Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Relaxation Procedure
2.3. Signal Acquisition
2.4. Psychological Questionnaires
2.5. Signal Analysis
2.5.1. ECG
- HR: number of heart beats occurring per time unit, expressed in bpm. The HR is normally related to the activity of the sympathetic branch of the ANS;
- Standard deviation of normal-to-normal intervals between two consecutive R peaks of the ECG signal (SDNN): measurement of the HRV, expressed in ms. SDNN is normally affected by both sympathetic and parasympathetic components of the ANS [19];
- Changes in successive normal sinus (NN) intervals exceeding 50 ms (pNN50), expressed as a percentage. Like other HRV measures, pNN50 also indicates the overall activity of the autonomic nervous system; however, under certain experimental conditions, pNN50 is often considered as a reliable indicator of the parasympathetic activity;
- Cardiac sympathetic index (CSI) extracted from the Lorenz plot. CSI is considered a reliable indicator for the sympathetic activity [20].
- Normalized component of the ECG signal power spectral density at low frequency (0.04–0.15 Hz) (nLF). nLF is normally considered to be related to both sympathetic and parasympathetic activity;
- Normalized component of the power spectral density of the ECG spectrum at high frequency (0.15–0.4 Hz) (nHF). nHF is normally related to the parasympathetic activity;
- Low- vs. high-frequency components of the power spectral density of the ECG spectrum (Low-to-High Frequency (LF/HF) ratio). LF/HF ratio is often considered as a sort of balance between sympathetic and parasympathetic activity.
2.5.2. GSR
2.6. Statistical Analysis
2.7. Machine Learning
3. Results
3.1. Normality Test
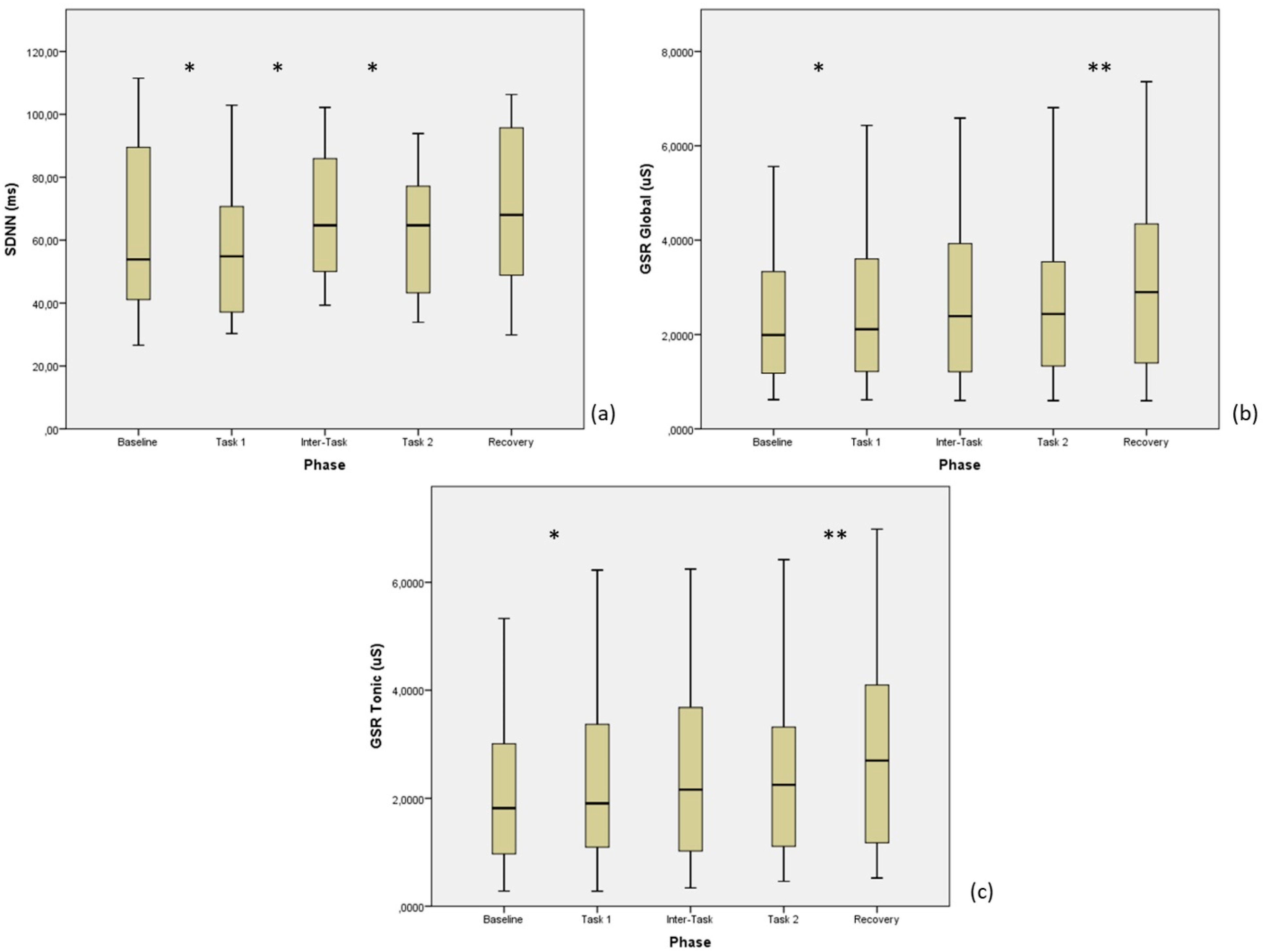
3.2. ECG Parameters
3.2.1. Group A
3.2.2. Group B
3.3. GSR Parameters
3.3.1. Group A
3.3.2. Group B
3.4. Questionnaires
3.5. Correlations between Autonomic Parameters and Questionnaires
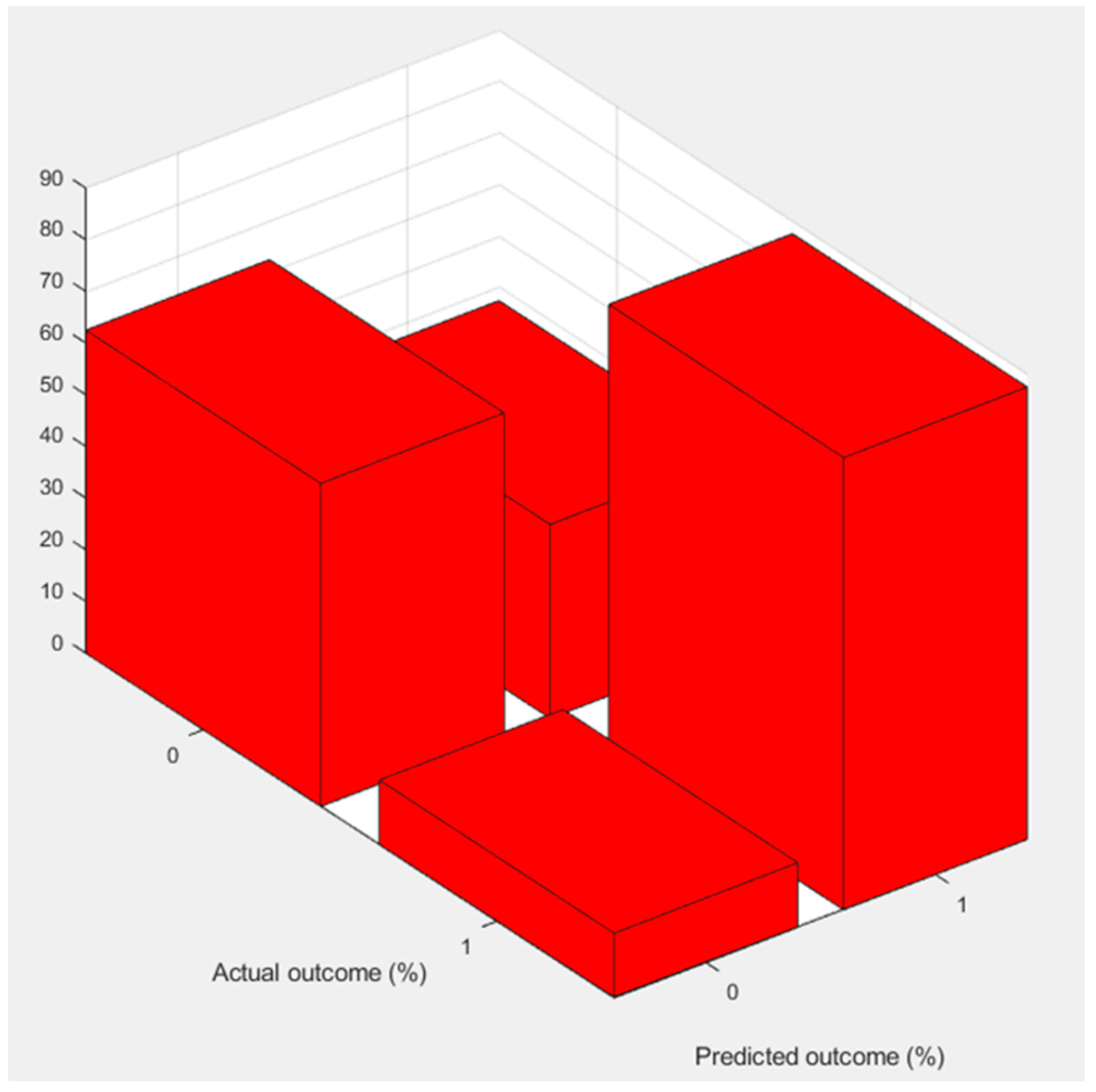
3.6. Machine Learning
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Slavich, G.M. Life Stress and Health: A Review of Conceptual Issues and Recent Findings. Teach. Psychol. 2016, 43, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Li, A.W.; Goldsmith, C.A. The effects of yoga on anxiety and stress. Altern. Med. Rev. 2012, 17, 21–35. [Google Scholar]
- Pascoe, M.C.; Thompson, D.R.; Ski, C.F. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology 2017, 86, 152–168. [Google Scholar] [CrossRef]
- Sawane, M.V.; Gupta, S.S. Resting heart rate variability after yogic training and swimming: A prospective randomized comparative trial. Int. J. Yoga 2015, 8, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Harinath, K.; Malhotra, A.S.; Pal, K.; Prasad, R.; Kumar, R.; Kain, T.C.; Rai, L.; Sawhney, R.C. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J. Altern. Complement Med. 2004, 10, 261–268. [Google Scholar] [CrossRef]
- Granath, J.; Ingvarsson, S.; Von Thiele, U.; Lundberg, U. Stress management: A randomized study of cognitive behavioural therapy and yoga. Cogn. Behav. Ther. 2006, 35, 3–10. [Google Scholar] [CrossRef]
- Tonacci, A.; Billeci, L.; Burrai, E.; Sansone, F.; Conte, R. Comparative Evaluation of the Autonomic Response to Cognitive and Sensory Stimulations through Wearable Sensors. Sensors 2019, 19, 4661. [Google Scholar] [CrossRef]
- Hernando, D.; Roca, S.; Sancho, J.; Alesanco, Á.; Bailón, R. Validation of the Apple Watch for Heart Rate Variability Measurements during Relax and Mental Stress in Healthy Subjects. Sensors 2018, 18, 2619. [Google Scholar] [CrossRef]
- Siirtola, P.; Koskimäki, H.; Mönttinen, H.; Röning, J. Using Sleep Time Data from Wearable Sensors for Early Detection of Migraine Attacks. Sensors 2018, 18, 1374. [Google Scholar] [CrossRef]
- Sano, A.; Taylor, S.; McHill, A.W.; Phillips, A.J.; Barger, L.K.; Klerman, E.; Picard, R. Identifying Objective Physiological Markers and Modifiable Behaviors for Self-Reported Stress and Mental Health Status Using Wearable Sensors and Mobile Phones: Observational Study. J. Med. Internet Res. 2018, 20, e210. [Google Scholar] [CrossRef] [PubMed]
- Van Puyvelde, M.; Collette, L.; Gorissen, A.S.; Pattyn, N.; McGlone, F. Infants Autonomic Cardio- Respiratory Responses to Nurturing Stroking Touch Delivered by the Mother or the Father. Front. Physiol. 2019, 10, 1117. [Google Scholar] [CrossRef]
- Tonacci, A.; Billeci, L.; Sansone, F.; Masci, A.; Pala, A.P.; Domenici, C.; Conte, R. An Innovative, Unobtrusive Approach to Investigate Smartphone Interaction in Nonaddicted Subjects Based on Wearable Sensors: A Pilot Study. Medicina 2019, 55, 37. [Google Scholar] [CrossRef]
- Rossi, V.; Pourtois, G. Transient state-dependent fluctuations in anxiety measured using STAI, POMS, PANAS or VAS: A comparative review. Anxiety Stress Coping 2012, 25, 603–645. [Google Scholar] [CrossRef] [PubMed]
- Freyd, M. The graphic rating scale. J. Educ. Psychol. 1923, 14, 83–102. [Google Scholar] [CrossRef]
- Spielberger, C.D. The nature and measurement of anxiety. In Cross-Cultural Anxiety; Spielberger, C.D., Diaz-Guerrero, R., Eds.; Hemisphere/Wiley: Washington, DC, USA, 1976. [Google Scholar]
- Pan, J.; Tompkins, W.J. A real-time QRS detection algorithm. IEEE Trans. Biomed. Eng. 1985, 32, 230–236. [Google Scholar] [CrossRef]
- Di Palma, S.; Tonacci, A.; Narzisi, A.; Domenici, C.; Pioggia, G.; Muratori, F.; Billeci, L. MICHELANGELO Study Group. Monitoring of autonomic response to sociocognitive tasks during treatment in children with Autism Spectrum Disorders by wearable technologies: A feasibility study. Comput. Biol. Med. 2016, 85, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Billeci, L.; Tonacci, A.; Narzisi, A.; Manigrasso, Z.; Varanini, M.; Fulceri, F.; Lattarulo, C.; Calderoni, S.; Muratori, F. Heart Rate Variability During a Joint Attention Task in Toddlers with Autism Spectrum Disorders. Front. Physiol. 2018, 9, 467. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Dodo, N.; Hashimoto, R. Autonomic Nervous System Activity During a Speech Task. Front Neurosci. 2019, 13, 406. [Google Scholar] [CrossRef] [PubMed]
- Welch, P.D. The use of Fast Fourier Transform for the estimation of power spectra: A method based on time averaging over short, modified periodograms. IEEE Trans. Audio Electroacoust. 1967, 15, 70–73. [Google Scholar] [CrossRef]
- Benedek, M.; Kaernbach, C. A continuous measure of phasic electrodermal activity. J. Neurosci. Methods 2010, 190, 80–91. [Google Scholar] [CrossRef]
- Shapiro, S.S.; Wilk, M.B. An analysis of variance test for normality (complete samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Ghosh, A.; Danieli, M.; Riccardi, G. Annotation and prediction of stress and workload from physiological and inertial signals. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2015, 2015, 1621–1624. [Google Scholar]
- Joshi, A.; Kiran, R.; Sah, A.N. Stress monitoring through non-invasive instrumental analysis of skin conductivity. Work 2017, 57, 233–243. [Google Scholar] [CrossRef]
- Nepal, O.; Jha, R.K.; Bhattarai, A.; Khadka, P.; Kapoor, B.K. Galvanic Skin Response as a Simple Physiology Lab Teaching Tool- An Alternative Indicator of Sympathetic Arousal. Kathmandu Univ. Med. J. (KUMJ) 2018, 16, 156–160. [Google Scholar]
- Nijjar, P.S.; Puppala, V.K.; Dickinson, O.; Duval, S.; Duprez, D.; Kreitzer, M.J.; Benditt, D.G. Modulation of the autonomic nervous system assessed through heart rate variability by a mindfulness based stress reduction program. Int. J. Cardiol. 2014, 177, 557–559. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Murata, T.; Hamada, T.; Omori, M.; Kosaka, H.; Kikuchi, M.; Yoshida, H.; Wada, Y. Changes in EEG and autonomic nervous activity during meditation and their association with personality traits. Int. J. Psychophysiol. 2005, 55, 199–207. [Google Scholar] [CrossRef]
- Sun, S.; Hu, C.; Pan, J.; Liu, C.; Huang, M. Trait Mindfulness is Associated with Self-Similarity of Heart Rate Variability. Front. Psychol. 2019, 10, 314. [Google Scholar] [CrossRef]
- Peressutti, C.; Martín-González, J.M.; García-Manso, J.M. Does mindfulness meditation shift the cardiac autonomic nervous system to a highly orderly operational state? Int. J. Cardiol. 2012, 154, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Nivethitha, L.; Mooventhan, A.; Manjunath, N.K. Effects of Various Prāṇāyāma on Cardiovascular and Autonomic Variables. Anc. Sci. Life. 2016, 36, 72–77. [Google Scholar] [CrossRef]
- Bhaskar, L.; Kharya, C.; Deepak, K.K.; Kochupillai, V. Assessment of Cardiac Autonomic Tone Following Long Sudarshan Kriya Yoga in Art of Living Practitioners. J. Altern. Complement Med. 2017, 23, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Muralikrishnan, K.; Balakrishnan, B.; Balasubramanian, K.; Visnegarawla, F. Measurement of the effect of Isha Yoga on cardiac autonomic nervous system using short-term heart rate variability. J. Ayurveda Integr. Med. 2012, 3, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Singh, S.N.; Chatterjee, A.; Saha, M. Age-related changes in cardiovascular system, autonomic functions, and levels of BDNF of healthy active males: Role of yogic practice. Age 2014, 36, 9683. [Google Scholar] [CrossRef] [PubMed]
- Maranesi, E.; Morettini, M.; Agostinelli, A.; Giuliani, C.; Di Nardo, F.; Burattini, L. Health Monitoring in Sport Through Wearable Sensors: A Novel Approach Based on Heart-Rate Variability. In Mobile Networks for Biometric Data Analysis; Conti, M., Martínez Madrid, N., Seepold, R., Orcioni, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Raglio, A.; Imbriani, M.; Imbriani, C.; Baiardi, P.; Manzoni, S.; Gianotti, M.; Castelli, M.; Vanneschi, L.; Vico, F.; Manzoni, L. Machine learning techniques to predict the effectiveness of music therapy: A randomized controlled trial. Comput. Methods Programs Biomed. 2019, 185, 105160. [Google Scholar] [CrossRef]

| Group A | |||||
| Feature | Baseline | Task 1 | Inter-Task | Task 2 | Recovery |
| HR (bpm) | 72.6 ± 17.4 | 71.5 ± 15.6 | 71.8 ± 14.3 | 71.1 ± 13.6 | 72.6 ± 14.0 |
| SDNN (ms) | 64.3 ± 28.6 | 57.7 ± 24.5 | 67.4 ± 20.4 | 61.5 ± 20.0 | 70.7 ± 25.8 |
| pNN50 (%) | 25.3 ± 20.0 | 24.9 ± 22.5 | 25.6 ± 21.1 | 26.4 ± 22.7 | 25.7 ± 20.5 |
| CSI (ratio) | 2.41 ± 0.92 | 2.41 ± 1.03 | 2.64 ± 0.88 | 2.50 ± 1.02 | 2.68 ± 0.64 |
| nLF (n.u.) | 0.54 ± 0.23 | 0.52 ± 0.25 | 0.60 ± 0.23 | 0.54 ± 0.26 | 0.57 ± 0.18 |
| nHF (n.u.) | 0.46 ± 0.23 | 0.48 ± 0.25 | 0.40 ± 0.23 | 0.46 ± 0.26 | 0.43 ± 0.18 |
| LF/HF (ratio) | 1.90 ± 1.79 | 1.93 ± 1.96 | 2.71 ± 2.60 | 2.25 ± 2.51 | 1.93 ± 1.68 |
| Group B | |||||
| Feature | Baseline | Task 1 | Inter-Task | Task 2 | Recovery |
| HR (bpm) | 78.6 ± 11.0 | 77.1 ± 10.7 | 77.6 ± 8.8 | 77.1 ± 9.6 | 77.3 ± 8.8 |
| SDNN (ms) | 52.6 ± 25.5 | 51.7 ± 27.1 | 53.9 ± 29.7 | 53.6 ± 25.9 | 60.4 ± 32.4 |
| pNN50 (%) | 15.3 ± 13.6 | 15.7 ± 14.0 | 14.4 ± 12.9 | 15.0 ± 13.3 | 15.4 ± 14.6 |
| CSI (ratio) | 2.78 ± 0.65 | 2.63 ± 0.53 | 2.76 ± 0.65 | 2.81 ± 0.77 | 2.99 ± 0.92 |
| nLF (n.u.) | 0.56 ± 0.11 | 0.56 ± 0.12 | 0.55 ± 0.12 | 0.62 ± 0.13 | 0.58 ± 0.15 |
| nHF (n.u.) | 0.44 ± 0.11 | 0.44 ± 0.12 | 0.45 ± 0.12 | 0.38 ± 0.13 | 0.42 ± 0.15 |
| LF/HF (ratio) | 1.43 ± 0.80 | 1.41 ± 0.59 | 1.40 ± 0.78 | 1.93 ± 1.03 | 1.81 ± 1.49 |
| Group A | |||||
| Feature | Baseline | Task 1 | Inter-Task | Task 2 | Recovery |
| GSR Global (µS) | 2.34 ± 1.54 | 2.54 ± 1.71 | 2.78 ± 1.88 | 2.80 ± 1.92 | 3.21 ± 2.11 |
| GSR Tonic (µS) | 2.10 ± 1.56 | 2.32 ± 1.73 | 2.54 ± 1.85 | 2.59 ± 1.87 | 2.98 ± 2.05 |
| Group B | |||||
| Feature | Baseline | Task 1 | Inter-Task | Task 2 | Recovery |
| GSR Global (µS) | 1.43 ± 0.82 | 1.57 ± 1.01 | 1.46 ± 0.93 | 1.52 ± 1.02 | 1.80 ± 1.31 |
| GSR Tonic (µS) | 1.31 ± 0.76 | 1.47 ± 0.97 | 1.37 ± 0.90 | 1.40 ± 0.99 | 1.65 ± 1.26 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonacci, A.; Dellabate, A.; Dieni, A.; Bachi, L.; Sansone, F.; Conte, R.; Billeci, L. Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study. Processes 2020, 8, 448. https://doi.org/10.3390/pr8040448
Tonacci A, Dellabate A, Dieni A, Bachi L, Sansone F, Conte R, Billeci L. Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study. Processes. 2020; 8(4):448. https://doi.org/10.3390/pr8040448
Chicago/Turabian StyleTonacci, Alessandro, Alessandro Dellabate, Andrea Dieni, Lorenzo Bachi, Francesco Sansone, Raffaele Conte, and Lucia Billeci. 2020. "Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study" Processes 8, no. 4: 448. https://doi.org/10.3390/pr8040448
APA StyleTonacci, A., Dellabate, A., Dieni, A., Bachi, L., Sansone, F., Conte, R., & Billeci, L. (2020). Can Machine Learning Predict Stress Reduction Based on Wearable Sensors’ Data Following Relaxation at Workplace? A Pilot Study. Processes, 8(4), 448. https://doi.org/10.3390/pr8040448







