Abstract
Current strategies of combating bacterial infections are limited and involve the use of antibiotics and preservatives. Each of these agents has generally inadequate efficacy and a number of serious adverse effects. Thus, there is an urgent need for new antimicrobial drugs and food preservatives with higher efficacy and lower toxicity. Edible plants have been used in medicine since ancient times and are well known for their successful antimicrobial activity. Often photosensitizers are present in many edible plants; they could be a promising source for a new generation of drugs and food preservatives. The use of photodynamic therapy allows enhancement of antimicrobial properties in plant photosensitizers. The purpose of this review is to present the verified data on the antimicrobial activities of photodynamic phytochemicals in edible species of the world’s flora, including the various mechanisms of their actions.
1. Introduction
Although plants are able to treat many pathological conditions [1], only 15% have been investigated phytochemically, and 6% have been screened for biological activity [2]. It is widely acknowledged that many antimicrobial compounds identified and isolated from medicinal plants are very active against both Gram-positive and Gram-negative bacteria [3,4,5,6,7]. Between 1981 and 2019, 162 new antimicrobial drugs were approved, 94 of which were produced from plants [8].
The best-known approach to combating bacterial diseases involves the use of antibiotics. During the last decades, the overuse of antibiotics resulted in selective pressures that led to the widespread appearance of antibiotic-resistant microorganisms [9]. Each of the antibiotics in use has generally inadequate efficacy and a number of serious adverse effects [10]. It is imperative to investigate new antimicrobial agents that are more effective and less toxic than these antibiotics. From this perspective, the application of herbal compounds may potentially hold great promise. Isolation and identification of plant-based antimicrobial agents is always a challenging task, because bioactive compounds often occur as complex mixtures with other secondary metabolites. In addition, these compounds are found in such small quantities that enhancement of their antimicrobial properties is very important. The use of photodynamic therapy presents a promising possibility to improve the antimicrobial activity of phytochemicals, since many of them are photosensitizers (PSs). Although many aspects of PSs were covered by numerous reviews [11,12,13,14,15,16], edible plants and their PSs were not seriously considered as sources of new drugs and preservatives. They in fact deserve special attention, because actively cultivated edible plants are already available which are rich in useful phytochemicals. These phytochemicals are not only potential antimicrobial drugs, but are also ideal as possible preservatives for the food industry. There is an urgent need for new natural agents that are more effective and less toxic than the currently popular compounds, such as sodium benzoate; acetic, lactic, benzoic, and sorbic acids; hydrogen peroxide, and chelators. They are used in many cases because of their ability to inhibit the activity of various microorganisms [17]. In addition, the majority of these compounds have good stability and excellent solubility in water [18]. Yet each of them has generally inadequate efficacy and a number of serious adverse effects [19]. Thus, plant-based compounds may be an alternative strategy for the food industry.
We collected and analyzed information on edible plants with antimicrobial compounds, including photodynamic phytochemicals. The aim of this review is to provide verified data on plant-based antimicrobial activities, and discuss the various mechanisms of their actions.
2. Antimicrobial Properties of Edible Plants
As already mentioned, many edible plants are important sources of antimicrobial compounds exhibiting high activity against both Gram-positive and Gram-negative bacteria (Table 1). Cultivated vegetables, fruits, nuts, herbs, and spices have been investigated more thoroughly than wild species; thus, they dominate the list (Table 1). Although more than 7000 species of wild edible plants are present in human nutrition [20], their antimicrobial properties are poorly investigated, and most of them still need to be studied [21,22].

Table 1.
Edible plants with antimicrobial properties.
A wide variety of compounds with different structures may have antimicrobial properties: polyphenols (phenolic acids, flavonoids, lignans, stilbenes, etc.); terpenoids, sulfides, coumarins, saponins, furils, alkaloids, polyines, thiophenes, different sugars, fatty oils, resins, glycosinolates, proteins, peptides, and others [23]. The quantitative distribution of the phytochemicals can vary from organ to organ or from plant to plant, depending on many factors: most notably, the plant genotype, growth conditions, developmental stage, soil, environmental conditions, agricultural practices, abiotic, and biotic stress [24].
Most edible plants are consumed after being cooked or dried. Frying, grilling, boiling, drying, and steaming are often detrimental to many phytochemicals.
Polyphenols, which occur in all plants, are the most potent antimicrobial compounds, especially phenolic acids and flavonoids. In cases where the identification and purification of active antimicrobial compounds from plants were not complete, the total phenol and flavonoid content was estimated, based on the high probability that the active phytochemicals belong to these groups.
Phenolic acids can be found in almost all edible plants. Antimicrobial properties of phenolic acids relate to the presence of double bonds and hydroxyl, methoxy, and carboxyl groups [25,26].
One phenolic acid is p-coumaric acid (4-hydroxycinnamic acid), which aroused interest because of contradicting reports on its antimicrobial activity. This compound exhibits antibacterial activity against three Gram-positive bacteria (Streptococcus pneumonia, Staphylococcus aureus, and Bacillus subtilis) and three Gram-negative bacteria (Escherichia coli, Shigella dysenteriae, and Salmonella typhimurium), eliminating bacterial cells via dual damage mechanisms: increasing the membrane permeability of the bacteria and binding to the phosphate anion of their DNA [27]. It was reported that p-coumaric acid demonstrated a much lower inhibitory activity against Staphylococcus aureus, and no inhibitory effect on Escherichia coli, Listeria monocytogenes, and Salmonella typhimurium [28]. In addition, it had no inhibitory effect on several Gram-positive bacteria and Gram-negative bacteria [29]. It was likewise found that p-coumaric acid was not effective against Klebsiella pneumonia, Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, and Proteus vulgaris; but a significant antimicrobial effect was observed in combination with syringaldehyde. It is noteworthy that syringaldehyde alone did not eliminate these microorganisms [30]. Thus, antimicrobial ability can be obtained in a synergistic action between p-coumaric acid and certain phytochemicals whose efficacy would be very low in its absence.
Chlorogenic acid is one of the most available acids among the phenolic acid compounds. It is a well-known component in green coffee extracts [31] and many other edible plants [32]. Its bactericidal effects against Stenotrophomonas maltophilia resistant to trimethoprim/sulfamethoxazole [33], Klebsiella pneumoniae [34], Helicobacter pylori [35], Escherichia coli [36], Staphylococcus epidermidis [37], and Staphylococcus aureus [38] were reported. In addition, chlorogenic acid had an inhibitory effect on the multidrug efflux systems of multidrug-resistant bacteria [38] and their biofilm formation [39]. On the other hand, it is not toxic against probiotic bacteria, which makes this compound suitable to use in the food industry [39].
Although caffeic acid is present in many edible plants, its antimicrobial properties were observed in propolis [40,41]. The caffeic acid enhanced the activity of several antibiotics against many bacterial strains [42,43,44]. The mechanism of its action is connected with the inhibition of the bacterial RNA polymerase enzyme [42]. Ferulic, p-coumaric, and sinapic acids of kidney beans also demonstrate antibacterial activity [42].
In many cases, there are synergistic or antagonistic reactions among phenolic acids and other compounds, which make the results from in vitro and in vivo studies variable.
Numerous antimicrobial flavonoids are present in many species of edible plants. Based on their differences in the phenyl-benzopyran core, flavonoids have been divided into several subgroups: flavanols, flavones, flavanones, anthocyanidins, and isoflavones. Several investigated mechanisms of their actions include the inhibition of nucleic acid synthesis via interference in bacterial type II topoisomerases (DNA gyrase and topoisomerase IV) activity [43]; inhibition of cytoplasmic membrane function [43]; inhibition of cell envelope synthesis [44]; inhibition of energy metabolism [43]; inhibition of cell-wall synthesis [43]; inhibition of efflux pumps in bacteria [45]; inhibition of bacterial enzyme-dependent virulence [46]; and membrane-disrupting activities [47,48]. In addition, the antiquorum sensing activity of flavonoids was reported [49,50]. Bacterial quorum sensing is a process of cell-to-cell communication that regulates genetic competence, bacterial colonization, biofilm formation, virulence, and other properties that make many bacteria more dangerous [3]. Although the mechanism of action of antiquorum-sensing flavonoids is still poorly understood, it became clear that the bacterial proteins TtgR in complex with flavonoids have properties that block the efflux pumps in bacteria [51]. In fact, epigallocatechin gallate is able to inhibit bacterial growth and suppress the expression of specific genes related to biofilm formation [52]. Remarkably, some flavonoids also inhibit bacterial toxins [53,54,55].
The antimicrobial activity of flavonoids is the result of a combination of several mechanisms. The flavonol morin is indicative of how many modes of actions are known, including promotion of bacterial aggregation, leakage of the cell membrane, intervention in the biofilm growth, suppression of the PBP2a-mediated resistant mechanism of action [56], and inhibition of bacterial enzyme-dependent virulence [57]. It is possible to improve antibiotic efficiency against bacteria using flavonoids as potentiators [58].
Stilbenes are nonflavonoid polyphenols found in a number of plant families, including Vitaceae. These compounds are produced in plants during the invasion of pathogens, with the most studied stilbene being resveratrol, a constitutive compound found in some foods and drinks such as red wine, of which it is a major component. Whereas resveratrol generally shows moderate antimicrobial activity, it is the precursor of more active derivatives such as pterostilbene and viniferin [59,60].
The vegetables of the Brassicaceae family are rich in glucosinolates, a group of sulfur-containing glucosides with significant antimicrobial properties [61]. At least 120 distinct glucosinolates have been identified [62]. Their modes of action include the breakdown of enzyme S-S bridges, DNA damage, and inhibition of bacterial cell growth and proliferation [63].
Terpenes are secondary metabolites (based on an isoprene structure) produced by all plants via two alternative metabolic pathways. The first is the mevalonate pathway in the cytoplasm, and the second is the methylerythritol phosphate pathway in the plastids [64]. These compounds have enormous structural diversity, with about 200,000 variants existing in nature [65]. Indeed, the terpenes are one of the most important classes of antimicrobial phytochemicals; they are mostly found in the form of essential oils [66].
Examination of the 33 terpenes frequently reported in the secondary metabolism of plants revealed that 16 of the 33 compounds showed antimicrobial activity at the initial screening. Higher antimicrobial activity was related to the presence of hydroxyl groups (phenolic and alcohol compounds), whereas hydrocarbons reduced that activity [67]. Support of this idea is found in terpineol and eugenol, whose antimicrobial properties were demonstrated in some studies [21,68]. Moreover, these compounds are able to cause dysfunction in the bacterial membrane [67]. It was found that essential oils and their compounds are divided into two groups: slow-acting and fast-acting [68]. It was reported that terpineol, eugenol, geraniol, carveol, and citronellol were fast-acting compounds, inactivating several bacterial organisms in a two-hour period [67]. A possible mechanism of their antimicrobial action is their ability to destroy cell membrane integrity by forming a phenolic cluster that initiates lipid–protein interaction, improves the membrane’s permeability, and results in leakage of the cellular contents [69,70].
Ursolic acid is a natural terpene identified in many edible plants, such as apples, marjoram leaves, oregano leaves, rosemary leaves, sage leaves, thyme leaves, black elder leaves and bark, hawthorn leaves and flowers, coffee leaves, and the wax layer of many fruits [71,72]. A number of studies have been performed to evaluate the antibacterial properties of ursolic acid [73,74,75]. Its antimicrobial mode of action is connected with its ability to influence the integrity of the bacterial membrane initially, followed by inhibition of protein synthesis and the metabolic pathway [76]. It was reported that ursolic acid is able to improve antibiotic activity [77,78].
Lupeol (phytosterol and triterpene) is identified in many edible vegetables and fruits; although it exhibits significant antimicrobial activity, the mechanism of its action is not clear [79].
The saponins are a subclass of terpenoids. There are three classes of saponins (triterpenoids, steroids and glycoalkaloids) based on their different aglycone structures [22]. The triterpenoid 18-β-glycyrrhetinic acid showed an antibiotic effect on Staphylococcus aureus by influencing some of its important genes [22]. In addition, this compound is an immunological adjuvant [80,81].
Six saponins from Chenopodium quinoa Willd. were identified; these compounds destroy the bacterial biofilm system. The mechanism of their action is related to disruption of the cytoplasmic membrane and membrane proteins [82].
Both licochalcone [83] and liquiritigenin were effective against Staphylococcus aureus [84]. In addition, licochalcone A inhibited the formation of biofilms in many cases [85].
Although Sapindus saponins are prevalent in nonedible plants, they have such broad-spectrum antibacterial effects that it is worthwhile to pay attention to these compounds. Screening of their antibacterial activity in various combinations against seven bacteria demonstrated that only the combination of Sapindoside A and B was effective against Micrococcus luteus, causing damage to cell membrane proteins [86]. Sapindus saponins (Mukurozisaponin E1, Rarasaponin II, Mukurozisaponin G, and Rarasa ponin VI) inhibited Propionibacterium acnes; the mechanism of their action is connected with suppressing the activities of bacterial enzymes, such as lipase and tyrosinase [87].
Two lignans (sesamin and sesamolin) found in Sesamum indicum (L.) had significant antiquorum sensing and antibiofilm properties against Pseudomonas aeruginosa. The possible mechanisms of action of the lignans were investigated; they influence LasR-mediated virulence factor production [88].
A number of antimicrobial phytochemicals have not yet been identified (Table 1). Whether the antimicrobial effects of many edible plants may be a synergy of multiple phytochemicals or a single component should be a focus for future investigations. In addition, various metabolites in plant extracts have synergic or antagonistic effects on antimicrobial activity.
3. Photosensitizers from Edible Plants as a Source of New Drugs
An important group of antimicrobial agents was mentioned in our Introduction: photosensitizers. Excitation of these compounds by light leads to the generation of reactive oxygen species (ROS) that damage pathogenic cells. Light is absorbed by a photosensitizer, leading to a photodynamic process which can develop either a type I or a type II process. The former results in the formation of free radicals, such as superoxide anion (O2−), hydroxyl radicals (OH·), and hydrogen peroxide (H2O2), which oxidize biomolecules. The type II process is characterized by the formation of singlet oxygen (1O2)—a highly reactive and strong oxidizing agent (Figure 1) [12,156,157]. ROS produced during the photodynamic process attack various targets outside of cells (for example, extracellular polysaccharides), on the surface of cells and inside them (such as proteins, lipids, and nucleic acids), and oxidize biomolecules, causing cell damage and ultimately their destruction [157,158,159]. The ratio between mechanisms I and II depends on the type of PS used and the microenvironment in which the photodynamic process occurs. Furthermore, an additional, oxygen-independent photoinactivation pathway has recently been proposed, a type III photochemical mechanism [160]. It includes photoinduced electron transfer, accompanied by the generation of reactive inorganic radicals which (according to the author’s assumption) then attack microbial cells.
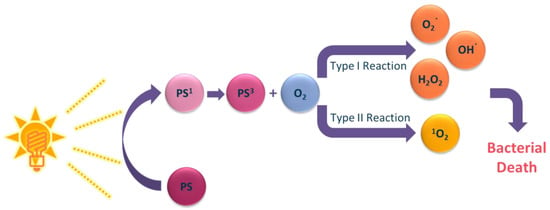
Figure 1.
Schematic presentation of light-mediated cell damage during photodynamic treatment.
Photodynamic therapy was discovered over a century ago. It has been studied and developed for many years for the treatment of cancer [161,162,163]. At the beginning of the 1990s, in response to the emergence of the first drug-resistant infections, interest was renewed in studying the antibacterial properties of PSs [164,165]. Since then, many “synthetic” PSs have been shown to be effective against various types of microorganisms [165,166,167,168]. The wider spectrum of PS action compared to antibiotics, their bactericidal efficacy regardless of antibiotic resistance, as well as a lack of development of resistance to them after several sessions of therapy, emphasize the potential of using photodynamic antimicrobial chemotherapy (PACT) for the eradication of various microorganisms, such as bacteria, protozoa, and fungi [11,169,170].
Natural products from plant and animal origins contain many bioactive components that are phototoxic when activated by light [19]. The cells of microorganisms, algae, plants, and animals produce pigments for various biological purposes: photochemical reactions, antioxidant activity, defense mechanisms, attraction of pollinators, etc. Some of these pigments are photoactive and exhibit the photodynamic properties required for therapeutic use [14]. To date, more than 100 natural compounds having photodynamic activity are known [14,171]. Both pure compounds and extracts are used as PSs for PACT [13].
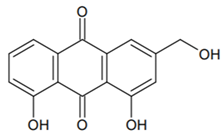
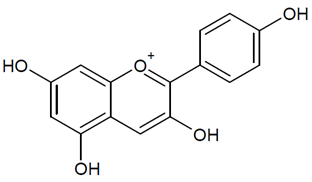
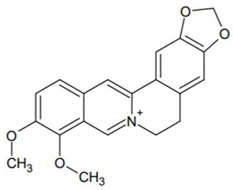
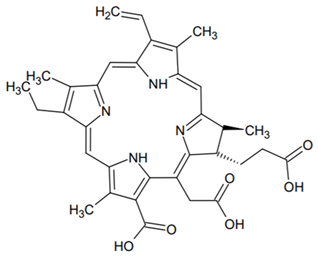
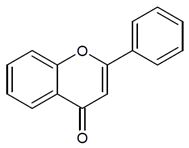
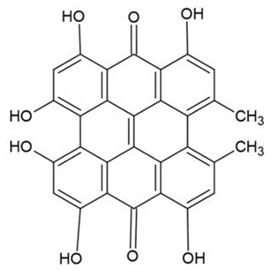
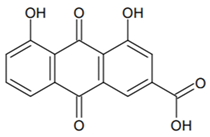
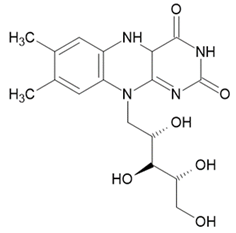
The main classes of natural PSs that can be found in edible plants are curcuminoids, anthraquinones, perylenequinones, furano-coumarins, alkaloids, chlorins, and flavins [13,14,171]. Table 2 presents structures of the most prospective antimicrobials from edible plants exhibiting photodynamic activity.

Table 2.
Structures of selected photosensitizers from edible plants.
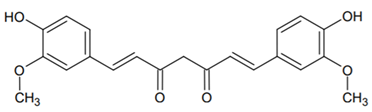
The curcuminoid class consists of four linear diarylheptanoids: dicinnamoylmethane, curcumin, demethoxycurcumin, and bisdemethoxycurcumin. These compounds have a wide range of pharmacological activities, including antiviral, anti-inflammatory, antitumor, and antibacterial properties [172,173,174]. The natural yellow pigment of curcumin (diferuloylmethane) is derived from the rhizomes of turmeric (Curcuma longa), which for centuries was widely used for nutritional and therapeutic purposes in Asian countries [175,176]. Curcumin demonstrates photodynamic activity when irradiated with blue light, leading to an increase in 1O2 production and induction of a strong phototoxic reaction [176]. The inhibitory effect of this pigment under illumination has been demonstrated against various Gram-positive and Gram-negative bacteria (Table 3), as well as against Candida sp. [177,178,179], human norovirus on food [180], and even against mosquito larvae [181]. Curcumin is known to participate in both type I and type II reactions [182], and its antibacterial activity is associated with damaging the membranes of bacterial cells [175,183]. However, poor water solubility, relatively low bioavailability, and intense staining limit the possibilities of using curcumin as a therapeutic agent [15].

Table 3.
Photodynamic antimicrobial phytochemicals from edible plants.
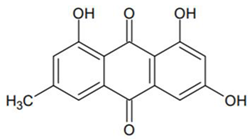
Anthraquinones (AQs) belong to a large family of compounds that are usually divided into monomeric and dimeric anthraquinones [13,15,171]. These compounds are produced by many species of flowering plants, as well as lichens and fungi. They can be found in any plant part: roots, rhizomes, leaves, flowers, and fruits [184]. Most of the studied plants containing AQ derivatives (81%) belong to the Polygonaceae, Rubiaceae, and Fabaceae families. The best known are: emodin, rhein, physcion, chrysophanol, catenarin, rubiadin, and pupurin [13,184]. AQs have a wide range of biological properties, including bactericidal, fungicidal, antioxidant, anti-inflammatory, anticancer, and many others [184]. For example, different research groups have demonstrated the photodynamic activity of aloe emodin from Rheum palmatum and Aloe vera against various bacteria [185,186,187] and fungi [188,189,190] (Table 3).
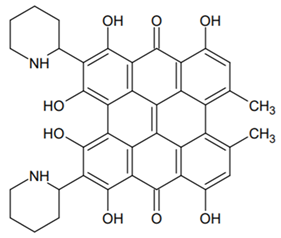
The perylenequinone (PQ) class, including hypericin, hypocrellins, elsinochromes, and others, has promising characteristics for photodynamic therapy [191]. PQs efficiently produce singlet oxygen, leading to a type II photodynamic process [171]. Their lipophilic nature helps them to penetrate cell membranes [14]. Major plant sources of PQs include herbs such as buckwheat (Fagopyrum esculentum) and St. John’s wort (Hypericum perforatum) [13]. For example, hypericin isolated from the latter is known for its antibacterial and antifungal properties (Table 3). At the same time, hypericin is poorly soluble in water; to increase efficiency of delivery, it was proposed to use liposomes or micelles [13,192]. The antimicrobial activity of some perylenequinones is summarized in Table 3, but it should be noted that a large number of PQ compounds have yet to be investigated for their photopharmaceutical properties [171].
Furanocoumarins (FCs) or psoralens are coumarins containing a furan ring, found in plants of the Rutaceae family (common rue (Ruta graveolens), bergamot fruits, lime, gas plant (Dictamnus albus), cloves (Syzygium aromaticum)); the Umbelliferae family (e.g., parsley (Petroselinum crispum), celery (Apium graveolens), parsnip (Pastinaca sativa)); the Moraceae family (figs (Ficus carica)); and others [14,171,193]. These compounds are phytoalexins, not normally found in uninfected tissues and appearing only when the plant is damaged by pathogens. Furthermore, the FC content is related to the growing season of the plant and can differ significantly before and after flowering [193].
FCs are incorporated into cell DNA in the dark; under the influence of UVA (ultraviolet A) or Vis illumination, a photochemical process then leads to the FC reacting with pyrimidine nucleobases. In addition, FC can react with RNA, cell membranes, and proteins; however, these reactions are less studied [171,193,194]. Moreover, under UVA illumination, psolarens can react with DNA in the absence of oxygen (type III photochemical mechanism) [160,195]. The antibacterial and antifungal activity of psolarens has been demonstrated (see Table 3), but their use for the treatment of humans is limited, due to possible toxicity [171,182].
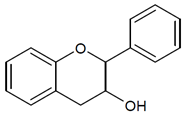
Alkaloids, the second largest group of natural products, contain a large number of photoactive compounds. These include quinoline (chinolin) alkaloids, pterins, benzylisoquinolines, beta-carbolines, and indigo alkaloids [13,171]. Many of them exhibit antimicrobial properties when exposed to light. For example, dictamnine (4-methoxyfuro [2,3-b] quinoline), found in many Rutaceae species such as Dictamnus albus, has been shown to be effective in killing yeast (Saccharomyces cerevisiae) and bacteria (E. coli) [196]. Among the edible plants containing alkaloids are Berberis species containing the well-known alkaloid berberine [197]. The light-dependent antibacterial properties of this compound have been demonstrated as effective against Gram-positive S. aureus and Gram-negative E. coli [198,199,200] (Table 3).
Chlorins belong to the class of tetrapyrroles, macrocyclic compounds widely known for their photodynamic properties. This group also includes porphyrins and bacteriochlorins [13,14,201]. Chlorophyll, the green pigment which plays a crucial role in photosynthesis, is found in plants, cyanobacteria, and eukaryotic algae. The most studied plant sources of chlorophyll are spinach, green cabbage, and dandelion [14,15,202]. Chlorophyll derivatives, chlorins, have strong photodynamic properties and generate large amounts of singlet oxygen (type II photodynamic mechanism) which are not accompanied by the formation of toxic byproducts [203]. However, their poor solubility and low photostability limit their use [13,182].
Flavins, yellow-colored compounds with the basic structure of 7,8-dimethyl-10-alkylisoalloxazine, are widespread in nature and are involved in many biochemical reactions [204]. A well-known representative of flavins, riboflavin (vitamin B2), is synthesized by a wide range of organisms, including plants, fungi, bacteria, and animals [13,205]. When exposed to visible or ultraviolet light, riboflavin generates singlet oxygen, hydrogen peroxide, hydroxyl, and superoxide radicals exhibiting photodynamic properties (type I or type II mechanisms, depending on the oxygen concentration) [14,182,206,207]. Edible plants rich in riboflavin are green leafy vegetables (for example, spinach), dark-green vegetables (for example, asparagus), nuts (for example, almonds) and legumes (for example, soybeans) [208,209,210]. The antimicrobial activity of riboflavin under illumination has been demonstrated against a variety of microorganisms (Table 3).
4. Use of Natural Plant Antimicrobials for Food Disinfection
The main demands concerning food are freshness, naturalness, and minimal processing. The concept of naturalness relates to healthy and unmodified food without chemical preservatives. However, consuming raw fruits, vegetables, fruit juices, and sprouts may cause foodborne outbreaks of illness [294].
Conventional methods of microbial inactivation and food decontamination include thermal processing, sanitization, water washing, drying, freezing, refrigeration, irradiation, modified atmosphere packaging (MAP), and the addition of antimicrobial agents, disinfectants, or salts. Irradiation, heat, high pressure, magnetic or electrical fields, and ultrasound are microbial inactivation methods that do not induce microbial resistance [16,57,294,295]. Water washing and sanitization reduce bacterial load with limited success, and disinfectants might cause genotoxicity and carcinogenicity. In addition, thermal processing reduces the level of some bioactive compounds such as anthocyanin pigment, carotenoids, and vitamin C, which can be found in several fruits. Therefore, nonthermal technologies, such as dense-phase carbon dioxide (DPCD), high hydrostatic pressure (HHP), ultraviolet or ozone processing, pulsed electric fields (PEF), and ultrasound, have been studied and analyzed, with promising results.
Each technique was developed for different phases, pigments, geometries, and goals (for instance, for control of microorganisms and inactivation of pathogens on the surface of solid foods vs. the total interior volume of liquids). The DPCD technique is generally used for liquid foods, since the pressure involved damages the tissues of fruits. In PEF, high intensity and long processing affect the nutritional quality of foods. For surface decontamination of food, both UV-C and ozone treatments can be used; however, they are limited to topical applications only. Moreover, a high dosage of ozone processing alters the sensory quality of the food. Although HHP is a size- and geometry-independent treatment, it needs water or sufficient humidity content within the sample in order to avoid structural and/or textural changes. Chemical preservatives such as sugar, acids, and salts (sodium benzoate, potassium sorbate, nitrites, and nitrates) are used commercially in fruits, dairy products, confections, meats and meat products, etc. [294,295]. However, growing evidence of the harmful effects and health risks of these chemical preservatives leaves no other option but to find new methods that will reduce their amounts in foods. The optimal alternative is to substitute appropriate additives that have no adverse effects. To achieve these goals, good candidates are natural antimicrobial compounds such as bacteriocins, chitosan-fermented ingredients, and plant antimicrobials, especially plant extracts and plant-isolated compounds exhibiting a broad-spectrum activity.
The antimicrobial and antioxidant properties of plant extracts are attributed to secondary metabolites such as phenylpropanoids, terpenes, flavonoids, and anthocyanins. Since plants are easily attacked by insects, fungi, and bacteria, they develop an efficient defense system against pathogens by producing secondary metabolites, such as phenols, oxygen-substituted derivatives, terpenoids, quinines, tannins, and antimicrobial peptides (AMPs). The most promising biopreservative plant products are essential oils, plant AMPs, and plant extracts in either pure or crude form [294].
5. Essential Oils
Liquid essential oils can be derived from several plant parts: flowers, buds, leaves, fruits, twigs, bark, seed, wood, and roots. In the food industry, essential oils serve as flavoring agents; however, their antimicrobial and antioxidant traits make them the best candidates for food preservation. Their chemical structure and active functional groups change with the types of plants, season, harvesting time, and methods of extraction. The main active groups of essential oil compounds that are correlated with antimicrobial properties are terpenes, terpenoids, phenylpropenes, and other chemical groups [294].
To date, the mechanism of operation is not clearly defined. There is no proof of a mechanism driven by chemically active functional groups, but only a general assumption of the oil penetrating the bacterial cell membrane due to its lipophilic nature, thus disrupting cell function. It was suggested that oil compounds, possessing a phenolic functional group, change the permeability of the bacteria cell membrane and hinder the generation of ATP. Moreover, low concentrations of essential oil inhibit enzymes that are involved in energy production, and in high concentrations it precipitates the protein. Since essential oil is hydrophobic, it is more effective against Gram-positive than Gram-negative bacteria; this is probably attributable to the difference in their cell structure, especially the cell envelope [294].
Different studies have demonstrated the effectiveness of essential oils in both fresh-cut fruit and juices (Table 4). Moreover, essential oil obtained from pink pepper (native to Brazil, Paraguay, and Argentina) exhibited antimicrobial and antioxidant action in cheese, with only 2% concentration [294]. Basil essential oil added to beef burger reduced the growth of Staphylococcus aureus from 3 log10 CFU/g to 2 log10 CFU/g at 4 °C after 24 h [294]. Treatments with both clove oil and cumin oil enhanced the shelf life of red meat at 2 °C for ~15 days, and reduced the bacterial concentration by ~3.78 log10, compared to control measurements. The combination of thyme essential oil added at 0.4, 0.8, and 1.2%, and nisin at 500 or 1000 IU/g, exhibited stronger antimicrobial activity than their individual usage, decreasing a Listeria monocytogenes population to below 2 log10 CFU/g in minced fish during storage at 4 °C for 12 days [294].

Table 4.
Plant antimicrobials for food disinfection and conservation.
Another synergetic effect was proven in the combination of Zataria multiflora Boiss essential oil and grapeseed extract in concentrations of 0.1% and 0.2%, respectively, which showed antioxidant activity and effective growth control of Listeria monocytogenes in raw buffalo patty. Another study showed that sage and thyme oils exhibited strong antimicrobial activity against vancomycin-resistant Enterococci and E. coli in minced beef meat [294].
6. Antimicrobial Peptides
AMPs are a part of a plant’s secondary metabolite defense system. They are widely distributed in plants, plant parts, and the immune system; they participate in enzymatic networks engaged in metabolism as nutrients and storage molecules [294]. AMPs are the first line of defense against invading pathogens, as biologically active peptides with antimicrobial, antioxidant, antithrombotic, antihypertensive, and immunomodulatory properties.
Due to their amphophilic nature and the presence of positively charged residues, they can penetrate bacterial membranes and alter their permeability. There are two types of AMPs: peptides produced without the involvement of ribosomes (bacitracins and glycopeptides), and peptides synthesized via the ribosomal pathway. The latter peptides participate in the immune defense system of the organism’s body. To extract and save crucial information about AMPs, an online antimicrobial peptide database was opened in 2003, with more than 2600 different peptides identified to date. The antifungal activity of AMPs is based on their attack on the fungal cell wall, especially a chitin component that hinders its synthesis and changes the membrane permeability. AMPs also exhibit antiviral activity, in which they bind the glycosaminoglycan moiety of the cell membrane and prevent interaction between the virus and the cell. Bacterial antimicrobial peptides, such as bacteriocins, have been used in food preservation for many years [294].
7. Plant Extracts
Since ancient times, spices and herbs have been used not only as flavoring agents but also as preservatives. These plant extracts include leaves such as mint and rosemary, flowers such as cloves (containing eugenol, which is associated with antibacterial activity), bulbs such as garlic and onion, and fruits such as cumin and red chili.
Antimicrobial activity in plant extracts is determined by their phytochemicals. Phenolics, phenolic acids, quinones, saponins, flavonoids, tannins, coumarins, terpenoids, and alkaloids are the major classes of chemical constituents that affect the antimicrobial and antioxidant activity, as well as the flavor of the plant. The hydroxyl group of the phenolic compounds interrupts the functionality of bacterial cell membranes and shifts the electrons, reducing the proton-motive force and inhibiting ATP synthesis, causing cell death. Cinnamaldehyde inhibits bacteria cell-wall synthesis, impairing cell membrane function and affecting the synthesis of nucleic acids. The antioxidant activity of extracts from many plants, such as rosemary, oregano, thyme, sage, marjoram, basil, coriander, and pimento, is attributed to their phenolic component. Phenolic compounds of black pepper damage bacterial membranes and increase antimicrobial activity. Selection of a proper solvent for extraction from plants is crucial for preserving their antioxidant properties [294].
8. Limitations in Plant Antimicrobials as Food Preservatives
The US FDA and the European Commission approved some essential oils as food preservatives. The main obstacle encountered in their use is irreproducibility of a standard quality. Essential oils have different qualitative and quantitative fluctuations in their chemical composition, which influence their biological activity [294]. In addition, their strong aromas or flavors alter the organoleptic properties of foods and might reduce the appeal of some food products. Although there are several in vitro studies of the antimicrobial activity of plants, they are barely relevant to the application of essential oils for food preservation, since in most cases the results of in vitro antimicrobial activity of plant extracts differed from those observed in food. In the latter, the low activity was due to the use of crude extracts, instead of pure compounds which possess higher potency. Crude extract comprises flavonoids in a glycosidic form, which hinders their effectiveness against microorganisms. The presence of an extracting solvent also creates an obstacle for using plant extracts in food. Thus, the use of antimicrobial peptides derived from plants in food is still at its early stage. More research is needed in order to confirm their potential as food preservatives [294].
9. Ultrasonic Activation
Recently, new technology was proposed for control and inactivation or eradication of microorganisms. This technology, based on treatment by low-frequency, high-power ultrasound (US), is considered to be very promising, since it is a nonthermal technology and does not induce microbial resistance.
As mentioned before, total volume depth phase performance (beyond the solid surface) is very crucial for foodborne pathogenic treatments; therefore, US is a more broad-scale method for activation of sensitizers than PDT with its very limited deep-phase penetration ability. Moreover, US may promote more uniform dispersion of a sensitizer in the growth medium. Generally, US is the transmittance of physical pressure (in longitudinal and transverse waves) through a medium at frequencies of more than 20 kHz, which is above the human hearing range [16,314]. US is already extensively applied in medicine and biology; it is now reaching the field of waterborne and foodborne disease prevention. The US technology enables deep penetration into biological tissues while retaining the treated food’s nutrient quality. This is in addition to other advantages: environmentally friendly, low-energy consumption; reduced chemical and physical hazards; shorter processing time; safe and convenient operation; relatively low cost and easy focus. In liquids, its mode of action against microbes involves intracellular cavitation and microstreaming around growing and collapsing cavitation bubbles, with speeds and shear rates producing shock waves and microjets (resulting from the bubble collapse), together with ROS formation in situ during the interaction between ultrasound, sonosensitizer, and molecular oxygen; all of which results in bacterial cell death.
However, US treatment alone, without the use of a sensitizer, requires higher intensity and might be dependent on the oxygen environment. Thus, activation of a natural sensitizer by US under normal oxygen conditions seems to be the most promising solution. This technique, called sonodynamic therapy, uses low-intensity ultrasound.
The factors that affect the efficacy of US on microbial decontamination are the US amplitude, exposure duration, treatment temperature, traits of the food, and the volume being processed [16,314,315,316]. In a recent study by Bhavya (2019), the influence of US on 50 and 100 µM curcumin-mediated PDT treated by blue light (70 J cm−2) against E. coli and S. aureus in freshly squeezed orange juice was investigated and analyzed [183].
The effect of US as a pretreatment in the presence and absence of PS, and in combination of PS with blue light, was also studied. It was observed that the effect of US on the inactivation of E. coli was dependent on the US intensity. The E. coli concentration was reduced by 3.02 ± 0.52 log10 CFU mL−1 when treated with US alone at 50 W cm−2. However, in the case of S. aureus, the US alone did not cause any significant inactivation of bacteria. It was suggested that these results were due to the structural difference between E. coli and S. aureus bacteria. US treatment in the presence of PS did not show any significant change in the E. coli concentration, but it did cause a significant decrease in the S. aureus concentration, compared to the US treatment alone (at 50 W cm−2). The results confirmed that the S. aureus bacteria were eradicated due to sonodynamic inactivation. The combined treatment of PS, US, and blue light showed a reduction in the E. coli concentration by 4.26 ± 0.32 log10 CFU mL−1, while S. aureus was only reduced by 2.35 ± 0.16 log10 CFU mL−1. This result showed a synergetic effect on the inactivation of the tested bacteria. Another study investigated sonodynamic action using curcumin on foodborne bacteria B. cereus and E. coli [315]. The sonodynamic antibacterial activity of curcumin on B. cereus was observed when the concentration of curcumin was 0.5 µM, and a concentration of 2.0 µM achieved a profound 5.6 log10 CFU mL−1 reduction of bacterial concentration. However, in the case of E. coli, the sonodynamic action of curcumin caused an antibacterial effect at a concentration of 20 µM, whereas when bacteria were treated by curcumin alone at 40 µM, the cell concentration was reduced by 2 log10 CFU mL−1 only. These results showed that curcumin at low concentrations exhibited sonodynamic antibacterial effects on B. cereus, while in the case of E. coli a higher concentration of curcumin and longer sonication time were needed to inhibit the cell growth. Gram-positive B. cereus was more sensitive to the curcumin sonodynamic treatment than the Gram-negative E. coli, probably because of a dense double outer membrane on the Gram-negative bacteria which interferes with the curcumin penetration into cells and mediates higher resistance of bacteria to disinfectants.
The mechanism of ROS generation under acoustic cavitation is not fully understood. The main hypothesis suggests that the energy release is due to the collapsing microbubbles, which lead to the sonolysis of water and/or sensitizer molecules. In this way, the resulting radicals react with oxygen to form ROS [16]. As in the case of classical photodynamic therapy, sonoluminescence may cause either the type I process, leading to the formation of secondary radicals, or the type II process, in which mainly singlet oxygen eradicates the pathogenic cells. US can damage not only Gram-positive and Gram-negative bacteria, but also yeasts, fungi, algae, and even viruses.
Unfortunately, all the key factors for bacteria eradication, such as sonication frequency, intensity, and pulse cycle, might not be effective in vivo, due to the different susceptibility levels of prokaryotes and eukaryotes to ultrasonic energy. Unlike eukaryotic cells, bacteria respond to the maximum (peak) ultrasound intensity, and not to the total amount of transmitted energy (more precisely, the average cumulative ultrasound intensity). Therefore, it is necessary to choose the suitable parameters when using ultrasound energy, selecting a peak high enough and average intensity low enough to maximize bacterial damage without damaging surrounding cells and tissues [16].
The effect of ultrasound activation on foodborne pathogenic eradication still requires further in-depth study.
10. Conclusions
In many cases, studies on antimicrobial effects of edible plants do not focus on the identification of antimicrobial phytochemicals and their modes of action. Among these phytochemicals, polyphenols are the most potent antimicrobial compounds, especially phenolic acids and flavonoids. In some cases, various plant metabolites tend to have synergic or antagonistic effects against both Gram-positive and Gram-negative bacteria. The data presented in this review support the idea that the antimicrobial activity of the plant compounds is the result of a combination of several mechanisms.
Edible plants offer a promising therapeutic potential, especially in the case of antimicrobial compounds such as PSs. Future research priorities should include the identification of PSs and a better understanding of the mechanisms of the phytochemical activity of the plants. Being potent antimicrobial agents, PSs can serve as effective food preservatives. Further studies are necessary to improve antibiotic efficiency of PSs and other phytochemicals.
Author Contributions
Conceptualization, F.N., L.Y. and S.B.-S.; writing—original draft preparation, E.H., L.Y., F.N. and B.K.; writing—review and editing, M.N., F.N. and L.Y.; supervision, S.B.-S.; project administration, F.N. and M.N.; funding acquisition, M.N. and F.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We acknowledge the Research Authorities of the Ariel University for supporting this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Thomford, N.E.; Senthebane, D.A.; Rowe, A.; Munro, D.; Seele, P.; Maroyi, A.; Dzobo, K. Natural products for drug discovery in the 21st century: Innovations for novel drug discovery. Int. J. Mol. Sci. 2018, 19, 1578. [Google Scholar] [CrossRef] [PubMed]
- Verpoorte, R. Pharmacognosy in the new millennium: Leadfinding and biotechnology. J. Pharm. Pharmacol. 2000, 52, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Yarmolinsky, L.; Bronstein, M.; Gorelick, J. Review: Inhibition of bacterial quorum sensing by plant extracts. Isr. J. Plant Sci. 2015, 62, 294–297. [Google Scholar] [CrossRef]
- Yarmolinsky, L.L.; Budovsky, A.; Yarmolinsky, L.L.; Khalfin, B.; Glukhman, V.; Ben-Shabat, S. Effect of bioactive phytochemicals from phlomis viscosa poiret on wound healing. Plants 2019, 8, 609. [Google Scholar] [CrossRef] [PubMed]
- Zaccai, M.; Yarmolinsky, L.; Khalfin, B.; Budovsky, A.; Gorelick, J.; Dahan, A.; Ben-Shabat, S. Medicinal Properties of Lilium candidum L. and Its Phytochemicals. Plants 2020, 9, 959. [Google Scholar] [CrossRef]
- Sharma, H.B.; Panigrahi, S.; Sarmah, A.K.; Dubey, B.K. Antibacterial and antibiofilm activities of Mayan medicinal plants against Methicillinsusceptible and -resistant strains of Staphylococcus aureus. Sci. Total Environ. 2019, 135907. [Google Scholar] [CrossRef]
- Wang, Z.; Zhou, Y.; Shi, X.; Xia, X.; He, Y.; Zhu, Y.; Xie, T.; Liu, T.; Xu, X.; Luo, X. Comparison of chemical constituents in diverse zanthoxylum herbs, and evaluation of their relative antibacterial and nematicidal activity. Food Biosci. 2021, 42, 101206. [Google Scholar] [CrossRef]
- Newman, D.J.; Cragg, G.M. Natural Products as Sources of New Drugs over the Nearly Four Decades from 01/1981 to 09/2019. J. Nat. Prod. 2020, 83, 770–803. [Google Scholar] [CrossRef]
- Escolà-Vergé, L.; Los-Arcos, I.; Almirante, B. New antibiotics for the treatment of infections by multidrug-resistant microorganisms. Med. Clín. Engl. Ed. 2020, 154, 351–357. [Google Scholar] [CrossRef]
- Neuman, H.; Forsythe, P.; Uzan, A.; Avni, O.; Koren, O. Antibiotics in early life: Dysbiosis and the damage done. FEMS Microbiol. Rev. 2018, 42, 489–499. [Google Scholar] [CrossRef]
- Abrahamse, H.; Hamblin, M.R. New photossensitizersfot photodynamic therapy. Biochem. J. 2017, 473, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Wozniak, A.; Grinholc, M. Combined Antimicrobial Activity of Photodynamic Inactivation and Antimicrobials-State of the Art. Front. Microbiol. 2018, 9, 930. [Google Scholar] [CrossRef] [PubMed]
- Polat, E.; Kang, K. Natural photosensitizers in antimicrobial photodynamic therapy. Biomedicines 2021, 9, 584. [Google Scholar] [CrossRef] [PubMed]
- Christina Pires Gonçalves, L. Photophysical properties and therapeutic use of natural photosensitizers. J. Photochem. Photobiol. 2021, 7, 100052. [Google Scholar] [CrossRef]
- Foresto, E.; Gilardi, P.; Ibarra, L.E.; Cogno, I.S. Light-activated green drugs: How we can use them in photodynamic therapy and mass-produce them with biotechnological tools. Phytomedicine Plus 2021, 1, 100044. [Google Scholar] [CrossRef]
- Nakonechny, F.; Nisnevitch, M. Different Aspects of Using Ultrasound to Combat Microorganisms. Adv. Funct. Mater. 2021, 2011042. [Google Scholar] [CrossRef]
- Yadav, A.; Kumar, A.; Das, M.; Tripathi, A. Sodium benzoate, a food preservative, affects the functional and activation status of splenocytes at non cytotoxic dose. Food Chem. Toxicol. 2016, 88, 40–47. [Google Scholar] [CrossRef]
- Ren, L.; Meng, M.; Wang, P.; Xu, Z.; Eremin, S.A.; Zhao, J.; Yin, Y.; Xi, R. Determination of sodium benzoate in food products by fluorescence polarization immunoassay. Talanta 2014, 121, 136–143. [Google Scholar] [CrossRef]
- Seidi Damyeh, M.; Mereddy, R.; Netzel, M.E.; Sultanbawa, Y. An insight into curcumin-based photosensitization as a promising and green food preservation technology. Compr. Rev. Food Sci. Food Saf. 2020, 19, 1727–1759. [Google Scholar] [CrossRef]
- Ceccanti, C.; Landi, M.; Benvenuti, S.; Pardossi, A.; Guidi, L. Mediterranean Wild Edible Plants: Weeds or “New Functional Crops”? Molecules 2018, 23, 2299. [Google Scholar] [CrossRef]
- Abdel-Reheem, M.A.T.; Oraby, M.M. Anti-microbial, cytotoxicity, and necrotic ripostes of Pimpinella anisum essential oil. Ann. Agric. Sci. 2015, 60, 335–340. [Google Scholar] [CrossRef]
- Abdelrahman, M.; Jogaiah, S. Saponins Versus Plant Fungal Pathogens. Bioact. Mol. Plant Def. 2020, 37–45. [Google Scholar] [CrossRef]
- Budovsky, A.; Yarmolinsky, L.; Ben-Shabat, S. Effect of medicinal plants on wound healing. Wound Repair Regen. 2015, 23, 171–183. [Google Scholar] [CrossRef]
- Isah, T. Stress and defense responses in plant secondary metabolites production. Biol. Res. 2019, 52, 39. [Google Scholar] [CrossRef]
- Sánchez-Maldonado, A.F.; Schieber, A.; Gänzle, M.G. Structure-function relationships of the antibacterial activity of phenolic acids and their metabolism by lactic acid bacteria. J. Appl. Microbiol. 2011, 111, 1176–1184. [Google Scholar] [CrossRef]
- Liu, J.; Du, C.; Beaman, H.T.; Monroe, M.B.B. Characterization of Phenolic Acid Antimicrobial and Antioxidant Structure-Property Relationships. Pharmaceutics 2020, 12, 419. [Google Scholar] [CrossRef]
- Lou, Z.; Wang, H.; Rao, S.; Sun, J.; Ma, C.; Li, J. p-Coumaric acid kills bacteria through dual damage mechanisms. Food Control 2012, 25, 550–554. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, M.; Zhao, Z.; Yu, S. The antibiotic activity and mechanisms of sugarcane (Saccharum officinarum L.) bagasse extract against food-borne pathogens. Food Chem. 2015, 185, 112–118. [Google Scholar] [CrossRef]
- Alves, M.J.; Ferreira, I.C.F.R.; Froufe, H.J.C.; Abreu, R.M.V.; Martins, A.; Pintado, M. Antimicrobial activity of phenolic compounds identified in wild mushrooms, SAR analysis and docking studies. J. Appl. Microbiol. 2013, 115, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Vamsi Krishna, N.A.; Saradhi, P.M. Cumulative activity of the p-coumaric acid and syringaldehyde for antimicrobial activity of different microbial strains. Pelagia Res. Libr. Eur. J. Exp. Biol. 2014, 4, 40–43. [Google Scholar]
- Kulapichitr, F.; Borompichaichartkul, C.; Fang, M.; Suppavorasatit, I.; Cadwallader, K.R. Effect of post-harvest drying process on chlorogenic acids, antioxidant activities and CIE-Lab color of Thai Arabica green coffee beans. Food Chem. 2022, 366, 130504. [Google Scholar] [CrossRef]
- Santana-Gálvez, J.; Cisneros-Zevallos, L.; Jacobo-Velázquez, D.A. Chlorogenic Acid: Recent Advances on Its Dual Role as a Food Additive and a Nutraceutical against Metabolic Syndrome. Molecules 2017, 22, 358. [Google Scholar] [CrossRef] [PubMed]
- Karunanidhi, A.; Thomas, R.; van Belkum, A.; Neela, V. In vitro antibacterial and antibiofilm activities of chlorogenic acid against clinical isolates of Stenotrophomonas maltophilia including the trimethoprim/sulfamethoxazole resistant strain. Biomed Res. Int. 2013, 2013, 392058. [Google Scholar] [CrossRef] [PubMed]
- Bajko, E.; Kalinowska, M.; Borowski, P.; Siergiejczyk, L.; Lewandowski, W. 5-O-Caffeoylquinic acid: A spectroscopic study and biological screening for antimicrobial activity. LWT-Food Sci. Technol. 2016, 65, 471–479. [Google Scholar] [CrossRef]
- Farzaei, M.H.; Abdollahi, M.; Rahimi, R. Role of dietary polyphenols in the management of peptic ulcer. World J. Gastroenterol. 2015, 21, 6499–6517. [Google Scholar] [CrossRef]
- Ayseli, M.T.; İpek Ayseli, Y. Flavors of the future: Health benefits of flavor precursors and volatile compounds in plant foods. Trends Food Sci. Technol. 2016, 48, 69–77. [Google Scholar] [CrossRef]
- Fu, L.; Lu, W.; Zhou, X. Phenolic Compounds and In Vitro Antibacterial and Antioxidant Activities of Three Tropic Fruits: Persimmon, Guava, and Sweetsop. Biomed Res. Int. 2016, 2016, 4287461. [Google Scholar] [CrossRef]
- Sousa, R.; Muñoz-Mahamud, E.; Quayle, J.; Dias da Costa, L.; Casals, C.; Scott, P.; Leite, P.; Vilanova, P.; Garcia, S.; Ramos, M.H.; et al. Is asymptomatic bacteriuria a risk factor for prosthetic joint infection? Clin. Infect. Dis. 2014, 59, 41–47. [Google Scholar] [CrossRef]
- Puupponen-Pimiä, R.; Nohynek, L.; Meier, C.; Kähkönen, M.; Heinonen, M.; Hopia, A.; Oksman-Caldentey, K.M. Antimicrobial properties of phenolic compounds from berries. J. Appl. Microbiol. 2001, 90, 494–507. [Google Scholar] [CrossRef]
- Aljadi, A.M.; Yusoff, K.M. Isolation and identification of phenolic acids in Malaysian honey with antibacterial properties. Turkish J. Med. Sci. 2003, 33, 229–236. [Google Scholar]
- Chun, S.-S.; Vattem, D.A.; Lin, Y.-T.; Shetty, K. Phenolic antioxidants from clonal oregano (Origanum vulgare) with antimicrobial activity against Helicobacter pylori. Process Biochem. 2005, 40, 809–816. [Google Scholar] [CrossRef]
- Amarowicz, R.; Dykes, G.A.; Pegg, R.B. Antibacterial activity of tannin constituents from Phaseolus vulgaris, Fagoypyrum esculentum, Corylus avellana and Juglans nigra. Fitoterapia 2008, 79, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Pommier, Y.; Leo, E.; Zhang, H.; Marchand, C. DNA topoisomerases and their poisoning by anticancer and antibacterial drugs. Chem. Biol. 2010, 17, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Elmasri, W.A.; Zhu, R.; Peng, W.; Al-Hariri, M.; Kobeissy, F.; Tran, P.; Hamood, A.N.; Hegazy, M.F.; Paré, P.W.; Mechref, Y. Multitargeted Flavonoid Inhibition of the Pathogenic Bacterium Staphylococcus aureus: A Proteomic Characterization. J. Proteome Res. 2017, 16, 2579–2586. [Google Scholar] [CrossRef] [PubMed]
- Ramalhete, C.; Spengler, G.; Martins, A.; Martins, M.; Viveiros, M.; Mulhovo, S.; Ferreira, M.-J.U.; Amaral, L. Inhibition of efflux pumps in methicillin-resistant Staphylococcus aureus and Enterococcus faecalis resistant strains by triterpenoids from Momordica balsamina. Int. J. Antimicrob. Agents 2011, 37, 70–74. [Google Scholar] [CrossRef]
- Liu, B.; Chen, F.; Bi, C.; Wang, L.; Zhong, X.; Cai, H.; Deng, X.; Niu, X.; Wang, D. Quercitrin, an inhibitor of Sortase A, interferes with the adhesion of Staphylococcal aureus. Molecules 2015, 20, 6533–6543. [Google Scholar] [CrossRef]
- Cushnie, T.P.T.; Lamb, A.J. Recent advances in understanding the antibacterial properties of flavonoids. Int. J. Antimicrob. Agents 2011, 38, 99–107. [Google Scholar] [CrossRef]
- Tsuchiya, H. Membrane Interactions of Phytochemicals as Their Molecular Mechanism Applicable to the Discovery of Drug Leads from Plants. Molecules 2015, 20, 18923–18966. [Google Scholar] [CrossRef]
- Ouyang, J.; Sun, F.; Feng, W.; Sun, Y.; Qiu, X.; Xiong, L.; Liu, Y.; Chen, Y. Quercetin is an effective inhibitor of quorum sensing, biofilm formation and virulence factors in Pseudomonas aeruginosa. J. Appl. Microbiol. 2016, 120, 966–974. [Google Scholar] [CrossRef]
- Ilk, S.; Sağlam, N.; Özgen, M.; Korkusuz, F. Chitosan nanoparticles enhances the anti-quorum sensing activity of kaempferol. Int. J. Biol. Macromol. 2017, 94, 653–662. [Google Scholar] [CrossRef]
- Terán, W.; Krell, T.; Ramos, J.L.; Gallegos, M.-T. Effector-repressor interactions, binding of a single effector molecule to the operator-bound TtgR homodimer mediates derepression. J. Biol. Chem. 2006, 281, 7102–7109. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.; Tan, K.S. Effects of Epigallocatechin gallate against Enterococcus faecalis biofilm and virulence. Arch. Oral Biol. 2015, 60, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Rasul, A.; Millimouno, F.M.; Ali Eltayb, W.; Ali, M.; Li, J.; Li, X. Pinocembrin: A Novel Natural Compound with Versatile Pharmacological and Biological Activities. Biomed Res. Int. 2013, 2013, 379850. [Google Scholar] [CrossRef] [PubMed]
- Soromou, L.W.; Zhang, Y.; Cui, Y.; Wei, M.; Chen, N.; Yang, X.; Huo, M.; Baldé, A.; Guan, S.; Deng, X.; et al. Subinhibitory concentrations of pinocembrin exert anti-Staphylococcus aureus activity by reducing α-toxin expression. J. Appl. Microbiol. 2013, 115, 41–49. [Google Scholar] [CrossRef]
- Cherubin, P.; Garcia, M.C.; Curtis, D.; Britt, C.B.T.; Craft Jr, J.W.; Burress, H.; Berndt, C.; Reddy, S.; Guyette, J.; Zheng, T.; et al. Inhibition of Cholera Toxin and Other AB Toxins by Polyphenolic Compounds. PLoS ONE 2016, 11, e0166477. [Google Scholar] [CrossRef]
- Yang, J.Y.; Lee, H.S. Evaluation of antioxidant and antibacterial activities of morin isolated from mulberry fruits (Morus alba L.). J. Korean Soc. Appl. Biol. Chem. 2012, 55, 485–489. [Google Scholar] [CrossRef]
- Wang, J.; Zhou, X.; Liu, S.; Li, G.; Shi, L.; Dong, J.; Li, W.; Deng, X.; Niu, X. Morin hydrate attenuates Staphylococcus aureus virulence by inhibiting the self-assembly of α-hemolysin. J. Appl. Microbiol. 2015, 118, 753–763. [Google Scholar] [CrossRef]
- Brynildsen, M.P.; Winkler, J.A.; Spina, C.S.; MacDonald, I.C.; Collins, J.J. Potentiating antibacterial activity by predictably enhancing endogenous microbial ROS production. Nat. Biotechnol. 2013, 31, 160–165. [Google Scholar] [CrossRef]
- Chalal, M.; Klinguer, A.; Echairi, A.; Meunier, P.; Vervandier-Fasseur, D.; Adrian, M. Antimicrobial Activity of Resveratrol Analogues. Molecules 2014, 19, 7679–7688. [Google Scholar] [CrossRef]
- Chong, J.; Poutaraud, A.; Hugueney, P. Metabolism and roles of stilbenes in plants. Plant Sci. 2009, 177, 143–155. [Google Scholar] [CrossRef]
- Petersen, A.; Wang, C.; Crocoll, C.; Halkier, B.A. Biotechnological approaches in glucosinolate production. J. Integr. Plant Biol. 2018, 60, 1231–1248. [Google Scholar] [CrossRef] [PubMed]
- Verkerk, R.; Schreiner, M.; Krumbein, A.; Ciska, E.; Holst, B.; Rowland, I.; De Schrijver, R.; Hansen, M.; Gerhäuser, C.; Mithen, R.; et al. Glucosinolates in Brassica vegetables: The influence of the food supply chain on intake, bioavailability and human health. Mol. Nutr. Food Res. 2009, 53 (Suppl. 2), S219. [Google Scholar] [CrossRef]
- Saladino, F.; Bordin, K.; Luciano, F.B.; Franzón, M.F.; Mañes, J.; Meca, G. Antimicrobial Activity of the Glucosinolates BT-Glucosinolates; Mérillon, J.-M., Ramawat, K.G., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 249–274. ISBN 978-3-319-25462-3. [Google Scholar]
- Eisenreich, W.; Rohdich, F.; Bacher, A. Deoxyxylulose phosphate pathway to terpenoids. Trends Plant Sci. 2001, 6, 78–84. [Google Scholar] [CrossRef]
- Hartmann, T. From waste products to ecochemicals: Fifty years research of plant secondary metabolism. Phytochemistry 2007, 68, 2831–2846. [Google Scholar] [CrossRef] [PubMed]
- Vilas, V.; Philip, D.; Mathew, J. Essential oil mediated synthesis of silver nanocrystals for environmental, anti-microbial and antioxidant applications. Mater. Sci. Eng. C. Mater. Biol. Appl. 2016, 61, 429–436. [Google Scholar] [CrossRef]
- Guimarães, A.C.; Meireles, L.M.; Lemos, M.F.; Guimarães, M.C.C.; Endringer, D.C.; Fronza, M.; Scherer, R. Antibacterial Activity of Terpenes and Terpenoids Present in Essential Oils. Molecules 2019, 24, 2471. [Google Scholar] [CrossRef]
- Ribeiro, M.; Malheiro, J.; Grenho, L.; Fernandes, M.H.; Simões, M. Cytotoxicity and antimicrobial action of selected phytochemicals against planktonic and sessile Streptococcus mutans. PeerJ 2018, 6, e4872. [Google Scholar] [CrossRef]
- Zore, G.B.; Thakre, A.D.; Jadhav, S.; Karuppayil, S.M. Terpenoids inhibit Candida albicans growth by affecting membrane integrity and arrest of cell cycle. Phytomedicine 2011, 18, 1181–1190. [Google Scholar] [CrossRef]
- Usmani, Y.; Ahmed, A.; Faizi, S.; Versiani, M.A.; Shamshad, S.; Khan, S.; Simjee, S.U. Antimicrobial and biofilm inhibiting potential of an amide derivative [N-(2′, 4′-dinitrophenyl)-3β-hydroxyurs-12-en-28-carbonamide] of ursolic acid by modulating membrane potential and quorum sensing against colistin resistant Acinetobacter baumannii. Microb. Pathog. 2021, 157, 104997. [Google Scholar] [CrossRef]
- Jäger, S.; Trojan, H.; Kopp, T.; Laszczyk, M.N.; Scheffler, A. Pentacyclic triterpene distribution in various plants-rich sources for a new group of multi-potent plant extracts. Molecules 2009, 14, 2016–2031. [Google Scholar] [CrossRef]
- Szakiel, A.; Pączkowski, C.; Pensec, F.; Bertsch, C. Fruit cuticular waxes as a source of biologically active triterpenoids. Phytochem. Rev. 2012, 11, 263–284. [Google Scholar] [CrossRef]
- Woźniak, Ł.; Skąpska, S.; Marszałek, K. Ursolic Acid--A Pentacyclic Triterpenoid with a Wide Spectrum of Pharmacological Activities. Molecules 2015, 20, 20614–20641. [Google Scholar] [CrossRef] [PubMed]
- Qian, W.; Wang, W.; Zhang, J.; Wang, T.; Liu, M.; Yang, M.; Sun, Z.; Li, X.; Li, Y. Antimicrobial and antibiofilm activities of ursolic acid against carbapenem-resistant Klebsiella pneumoniae. J. Antibiot. 2020, 73, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Lyu, X.; Wang, L.; Shui, Y.; Jiang, Q.; Chen, L.; Yang, W.; He, X.; Zeng, J.; Li, Y. Ursolic acid inhibits multi-species biofilms developed by Streptococcus mutans, Streptococcus sanguinis, and Streptococcus gordonii. Arch. Oral Biol. 2021, 125, 105107. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-M.; Jhan, Y.-L.; Tsai, S.-J.; Chou, C.-H. The Pleiotropic Antibacterial Mechanisms of Ursolic Acid against Methicillin-Resistant Staphylococcus aureus (MRSA). Molecules 2016, 21, 884. [Google Scholar] [CrossRef]
- Kim, S.G.; Kim, M.J.; Jin, D.; Park, S.N.; Cho, E.; Freire, M.O.; Jang, S.J.; Park, Y.J.; Kook, J.K. Antimicrobial effect of ursolic acid and oleanolic acid against methicillin-resistant staphylococcus aureus. Korean J. Microbiol. 2012, 48, 212–215. [Google Scholar] [CrossRef][Green Version]
- Horiuchi, K.; Shiota, S.; Hatano, T.; Yoshida, T.; Kuroda, T.; Tsuchiya, T. Antimicrobial activity of oleanolic acid from Salvia officinalis and related compounds on vancomycin-resistant enterococci (VRE). Biol. Pharm. Bull. 2007, 30, 1147–1149. [Google Scholar] [CrossRef]
- Siddique, H.R.; Saleem, M. Beneficial health effects of lupeol triterpene: A review of preclinical studies. Life Sci. 2011, 88, 285–293. [Google Scholar] [CrossRef]
- Sharma, P.; Tyagi, A.; Bhansali, P.; Pareek, S.; Singh, V.; Ilyas, A.; Mishra, R.; Poddar, N.K. Saponins: Extraction, bio-medicinal properties and way forward to anti-viral representatives. Food Chem. Toxicol. 2021, 150, 112075. [Google Scholar] [CrossRef]
- Kim, J.; Joo, I.; Kim, H.; Han, Y. 18β-glycyrrhetinic acid induces immunological adjuvant activity of Th1 against Candida albicans surface mannan extract. Phytomedicine 2013, 20, 951–955. [Google Scholar] [CrossRef]
- Dong, S.; Yang, X.; Zhao, L.; Zhang, F.; Hou, Z.; Xue, P. Antibacterial activity and mechanism of action saponins from Chenopodium quinoa Willd. husks against foodborne pathogenic bacteria. Ind. Crops Prod. 2020, 149, 112350. [Google Scholar] [CrossRef]
- Zhou, T.; Deng, X.; Qiu, J. Antimicrobial activity of licochalcone E against Staphylococcus aureus and its impact on the production of staphylococcal alpha-toxin. J. Microbiol. Biotechnol. 2012, 22, 800–805. [Google Scholar] [CrossRef]
- Dai, X.-H.; Li, H.-E.; Lu, C.-J.; Wang, J.-F.; Dong, J.; Wei, J.-Y.; Zhang, Y.; Wang, X.; Tan, W.; Deng, X.-M.; et al. Liquiritigenin prevents Staphylococcus aureus-mediated lung cell injury via inhibiting the production of α-hemolysin. J. Asian Nat. Prod. Res. 2013, 15, 390–399. [Google Scholar] [CrossRef]
- Messier, C.; Grenier, D. Effect of licorice compounds licochalcone A, glabridin and glycyrrhizic acid on growth and virulence properties of Candida albicans. Mycoses 2011, 54, e801-6. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Yu, H.; Guo, Y.; Cheng, Y.; Xie, Y.; Yao, W. Antibacterial activity of Sapindus saponins against microorganisms related to food hygiene and the synergistic action mode of Sapindoside A and B against Micrococcus luteus in vitro. Food Control 2021, 130, 108337. [Google Scholar] [CrossRef]
- Wei, M.-P.; Qiu, J.-D.; Li, L.; Xie, Y.-F.; Yu, H.; Guo, Y.-H.; Yao, W.-R. Saponin fraction from Sapindus mukorossi Gaertn as a novel cosmetic additive: Extraction, biological evaluation, analysis of anti-acne mechanism and toxicity prediction. J. Ethnopharmacol. 2021, 268, 113552. [Google Scholar] [CrossRef] [PubMed]
- Anju, V.T.; Busi, S.; Ranganathan, S.; Ampasala, D.R.; Kumar, S.; Suchiang, K.; Kumavath, R.; Dyavaiah, M. Sesamin and sesamolin rescues Caenorhabditis elegans from Pseudomonas aeruginosa infection through the attenuation of quorum sensing regulated virulence factors. Microb. Pathog. 2021, 155, 104912. [Google Scholar] [CrossRef]
- Farag, M.A.; Ali, S.E.; Hodaya, R.H.; El-Seedi, H.R.; Sultani, H.N.; Laub, A.; Eissa, T.F.; Abou-Zaid, F.O.F.; Wessjohann, L.A. Phytochemical Profiles and Antimicrobial Activities of Allium cepa Red cv. and A. sativum Subjected to Different Drying Methods: A Comparative MS-Based Metabolomics. Molecules 2017, 22, 761. [Google Scholar] [CrossRef]
- Persson, T.; Hansen, T.H.; Rasmussen, T.B.; Skindersø, M.E.; Givskov, M.; Nielsen, J. Rational design and synthesis of new quorum-sensing inhibitors derived from acylated homoserine lactones and natural products from garlic. Org. Biomol. Chem. 2005, 3, 253–262. [Google Scholar] [CrossRef]
- Birring, O.J.S.; Viloria, I.L.; Nunez, P. Anti-microbial efficacy of Allium sativum extract against Enterococcus faecalis biofilm and its penetration into the root dentin: An in vitro study. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2015, 26, 477–482. [Google Scholar] [CrossRef]
- Bayan, L.; Koulivand, P.H.; Gorji, A. Garlic: A review of potential therapeutic effects. Avicenna J. phytomedicine 2014, 4, 1–14. [Google Scholar]
- Vadekeetil, A.; Kaur, G.; Chhibber, S.; Harjai, K. Applications of thin-layer chromatography in extraction and characterisation of ajoene from garlic bulbs. Nat. Prod. Res. 2015, 29, 768–771. [Google Scholar] [CrossRef]
- Dutta, S.; Bhattacharyya, D. Enzymatic, antimicrobial and toxicity studies of the aqueous extract of Ananas comosus (pineapple) crown leaf. J. Ethnopharmacol. 2013, 150, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Zorga, J.; Kunicka-Styczyńska, A.; Gruska, R.; Śmigielski, K. Ultrasound-Assisted Hydrodistillation of Essential Oil from Celery Seeds (Apium graveolens L.) and Its Biological and Aroma Profiles. Molecules 2020, 25, 5322. [Google Scholar] [CrossRef] [PubMed]
- Petrović, S.; Drobac, M.; Ušjak, L.; Filipović, V.; Milenković, M.; Niketić, M. Volatiles of roots of wild-growing and cultivated Armoracia macrocarpa and their antimicrobial activity, in comparison to horseradish, A. rusticana. Ind. Crops Prod. 2017, 109, 398–403. [Google Scholar] [CrossRef]
- Park, H.-W.; Choi, K.-D.; Shin, I.-S. Antimicrobial activity of isothiocyanates (ITCs) extracted from horseradish (Armoracia rusticana) root against oral microorganisms. Biocontrol Sci. 2013, 18, 163–168. [Google Scholar] [CrossRef]
- Jakobsen, T.H.; Bragason, S.K.; Phipps, R.K.; Christensen, L.D.; van Gennip, M.; Alhede, M.; Skindersoe, M.; Larsen, T.O.; Høiby, N.; Bjarnsholt, T.; et al. Food as a source for quorum sensing inhibitors: Iberin from horseradish revealed as a quorum sensing inhibitor of Pseudomonas aeruginosa. Appl. Environ. Microbiol. 2012, 78, 2410–2421. [Google Scholar] [CrossRef]
- Dekić, M.S.; Radulović, N.S.; Stojanović, N.M.; Randjelović, P.J.; Stojanović-Radić, Z.Z.; Najman, S.; Stojanović, S. Spasmolytic, antimicrobial and cytotoxic activities of 5-phenylpentyl isothiocyanate, a new glucosinolate autolysis product from horseradish (Armoracia rusticana P. Gaertn., B. Mey. & Scherb., Brassicaceae). Food Chem. 2017, 232, 329–339. [Google Scholar] [CrossRef]
- Staszowska-Karkut, M.; Materska, M. Phenolic Composition, Mineral Content, and Beneficial Bioactivities of Leaf Extracts from Black Currant (Ribes nigrum L.), Raspberry (Rubus idaeus), and Aronia (Aronia melanocarpa). Nutrients 2020, 12, 463. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Lin, J.-H.; Chou, S.-C.; Chang, S.-J.; Chung, C.-C.; Chen, Y.-S.; Chang, C.-H. Berberine-loaded targeted nanoparticles as specific Helicobacter pylori eradication therapy: In vitro and in vivo study. Nanomedicine 2015, 10, 57–71. [Google Scholar] [CrossRef]
- Guan, Y.; Chye, M.-L. A Brassica juncea chitinase with two-chitin binding domains show anti-microbial properties against phytopathogens and Gram-negative bacteria. Plant Signal. Behav. 2008, 3, 1103–1105. [Google Scholar] [CrossRef][Green Version]
- Sharma, A.; Gupta, S.; Sarethy, I.P.; Dang, S.; Gabrani, R. Green tea extract: Possible mechanism and antibacterial activity on skin pathogens. Food Chem. 2012, 135, 672–675. [Google Scholar] [CrossRef]
- Cichewicz, R.H.; Thorpe, P.A. The antimicrobial properties of chile peppers (Capsicum species) and their uses in Mayan medicine. J. Ethnopharmacol. 1996, 52, 61–70. [Google Scholar] [CrossRef]
- Vasavi, H.S.; Arun, A.B.; Rekha, P.D. Anti-quorum sensing activity of Psidium guajava L. flavonoids against Chromobacterium violaceum and Pseudomonas aeruginosa PAO1. Microbiol. Immunol. 2014, 58, 286–293. [Google Scholar] [CrossRef]
- Sarumathi, A.; Anbu, S.; Saravanan, N. Antibacterial activity of Centella asiatica (Linn.,) leaves. Int. J. Chem. Pharm. Sci. 2013, 1, 393–395. [Google Scholar]
- Papetti, A.; Mascherpa, D.; Carazzone, C.; Stauder, M.; Spratt, D.A.; Wilson, M.; Pratten, J.; Ciric, L.; Lingström, P.; Zaura, E.; et al. Identification of organic acids in Cichorium intybus inhibiting virulence-related properties of oral pathogenic bacteria. Food Chem. 2013, 138, 1706–1712. [Google Scholar] [CrossRef]
- Alva, P.P.; Suresh, S.; MP, G.; Premanath, R. Evaluation of anti-quorum sensing activity of indigenous dietary plants against Pseudomonas aeruginosa. Eur. J. Integr. Med. 2019, 30, 100931. [Google Scholar] [CrossRef]
- Gao, Z.; Zhong, W.; Chen, K.; Tang, P.; Guo, J. Chemical composition and anti-biofilm activity of essential oil from Citrus medica L. var. sarcodactylis Swingle against Listeria monocytogenes. Ind. Crops Prod. 2020, 144, 112036. [Google Scholar] [CrossRef]
- Sultana, H.S.; Ali, M.; Panda, B.P. Influence of volatile constituents of fruit peels of Citrus reticulata Blanco on clinically isolated pathogenic microorganisms under In–vitro. Asian Pac. J. Trop. Biomed. 2012, 2, S1299–S1302. [Google Scholar] [CrossRef]
- Oikeh, E.I.; Oviasogie, F.E.; Omoregie, E.S. Quantitative phytochemical analysis and antimicrobial activities of fresh and dry ethanol extracts of Citrus sinensis (L.) Osbeck (sweet Orange) peels. Clin. Phytoscience 2020, 6, 46. [Google Scholar] [CrossRef]
- Duangjai, A.; Suphrom, N.; Wungrath, J.; Ontawong, A.; Nuengchamnong, N.; Yosboonruang, A. Comparison of antioxidant, antimicrobial activities and chemical profiles of three coffee (Coffea arabica L.) pulp aqueous extracts. Integr. Med. Res. 2016, 5, 324–331. [Google Scholar] [CrossRef]
- Delaquis, P.J.; Stanich, K.; Girard, B.; Mazza, G. Antimicrobial activity of individual and mixed fractions of dill, cilantro, coriander and eucalyptus essential oils. Int. J. Food Microbiol. 2002, 74, 101–109. [Google Scholar] [CrossRef]
- Rolnik, A.; Olas, B. Vegetables from the Cucurbitaceae family and their products: Positive effect on human health. Nutrition 2020, 78, 110788. [Google Scholar] [CrossRef]
- Amin, M.Z.; IslamRity, T.; RaselUddin, M.; Rahman, M.M.; Uddin, M.J. A comparative assessment of anti-inflammatory, anti-oxidant and anti-bacterial activities of hybrid and indigenous varieties of pumpkin (Cucurbita maxima Linn.) seed oil. Biocatal. Agric. Biotechnol. 2020, 28, 101767. [Google Scholar] [CrossRef]
- Morita, A.; Tai, A.; Ito, H.; Ganeko, N.; Aizawa, S.-I. Proanthocyanidins in an astringent persimmon inhibit Salmonella pathogenicity island 1 (SPI1) secretion. J. Sci. Food Agric. 2016, 96, 1798–1802. [Google Scholar] [CrossRef]
- Liu, F.; Liu, C.; Liu, W.; Ding, Z.; Ma, H.; Seeram, N.P.; Xu, L.; Mu, Y.; Huang, X.; Li, L. New Sesquiterpenoids from Eugenia jambolana Seeds and Their Anti-microbial Activities. J. Agric. Food Chem. 2017, 65, 10214–10222. [Google Scholar] [CrossRef]
- Di Vito, M.; Gentile, M.; Mattarelli, P.; Barbanti, L.; Micheli, L.; Mazzuca, C.; Garzoli, S.; Titubante, M.; Vitali, A.; Cacaci, M.; et al. Phytocomplex Influences Antimicrobial and Health Properties of Concentrated Glycerine Macerates. Antibiotics 2020, 9, 858. [Google Scholar] [CrossRef]
- Da-Costa-Rocha, I.; Bonnlaender, B.; Sievers, H.; Pischel, I.; Heinrich, M. Hibiscus sabdariffa L.–A phytochemical and pharmacological review. Food Chem. 2014, 165, 424–443. [Google Scholar] [CrossRef]
- Otsuka, N.; Liu, M.-H.; Shiota, S.; Ogawa, W.; Kuroda, T.; Hatano, T.; Tsuchiya, T. Anti-methicillin resistant Staphylococcus aureus (MRSA) compounds isolated from Laurus nobilis. Biol. Pharm. Bull. 2008, 31, 1794–1797. [Google Scholar] [CrossRef]
- Liu, M.-H.; Otsuka, N.; Noyori, K.; Shiota, S.; Ogawa, W.; Kuroda, T.; Hatano, T.; Tsuchiya, T. Synergistic effect of kaempferol glycosides purified from Laurus nobilis and fluoroquinolones on methicillin-resistant Staphylococcus aureus. Biol. Pharm. Bull. 2009, 32, 489–492. [Google Scholar] [CrossRef]
- Rafińska, K.; Pomastowski, P.; Rudnicka, J.; Krakowska, A.; Maruśka, A.; Narkute, M.; Buszewski, B. Effect of solvent and extraction technique on composition and biological activity of Lepidium sativum extracts. Food Chem. 2019, 289, 16–25. [Google Scholar] [CrossRef]
- Gao, M.; Teplitski, M.; Robinson, J.B.; Bauer, W.D. Production of substances by Medicago truncatula that affect bacterial quorum sensing. Mol. Plant. Microbe. Interact. 2003, 16, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Keshavan, N.D.; Chowdhary, P.K.; Haines, D.C.; González, J.E. L-Canavanine made by Medicago sativa interferes with quorum sensing in Sinorhizobium meliloti. J. Bacteriol. 2005, 187, 8427–8436. [Google Scholar] [CrossRef] [PubMed]
- Lucena Filho, J.H.; Medeiros, A.C.; Pereira, J.V.; Granville-Garcia, A.F.; Costa, E.M. Antimicrobial Potential of Momordica charantia L. against Multiresistant Standard Species and Clinical Isolates. J. Contemp. Dent. Pract. 2015, 16, 854–858. [Google Scholar] [CrossRef] [PubMed]
- Jabeen, U.; Khanum, A. Isolation and characterization of potential food preservative peptide from Momordica charantia L. Arab. J. Chem. 2017, 10, S3982–S3989. [Google Scholar] [CrossRef]
- Paikra, B.K.; Dhongade, H.K.J.; Gidwani, B. Phytochemistry and Pharmacology of Moringa oleifera Lam. J. pharmacopuncture 2017, 20, 194–200. [Google Scholar] [CrossRef]
- Ningappa, M.B.; Dhananjaya, B.L.; Dinesha, R.; Harsha, R.; Srinivas, L. Potent antibacterial property of APC protein from curry leaves (Murraya koenigii L.). Food Chem. 2010, 118, 747–750. [Google Scholar] [CrossRef]
- Avetisyan, A.; Markosian, A.; Petrosyan, M.; Sahakyan, N.; Babayan, A.; Aloyan, S.; Trchounian, A. Chemical composition and some biological activities of the essential oils from basil Ocimum different cultivars. BMC Complement. Altern. Med. 2017, 17, 60. [Google Scholar] [CrossRef]
- Peng, M.; Zhao, X.; Biswas, D. Polyphenols and tri-terpenoids from Olea europaea L. in alleviation of enteric pathogen infections through limiting bacterial virulence and attenuating inflammation. J. Funct. Foods 2017, 36, 132–143. [Google Scholar] [CrossRef]
- Alvarez, M.V.; Ortega-Ramirez, L.A.; Gutierrez-Pacheco, M.M.; Bernal-Mercado, A.T.; Rodriguez-Garcia, I.; Gonzalez-Aguilar, G.A.; Ponce, A.; Moreira, M.D.R.; Roura, S.I.; Ayala-Zavala, J.F. Oregano essential oil-pectin edible films as anti-quorum sensing and food antimicrobial agents. Front. Microbiol. 2014, 5, 699. [Google Scholar] [CrossRef]
- Bharti, V.; Vasudeva, N.; Kumar, S. Anti-oxidant studies and anti-microbial effect of Origanum vulgare Linn in combination with standard antibiotics. Ayu 2014, 35, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.N.; Alves, F.C.B.; Andrade, B.F.M.T.; Albano, M.; Rall, V.L.M.; Fernandes, A.A.H.; Buzalaf, M.A.R.; de Lima Leite, A.; de Pontes, L.G.; Dos Santos, L.D.; et al. Proteomic analysis and antibacterial resistance mechanisms of Salmonella Enteritidis submitted to the inhibitory effect of Origanum vulgare essential oil, thymol and carvacrol. J. Proteomics 2020, 214, 103625. [Google Scholar] [CrossRef]
- Kenari, H.M.; Kordafshari, G.; Moghimi, M.; Eghbalian, F.; TaherKhani, D. Review of Pharmacological Properties and Chemical Constituents of Pastinaca sativa. J. Pharmacopunct. 2021, 24, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Linde, G.A.; Gazim, Z.C.; Cardoso, B.K.; Jorge, L.F.; Tešević, V.; Glamoćlija, J.; Soković, M.; Colauto, N.B. Antifungal and antibacterial activities of Petroselinum crispum essential oil. Genet. Mol. Res. 2016, 15. [Google Scholar] [CrossRef]
- Zaki, A.A.; Shaaban, M.I.; Hashish, N.E.; Amer, M.A.; Lahloub, M.-F. Assessment of anti-quorum sensing activity for some ornamental and medicinal plants native to egypt. Sci. Pharm. 2013, 81, 251–258. [Google Scholar] [CrossRef]
- Rajaei, A.; Barzegar, M.; Mobarez, A.M.; Sahari, M.A.; Esfahani, Z.H. Antioxidant, anti-microbial and antimutagenicity activities of pistachio (Pistachia vera) green hull extract. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2010, 48, 107–112. [Google Scholar] [CrossRef]
- Hu, S.; Chai, W.C.; Xu, L.; Li, S.; Jin, C.; Zhu, R.; Yang, L.; Zhang, R.; Tang, K.; Li, P.; et al. Catecholic alkaloid sulfonates and aromatic nitro compounds from Portulaca oleracea and screening of their anti-inflammatory and anti-microbial activities. Phytochemistry 2021, 181, 112587. [Google Scholar] [CrossRef]
- Afonso, S.; Oliveira, I.V.; Meyer, A.S.; Aires, A.; Saavedra, M.J.; Gonçalves, B. Phenolic Profile and Bioactive Potential of Stems and Seed Kernels of Sweet Cherry Fruit. Antioxidants 2020, 9, 1295. [Google Scholar] [CrossRef]
- Mitani, T.; Ota, K.; Inaba, N.; Kishida, K.; Koyama, H.A. Antimicrobial Activity of the Phenolic Compounds of Prunus mume against Enterobacteria. Biol. Pharm. Bull. 2018, 41, 208–212. [Google Scholar] [CrossRef]
- Li, X.; Zhang, J.; Gao, W.; Wang, H. Study on chemical composition, anti-inflammatory and anti-microbial activities of extracts from Chinese pear fruit (Pyrus bretschneideri Rehd.). Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2012, 50, 3673–3679. [Google Scholar] [CrossRef]
- Iyda, J.H.; Fernandes, Â.; Ferreira, F.D.; Alves, M.J.; Pires, T.C.S.P.; Barros, L.; Amaral, J.S.; Ferreira, I.C.F.R. Chemical composition and bioactive properties of the wild edible plant Raphanus raphanistrum L. Food Res. Int. 2019, 121, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Han, S.-W.; Kim, J. Sulforaphene identified from radish (Raphanus sativus L.) seeds possesses antimicrobial properties against multidrug-resistant bacteria and methicillin-resistant Staphylococcus aureus. J. Funct. Foods 2016, 24, 131–141. [Google Scholar] [CrossRef]
- Kuo, I.-P.; Lee, P.-T.; Nan, F.-H. Rheum officinale extract promotes the innate immunity of orange-spotted grouper (Epinephelus coioides) and exerts strong bactericidal activity against six aquatic pathogens. Fish Shellfish Immunol. 2020, 102, 117–124. [Google Scholar] [CrossRef]
- Cendrowski, A.; Kraśniewska, K.; Przybył, J.L.; Zielińska, A.; Kalisz, S. Antibacterial and Antioxidant Activity of Extracts from Rose Fruits (Rosa rugosa). Molecules 2020, 25, 1365. [Google Scholar] [CrossRef]
- Akroum, S. [Anti-microbial activity of Rosmarinus officinalis and Zingiber officinale extracts on the species of the genus Candida and on Streptococcus pneumonia]. Ann. Pharm. Fr. 2021, 79, 62–69. [Google Scholar] [CrossRef]
- Wei, Q.; Bhasme, P.; Wang, Z.; Wang, L.; Wang, S.; Zeng, Y.; Wang, Y.; Ma, L.Z.; Li, Y. Chinese medicinal herb extract inhibits PQS-mediated quorum sensing system in Pseudomonas aeruginosa. J. Ethnopharmacol. 2020, 248, 112272. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, Y.; Guo, L.; Jiang, H.; Ji, Q. In Vitro Evaluation of Antioxidant and Antimicrobial Activities of Melaleuca alternifolia Essential Oil. Biomed Res. Int. 2018, 2018, 2396109. [Google Scholar] [CrossRef]
- de Carvalho Bernardo, W.L.; Boriollo, M.F.G.; Tonon, C.C.; da Silva, J.J.; Cruz, F.M.; Martins, A.L.; Höfling, J.F.; Spolidorio, D.M.P. Antimicrobial effects of silver nanoparticles and extracts of Syzygium cumini flowers and seeds: Periodontal, cariogenic and opportunistic pathogens. Arch. Oral Biol. 2021, 125, 105101. [Google Scholar] [CrossRef]
- Gopu, V.; Kothandapani, S.; Shetty, P.H. Quorum quenching activity of Syzygium cumini (L.) Skeels and its anthocyanin malvidin against Klebsiella pneumoniae. Microb. Pathog. 2015, 79, 61–69. [Google Scholar] [CrossRef]
- Sirdaarta, J.; Matthews, B.; Cock, I.E. Kakadu plum fruit extracts inhibit growth of the bacterial triggers of rheumatoid arthritis: Identification of stilbene and tannin components. J. Funct. Foods 2015, 17, 610–620. [Google Scholar] [CrossRef]
- Borugă, O.; Jianu, C.; Mişcă, C.; Goleţ, I.; Gruia, A.T.; Horhat, F.G. Thymus vulgaris essential oil: Chemical composition and antimicrobial activity. J. Med. Life 2014, 7, 56–60. [Google Scholar]
- Choo, J.H.; Rukayadi, Y.; Hwang, J.-K. Inhibition of bacterial quorum sensing by vanilla extract. Lett. Appl. Microbiol. 2006, 42, 637–641. [Google Scholar] [CrossRef]
- Uchida, K.; Miura, Y.; Nagai, M.; Tominaga, M. Isothiocyanates from Wasabia japonica activate transient receptor potential ankyrin 1 channel. Chem. Senses 2012, 37, 809–818. [Google Scholar] [CrossRef]
- Kumar, L.; Chhibber, S.; Harjai, K. Structural alterations in Pseudomonas aeruginosa by zingerone contribute to enhanced susceptibility to antibiotics, serum and phagocytes. Life Sci. 2014, 117, 24–32. [Google Scholar] [CrossRef]
- Macdonald, I.J.; Dougherty, T.J. Basic principles of photodynamic therapy. J. Porphyr. Phthalocyanines 2001, 5, 105–129. [Google Scholar] [CrossRef]
- Huang, L.; Xuan, Y.; Koide, Y.; Zhiyentayev, T.; Tanaka, M.; Hamblin, M.R. Type I and Type II mechanisms of antimicrobial photodynamic therapy: An in vitro study on gram-negative and gram-positive bacteria. Lasers Surg. Med. 2012, 44, 490–499. [Google Scholar] [CrossRef]
- Alves, E.; Faustino, M.A.; Neves, M.G.; Cunha, A.; Tome, J.; Almeida, A. An insight on bacterial cellular targets of photodynamic inactivation. Future Med. Chem. 2014, 6, 141–164. [Google Scholar] [CrossRef]
- Liu, Y.; Qin, R.; Zaat, S.A.J.; Breukink, E.; Heger, M. Antibacterial photodynamic therapy: Overview of a promising approach to fight antibiotic-resistant bacterial infections. J. Clin. Transl. Res. 2015, 1, 140–167. [Google Scholar] [PubMed]
- Hamblin, M.R.; Abrahamse, H. Oxygen-Independent Antimicrobial Photoinactivation: Type III Photochemical Mechanism? Antibiotics 2020, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Daniell, M.D.; Hill, J.S. A history of photodynamic therapy. Aust. N. Z. J. Surg. 1991, 61, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Moan, J.; Peng, Q. An outline of the hundred-year history of PDT. Anticancer Res. 2003, 23, 3591–3600. [Google Scholar] [PubMed]
- Ackroyd, R.; Kelty, C.; Brown, N.; Reed, M. The history of photodetection and photodynamic therapy. Photochem. Photobiol. 2001, 74, 656–669. [Google Scholar] [CrossRef]
- Hamblin, M.R. Potentiation of antimicrobial photodynamic inactivation by inorganic salts. Expert Rev. Anti. Infect. Ther. 2017, 15, 1059–1069. [Google Scholar] [CrossRef]
- Cieplik, F.; Deng, D.; Crielaard, W.; Buchalla, W.; Hellwig, E.; Al-Ahmad, A.; Maisch, T. Antimicrobial photodynamic therapy-what we know and what we don’t. Crit. Rev. Microbiol. 2018, 44, 571–589. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Antimicrobial photodynamic inactivation: A bright new technique to kill resistant microbes. Curr. Opin. Microbiol. 2016, 33, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Nisnevitch, M.; Nakonechny, F.; Nitzan, Y. Photodynamic antimicrobial chemotherapy by liposome-encapsulated water-soluble photosensitizers. Russ. J. Bioorganic Chem. 2010, 36, 363–369. [Google Scholar] [CrossRef]
- Ilizirov, Y.; Formanovsky, A.; Mikhura, I.; Paitan, Y.; Nakonechny, F.; Nisnevitch, M. Effect of photodynamic antibacterial chemotherapy combined with antibiotics on Gram-positive and gram-negative bacteria. Molecules 2018, 23, 3152. [Google Scholar] [CrossRef]
- Wainwright, M.; Maisch, T.; Nonell, S.; Plaetzer, K.; Almeida, A.; Tegos, G.P.; Hamblin, M.R. Photoantimicrobials-are we afraid of the light? Lancet. Infect. Dis. 2017, 17, e49–e55. [Google Scholar] [CrossRef]
- Ghorbani, J.; Rahban, D.; Aghamiri, S.; Teymouri, A.; Bahador, A. Photosensitizers in antibacterial photodynamic therapy: An overview. Laser Ther. 2018, 27, 293–302. [Google Scholar] [CrossRef]
- Siewert, B.; Stuppner, H. The photoactivity of natural products–An overlooked potential of phytomedicines? Phytomedicine 2019, 60, 152985. [Google Scholar] [CrossRef]
- Jha, A.; Mohapatra, P.P.; AlHarbi, S.A.; Jahan, N. Curcumin: Not So Spicy After All. Mini Rev. Med. Chem. 2017, 17, 1425–1434. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Wu, J.; Pang, X.; Jiang, Y.; Wang, P.; Leung, A.W.; Gao, L.; Jiang, S.; Xu, C. Discovery and Development of Natural Products and their Derivatives as Photosensitizers for Photodynamic Therapy. Curr. Med. Chem. 2018, 25, 839–860. [Google Scholar] [CrossRef]
- Kotha, R.R.; Luthria, D.L. Curcumin: Biological, Pharmaceutical, Nutraceutical, and Analytical Aspects. Molecules 2019, 24, 2930. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, P.; Singh, M.; Kumari, H.; Kumari, A.; Mukhopadhyay, K. Bactericidal activity of curcumin I is associated with damaging of bacterial membrane. PLoS ONE 2015, 10, e0121313. [Google Scholar] [CrossRef] [PubMed]
- Dias, L.D.; Blanco, K.C.; Mfouo-Tynga, I.S.; Inada, N.M.; Bagnato, V.S. Curcumin as a photosensitizer: From molecular structure to recent advances in antimicrobial photodynamic therapy. J. Photochem. Photobiol. C Photochem. Rev. 2020, 45, 100384. [Google Scholar] [CrossRef]
- Trigo Gutierrez, J.K.; Zanatta, G.C.; Ortega, A.L.M.; Balastegui, M.I.C.; Sanitá, P.V.; Pavarina, A.C.; Barbugli, P.A.; de Oliveira Mima, E.G. Encapsulation of curcumin in polymeric nanoparticles for antimicrobial Photodynamic Therapy. PLoS ONE 2017, 12, e0187418. [Google Scholar] [CrossRef]
- Rocha, M.P.; Santos, M.S.; Rodrigues, P.L.F.; Araújo, T.S.D.; de Oliveira, J.M.; Rosa, L.P.; Bagnato, V.S.; da Silva, F.C. Photodynamic therapry with curcumin in the reduction of enterococcus faecalis biofilm in bone cavity: rMicrobiological and spectral fluorescense analysis. Photodiagnosis Photodyn. Ther. 2021, 33, 102084. [Google Scholar] [CrossRef]
- Santezi, C.; Reina, B.D.; de Annunzio, S.R.; Calixto, G.; Chorilli, M.; Dovigo, L.N. Photodynamic potential of curcumin in bioadhesive formulations: Optical characteristics and antimicrobial effect against biofilms. Photodiagnosis Photodyn. Ther. 2021, 35, 102416. [Google Scholar] [CrossRef] [PubMed]
- Randazzo, W.; Aznar, R.; Sánchez, G. Curcumin-Mediated Photodynamic Inactivation of Norovirus Surrogates. Food Environ. Virol. 2016, 8, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Araújo, B.P.; Silva, E.A.; Rosa, L.P.; Inada, N.M.; Iermak, I.; Romano, R.A.; Mezzacappo, N.F.; Melo, F.F.; Silva, F.C.; Rocha, M.P.; et al. Morpho-molecular mechanisms study of photodynamic therapy and curcumin larvicide action on wild mosquitoes larvae of genus Aedes. bioRxiv 2020, 200295. [Google Scholar] [CrossRef]
- Buchovec, I.; Gricajeva, A.; Kalėdienė, L.; Vitta, P. Antimicrobial Photoinactivation Approach Based on Natural Agents for Control of Bacteria Biofilms in Spacecraft. Int. J. Mol. Sci. 2020, 21, 6932. [Google Scholar] [CrossRef] [PubMed]
- Bhavya, M.L.; Umesh Hebbar, H. Efficacy of blue LED in microbial inactivation: Effect of photosensitization and process parameters. Int. J. Food Microbiol. 2019, 290, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Duval, J.; Pecher, V.; Poujol, M.; Lesellier, E. Research advances for the extraction, analysis and uses of anthraquinones: A review. Ind. Crops Prod. 2016, 94, 812–833. [Google Scholar] [CrossRef]
- Otieno, W.; Liu, C.; Ji, Y. Aloe-Emodin-Mediated Photodynamic Therapy Attenuates Sepsis-Associated Toxins in Selected Gram-Positive Bacteria In Vitro. J. Microbiol. Biotechnol. 2021, 31, 1200–1209. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Qin, M.; Liu, C.; Ma, W.; Zeng, X.; Ji, Y. Antimicrobial photodynamic therapy against multidrug-resistant Acinetobacter baumannii clinical isolates mediated by aloe-emodin: An in vitro study. Photodiagnosis Photodyn. Ther. 2020, 29, 101632. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.; Geng, S.; Wang, X.; Cui, Z.; Ma, W.; Yuan, M.; Liu, C.; Ji, Y. Aloe-emodin-mediated antimicrobial photodynamic therapy against multidrug-resistant Acinetobacter baumannii: An in vivo study. Photodiagnosis Photodyn. Ther. 2021, 34, 102311. [Google Scholar] [CrossRef]
- Yao, J.-Y.; Lin, L.-Y.; Yuan, X.-M.; Ying, W.-L.; Xu, Y.; Pan, X.-Y.; Hao, G.-J.; Shen, J.-Y.; Wu, J.-C.; Ye, T.; et al. Antifungal Activity of Rhein and Aloe-Emodin from Rheum palmatum on Fish Pathogenic Saprolegnia sp. J. World Aquac. Soc. 2017, 48, 137–144. [Google Scholar] [CrossRef]
- Ma, W.; Liu, C.; Li, J.; Hao, M.; Ji, Y.; Zeng, X. The effects of aloe emodin-mediated antimicrobial photodynamic therapy on drug-sensitive and resistant Candida albicans. Photochem. Photobiol. Sci. 2020, 19, 485–494. [Google Scholar] [CrossRef]
- Ma, W.; Zhang, M.; Cui, Z.; Wang, X.; Niu, X.; Zhu, Y.; Yao, Z.; Ye, F.; Geng, S.; Liu, C. Aloe-emodin-mediated antimicrobial photodynamic therapy against dermatophytosis caused by Trichophyton rubrum. Microb. Biotechnol. 2021. [Google Scholar] [CrossRef]
- Mulrooey, C.A.; O’Brien, E.M.; Morgan, B.J.; Kozlowski, M.C. Perylenequinones: Isolation, Synthesis, and Biological Activity. European J. Org. Chem. 2012, 2012, 3887–3904. [Google Scholar] [CrossRef]
- Borghi-Pangoni, F.B.; Junqueira, M.V.; de Souza Ferreira, S.B.; Silva, L.L.; Rabello, B.R.; de Castro, L.V.; Baesso, M.L.; Diniz, A.; Caetano, W.; Bruschi, M.L. Preparation and characterization of bioadhesive system containing hypericin for local photodynamic therapy. Photodiagnosis Photodyn. Ther. 2017, 19, 284–297. [Google Scholar] [CrossRef]
- Bruni, R.; Barreca, D.; Protti, M.; Brighenti, V.; Righetti, L.; Anceschi, L.; Mercolini, L.; Benvenuti, S.; Gattuso, G.; Pellati, F. Botanical Sources, Chemistry, Analysis, and Biological Activity of Furanocoumarins of Pharmaceutical Interest. Molecules 2019, 24, 2163. [Google Scholar] [CrossRef]
- Kitamura, N.; Kohtani, S.; Nakagaki, R. Molecular aspects of furocoumarin reactions: Photophysics, photochemistry, photobiology, and structural analysis. J. Photochem. Photobiol. C Photochem. Rev. 2005, 6, 168–185. [Google Scholar] [CrossRef]
- AYa, P. Mechanisms of photodynamic effects of furocoumarins. J. Photochem. Photobiol. B. 1991, 9, 1–33. [Google Scholar] [CrossRef]
- Towers, G.H.; Graham, E.A.; Spenser, I.D.; Abramowski, Z. Phototoxic furanoquinolines of the Rutaceae. Planta Med. 1981, 41, 136–142. [Google Scholar] [CrossRef]
- An, Y.-W.; Jin, H.-T.; Yuan, B.; Wang, J.-C.; Wang, C.; Liu, H.-Q. Research progress of berberine mediated photodynamic therapy (Review). Oncol. Lett. 2021, 21, 359. [Google Scholar] [CrossRef]
- Lee, M.M.S.; Zheng, L.; Yu, B.; Xu, W.; Kwok, R.T.K.; Lam, J.W.Y.; Xu, F.; Wang, D.; Tang, B.Z. A highly efficient and AIE-active theranostic agent from natural herbs. Mater. Chem. Front. 2019, 3, 1454–1461. [Google Scholar] [CrossRef]
- Xie, Y.-Y.; Zhang, Y.-W.; Liu, X.-Z.; Ma, X.-F.; Qin, X.-T.; Jia, S.-R.; Zhong, C. Aggregation-induced emission-active amino acid/berberine hydrogels with enhanced photodynamic antibacterial and anti-biofilm activity. Chem. Eng. J. 2021, 413, 127542. [Google Scholar] [CrossRef]
- Ma, K.; Zhe, T.; Li, F.; Zhang, Y.; Yu, M.; Li, R.; Wang, L. Sustainable films containing AIE-active berberine-based nanoparticles: A promising antibacterial food packaging. Food Hydrocoll. 2022, 123, 107147. [Google Scholar] [CrossRef]
- Sobotta, L.; Skupin-Mrugalska, P.; Piskorz, J.; Mielcarek, J. Porphyrinoid photosensitizers mediated photodynamic inactivation against bacteria. Eur. J. Med. Chem. 2019, 175, 72–106. [Google Scholar] [CrossRef]
- Leite, A.C.; Ferreira, A.M.; Morais, E.S.; Khan, I.; Freire, M.G.; Coutinho, J.A.P. Cloud Point Extraction of Chlorophylls from Spinach Leaves Using Aqueous Solutions of Nonionic Surfactants. ACS Sustain. Chem. Eng. 2018, 6, 590–599. [Google Scholar] [CrossRef]
- Garcia de Carvalho, G.; Sanchez-Puetate, J.C.; Donatoni, M.C.; Maquera Huacho, P.M.; de Souza Rastelli, A.N.; de Oliveira, K.T.; Palomari Spolidorio, D.M.; Leal Zandim-Barcelos, D. Photodynamic inactivation using a chlorin-based photosensitizer with blue or red-light irradiation against single-species biofilms related to periodontitis. Photodiagnosis Photodyn. Ther. 2020, 31, 101916. [Google Scholar] [CrossRef]
- Edwards, A.M. Structure and general properties of flavins. Methods Mol. Biol. 2014, 1146, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Hiltunen, H.-M.; Illarionov, B.; Hedtke, B.; Fischer, M.; Grimm, B. Arabidopsis RIBA proteins: Two out of three isoforms have lost their bifunctional activity in riboflavin biosynthesis. Int. J. Mol. Sci. 2012, 13, 14086–14105. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Choe, E.; Min, D.B. Kinetics for Singlet Oxygen Formation by Riboflavin Photosensitization and the Reaction between Riboflavin and Singlet Oxygen. J. Food Sci. 2004, 69, C726–C732. [Google Scholar] [CrossRef]
- Cardoso, D.R.; Libardi, S.H.; Skibsted, L.H. Riboflavin as a photosensitizer. Effects on human health and food quality. Food Funct. 2012, 3, 487–502. [Google Scholar] [CrossRef] [PubMed]
- Powers, H.J. Riboflavin (vitamin B-2) and health. Am. J. Clin. Nutr. 2003, 77, 1352–1360. [Google Scholar] [CrossRef]
- Saedisomeolia, A.; Ashoori, M. Riboflavin in Human Health: A Review of Current Evidences. Adv. Food Nutr. Res. 2018, 83, 57–81. [Google Scholar] [CrossRef]
- Suwannasom, N.; Kao, I.; Pruß, A.; Georgieva, R.; Bäumler, H. Riboflavin: The Health Benefits of a Forgotten Natural Vitamin. Int. J. Mol. Sci. 2020, 21, 950. [Google Scholar] [CrossRef]
- Chang, K.-C.; Cheng, Y.-Y.; Lai, M.-J.; Hu, A. Identification of carbonylated proteins in a bactericidal process induced by curcumin with blue light irradiation on imipenem-resistant Acinetobacter baumannii. Rapid Commun. Mass Spectrom. 2020, 34 (Suppl. 1), e8548. [Google Scholar] [CrossRef]
- Pan, H.; Wang, D.; Zhang, F. In vitro antimicrobial effect of curcumin-based photodynamic therapy on Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. Photodiagnosis Photodyn. Ther. 2020, 32, 102055. [Google Scholar] [CrossRef]
- Najafi, S.; Khayamzadeh, M.; Paknejad, M.; Poursepanj, G.; Kharazi Fard, M.J.; Bahador, A. An In Vitro Comparison of Antimicrobial Effects of Curcumin-Based Photodynamic Therapy and Chlorhexidine, on Aggregatibacter actinomycetemcomitans. J. lasers Med. Sci. 2016, 7, 21–25. [Google Scholar] [CrossRef]
- Condat, M.; Mazeran, P.-E.; Malval, J.-P.; Lalevée, J.; Morlet-Savary, F.; Renard, E.; Langlois, V.; Abbad Andalloussi, S.; Versace, D.-L. Photoinduced curcumin derivative-coatings with antibacterial properties. RSC Adv. 2015, 5, 85214–85224. [Google Scholar] [CrossRef]
- Penha, C.B.; Bonin, E.; da Silva, A.F.; Hioka, N.; Zanqueta, É.B.; Nakamura, T.U.; de Abreu Filho, B.A.; Campanerut-Sá, P.A.Z.; Mikcha, J.M.G. Photodynamic inactivation of foodborne and food spoilage bacteria by curcumin. LWT-Food Sci. Technol. 2017, 76, 198–202. [Google Scholar] [CrossRef]
- de Oliveira, E.F.; Tosati, J.V.; Tikekar, R.V.; Monteiro, A.R.; Nitin, N. Antimicrobial activity of curcumin in combination with light against Escherichia coli O157:H7 and Listeria innocua: Applications for fresh produce sanitation. Postharvest Biol. Technol. 2018, 137, 86–94. [Google Scholar] [CrossRef]
- Tao, R.; Zhang, F.; Tang, Q.-J.; Xu, C.-S.; Ni, Z.-J.; Meng, X.-H. Effects of curcumin-based photodynamic treatment on the storage quality of fresh-cut apples. Food Chem. 2019, 274, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Le, T.D.; Phasupan, P.; Nguyen, L.T. Antimicrobial photodynamic efficacy of selected natural photosensitizers against food pathogens: Impacts and interrelationship of process parameters. Photodiagnosis Photodyn. Ther. 2020, 32, 102024. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Wu, J.; Li, Z.; Zhang, X.; Lu, N.; Xue, C.; Leung, A.W.; Xu, C.; Tang, Q. Curcumin-mediated photodynamic inactivation (PDI) against DH5α contaminated in oysters and cellular toxicological evaluation of PDI-treated oysters. Photodiagnosis Photodyn. Ther. 2019, 26, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Rocha, M.P.; Ruela, A.L.M.; Rosa, L.P.; Santos, G.P.O.; Rosa, F.C.S. Antimicrobial photodynamic therapy in dentistry using an oil-in-water microemulsion with curcumin as a mouthwash. Photodiagnosis Photodyn. Ther. 2020, 32, 101962. [Google Scholar] [CrossRef]
- Pileggi, G.; Wataha, J.C.; Girard, M.; Grad, I.; Schrenzel, J.; Lange, N.; Bouillaguet, S. Blue light-mediated inactivation of Enterococcus faecalis in vitro. Photodiagnosis Photodyn. Ther. 2013, 10, 134–140. [Google Scholar] [CrossRef]
- da Frota, M.F.; Guerreiro-Tanomaru, J.M.; Tanomaru-Filho, M.; Bagnato, V.S.; Espir, C.G.; Berbert, F.L.C.V. Photodynamic therapy in root canals contaminated with Enterococcus faecalis using curcumin as photosensitizer. Lasers Med. Sci. 2015, 30, 1867–1872. [Google Scholar] [CrossRef]
- Neelakantan, P.; Cheng, C.Q.; Ravichandran, V.; Mao, T.; Sriraman, P.; Sridharan, S.; Subbarao, C.; Sharma, S.; Kishen, A. Photoactivation of curcumin and sodium hypochlorite to enhance antibiofilm efficacy in root canal dentin. Photodiagnosis Photodyn. Ther. 2015, 12, 108–114. [Google Scholar] [CrossRef] [PubMed]
- de Annunzio, S.R.; de Freitas, L.M.; Blanco, A.L.; da Costa, M.M.; Carmona-Vargas, C.C.; de Oliveira, K.T.; Fontana, C.R. Susceptibility of Enterococcus faecalis and Propionibacterium acnes to antimicrobial photodynamic therapy. J. Photochem. Photobiol. B Biol. 2018, 178, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Pourhajibagher, M.; Kazemian, H.; Chiniforush, N.; Hosseini, N.; Pourakbari, B.; Azizollahi, A.; Rezaei, F.; Bahador, A. Exploring different photosensitizers to optimize elimination of planktonic and biofilm forms of Enterococcus faecalis from infected root canal during antimicrobial photodynamic therapy. Photodiagnosis Photodyn. Ther. 2018, 24, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Cusicanqui Méndez, D.A.; Cardenas Cuéllar, M.R.; Feliz Pedrinha, V.; Velásquez Espedilla, E.G.; Bombarda de Andrade, F.; de Almeida Rodrigues, P.; Cruvinel, T. Effects of curcumin-mediated antimicrobial photodynamic therapy associated to different chelators against Enterococcus faecalis biofilms. Photodiagnosis Photodyn. Ther. 2021, 35, 102464. [Google Scholar] [CrossRef]
- Ghorbanzadeh, R.; Assadian, H.; Chiniforush, N.; Parker, S.; Pourakbari, B.; Ehsani, B.; Alikhani, M.Y.; Bahador, A. Modulation of virulence in Enterococcus faecalis cells surviving antimicrobial photodynamic inactivation with reduced graphene oxide-curcumin: An ex vivo biofilm model. Photodiagnosis Photodyn. Ther. 2020, 29, 101643. [Google Scholar] [CrossRef]
- Vetvicka, V.; Vetvickova, J.; Fernandez-Botran, R. Effects of curcumin on Helicobacter pylori infection. Ann. Transl. Med. 2016, 4, 479. [Google Scholar] [CrossRef]
- Bonifácio, D.; Martins, C.; David, B.; Lemos, C.; Neves, M.G.P.M.S.; Almeida, A.; Pinto, D.C.G.A.; Faustino, M.A.F.; Cunha, Â. Photodynamic inactivation of Listeria innocua biofilms with food-grade photosensitizers: A curcumin-rich extract of Curcuma longa vs commercial curcumin. J. Appl. Microbiol. 2018, 125, 282–294. [Google Scholar] [CrossRef]
- Gao, J.; Matthews, K.R. Effects of the photosensitizer curcumin in inactivating foodborne pathogens on chicken skin. Food Control 2020, 109, 106959. [Google Scholar] [CrossRef]
- Huang, J.; Chen, B.; Li, H.; Zeng, Q.-H.; Wang, J.J.; Liu, H.; Pan, Y.; Zhao, Y. Enhanced antibacterial and antibiofilm functions of the curcumin-mediated photodynamic inactivation against Listeria monocytogenes. Food Control 2020, 108, 106886. [Google Scholar] [CrossRef]
- Yang, M.-Y.; Chang, K.-C.; Chen, L.-Y.; Hu, A. Low-dose blue light irradiation enhances the antimicrobial activities of curcumin against Propionibacterium acnes. J. Photochem. Photobiol. B Biol. 2018, 189, 21–28. [Google Scholar] [CrossRef]
- Gong, C.; Li, Y.; Gao, R.; Xiao, F.; Zhou, X.; Wang, H.; Xu, H.; Wang, R.; Huang, P.; Zhao, Y. Inactivation of specific spoilage organism (Pseudomonas) of sturgeon by curcumin-mediated photodynamic inactivation. Photodiagnosis Photodyn. Ther. 2020, 31, 101827. [Google Scholar] [CrossRef]
- Mirzahosseinipour, M.; Khorsandi, K.; Hosseinzadeh, R.; Ghazaeian, M.; Shahidi, F.K. Antimicrobial photodynamic and wound healing activity of curcumin encapsulated in silica nanoparticles. Photodiagnosis Photodyn. Ther. 2020, 29, 101639. [Google Scholar] [CrossRef]
- Dos Santos, R.F.; Campos, B.S.; Francisco de Assis Filho, M.G.; de Oliveira Moraes, J.; Albuquerque, A.L.I.; da Silva, M.C.D.; Dos Santos, P.V.; de Araujo, M.T. Photodynamic inactivation of S. aureus with a water-soluble curcumin salt and an application to cheese decontamination. Photochem. Photobiol. Sci. Off. J. Eur. Photochem. Assoc. Eur. Soc. Photobiol. 2019, 18, 2707–2716. [Google Scholar] [CrossRef]
- Freitas, M.A.; Pereira, A.H.; Pinto, J.G.; Casas, A.; Ferreira-Strixino, J. Bacterial viability after antimicrobial photodynamic therapy with curcumin on multiresistant Staphylococcus aureus. Future Microbiol. 2019, 14, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Paolillo, F.R.; Rodrigues, P.G.S.; Bagnato, V.S.; Alves, F.; Pires, L.; Corazza, A.V. The effect of combined curcumin-mediated photodynamic therapy and artificial skin on Staphylococcus aureus-infected wounds in rats. Lasers Med. Sci. 2021, 36, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Soares, J.M.; Inada, N.M.; Bagnato, V.S.; Blanco, K.C. Evolution of surviving Streptoccocus pyogenes from pharyngotonsillitis patients submit to multiple cycles of antimicrobial photodynamic therapy. J. Photochem. Photobiol. B Biol. 2020, 210, 111985. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Song, Z.; Zhi, X.; Du, B. Photoinduced Antimicrobial Activity of Curcumin-Containing Coatings: Molecular Interaction, Stability and Potential Application in Food Decontamination. ACS Omega 2020, 5, 31044–31054. [Google Scholar] [CrossRef]
- Ribeiro, A.P.D.; Pavarina, A.C.; Dovigo, L.N.; Brunetti, I.L.; Bagnato, V.S.; Vergani, C.E.; Costa, C.A. de S. Phototoxic effect of curcumin on methicillin-resistant Staphylococcus aureus and L929 fibroblasts. Lasers Med. Sci. 2013, 28, 391–398. [Google Scholar] [CrossRef]
- Jiang, Y.; Leung, A.W.; Hua, H.; Rao, X.; Xu, C. Photodynamic action of LED-activated curcumin against staphylococcus aureus involving intracellular ROS increase and membrane damage. Int. J. Photoenergy 2014, 2014, 9–11. [Google Scholar] [CrossRef]
- Almeida, P.P.; Pereira, Í.S.; Rodrigues, K.B.; Leal, L.S.; Marques, A.S.; Rosa, L.P.; da Silva, F.C.; da Silva, R.A.A. Photodynamic therapy controls of Staphylococcus aureus intradermal infection in mice. Lasers Med. Sci. 2017, 32, 1337–1342. [Google Scholar] [CrossRef] [PubMed]
- Araújo, T.S.D.; Rodrigues, P.L.F.; Santos, M.S.; de Oliveira, J.M.; Rosa, L.P.; Bagnato, V.S.; Blanco, K.C.; da Silva, F.C. Reduced methicillin-resistant Staphylococcus aureus biofilm formation in bone cavities by photodynamic therapy. Photodiagnosis Photodyn. Ther. 2018, 21, 219–223. [Google Scholar] [CrossRef]
- Tonon, C.C.; Paschoal, M.A.; Correia, M.; Spolidório, D.M.P.; Bagnato, V.S.; Giusti, J.S.M.; Santos-Pinto, L. Comparative effects of photodynamic therapy mediated by curcumin on standard and clinical isolate of Streptococcus mutans. J. Contemp. Dent. Pract. 2015, 16, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Paschoal, M.A.; Tonon, C.C.; Spolidório, D.M.P.; Bagnato, V.S.; Giusti, J.S.M.; Santos-Pinto, L. Photodynamic potential of curcumin and blue LED against Streptococcus mutans in a planktonic culture. Photodiagnosis Photodyn. Ther. 2013, 10, 313–319. [Google Scholar] [CrossRef]
- Paschoal, M.A.; Lin, M.; Santos-Pinto, L.; Duarte, S. Photodynamic antimicrobial chemotherapy on Streptococcus mutans using curcumin and toluidine blue activated by a novel LED device. Lasers Med. Sci. 2015, 30, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Paschoal, M.A.; Santos-Pinto, L.; Lin, M.; Duarte, S. Streptococcus mutans photoinactivation by combination of short exposure of a broad-spectrum visible light and low concentrations of photosensitizers. Photomed. Laser Surg. 2014, 32, 175–180. [Google Scholar] [CrossRef]
- Soria-Lozano, P.; Gilaberte, Y.; Paz-Cristobal, M.P.; Pérez-Artiaga, L.; Lampaya-Pérez, V.; Aporta, J.; Pérez-Laguna, V.; García-Luque, I.; Revillo, M.J.; Rezusta, A. In vitro effect photodynamic therapy with differents photosensitizers on cariogenic microorganisms. BMC Microbiol. 2015, 15, 187. [Google Scholar] [CrossRef]
- Manoli, E.; Samara, C. The removal of Polycyclic Aromatic Hydrocarbons in the wastewater treatment process: Experimental calculations and model predictions. Environ. Pollut. 2008, 151, 477–485. [Google Scholar] [CrossRef]
- Araújo, N.C.; Fontana, C.R.; Bagnato, V.S.; Gerbi, M.E.M. Photodynamic antimicrobial therapy of curcumin in biofilms and carious dentine. Lasers Med. Sci. 2014, 29, 629–635. [Google Scholar] [CrossRef]
- Araújo, N.C.; de Menezes, R.F.; Carneiro, V.S.M.; Dos Santos-Neto, A.P.; Fontana, C.R.; Bagnato, V.S.; Harvey, C.M.; Gerbi, M.E.M. Photodynamic Inactivation of Cariogenic Pathogens Using Curcumin as Photosensitizer. Photomed. Laser Surg. 2017, 35, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Kang, S.-M.; Jeong, S.-H.; Chung, K.-H.; Kim, B.-I. Antibacterial photodynamic therapy with curcumin and Curcuma xanthorrhiza extract against Streptococcus mutans. Photodiagnosis Photodyn. Ther. 2017, 20, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Jia, Y.; Li, W.; Zhang, M. Antimicrobial photodynamic inactivation with curcumin against Staphylococcus saprophyticus, in vitro and on fresh dough sheet. LWT 2021, 147, 111567. [Google Scholar] [CrossRef]
- Wu, J.; Mou, H.; Xue, C.; Leung, A.W.; Xu, C.; Tang, Q.-J. Photodynamic effect of curcumin on Vibrio parahaemolyticus. Photodiagnosis Photodyn. Ther. 2016, 15, 34–39. [Google Scholar] [CrossRef]
- Chen, B.; Huang, J.; Li, H.; Zeng, Q.-H.; Wang, J.J.; Liu, H.; Pan, Y.; Zhao, Y. Eradication of planktonic Vibrio parahaemolyticus and its sessile biofilm by curcumin-mediated photodynamic inactivation. Food Control 2020, 113, 107181. [Google Scholar] [CrossRef]
- Bulit, F.; Grad, I.; Manoil, D.; Simon, S.; Wataha, J.C.; Filieri, A.; Feki, A.; Schrenzel, J.; Lange, N.; Bouillaguet, S. Antimicrobial activity and cytotoxicity of 3 photosensitizers activated with blue light. J. Endod. 2014, 40, 427–431. [Google Scholar] [CrossRef]
- Ricci Donato, H.A.; Pratavieira, S.; Grecco, C.; Brugnera-Júnior, A.; Bagnato, V.S.; Kurachi, C. Clinical Comparison of Two Photosensitizers for Oral Cavity Decontamination. Photomed. Laser Surg. 2017, 35, 105–110. [Google Scholar] [CrossRef]
- Cusicanqui Méndez, D.A.; Gutierres, E.; José Dionisio, E.; Afonso Rabelo Buzalaf, M.; Cardoso Oliveira, R.; Andrade Moreira Machado, M.A.; Cruvinel, T. Curcumin-mediated antimicrobial photodynamic therapy reduces the viability and vitality of infected dentin caries microcosms. Photodiagnosis Photodyn. Ther. 2018, 24, 102–108. [Google Scholar] [CrossRef]
- Méndez, D.A.C.; Rizzato, V.L.; Lamarque, G.C.C.; Dionisio, E.J.; Buzalaf, M.A.R.; Rios, D.; Machado, M.A.A.M.; Cruvinel, T. Could a chelant improve the effect of curcumin-mediated photodynamic antimicrobial chemotherapy against dental intact biofilms? Lasers Med. Sci. 2019, 34, 1185–1192. [Google Scholar] [CrossRef]
- Cusicanqui Méndez, D.A.; Gutierrez, E.; Campos Chaves Lamarque, G.; Lopes Rizzato, V.; Afonso Rabelo Buzalaf, M.; Andrade Moreira Machado, M.A.; Cruvinel, T. The effectiveness of curcumin-mediated antimicrobial photodynamic therapy depends on pre-irradiation and biofilm growth times. Photodiagnosis Photodyn. Ther. 2019, 27, 474–480. [Google Scholar] [CrossRef]
- Oda, D.F.; Duarte, M.A.H.; Andrade, F.B.; Moriyama, L.T.; Bagnato, V.S.; de Moraes, I.G. Antimicrobial action of photodynamic therapy in root canals using LED curing light, curcumin and carbopol gel. Int. Endod. J. 2019, 52, 1010–1019. [Google Scholar] [CrossRef]
- Dou, F.; Huang, K.; Nitin, N. Targeted Photodynamic Treatment of Bacterial Biofilms Using Curcumin Encapsulated in Cells and Cell Wall Particles. ACS Appl. Bio Mater. 2021, 4, 514–522. [Google Scholar] [CrossRef]
- Dovigo, L.N.; Pavarina, A.C.; Ribeiro, A.P.D.; Brunetti, I.L.; de S. Costa, C.A.; Jacomassi, D.P.; Bagnato, V.S.; Kurachi, C. Investigation of the photodynamic effects of curcumin against Candida albicans. Photochem. Photobiol. 2011, 87, 895–903. [Google Scholar] [CrossRef]
- Jordão, C.C.; Viana de Sousa, T.; Inêz Klein, M.; Mendonça Dias, L.; Pavarina, A.C.; Carmello, J.C. Antimicrobial photodynamic therapy reduces gene expression of Candida albicans in biofilms. Photodiagnosis Photodyn. Ther. 2020, 31, 101825. [Google Scholar] [CrossRef]
- Chukwujekwu, J.C.; Coombes, P.H.; Mulholland, D.A.; van Staden, J. Emodin, an antibacterial anthraquinone from the roots of Cassia occidentalis. South African J. Bot. 2006, 72, 295–297. [Google Scholar] [CrossRef]
- Azelmat, J.; Larente, J.F.; Grenier, D. The anthraquinone rhein exhibits synergistic antibacterial activity in association with metronidazole or natural compounds and attenuates virulence gene expression in Porphyromonas gingivalis. Arch. Oral Biol. 2015, 60, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Aponiene, K.; Paskeviciute, E.; Reklaitis, I.; Luksiene, Z. Reduction of microbial contamination of fruits and vegetables by hypericin-based photosensitization: Comparison with other emerging antimicrobial treatments. J. Food Eng. 2015, 144, 29–35. [Google Scholar] [CrossRef]
- Yow, C.M.N.; Tang, H.M.; Chu, E.S.M.; Huang, Z. Hypericin-mediated photodynamic antimicrobial effect on clinically isolated pathogens. Photochem. Photobiol. 2012, 88, 626–632. [Google Scholar] [CrossRef] [PubMed]
- de Melo, W. de C.M.A.; Lee, A.N.; Perussi, J.R.; Hamblin, M.R. Electroporation enhances antimicrobial photodynamic therapy mediated by the hydrophobic photosensitizer, hypericin. Photodiagnosis Photodyn. Ther. 2013, 10, 647–650. [Google Scholar] [CrossRef]
- Kashef, N.; Borghei, Y.S.; Djavid, G.E. Photodynamic effect of hypericin on the microorganisms and primary human fibroblasts. Photodiagnosis Photodyn. Ther. 2013, 10, 150–155. [Google Scholar] [CrossRef]
- Barroso, R.A.; Navarro, R.; Tim, C.R.; de Paula Ramos, L.; de Oliveira, L.D.; Araki, Â.T.; Fernandes, K.G.C.; Macedo, D.; Assis, L. Antimicrobial photodynamic therapy against Propionibacterium acnes biofilms using hypericin (Hypericum perforatum) photosensitizer: In vitro study. Lasers Med. Sci. 2021, 36, 1235–1240. [Google Scholar] [CrossRef]
- García, I.; Ballesta, S.; Gilaberte, Y.; Rezusta, A.; Pascual, Á. Antimicrobial photodynamic activity of hypericin against methicillin-susceptible and resistant Staphylococcus aureus biofilms. Future Microbiol. 2015, 10, 347–356. [Google Scholar] [CrossRef]
- Kashef, N.; Karami, S.; Djavid, G.E. Phototoxic effect of hypericin alone and in combination with acetylcysteine on Staphylococcus aureus biofilms. Photodiagnosis Photodyn. Ther. 2015, 12, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Plenagl, N.; Seitz, B.S.; Duse, L.; Pinnapireddy, S.R.; Jedelska, J.; Brüßler, J.; Bakowsky, U. Hypericin inclusion complexes encapsulated in liposomes for antimicrobial photodynamic therapy. Int. J. Pharm. 2019, 570, 118666. [Google Scholar] [CrossRef] [PubMed]
- Rezusta, A.; López-Chicón, P.; Paz-Cristobal, M.P.; Alemany-Ribes, M.; Royo-Díez, D.; Agut, M.; Semino, C.; Nonell, S.; Revillo, M.J.; Aspiroz, C.; et al. In vitro fungicidal photodynamic effect of hypericin on Candida species. Photochem. Photobiol. 2012, 88, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Sytar, O.; Kotta, K.; Valasiadis, D.; Kosyan, A.; Brestic, M.; Koidou, V.; Papadopoulou, E.; Kroustalaki, M.; Emmanouilidou, C.; Pashalidis, A.; et al. The Effects of Photosensitizing Dyes Fagopyrin and Hypericin on Planktonic Growth and Multicellular Life in Budding Yeast. Molecules 2021, 26, 4708. [Google Scholar] [CrossRef] [PubMed]
- Sytar, O.; Švedienė, J.; Ložienė, K.; Paškevičius, A.; Kosyan, A.; Taran, N. Antifungal properties of hypericin, hypericin tetrasulphonic acid and fagopyrin on pathogenic fungi and spoilage yeasts. Pharm. Biol. 2016, 54, 3121–3125. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, S.; Lee, K.; Kim, R.H.; Hwang, K.T. Antibacterial Photodynamic Inactivation of Fagopyrin F from Tartary Buckwheat (Fagopyrum tataricum) Flower against Streptococcus mutans and Its Biofilm. Int. J. Mol. Sci. 2021, 22, 6205. [Google Scholar] [CrossRef]
- Oginsky, E.L.; Green, G.S.; Griffith, D.G.; Fowlks, W.L. Lethal photosensitization of bacteria with 8-methoxypsoralen to long wave length ultraviolet radiation. J. Bacteriol. 1959, 78, 821–833. [Google Scholar] [CrossRef]
- Bianchi, L.; Melli, R.; Pizzala, R.; Stivala, L.A.; Rehak, L.; Quarta, S.; Vannini, V. Effects of beta-carotene and alpha-tocopherol on photogenotoxicity induced by 8-methoxypsoralen: The role of oxygen. Mutat. Res. 1996, 369, 183–194. [Google Scholar] [CrossRef]
- Park, J.-H.; Moon, Y.-H.; Bang, I.-S.; Kim, Y.-C.; Kim, S.-A.; Ahn, S.-G.; Yoon, J.-H. Antimicrobial effect of photodynamic therapy using a highly pure chlorin e6. Lasers Med. Sci. 2010, 25, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.-M.; Lee, H.-S.; Jeong, D.; Oh, H.-K.; Ra, K.-H.; Lee, M.-Y. Antimicrobial photodynamic therapy using chlorin e6 with halogen light for acne bacteria-induced inflammation. Life Sci. 2015, 124, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Ahn, M.-Y.; Kim, Y.-C.; Kim, S.-A.; Moon, Y.-H.; Ahn, S.-G.; Yoon, J.-H. In vitro and in vivo antimicrobial effect of photodynamic therapy using a highly pure chlorin e6 against Staphylococcus aureus Xen29. Biol. Pharm. Bull. 2012, 35, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Nie, M.; Deng, D.M.; Wu, Y.; de Oliveira, K.T.; Bagnato, V.S.; Crielaard, W.; Rastelli, A.N. de S. Photodynamic inactivation mediated by methylene blue or chlorin e6 against Streptococcus mutans biofilm. Photodiagnosis Photodyn. Ther. 2020, 31, 101817. [Google Scholar] [CrossRef] [PubMed]
- Luke-Marshall, N.R.; Hansen, L.A.; Shafirstein, G.; Campagnari, A.A. Antimicrobial Photodynamic Therapy with Chlorin e6 Is Bactericidal against Biofilms of the Primary Human Otopathogens. mSphere 2020, 5, e00492-20. [Google Scholar] [CrossRef]
- Eichner, A.; Gollmer, A.; Späth, A.; Bäumler, W.; Regensburger, J.; König, B.; Maisch, T. Fast and effective inactivation of Bacillus atrophaeus endospores using light-activated derivatives of vitamin B2. Photochem. Photobiol. Sci. Off. J. Eur. Photochem. Assoc. Eur. Soc. Photobiol. 2015, 14, 387–396. [Google Scholar] [CrossRef]
- Khan, S.; Rayis, M.; Rizvi, A.; Alam, M.M.; Rizvi, M.; Naseem, I. ROS mediated antibacterial activity of photoilluminated riboflavin: A photodynamic mechanism against nosocomial infections. Toxicol. Rep. 2019, 6, 136–142. [Google Scholar] [CrossRef]
- Banerjee, S.; Ghosh, D.; Vishakha, K.; Das, S.; Mondal, S.; Ganguli, A. Photodynamic antimicrobial chemotherapy (PACT) using riboflavin inhibits the mono and dual species biofilm produced by antibiotic resistant Staphylococcus aureus and Escherichia coli. Photodiagnosis Photodyn. Ther. 2020, 32, 102002. [Google Scholar] [CrossRef]
- Kim, M.-J.; Da Jeong, M.; Zheng, Q.; Yuk, H.-G. Antimicrobial activity of 405 nm light-emitting diode (LED) in the presence of riboflavin against Listeria monocytogenes on the surface of smoked salmon. Food Sci. Biotechnol. 2021, 30, 609–618. [Google Scholar] [CrossRef]
- Su, L.; Huang, J.; Li, H.; Pan, Y.; Zhu, B.; Zhao, Y.; Liu, H. Chitosan-riboflavin composite film based on photodynamic inactivation technology for antibacterial food packaging. Int. J. Biol. Macromol. 2021, 172, 231–240. [Google Scholar] [CrossRef]
- Kamran, M.A.; Qasim, M.; Udeabor, S.E.; Hameed, M.S.; Mannakandath, M.L.; Alshahrani, I. Impact of riboflavin mediated photodynamic disinfection around fixed orthodontic system infected with oral bacteria. Photodiagnosis Photodyn. Ther. 2021, 34, 102232. [Google Scholar] [CrossRef]
- Li, H.; Tan, L.; Chen, B.; Huang, J.; Zeng, Q.; Liu, H.; Zhao, Y.; Wang, J.J. Antibacterial potency of riboflavin-mediated photodynamic inactivation against Salmonella and its influences on tuna quality. LWT 2021, 146, 111462. [Google Scholar] [CrossRef]
- Alshehri, A.H. Mechanical and antimicrobial effects of riboflavin-mediated photosensitization of in vitro C. albicans formed on polymethyl methacrylate resin. Photodiagnosis Photodyn. Ther. 2021, 36, 102488. [Google Scholar] [CrossRef] [PubMed]
- Dhiman, R.; Kumar, N. Efficacy of Plant Antimicrobials as Preservative in Food. Intech 2019, 13. [Google Scholar]
- do Prado-Silva, L.; Brancini, G.T.P.; Braga, G.Ú.L.; Liao, X.; Ding, T.; Sant’Ana, A.S. Antimicrobial photodynamic treatment (aPDT) as an innovative technology to control spoilage and pathogenic microorganisms in agri-food products: An updated review. Food Control 2022, 132, 108527. [Google Scholar] [CrossRef]
- da Silveira, S.M.; Luciano, F.B.; Fronza, N.; Cunha, A.; Scheuermann, G.N.; Vieira, C.R.W. Chemical composition and antibacterial activity of Laurus nobilis essential oil towards foodborne pathogens and its application in fresh Tuscan sausage stored at 7 C. LWT-Food Sci. Technol. 2014, 59, 86–93. [Google Scholar] [CrossRef]
- Shi, M.; Chen, L.; Wang, Y.; Wang, W.; Yan, S. Effect of low-frequency pulsed ultrasound on drug delivery, antibacterial efficacy, and bone cement degradation in vancomycin-loaded calcium phosphate cement. Med. Sci. Monit. 2018, 24, 797–802. [Google Scholar] [CrossRef]
- Hernández-Ochoa, L.; Aguirre-Prieto, Y.B.; Nevárez-Moorillón, G.V.; Gutierrez-Mendez, N.; Salas-Muñoz, E. Use of essential oils and extracts from spices in meat protection. J. Food Sci. Technol. 2014, 51, 957–963. [Google Scholar] [CrossRef][Green Version]
- Kedia, A.; Prakash, B.; Mishra, P.K.; Dubey, N.K. Antifungal and antiaflatoxigenic properties of Cuminum cyminum (L.) seed essential oil and its efficacy as a preservative in stored commodities. Int. J. Food Microbiol. 2014, 168–169, 1–7. [Google Scholar] [CrossRef]
- Govaris, A.; Solomakos, N.; Pexara, A.; Chatzopoulou, P.S. The antimicrobial effect of oregano essential oil, nisin and their combination against Salmonella Enteritidis in minced sheep meat during refrigerated storage. Int. J. Food Microbiol. 2010, 137, 175–180. [Google Scholar] [CrossRef]
- El Moussaoui, N.; El Ouardy Khay, N.A.; Amajoud, N.; Boujida, N.; Charfi, S.; Senhaji, N.; Abrini, J. Effect of Origanum elongatum essential oil and heating on Pomegranate Juice Quality. Int. J. Curr. Microbiol. Appl. Sci. 2016, 5, 1–8. [Google Scholar] [CrossRef]
- Tserennadmid, R.; Takó, M.; Galgóczy, L.; Papp, T.; Vágvölgyi, C.; Gerő, L.; Krisch, J. Antibacterial effect of essential oils and interaction with food components. Open Life Sci. 2010, 5, 641–648. [Google Scholar] [CrossRef]
- Solomakos, N.; Govaris, A.; Koidis, P.; Botsoglou, N. The antimicrobial effect of thyme essential oil, nisin, and their combination against Listeria monocytogenes in minced beef during refrigerated storage. Food Microbiol. 2008, 25, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Selim, S. Antimicrobial activity of essential oils against vancomycin-resistant enterococci (vre) and Escherichia coli o157:h7 in feta soft cheese and minced beef meat. Brazilian J. Microbiol. Publ. Brazilian Soc. Microbiol. 2011, 42, 187–196. [Google Scholar] [CrossRef]
- Tajik, H.; Aminzare, M.; Mounesi Raad, T.; Hashemi, M.; Hassanzad Azar, H.; Raeisi, M.; Naghili, H. Effect of Zataria multiflora Boiss Essential Oil and Grape Seed Extract on the Shelf Life of Raw Buffalo Patty and Fate of Inoculated Listeria monocytogenes. J. Food Process. Preserv. 2015, 39, 3005–3013. [Google Scholar] [CrossRef]
- Thery, T.; Arendt, E.K. Antifungal activity of synthetic cowpea defensin Cp-thionin II and its application in dough. Food Microbiol. 2018, 73, 111–121. [Google Scholar] [CrossRef] [PubMed]
- López-Solanilla, E.; González-Zorn, B.; Novella, S.; Vázquez-Boland, J.A.; Rodríguez-Palenzuela, P. Susceptibility of Listeria monocytogenes to antimicrobial peptides. FEMS Microbiol. Lett. 2003, 226, 101–105. [Google Scholar] [CrossRef]
- Shwaiki, L.N.; Arendt, E.K.; Lynch, K.M. Study on the characterisation and application of synthetic peptide Snakin-1 derived from potato tubers–Action against food spoilage yeast. Food Control 2020, 118, 107362. [Google Scholar] [CrossRef]
- Hintz, T.; Matthews, K.K.; Di, R. The Use of Plant Antimicrobial Compounds for Food Preservation. Biomed Res. Int. 2015, 2015, 246264. [Google Scholar] [CrossRef]
- Tshabalala, R.; Kabelinde, A.; Kaptchouang Tchatchouang, C.-D.; Ateba, C.N.; Manganyi, M.C. Effect of Clove (Syzygium aromaticum) spice as microbial inhibitor of resistant bacteria and Organoleptic Quality of meat. Saudi J. Biol. Sci. 2021, 28, 3855–3863. [Google Scholar] [CrossRef]
- Temba, B.A.; Fletcher, M.T.; Fox, G.P.; Harvey, J.; Okoth, S.A.; Sultanbawa, Y. Curcumin-based photosensitization inactivates Aspergillus flavus and reduces aflatoxin B1 in maize kernels. Food Microbiol. 2019, 82, 82–88. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, J.; Li, S.; Hamzah, S.S.; Jiang, H.; Zhou, A.; Zeng, S.; Lin, S. Curcumin-based photodynamic sterilization for preservation of fresh-cut hami melon. Molecules 2019, 24, 2374. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Wolf-Hall, C.; Hall, C.A. 3rd Application of raisin extracts as preservatives in liquid bread and bread systems. J. Food Sci. 2009, 74, M177–M184. [Google Scholar] [CrossRef] [PubMed]
- Bhavya, M.L.; Hebbar, H.U. Sono-photodynamic inactivation of Escherichia coli and Staphylococcus aureus in orange juice. Ultrason. Sonochem. 2019, 57, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ip, M.; Leung, A.W.; Yang, Z.; Wang, P.; Zhang, B.; Ip, S.; Xu, C. Sonodynamic action of curcumin on foodborne bacteria Bacillus cereus and Escherichia coli. Ultrasonics 2015, 62, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ip, M.; Leung, A.W.; Xu, C. Sonodynamic inactivation of methicillin-resistant Staphylococcus aureus in planktonic condition by curcumin under ultrasound sonication. Ultrasonics 2014, 54, 2109–2114. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).