A Novel Seeding and Conditioning Bioreactor for Vascular Tissue Engineering
Abstract
:1. Introduction
2. Experimental Section
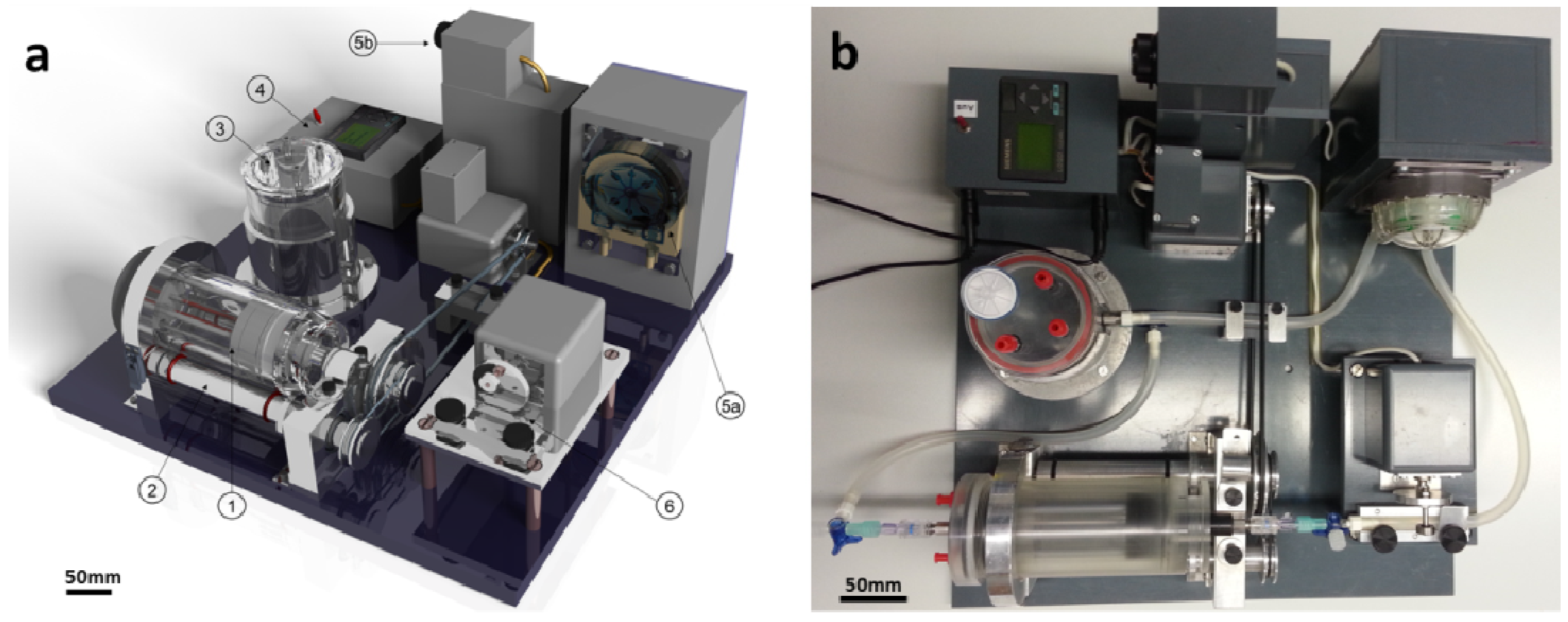
2.1. Bioreactor Development
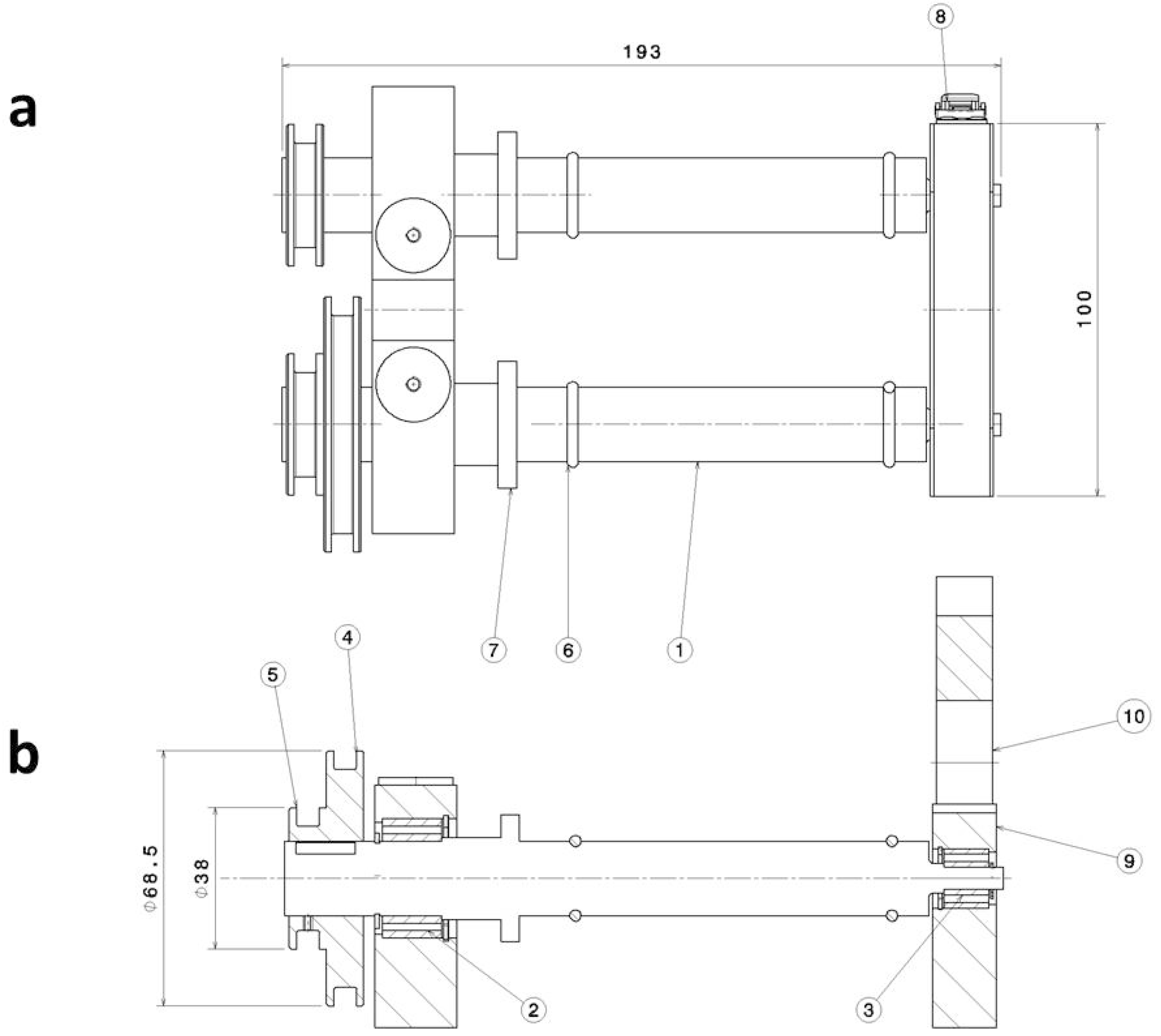
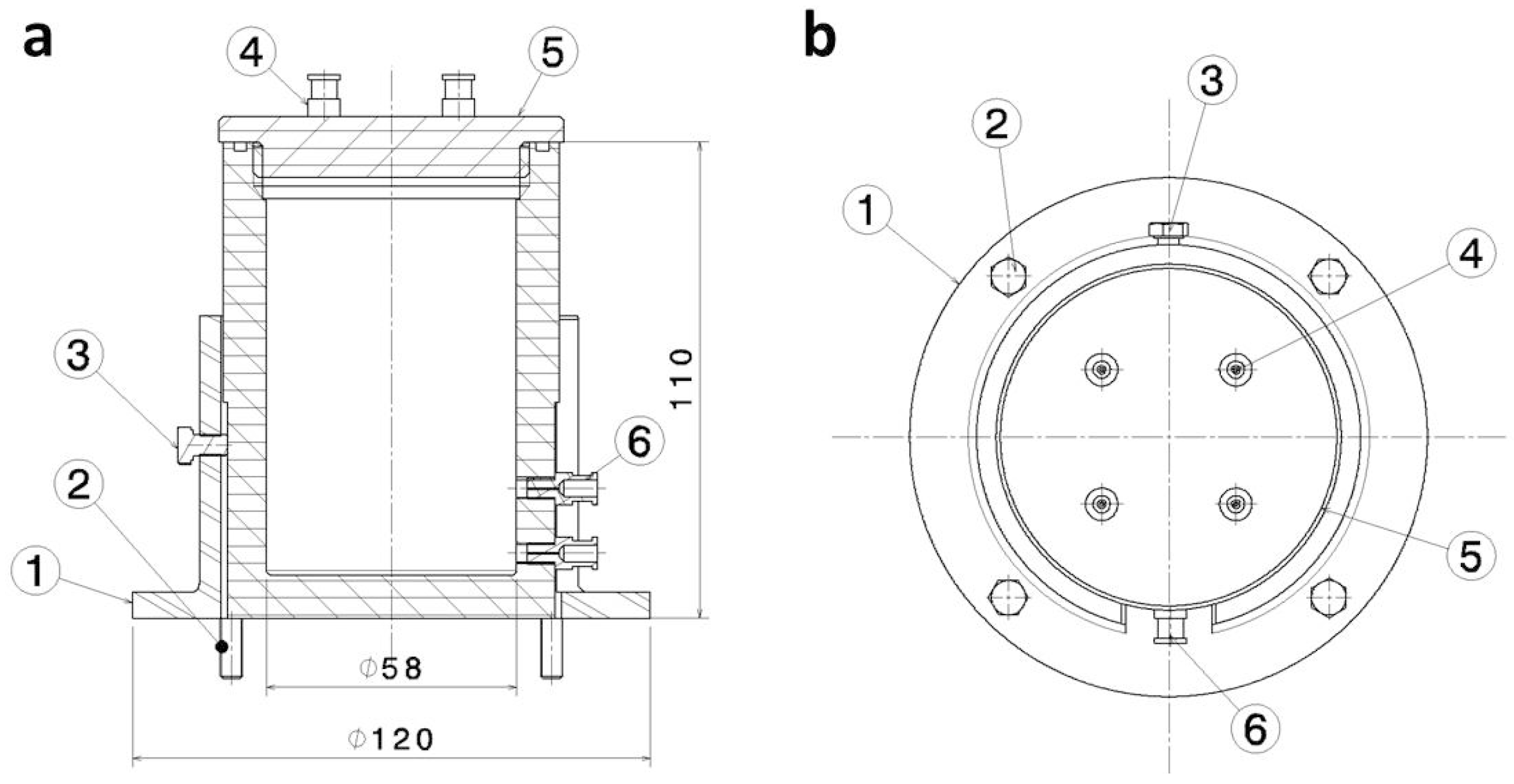
2.1.1. Construction
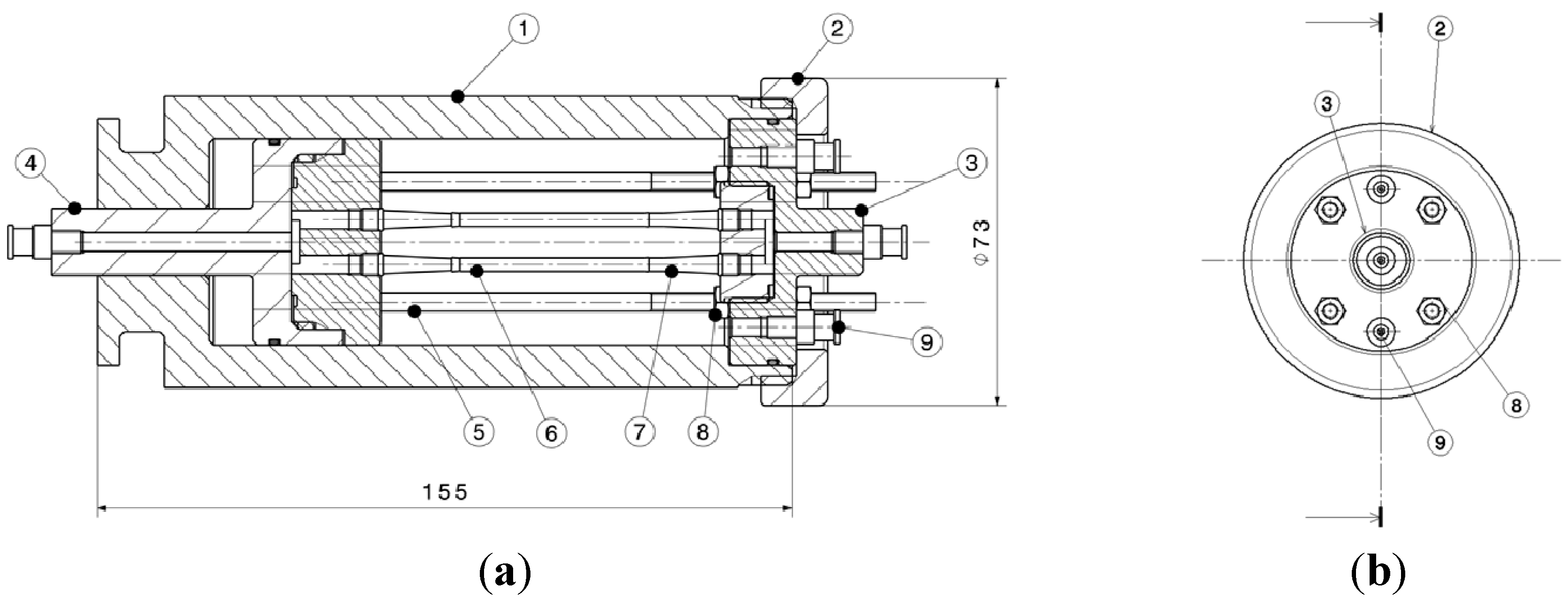
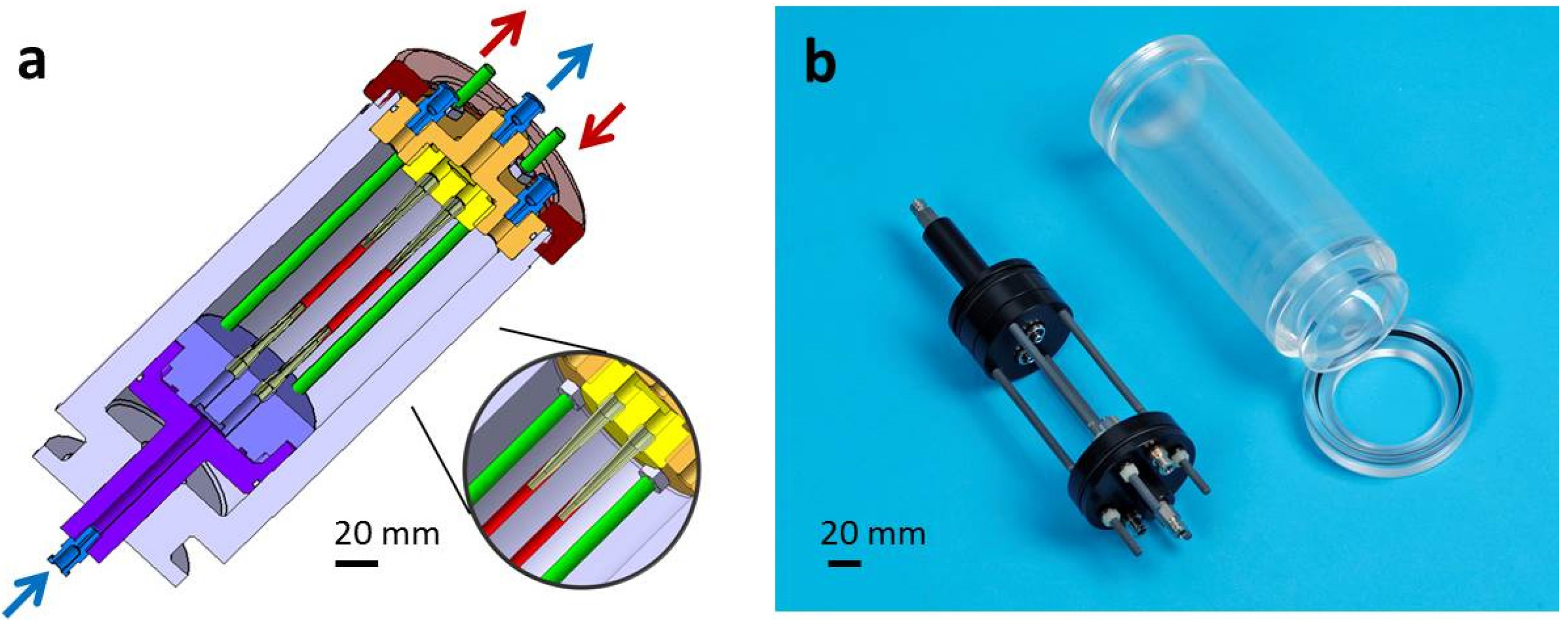
Seeding Device
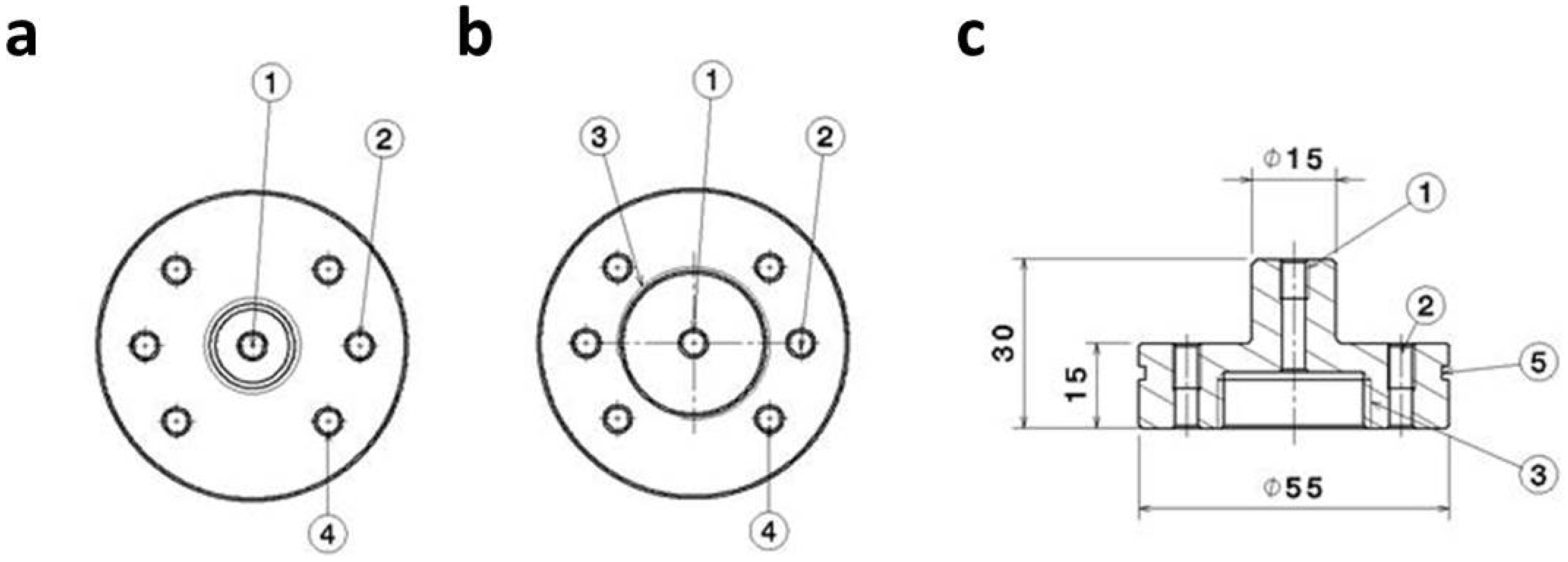
Mixer
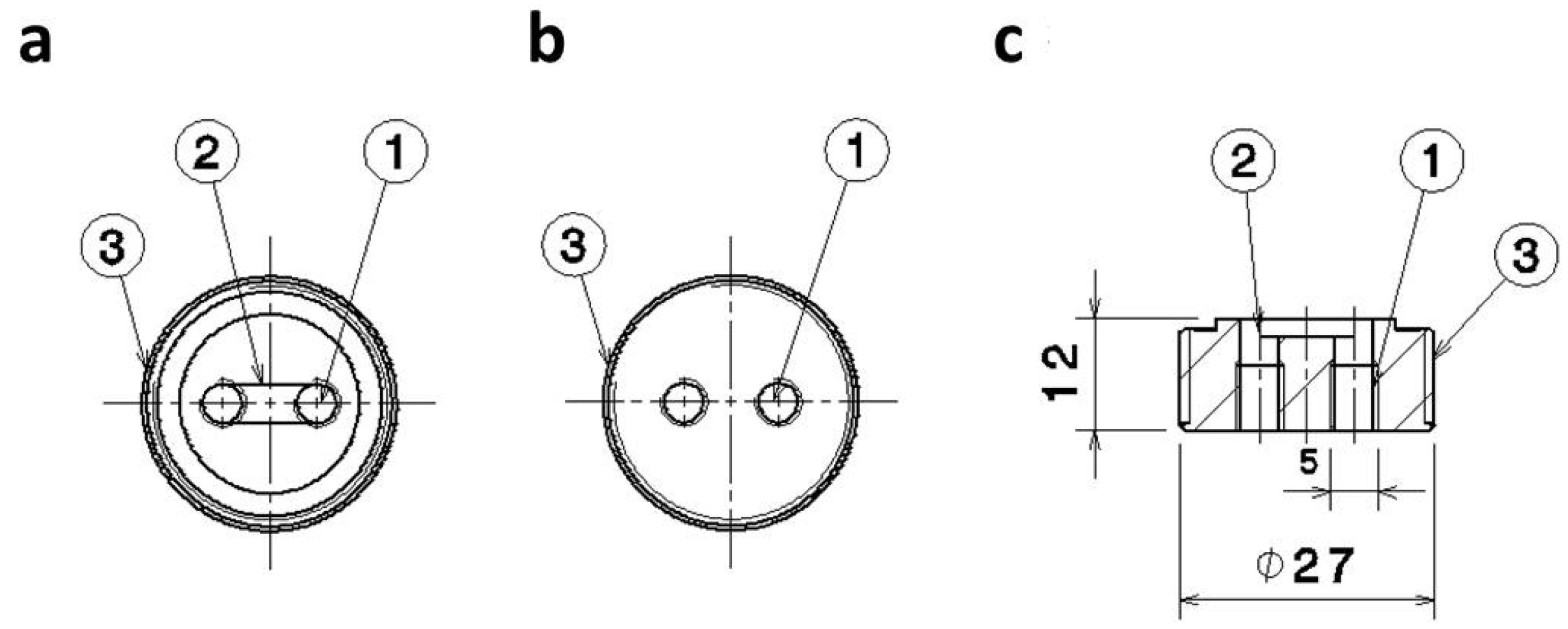
Media Reservoir
2.1.2. Sterilization
2.1.3. Functionality
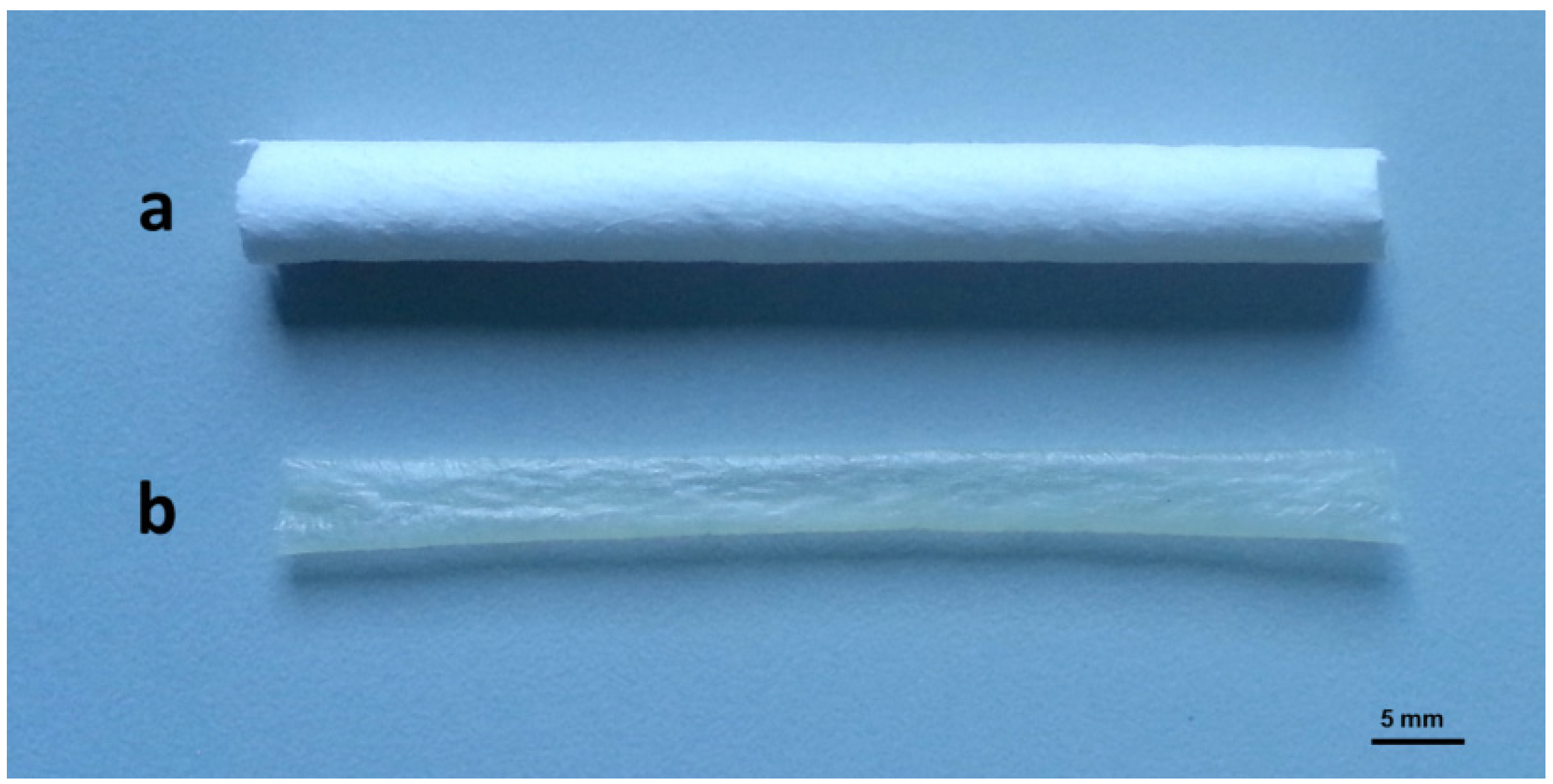
2.2. Scaffold Materials
2.3. Cell Source
2.3.1. Cell Isolation and Sub Culturing
2.3.2. Cell Characterization
2.4. Bioreactor Setups
2.4.1. Seeding Protocol
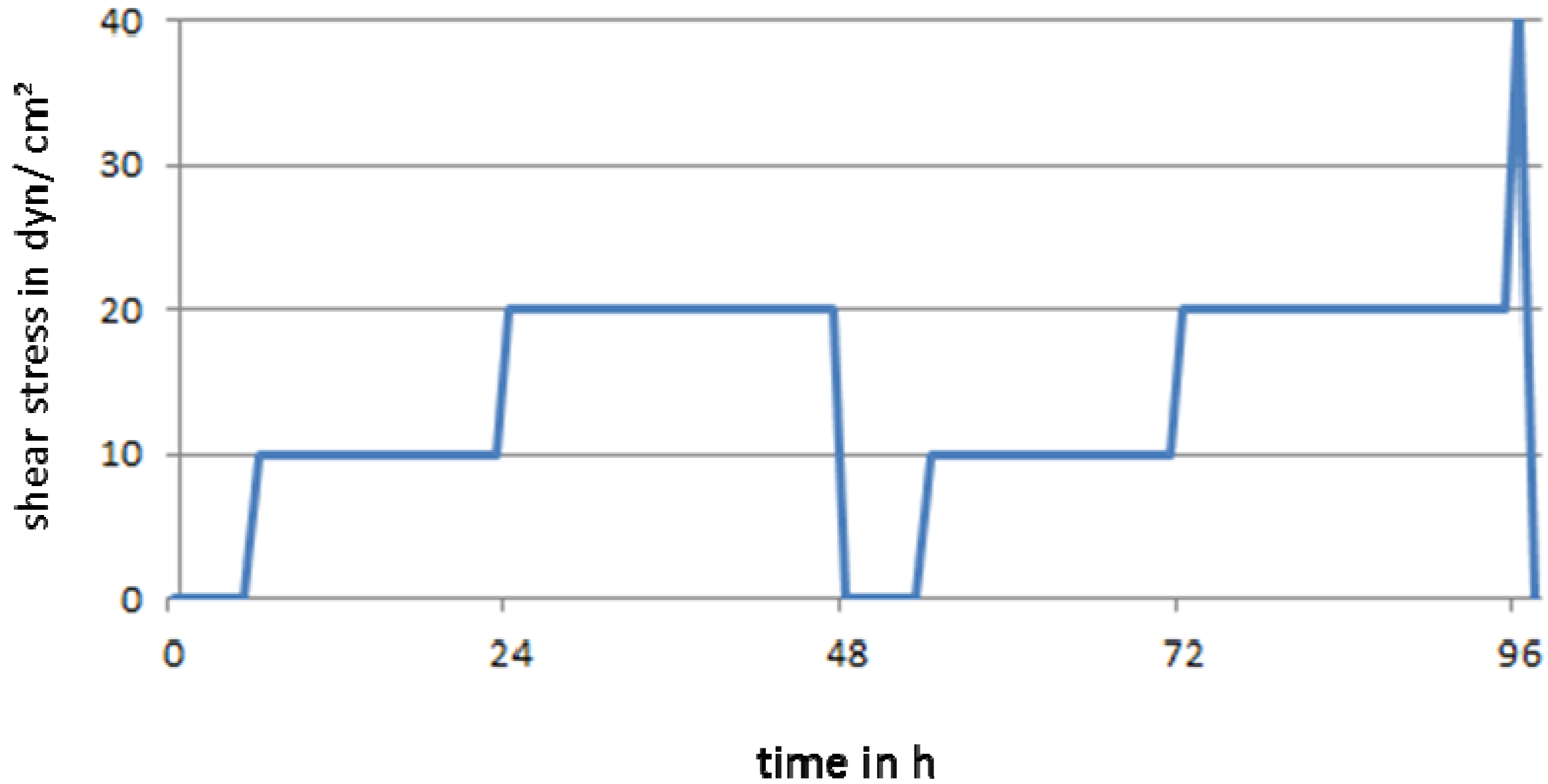
2.4.2. Perfusion Protocol
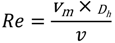
 ) divided by the pipes cross-sectional area (A)
) divided by the pipes cross-sectional area (A)

2.5. Sample Evaluation
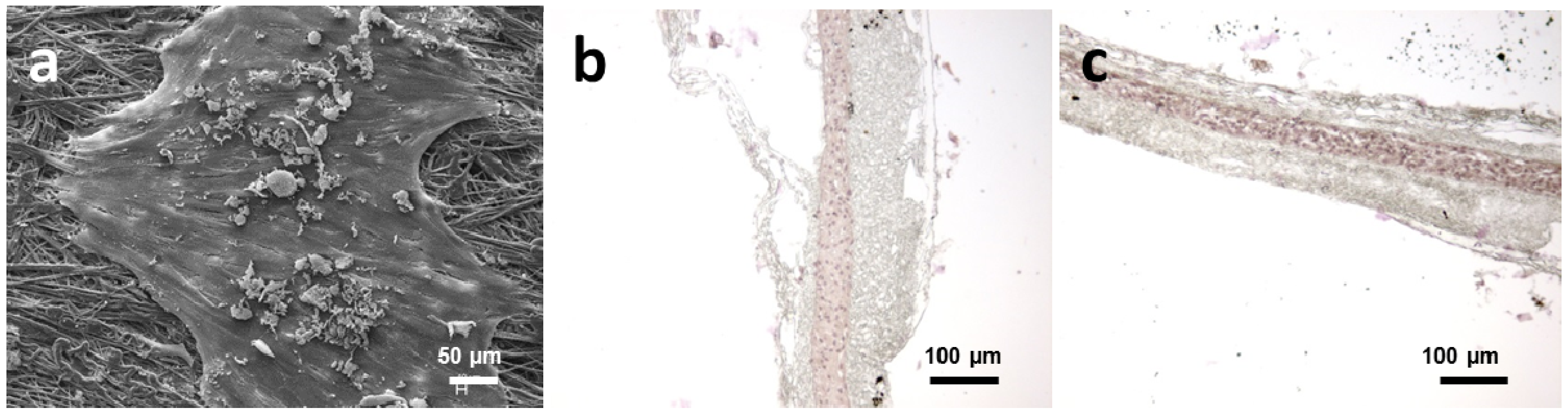
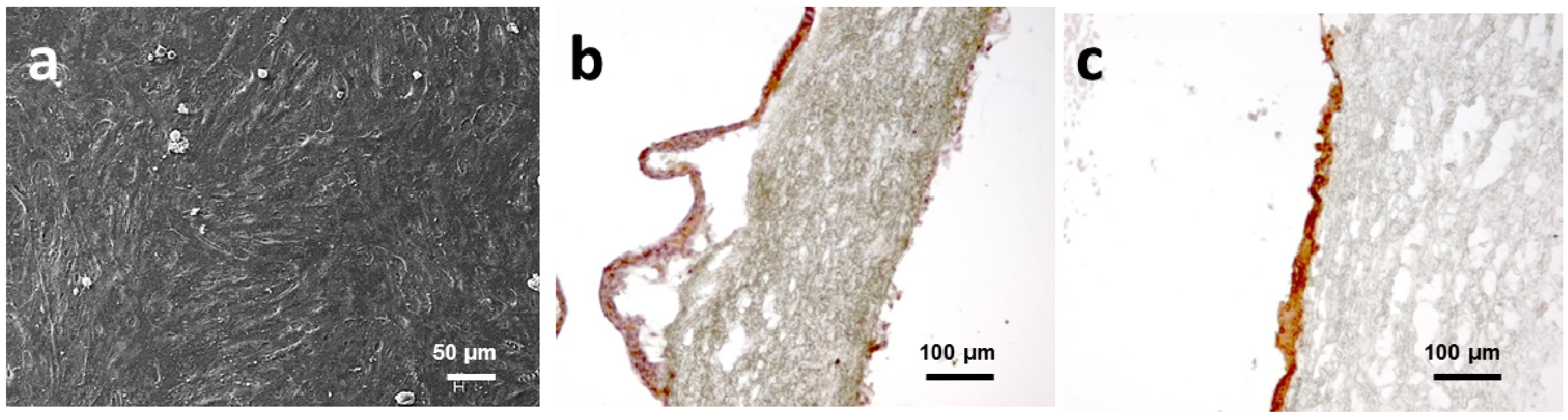
2.5.1. Scanning Electron Microscopy (SEM)
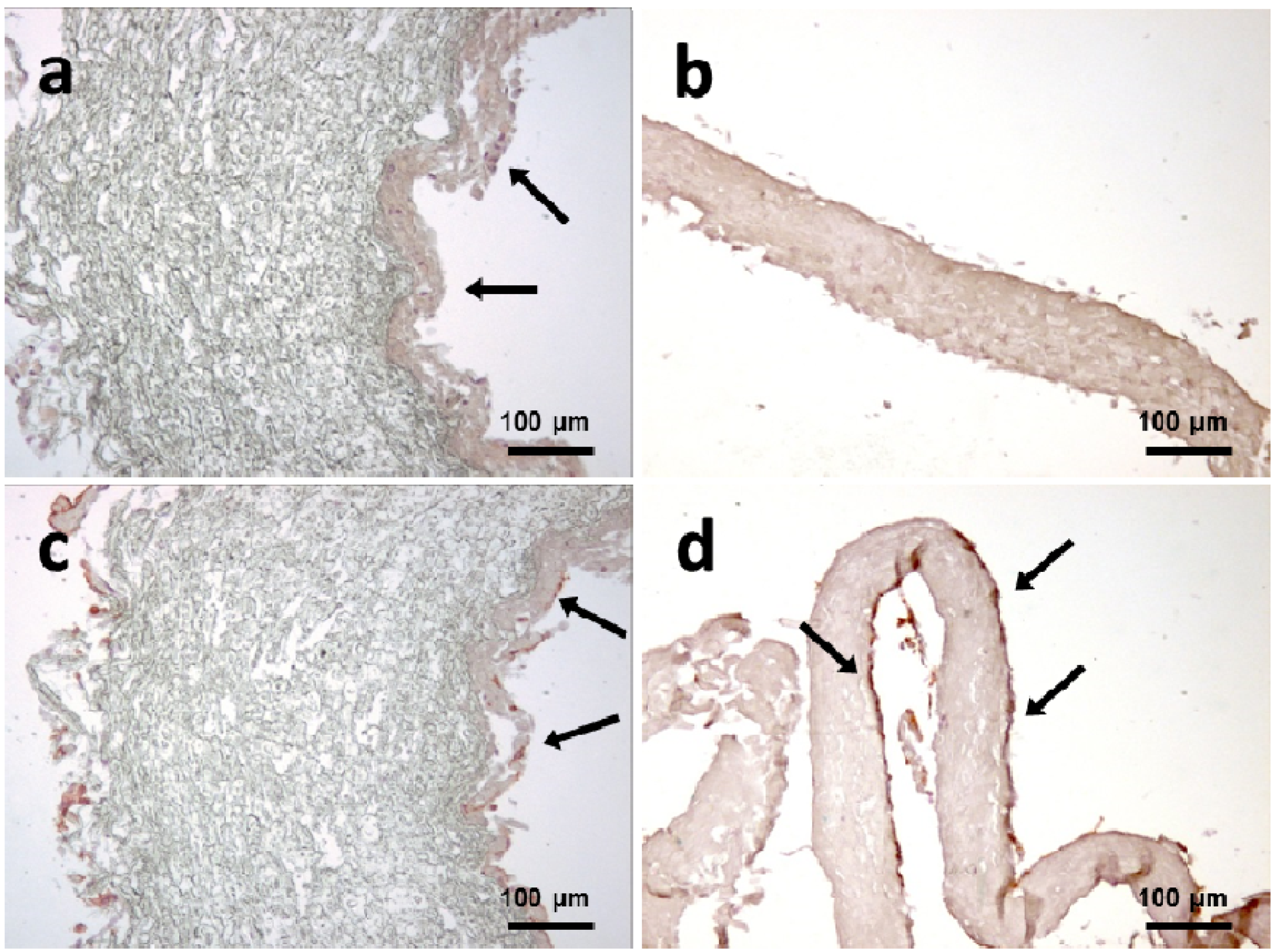
2.5.2. Immunohistochemistry (IHC)
3. Results and Discussion
3.1. Bioreactor Assembly
3.2. Bioreactor Sterility
3.3. Bioreactor Function
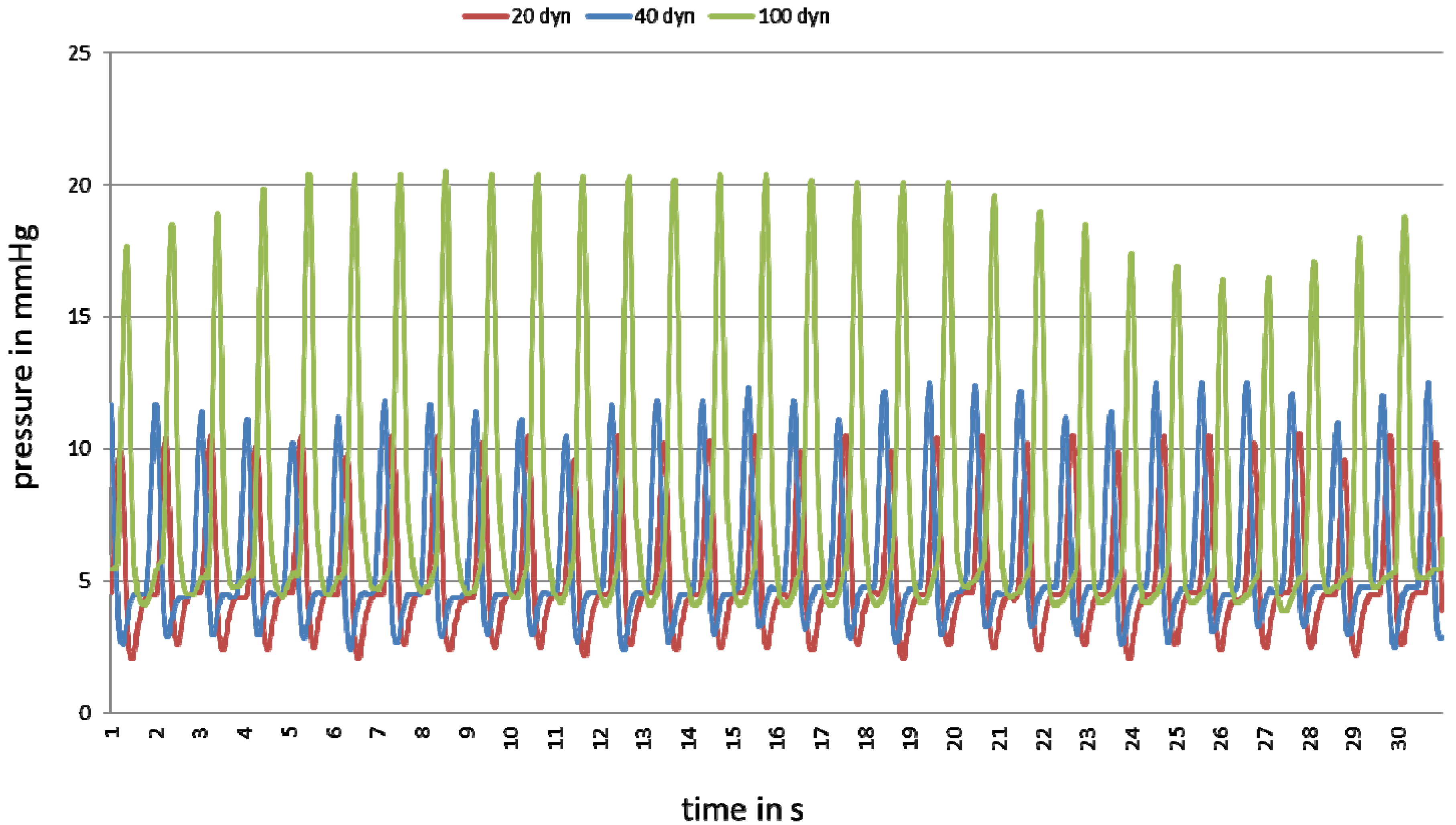
| Shear Stress (dyn/cm2) | Pressuremin (mmHg) | Pressuremax (mmHg) | Pressureaverage (mmHg) | |
|---|---|---|---|---|
| Without pulsation | 10 | 5.1 | 5.5 | 5.4 |
| 20 | 5.6 | 5.9 | 5.8 | |
| 40 | 5.7 | 6.1 | 5.9 | |
| 100 | 6.2 | 6.7 | 6.5 | |
| With pulsation | 20 | 2.1 | 10.6 | 5.2 |
| 40 | 2.4 | 12.5 | 5.7 | |
| 100 | 3.9 | 20.5 | 8.0 |
3.4. Experimental Evaluation of the Bioreactor

4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Causes of Death 2008 Summary Tables; Health Statistics and Informatics Department: Geneva, Switzerland, 2011. [Google Scholar]
- Löwel, H. Koronare Herzkrankheit und akuter Myokardinfark. In Gesundheitsberichterstattung des Bundes; Robert Koch-Institut: Berlin, Germany, 2006; Heft 33 (In German). [Google Scholar]
- Ku, D.N.; Allen, R.C. Vascular Grafts. In Tissue Engineering and Artificial Organs, 3rd ed.; Brozino, J.D., Ed.; The Biomedical Engineering Handbook, Third Edition; CRC Press: Boca Raton, FL, USA, 2006. [Google Scholar]
- Aper, T.; Haverich, A.; Teebken, O. New developments in tissue engineering of vascular prosthetic grafts. Vasa 2009, 38, 99–122. [Google Scholar] [CrossRef]
- Takayama, T.; Hiro, T.; Hirayama, A. Is angioplasty able to become the gold standard of treatment beyond bypass surgery for patients with multivessel coronary artery disease? Therapeutic strategies for 3-vessel coronary artery disease: OPCAB vs. PCI(PCI-Side). Circ. J. 2010, 74, 2744–2749. [Google Scholar] [CrossRef]
- Sündermann, S.H.; Salzberg, S.P. Renaissance of surgery for coronary artery disease. Praxis (Bern 1994) 2011, 100, 23–28. [Google Scholar] [CrossRef]
- Daemen, J.; Boersma, E.; Flather, M.; Booth, J.; Stables, R.; Rodriguez, A.; Rodriguez-Granillo, G.; Hueb, W.A.; Lemos, P.A.; Serruys, P.W. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: A meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation 2008, 118, 1146–1154. [Google Scholar] [CrossRef]
- Guyton, R.A. Coronary artery bypass is superior to drug-eluting stents in multivessel coronary artery disease. Ann. Thorac. Surg. 2006, 81, 1949–1957. [Google Scholar]
- Cohen, D.J.; Lavelle, T.A.; van Hout, B.; Li, H.; Lei, Y.; Robertus, K.; Pinto, D.; Magnuson, E.A.; McGarry, T.F.; Lucas, S.K.; et al. Economic outcomes of percutaneous coronary intervention with drug-eluting stents versus bypass surgery for patients with left main or three-vessel coronary artery disease: One-year results from the SYNTAX trial. Catheter. Cardiovasc. Interv. 2012, 79, 198–209. [Google Scholar] [CrossRef] [Green Version]
- Cohen, D.J.; van Hout, B.; Serruys, P.W.; Mohr, F.W.; Macaya, C.; den Heijer, P.; Vrakking, M.M.; Wang, K.; Mahoney, E.M.; Audi, S.; et al. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N. Engl. J. Med. 2011, 364, 1016–1026. [Google Scholar]
- Moneta, G.L.; Porter, J.M. Arterial substitutes in peripheral vascular surgery: A review. J. Long Term Eff. Med. Implants 1995, 5, 47–67. [Google Scholar]
- Burkel, W.E. The challenge of small diameter vascular grafts. Med. Prog. Technol. 1988, 14, 165–175. [Google Scholar]
- Peppas, N.A.; Langer, R. New challenges in biomaterials. Science 1994, 263, 1715–1720. [Google Scholar]
- Zhou, M.; Liu, Z.; Liu, C.; Jiang, X.; Wei, Z.; Qiao, W.; Ran, F.; Wang, W.; Qiao, T.; Liu, C. Tissue engineering of small-diameter vascular grafts by endothelial progenitor cells seeding heparin-coated decellularized scaffolds. J. Biomed. Mater. Res. Part B 2012, 100, 111–120. [Google Scholar]
- Wood, S.C.; Tang, X.; Tesfamariam, B. Paclitaxel potentiates inflammatory cytokine-induced prothrombotic molecules in endothelial cells. J. Cardiovasc. Pharmacol. 2010, 55, 276–285. [Google Scholar]
- Kannan, R.Y.; Salacinski, H.J.; Butler, P.E.; Hamilton, G.; Seifalian, A.M. Current status of prosthetic bypass grafts: A review. J. Biomed. Mater. Res. Part B 2005, 74, 570–581. [Google Scholar]
- Yazdani, S.K.; Tillman, B.W.; Berry, J.L.; Soker, S.; Geary, R.L. The fate of an endothelium layer after preconditioning. J. Vasc. Surg. 2010, 51, 174–183. [Google Scholar] [CrossRef]
- Kerdjoudj, H.; Moby, V.; Berthelemy, N.; Gentils, M.; Boura, C.; Bordenave, L.; Stoltz, J.F.; Menu, P. The ideal small arterial substitute: Role of cell seeding and tissue engineering. Clin. Hemorheol. Microcirc. 2007, 37, 89–98. [Google Scholar]
- Bourget, J.M.; Gauvin, R.; Larouche, D.; Lavoie, A.; Labbe, R.; Auger, F.A.; Germain, L. Human fibroblast-derived ECM as a scaffold for vascular tissue engineering. Biomaterials 2012, 33, 9205–9213. [Google Scholar] [CrossRef]
- Gulbins, H.; Goldemund, A.; Anderson, I.; Haas, U.; Uhlig, A.; Meiser, B.; Reichart, B. Preseeding with autologous fibroblasts improves endothelialization of glutaraldehyde-fixed porcine aortic valves. J. Thorac. Cardiovasc. Surg. 2003, 125, 592–601. [Google Scholar] [CrossRef]
- DiMuzio, P.; Fischer, L.; McIlhenny, S.; DiMatteo, C.; Golesorhki, N.; Grabo, D.; Tarola, N.; Mericli, A.; Shapiro, I.; Tulenko, T. Development of a tissue-engineered bypass graft seeded with stem cells. Vascular 2006, 14, 338–342. [Google Scholar] [CrossRef]
- Kawamoto, A.; Asahara, T. Role of progenitor endothelial cells in cardiovascular disease and upcoming therapies. Catheter. Cardiovasc. Interv. 2007, 70, 477–484. [Google Scholar]
- Gulbins, H.; Pritisanac, A.; Dauner, M.; Petzold, R.; Goldemund, A.; Doser, M.; Meiser, B.; Reichart, B. Seeding of human vascular cells onto small diameter polyurethane vascular grafts. Thorac. Cardiovasc. Surg. 2006, 54, 102–107. [Google Scholar] [CrossRef]
- Alison, M.R.; Poulsom, R.; Forbes, S.; Wright, N.A. An introduction to stem cells. J. Pathol. 2002, 197, 419–423. [Google Scholar] [CrossRef]
- Martin-Rendon, E.; Watt, S.M. Exploitation of stem cell plasticity. Transfus. Med. 2003, 13, 325–349. [Google Scholar]
- Ringe, J.; Kaps, C.; Burmester, G.R.; Sittinger, M. Stem cells for regenerative medicine: Advances in the engineering of tissues and organs. Die Naturwissenschaften 2002, 89, 338–351. [Google Scholar] [CrossRef]
- Zimmermann, W.H.; Eschenhagen, T. Cardiac tissue engineering for replacement therapy. Heart Fail. Rev. 2003, 8, 259–269. [Google Scholar] [CrossRef]
- Petit-Zeman, S. Regenerative medicine. Nat. Biotechnol. 2001, 19, 201–206. [Google Scholar]
- Pittenger, M.F.; Mackay, A.M.; Beck, S.C.; Jaiswal, R.K.; Douglas, R.; Mosca, J.D.; Moorman, M.A.; Simonetti, D.W.; Craig, S.; Marshak, D.R. Multilineage potential of adult human mesenchymal stem cells. Science 1999, 284, 143–147. [Google Scholar] [CrossRef]
- Matsumura, G.; Hibino, N.; Ikada, Y.; Kurosawa, H.; Shin’oka, T. Successful application of tissue engineered vascular autografts: Clinical experience. Biomaterials 2003, 24, 2303–2308. [Google Scholar]
- Ballermann, B.J.; Dardik, A.; Eng, E.; Liu, A. Shear stress and the endothelium. Kidney Int. Suppl. 1998, 67, S100–S108. [Google Scholar]
- Solan, A.; Dahl, S.L.; Niklason, L.E. Effects of mechanical stretch on collagen and cross-linking in engineered blood vessels. Cell Transpl. 2009, 18, 915–921. [Google Scholar] [CrossRef]
- Barron, V.; Lyons, E.; Stenson-Cox, C.; McHugh, P.E.; Pandit, A. Bioreactors for cardiovascular cell and tissue growth: A review. Ann. Biomed. Eng. 2003, 31, 1017–1030. [Google Scholar] [CrossRef]
- Lee, D.J.; Steen, J.; Jordan, J.E.; Kincaid, E.H.; Kon, N.D.; Atala, A.; Berry, J.; Yoo, J.J. Endothelialization of heart valve matrix using a computer-assisted pulsatile bioreactor. Tissue Eng. Part A 2009, 15, 807–814. [Google Scholar]
- Chen, H.C.; Hu, Y.C. Bioreactors for tissue engineering. Biotechnol. Lett. 2006, 28, 1415–1423. [Google Scholar]
- Morsi, Y.S.; Yang, W.W.; Owida, A.; Wong, C.S. Development of a novel pulsatile bioreactor for tissue culture. J. Artif. Org. 2007, 10, 109–114. [Google Scholar] [CrossRef]
- Wendt, D.; Riboldi, S.A.; Cioffi, M.; Martin, I. Bioreactors in tissue engineering: Scientific challenges and clinical perspectives. Adv. Biochem. Eng. Biotechnol. 2009, 112, 1–27. [Google Scholar]
- Chlupac, J.; Filova, E.; Bacakova, L. Blood vessel replacement: 50 years of development and tissue engineering paradigms in vascular surgery. Physiol. Res. Acad. Sci. Bohemoslov. 2009, 58 (Suppl. 2), S119–S139. [Google Scholar]
- Rademacher, A.; Paulitschke, M.; Meyer, R.; Hetzer, R. Endothelialization of PTFE vascular grafts under flow induces significant cell changes. Int. J. Artif. Org. 2001, 24, 235–242. [Google Scholar]
- Martin, I.; Smith, T.; Wendt, D. Bioreactor-based roadmap for the translation of tissue engineering strategies into clinical products. Trends Biotechnol. 2009, 27, 495–502. [Google Scholar] [Green Version]
- Bilodeau, K.; Couet, F.; Boccafoschi, F.; Mantovani, D. Design of a perfusion bioreactor specific to the regeneration of vascular tissues under mechanical stresses. Artif. Org. 2005, 29, 906–912. [Google Scholar] [CrossRef]
- Dunkern, T.R.; Paulitschke, M.; Meyer, R.; Buttemeyer, R.; Hetzer, R.; Burmester, G.; Sittinger, M. A novel perfusion system for the endothelialisation of PTFE grafts under defined flow. Eur. J. Vasc. Endovasc. Surg. 1999, 18, 105–110. [Google Scholar]
- Heydarkhan-Hagvall, S.; Esguerra, M.; Helenius, G.; Soderberg, R.; Johansson, B.R.; Risberg, B. Production of extracellular matrix components in tissue-engineered blood vessels. Tissue Eng. 2006, 12, 831–842. [Google Scholar]
- Sodian, R.; Lemke, T.; Fritsche, C.; Hoerstrup, S.P.; Fu, P.; Potapov, E.V.; Hausmann, H.; Hetzer, R. Tissue-engineering bioreactors: A new combined cell-seeding and perfusion system for vascular tissue engineering. Tissue Eng. 2002, 8, 863–870. [Google Scholar]
- Williams, C.; Wick, T.M. Perfusion bioreactor for small diameter tissue-engineered arteries. Tissue Eng. 2004, 10, 930–941. [Google Scholar] [CrossRef]
- Arrigoni, C.; Chitto, A.; Mantero, S.; Remuzzi, A. Rotating versus perfusion bioreactor for the culture of engineered vascular constructs based on hyaluronic acid. Biotechnol. Bioeng. 2008, 100, 988–997. [Google Scholar] [CrossRef]
- Engbers-Buijtenhuijs, P.; Buttafoco, L.; Poot, A.A.; Dijkstra, P.J.; de Vos, R.A.; Sterk, L.M.; Geelkerken, R.H.; Vermes, I.; Feijen, J. Biological characterisation of vascular grafts cultured in a bioreactor. Biomaterials 2006, 27, 2390–2397. [Google Scholar]
- Hahn, M.S.; McHale, M.K.; Wang, E.; Schmedlen, R.H.; West, J.L. Physiologic pulsatile flow bioreactor conditioning of poly(ethylene glycol)-based tissue engineered vascular grafts. Ann. Biomed. Eng. 2007, 35, 190–200. [Google Scholar]
- Aleksieva, G.; Hollweck, T.; Thierfelder, N.; Haas, U.; Koenig, F.; Fano, C.; Dauner, M.; Wintermantel, E.; Reichart, B.; Schmitz, C.; et al. Use of a special bioreactor for the cultivation of a new flexible polyurethane scaffold for aortic valve tissue engineering. Biomed. Eng. Online 2012, 11. [Google Scholar] [CrossRef]
- Huang, A.H.; Niklason, L.E. Engineering biological-based vascular grafts using a pulsatile bioreactor. J. Vis. Exp. 2011. [Google Scholar] [CrossRef]
- Thompson, C.A.; Colon-Hernandez, P.; Pomerantseva, I.; MacNeil, B.D.; Nasseri, B.; Vacanti, J.P.; Oesterle, S.N. A novel pulsatile, laminar flow bioreactor for the development of tissue-engineered vascular structures. Tissue Eng. 2002, 8, 1083–1088. [Google Scholar]
- Massai, D.; Cerino, G.; Gallo, D.; Pennella, F.; Deriu, M.A.; Rodriguez, A.; Montevecchi, F.M.; Bignardi, C.; Audenino, A.; Morbiducci, U. Bioreactors as engineering support to treat cardiac muscle and vascular disease. J. Healthc. Eng. 2013, 4, 329–370. [Google Scholar] [CrossRef]
- Peterson, A.; Landeen, L.K.; Bennett, J.; Gee, G.; Chesla, S.; Zeltinger, J.; Flatt, J.H.; Applegate, M.A.; Dunkelman, N.; Kemmerrer, S. Aparatus and Method for Simulating in vivo Conditions While Seeding and Culturing Three-Dimensional Tissue Constructs. U.S. Patent 6,121,042, 19 September 2000. [Google Scholar]
- Syedain, Z.H.; Meier, L.A.; Bjork, J.W.; Lee, A.; Tranquillo, R.T. Implantable arterial grafts from human fibroblasts and fibrin using a multi-graft pulsed flow-stretch bioreactor with noninvasive strength monitoring. Biomaterials 2011, 32, 714–722. [Google Scholar]
- Hsu, S.H.; Tsai, I.J.; Lin, D.J.; Chen, D.C. The effect of dynamic culture conditions on endothelial cell seeding and retention on small diameter polyurethane vascular grafts. Med. Eng. Phys. 2005, 27, 267–272. [Google Scholar] [CrossRef]
- Akra, B.; Uhlig, A.; Haas, U.; Fano, C.; Dauner, M.; Lohse, P.; Gulbins, H.; Meiser, B.; Eissner, G.; Reichart, B.; et al. Perfusion Bioreactor: A New Pulsatile System for the Perfusion of Tissue Engineered Cardiovascular Prostheses. In World Congress on Medical Physics and Biomedical Engineering, September 7–12, 2009, Munich, Germany; Magjarevic, R., Ed.; Springer: Berlin, Germany, 2009; Volume 25/10, pp. 7–8. [Google Scholar]
- Peck, M.; Gebhart, D.; Dusserre, N.; McAllister, T.N.; L’Heureux, N. The Evolution of Vascular Tissue Engineering and Current State of the Art. Cells Tissues Org. 2012, 195, 144–158. [Google Scholar]
- Feugier, P.; Black, R.A.; Hunt, J.A.; How, T.V. Attachment, morphology and adherence of human endothelial cells to vascular prosthesis materials under the action of shear stress. Biomaterials 2005, 26, 1457–1466. [Google Scholar]
- Ballard, V.L.; Sharma, A.; Duignan, I.; Holm, J.M.; Chin, A.; Choi, R.; Hajjar, K.A.; Wong, S.C.; Edelberg, J.M. Vascular tenascin-C regulates cardiac endothelial phenotype and neovascularization. FASEB J. 2006, 20, 717–719. [Google Scholar]
- Corda, S.; Samuel, J.L.; Rappaport, L. Extracellular matrix and growth factors during heart growth. Heart Fail Rev. 2000, 5, 119–130. [Google Scholar] [CrossRef]
- Hallmann, R.; Horn, N.; Selg, M.; Wendler, O.; Pausch, F.; Sorokin, L.M. Expression and function of laminins in the embryonic and mature vasculature. Physiol. Rev. 2005, 85, 979–1000. [Google Scholar]
- Laflamme, K.; Roberge, C.J.; Grenier, G.; Remy-Zolghadri, M.; Pouliot, S.; Baker, K.; Labbe, R.; D’Orleans-Juste, P.; Auger, F.A.; Germain, L. Adventitia contribution in vascular tone: Insights from adventitia-derived cells in a tissue-engineered human blood vessel. FASEB J. 2006, 20, 1245–1247. [Google Scholar] [CrossRef]
- Buttafoco, L.; Boks, N.P.; Engbers-Buijtenhuijs, P.; Grijpma, D.W.; Poot, A.A.; Dijkstra, P.J.; Vermes, I.; Feijen, J. Porous hybrid structures based on P(DLLA-co-TMC) and collagen for tissue engineering of small-diameter blood vessels. J. Biomed. Mater. Res. Part B 2006, 79, 425–434. [Google Scholar]
- Newman, P.J. The role of PECAM-1 in vascular cell biology. Ann. N. Y. Acad. Sci. 1994, 714, 165–174. [Google Scholar] [CrossRef]
- McIlhenny, S.E.; Hager, E.S.; Grabo, D.J.; DiMatteo, C.; Shapiro, I.M.; Tulenko, T.N.; DiMuzio, P.J. Linear shear conditioning improves vascular graft retention of adipose-derived stem cells by upregulation of the α5β1 integrin. Tissue Eng. Part A 2010, 16, 245–255. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Schulte, J.; Friedrich, A.; Hollweck, T.; König, F.; Eblenkamp, M.; Beiras-Fernandez, A.; Fano, C.; Hagl, C.; Akra, B. A Novel Seeding and Conditioning Bioreactor for Vascular Tissue Engineering. Processes 2014, 2, 526-547. https://doi.org/10.3390/pr2030526
Schulte J, Friedrich A, Hollweck T, König F, Eblenkamp M, Beiras-Fernandez A, Fano C, Hagl C, Akra B. A Novel Seeding and Conditioning Bioreactor for Vascular Tissue Engineering. Processes. 2014; 2(3):526-547. https://doi.org/10.3390/pr2030526
Chicago/Turabian StyleSchulte, Julia, Anja Friedrich, Trixi Hollweck, Fabian König, Markus Eblenkamp, Andres Beiras-Fernandez, Cornelia Fano, Christian Hagl, and Bassil Akra. 2014. "A Novel Seeding and Conditioning Bioreactor for Vascular Tissue Engineering" Processes 2, no. 3: 526-547. https://doi.org/10.3390/pr2030526
APA StyleSchulte, J., Friedrich, A., Hollweck, T., König, F., Eblenkamp, M., Beiras-Fernandez, A., Fano, C., Hagl, C., & Akra, B. (2014). A Novel Seeding and Conditioning Bioreactor for Vascular Tissue Engineering. Processes, 2(3), 526-547. https://doi.org/10.3390/pr2030526




