (SRQ); Beusenberg, M.; Orley, J.H. (Eds.) Division of Mental Health, World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Ventevogel, P.; De Vries, G.; Scholte, W.F.; Shinwari, N.R.; Faiz, H.; Nassery, R.; van den Brink, W.; Olff, M. Properties of the Hopkins Symptom Checklist-25 (HSCL-25) and the Self-Reporting Questionnaire (SRQ-20) as Screening Instruments Used in Primary Care in Afghanistan. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 328–335. [Google Scholar] [CrossRef]
- Scholte, W.F.; Verduin, F.; van Lammeren, A.; Rutayisire, T.; Kamperman, A.M. Psychometric Properties and Longitudinal Validation of the Self-Reporting Questionnaire (SRQ-20) in a Rwandan Community Setting: A Validation Study. BMC Med. Res. Methodol. 2011, 11, 116. [Google Scholar] [CrossRef] [Green Version]
- Langvik, E.; Hjemdal, O.; Nordahl, H.M. Personality Traits, Gender Differences and Symptoms of Anhedonia: What Does the Hospital Anxiety and Depression Scale (HADS) Measure in Nonclinical Settings? Scand. J. Psychol. 2016, 57, 144–151. [Google Scholar] [CrossRef] [Green Version]
- Yamada, Y.; Ćepulić, D.-B.; Coll-Martín, T.; Debove, S.; Gautreau, G.; Han, H.; Rasmussen, J.; Tran, T.P.; Travaglino, G.A.; Lieberoth, A. COVIDiSTRESS Global Survey Dataset on Psychological and Behavioural Consequences of the COVID-19 Outbreak. Sci. Data 2021, 8, 3. [Google Scholar] [CrossRef]
- Lieberoth, A.; Lin, S.-Y.; Stöckli, S.; Han, H.; Kowal, M.; Gelpi, R.; Chrona, S.; Tran, T.P.; Jeftić, A.; Rasmussen, J.; et al. Stress and Worry in the 2020 Coronavirus Pandemic: Relationships to Trust and Compliance with Preventive Measures across 48 Countries in the COVIDiSTRESS Global Survey. R. Soc. Open Sci. 2021, 8, 200589. [Google Scholar] [CrossRef]
| CWS | Age | Phase (PE) | Anxiety | Depression | Distress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | PE-1 | PE-2 | PE-1 | PE-2 | PE-1 | PE-2 | ||||||||
| N | N | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | ||
| Women | 709 | 529 | 7.11 | 4.45 | 7.37 | 4.56 | 5.59 | 3.80 | 5.95 | 4.14 | 5.09 | 4.12 | 5.59 | 4.37 | |
| CWS-I | 18–25 | 44 | 22 | 8.77 | 4.88 | 6.91 | 3.95 | 6.86 | 3.22 | 5.23 | 4.42 | 7.55 | 4.25 | 6.64 | 4.76 |
| 26–34 | 101 | 48 | 6.33 | 4.07 | 8.04 | 5.52 | 5.33 | 3.19 | 7.27 | 4.42 | 5.16 | 3.96 | 6.83 | 4.60 | |
| 35–44 | 104 | 45 | 7.70 | 4.78 | 7.24 | 4.55 | 6.33 | 4.28 | 6.69 | 4.57 | 4.94 | 4.14 | 5.87 | 4.63 | |
| 45–64 | 98 | 45 | 7.30 | 4.36 | 7.04 | 4.22 | 5.55 | 3.85 | 6.09 | 4.36 | 4.45 | 4.17 | 4.58 | 3.89 | |
| Total | 347 | 160 | 7.32 | 4.53 | 7.38 | 4.68 | 5.88 | 3.76 | 6.49 | 4.46 | 5.20 | 4.20 | 5.90 | 4.49 | |
| CWS-C | 18–25 | 65 | 66 | 6.32 | 4.47 | 7.92 | 4.69 | 4.89 | 3.31 | 6.52 | 4.07 | 5.66 | 4.50 | 7.20 | 4.65 |
| 26–34 | 72 | 90 | 7.64 | 4.66 | 7.48 | 4.52 | 6.13 | 4.05 | 5.21 | 3.67 | 5.76 | 4.32 | 5.90 | 4.27 | |
| 35–44 | 81 | 100 | 6.65 | 4.32 | 7.40 | 4.60 | 5.22 | 3.98 | 5.76 | 4.49 | 4.60 | 3.85 | 5.49 | 4.19 | |
| 45–64 | 144 | 113 | 6.94 | 4.21 | 6.91 | 4.32 | 5.14 | 3.80 | 5.63 | 3.66 | 4.51 | 3.72 | 4.06 | 3.83 | |
| Total | 362 | 369 | 6.91 | 4.38 | 7.36 | 4.51 | 5.31 | 3.82 | 5.72 | 3.98 | 4.99 | 4.04 | 5.46 | 4.31 | |
| Men | 221 | 144 | 4.80 | 3.87 | 5.47 | 3.94 | 4.49 | 3.64 | 4.70 | 3.69 | 3.40 | 3.53 | 3.54 | 3.67 | |
| CWS-I | 18–25 | 10 | 6 | 5.20 | 2.62 | 9.17 | 6.65 | 6.90 | 3.07 | 6.00 | 2.37 | 6.50 | 3.10 | 7.50 | 5.24 |
| 26–34 | 31 | 14 | 5.26 | 4.46 | 6.07 | 3.83 | 4.52 | 3.29 | 6.64 | 4.55 | 3.55 | 4.06 | 4.14 | 2.80 | |
| 35–44 | 21 | 8 | 6.14 | 4.80 | 6.00 | 3.66 | 4.90 | 3.53 | 6.25 | 3.88 | 3.62 | 3.93 | 5.25 | 3.65 | |
| 45–64 | 22 | 13 | 4.95 | 4.31 | 6.08 | 3.50 | 4.77 | 3.78 | 4.92 | 2.78 | 3.18 | 3.91 | 3.15 | 3.16 | |
| Total | 84 | 41 | 5.39 | 4.29 | 6.51 | 4.19 | 4.96 | 3.48 | 5.93 | 3.59 | 3.82 | 3.95 | 4.54 | 3.66 | |
| CWS-C | 18–25 | 33 | 12 | 4.58 | 3.73 | 6.58 | 4.42 | 4.27 | 4.15 | 5.92 | 4.08 | 4.12 | 4.23 | 5.58 | 4.85 |
| 26–34 | 42 | 37 | 4.40 | 3.52 | 5.27 | 4.07 | 4.31 | 4.09 | 4.24 | 3.74 | 3.00 | 2.85 | 3.16 | 3.46 | |
| 35–44 | 22 | 28 | 5.45 | 3.26 | 5.36 | 3.62 | 4.00 | 2.83 | 4.21 | 3.07 | 2.82 | 2.67 | 2.79 | 3.01 | |
| 45–64 | 40 | 26 | 3.78 | 3.58 | 3.73 | 2.88 | 4.15 | 3.48 | 3.38 | 3.76 | 2.65 | 2.86 | 2.38 | 3.52 | |
| Total | 137 | 103 | 4.43 | 3.55 | 5.06 | 3.77 | 4.20 | 3.72 | 4.21 | 3.63 | 3.14 | 3.23 | 3.15 | 3.62 | |
| Factor | MHI 1 | Groups | Est. MM | 95% CI | F (df 1) | SMD | Sig. | Gender Effect 1 | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Gender 2 | Distress ** | W | 5.40 | 5.16 | 5.64 | 51.75 | 0.43 | 0.00 | – |
| M | 3.60 | 3.15 | 4.06 | ||||||
| Anxiety ** | W | 7.25 | 6.99 | 7.51 | 42.64 | 0.43 | 0.00 | – | |
| M | 5.33 | 4.84 | 5.83 | ||||||
| Depression ** | W | 5.86 | 5.63 | 6.08 | 14.60 | 0.27 | 0.00 | – | |
| M | 4.82 | 4.38 | 5.25 | ||||||
| CWS 2 | Distress * | I | 4.83 | 4.41 | 5.25 | 7.88 | 0.16 | 0.01 | * SMD(M) = 0.25 |
| C | 4.17 | 3.87 | 4.46 | ||||||
| Anxiety * | I | 6.64 | 6.19 | 7.10 | 6.42 | 0.16 | 0.01 | ** SMD(M) = 0.27 | |
| C | 5.94 | 5.62 | 6.26 | ||||||
| Depression ** | I | 5.81 | 5.41 | 6.22 | 18.35 | 0.24 | 0.00 | ** SMD(W) = 0.17 | |
| C | 4.86 | 4.58 | 5.14 | ** SMD(M) = 0.32 | |||||
| PE 2 | Distress | PE-1 | 4.27 | 3.96 | 4.58 | 3.32 | −0.11 | 0.07 | * SMD(W) = 0.12 |
| PE-2 | 4.73 | 4.32 | 5.14 | ||||||
| Anxienty * | PE-1 | 6.01 | 5.67 | 6.35 | 5.99 | −0.13 | 0.02 | ||
| PE-2 | 6.57 | 6.13 | 7.01 | ||||||
| Depression | PE-1 | 5.09 | 4.79 | 5.39 | 3.88 | −0.13 | 0.07 | ** SMD(W) = 0.13 | |
| PE-2 | 5.58 | 5.19 | 5.98 | ||||||
| Age Group Factor 3 | |||||||||
| Gender | MHI 1 | Age | Est. MM | 95% CI | F (df 3) | Sig. | Pairwise tests 1 | ||
| Lower | Upper | ||||||||
| Women | Distress ** | 18–25 | 6.76 | 6.14 | 7.38 | 13.86 | 0.00 | 18–25 > 26–34 **, 35–44 **, 45–64 **; 26–35 > 45–64 ** | |
| 26–34 | 5.91 | 5.45 | 6.38 | ||||||
| 35–44 | 5.23 | 4.77 | 5.68 | ||||||
| 45–64 | 4.40 | 3.97 | 4.83 | ||||||
| Anxiety | 18–25 | 7.48 | 6.81 | 8.15 | 0.44 | 0.73 | |||
| 26–34 | 7.37 | 6.87 | 7.88 | ||||||
| 35–44 | 7.25 | 6.75 | 7.75 | ||||||
| 45–64 | 7.05 | 6.58 | 7.52 | ||||||
| Depression | 18–25 | 5.87 | 5.28 | 6.47 | 0.70 | 0.55 | |||
| 26–34 | 5.98 | 5.54 | 6.43 | ||||||
| 35–44 | 6.00 | 5.56 | 6.44 | ||||||
| 45–64 | 5.60 | 5.19 | 6.02 | ||||||
| Men | Distress ** | 18–25 | 5.93 | 4.71 | 7.14 | 7.75 | 0.00 | 18–25 > 26–34 **, 35–44 **, 45–64 ** | |
| 26–34 | 3.46 | 2.69 | 4.24 | ||||||
| 35–44 | 3.62 | 2.63 | 4.61 | ||||||
| 45–64 | 2.84 | 1.99 | 3.69 | ||||||
| Anxiety * | 18–25 | 6.38 | 5.06 | 7.70 | 2.22 | 0.09 | |||
| 26–34 | 5.25 | 4.41 | 6.09 | ||||||
| 35–44 | 5.74 | 4.66 | 6.82 | ||||||
| 45–64 | 4.63 | 3.71 | 5.56 | ||||||
| Depression | 18–25 | 5.77 | 4.60 | 6.94 | 1.55 | 0.20 | |||
| 26–34 | 4.93 | 4.18 | 5.67 | ||||||
| 35–44 | 4.84 | 3.89 | 5.80 | ||||||
| 45–64 | 4.31 | 3.49 | 5.12 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kučera, D.; Stuchlíková, I.; Mrhálek, T. Impacts of COVID-19 Pandemic on the Mental Health of Working Adults in the Czech Republic: Analysis of Self-Report Psychological Data in a One Year Perspective. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1061-1072. https://doi.org/10.3390/ejihpe11030079
Kučera D, Stuchlíková I, Mrhálek T. Impacts of COVID-19 Pandemic on the Mental Health of Working Adults in the Czech Republic: Analysis of Self-Report Psychological Data in a One Year Perspective. European Journal of Investigation in Health, Psychology and Education. 2021; 11(3):1061-1072. https://doi.org/10.3390/ejihpe11030079
Chicago/Turabian StyleKučera, Dalibor, Iva Stuchlíková, and Tomáš Mrhálek. 2021. "Impacts of COVID-19 Pandemic on the Mental Health of Working Adults in the Czech Republic: Analysis of Self-Report Psychological Data in a One Year Perspective" European Journal of Investigation in Health, Psychology and Education 11, no. 3: 1061-1072. https://doi.org/10.3390/ejihpe11030079
APA StyleKučera, D., Stuchlíková, I., & Mrhálek, T. (2021). Impacts of COVID-19 Pandemic on the Mental Health of Working Adults in the Czech Republic: Analysis of Self-Report Psychological Data in a One Year Perspective. European Journal of Investigation in Health, Psychology and Education, 11(3), 1061-1072. https://doi.org/10.3390/ejihpe11030079







