The Importance of Drug Delivery in the Clinical Development and Lifecycle of Drug Products with Examples from Authorised Medicinal Products
Abstract
:1. Introduction
- i.
- Inability to develop an appropriate DDS/formulation fit for the intended purpose of the drug product could be a reason for attrition of a new chemical entity (NCE) in drug development.
- ii.
- Advances in formulation strategies related to the enhancement of solubility, permeability and thus bioavailability of drugs have been successfully used by the pharmaceutical industry to reduce attrition due to the poor PK and erratic bioavailability of NCEs.
- iii.
- Focus should be given on the development of formulations/DDS that could improve the efficacy and safety of NCEs and currently approved APIs. Such formulations could improve the benefit–risk ratio of drugs facilitating their clinical development and could also be used to re-purpose already established medicines.
2. Drug Formulations to Deliver the Drug to the Site of Action
3. Drug Formulations to Enhance Patient Adherence to Medication
4. Drug Formulations to Improve Safety
5. Drug Formulations to Improve Efficacy
6. Conclusions
Funding
Conflicts of Interest
References
- Bruschi, M.L. Strategies to Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Cambridge, UK, 2015; pp. 15–28. [Google Scholar]
- Wen, H.; Jung, H.; Li, X. Drug Delivery Approaches in Addressing Clinical Pharmacology-Related Issues: Opportunities and Challenges. AAPS J. 2015, 17, 1327–1340. [Google Scholar] [CrossRef]
- Vargason, A.M.; Anselmo, A.C.; Mitragotri, S. The Evolution of Commercial Drug Delivery Technologies. Nat. Biomed. Eng. 2021, 5, 951–967. [Google Scholar] [CrossRef] [PubMed]
- Makurvet, F.D. Biologics vs. Small Molecules: Drug Costs and Patient Access. Med. Drug Discov. 2021, 9, 100075. [Google Scholar]
- De la Torre, B.G.; Albericio, F. The Pharmaceutical Industry in 2021. An Analysis of FDA Drug Approvals from the Perspective of Molecules. Molecules 2022, 27, 1075. [Google Scholar]
- Ngo, H.X.; Garneau-Tsodikova, S. What Are the Drugs of the Future? Med. Chem. Commun. 2018, 9, 757–758. [Google Scholar] [CrossRef] [PubMed]
- Kola, I.; Landis, J. Can the Pharmaceutical Industry Reduce Attrition Rates? Nat. Rev. Drug Discov. 2004, 3, 711–716. [Google Scholar] [CrossRef]
- Sun, D.; Gao, W.; Hu, H.; Zhou, S. Why 90% of Clinical Drug Development Fails and How to Improve It? Acta Pharm. Sin. B 2022, 12, 3049–3062. [Google Scholar] [CrossRef]
- Dowden, H.; Munro, J. Trends in Clinical Success Rates and Therapeutic Focus. Nat. Rev. Drug Discov. 2019, 18, 495–496. [Google Scholar] [CrossRef]
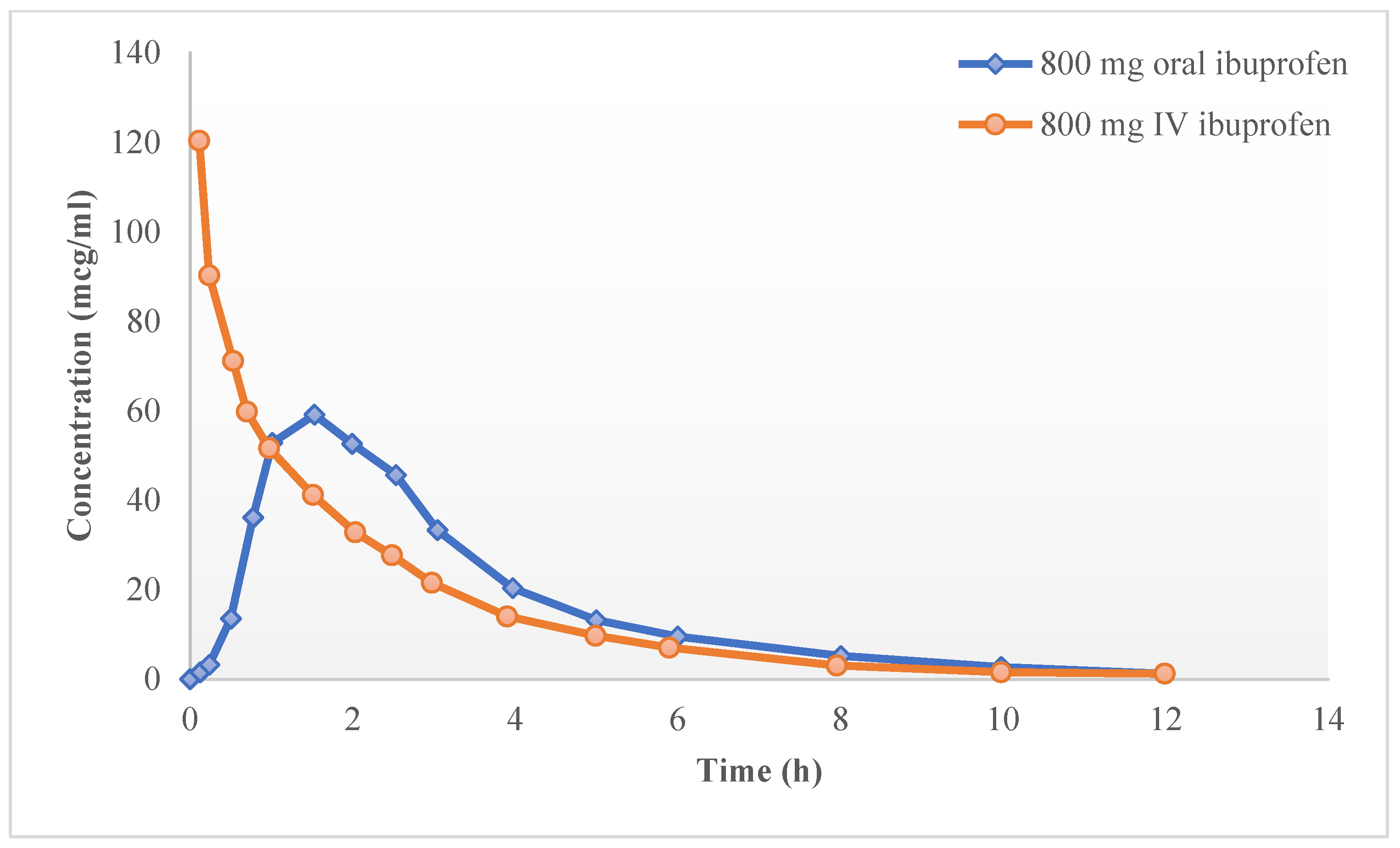
- Pavliv, L.; Voss, B.; Rock, A. Pharmacokinetics, Safety, and Tolerability of a Rapid Infusion of i.v. Ibuprofen in Healthy Adults. Am. J. Health-Syst. Pharm. 2011, 68, 47–51. [Google Scholar] [CrossRef]
- Labiris, N.R.; Dolovich, M.B. Pulmonary Drug Delivery. Part I: Physiological Factors Affecting Therapeutic Effectiveness of Aerosolized Medications. Br. J. Clin. Pharmacol. 2003, 56, 588–599. [Google Scholar]
- Arikayce Liposomal 590 mg Nebuliser Dispersion—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/12067/smpc (accessed on 9 July 2023).
- Cayston 75 mg Powder and Solvent for Nebuliser Solution—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/4456/smpc (accessed on 28 September 2023).
- Colobreathe 1,662,500 IU Inhalation Powder, Hard Capsules—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/3063/smpc (accessed on 28 September 2023).
- Promixin 1 Million International Units (IU) Powder for Nebuliser Solution—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/4/smpc (accessed on 28 September 2023).
- Quinsair 240 mg Nebuliser Solution—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/7202/smpc (accessed on 28 September 2023).
- Tobi 300 mg/5 mL Nebuliser Solution—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/262/smpc (accessed on 28 September 2023).
- Tobi Podhaler 28 mg Inhalation Powder, Hard Capsules—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/4757/smpc (accessed on 28 September 2023).
- Amikacin 250 mg/mL Injection—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/3784/smpc (accessed on 9 July 2023).
- Johnson, M.M.; Odell, J.A. Nontuberculous Mycobacterial Pulmonary Infections. J. Thorac. Dis. 2014, 6, 210–220. [Google Scholar] [PubMed]
- Li, Z.; Perkins, W.; Cipolla, D. Robustness of Aerosol Delivery of Amikacin Liposome Inhalation Suspension Using the eFlow® Technology. Eur. J. Pharm. Biopharm. 2021, 166, 10–18. [Google Scholar] [CrossRef]
- Zhang, J.; Leifer, F.; Rose, S.; Chun, D.Y.; Thaisz, J.; Herr, T.; Nashed, M.; Joseph, J.; Perkins, W.R.; DiPetrillo, K. Amikacin Liposome Inhalation Suspension (ALIS) Penetrates Non-Tuberculous Mycobacterial Biofilms and Enhances Amikacin Uptake Into Macrophages. Front. Microbiol. 2018, 9, 915. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M. Amikacin Liposome Inhalation Suspension: A Review in Mycobacterium Avium Complex Lung Disease. Drugs 2019, 79, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Gänger, S.; Schindowski, K. Tailoring Formulations for Intranasal Nose-to-Brain Delivery: A Review on Architecture, Physico-Chemical Characteristics and Mucociliary Clearance of the Nasal Olfactory Mucosa. Pharmaceutics 2018, 10, 116. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.P.; Moreira, J.N.; Sousa Lobo, J.M.; Silva, A.C. Intranasal Delivery of Nanostructured Lipid Carriers, Solid Lipid Nanoparticles and Nanoemulsions: A Current Overview of in Vivo Studies. Acta Pharm. Sin. B 2021, 11, 925–940. [Google Scholar] [CrossRef]
- SPRAVATO® (Esketamine). Available online: https://www.spravato.com/ (accessed on 9 July 2023).
- Swainson, J.; Thomas, R.K.; Archer, S.; Chrenek, C.; MacKay, M.-A.; Baker, G.; Dursun, S.; Klassen, L.J.; Chokka, P.; Demas, M.L. Esketamine for Treatment Resistant Depression. Expert Rev. Neurother. 2019, 19, 899–911. [Google Scholar] [CrossRef] [PubMed]
- Kasper, S.; Cubała, W.J.; Fagiolini, A.; Ramos-Quiroga, J.A.; Souery, D.; Young, A.H. Practical Recommendations for the Management of Treatment-Resistant Depression with Esketamine Nasal Spray Therapy: Basic Science, Evidence-Based Knowledge and Expert Guidance. World J. Biol. Psychiatry 2021, 22, 468–482. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- National Institute for Health and Care Excellence. Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence; National Institute for Health and Care Excellence: Manchester, UK, 2009. [Google Scholar]
- Stentzel, U.; van den Berg, N.; Schulze, L.N.; Schwaneberg, T.; Radicke, F.; Langosch, J.M.; Freyberger, H.J.; Hoffmann, W.; Grabe, H.-J. Predictors of Medication Adherence among Patients with Severe Psychiatric Disorders: Findings from the Baseline Assessment of a Randomized Controlled Trial (Tecla). BMC Psychiatry 2018, 18, 155. [Google Scholar] [CrossRef]
- Baryakova, T.H.; Pogostin, B.H.; Langer, R.; McHugh, K.J. Overcoming Barriers to Patient Adherence: The Case for Developing Innovative Drug Delivery Systems. Nat. Rev. Drug Discov. 2023, 22, 387–409. [Google Scholar] [CrossRef]
- Wilkinson, J.; Ajulo, D.; Tamburrini, V.; Gall, G.L.; Kimpe, K.; Holm, R.; Belton, P.; Qi, S. Lipid Based Intramuscular Long-Acting Injectables: Current State of the Art. Eur. J. Pharm. Sci. 2022, 178, 106253. [Google Scholar] [CrossRef]
- Correll, C.U.; Kim, E.; Sliwa, J.K.; Hamm, W.; Gopal, S.; Mathews, M.; Venkatasubramanian, R.; Saklad, S.R. Pharmacokinetic Characteristics of Long-Acting Injectable Antipsychotics for Schizophrenia: An Overview. CNS Drugs 2021, 35, 39–59. [Google Scholar] [CrossRef]
- Invega 3 mg Prolonged-Release Tablets—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/6816/smpc#gref (accessed on 9 July 2023).
- Xeplion 100 mg Prolonged-Release Suspension for Injection—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/7653/smpc#gref (accessed on 9 July 2023).
- TREVICTA 175 mg Prolonged Release Suspension for Injection—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/7230/smpc#gref (accessed on 9 July 2023).
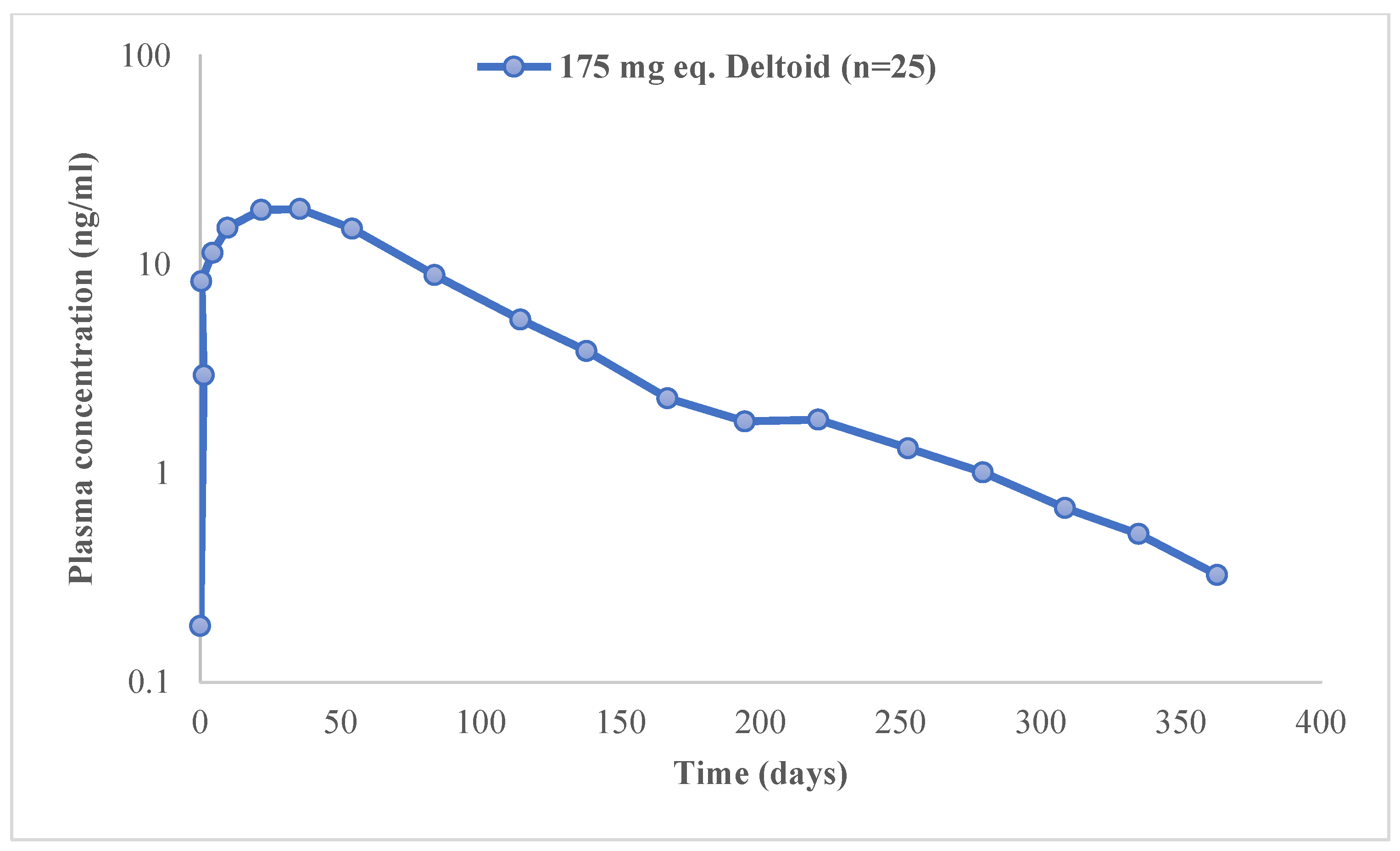
- Ravenstijn, P.; Remmerie, B.; Savitz, A.; Samtani, M.N.; Nuamah, I.; Chang, C.-T.; De Meulder, M.; Hough, D.; Gopal, S. Pharmacokinetics, Safety, and Tolerability of Paliperidone Palmitate 3-Month Formulation in Patients with Schizophrenia: A Phase-1, Single-Dose, Randomized, Open-Label Study. J. Clin. Pharmacol. 2016, 56, 330–339. [Google Scholar] [CrossRef]
- Mathews, M.; Gopal, S.; Singh, A.; Nuamah, I.; Pungor, K.; Tan, W.; Soares, B.; Kim, E.; Savitz, A.J. Comparison of Relapse Prevention with 3 Different Paliperidone Formulations in Patients with Schizophrenia Continuing versus Discontinuing Active Antipsychotic Treatment: A Post-hoc Analysis of 3 Similarly Designed Randomized Studies. Neuropsychiatr. Dis. Treat. 2020, 16, 1533–1542. [Google Scholar] [CrossRef]
- Lin, D.; Thompson-Leduc, P.; Ghelerter, I.; Nguyen, H.; Lafeuille, M.-H.; Benson, C.; Mavros, P.; Lefebvre, P. Real-World Evidence of the Clinical and Economic Impact of Long-Acting Injectable Versus Oral Antipsychotics Among Patients with Schizophrenia in the United States: A Systematic Review and Meta-Analysis. CNS Drugs 2021, 35, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.; Yan, T.; Chang, E.; Hartry, A.; Touya, M.; Broder, M.S. Medication Adherence and Discontinuation of Long-Acting Injectable versus Oral Antipsychotics in Patients with Schizophrenia or Bipolar Disorder. J. Med. Econ. 2018, 21, 127–134. [Google Scholar] [CrossRef]
- Kim, H.O.; Seo, G.H.; Lee, B.C. Real-World Effectiveness of Long-Acting Injections for Reducing Recurrent Hospitalizations in Patients with Schizophrenia. Ann. Gen. Psychiatry 2020, 19, 1. [Google Scholar] [CrossRef] [PubMed]
- O’ Rourke, G.; O’ Brien, J.J. Identifying the Barriers to Antiepileptic Drug Adherence among Adults with Epilepsy. Seizure 2017, 45, 160–168. [Google Scholar] [CrossRef]
- Eatock, J.; Baker, G.A. Managing Patient Adherence and Quality of Life in Epilepsy. Neuropsychiatr. Dis. Treat. 2007, 3, 117–131. [Google Scholar] [CrossRef]
- Al-Aqeel, S.; Gershuni, O.; Al-Sabhan, J.; Hiligsmann, M. Strategies for Improving Adherence to Antiepileptic Drug Treatment in People with Epilepsy. Cochrane Database Syst. Rev. 2020, 10, CD008312. [Google Scholar] [CrossRef] [PubMed]
- Plessinger, D.; Ryan, M.; Gache, L.; Gunnarsson, C.; Faugh, E. Estimating the Incremental Burden of Dysphagia in Epilepsy Patients: A Retrospective Payer Database Analysis. Presented at the 2016 American Epilepsy Society Annual Meeting, Houston TX, USA, 2–6 December 2016. [Google Scholar]
- Liu, F.; Ranmal, S.; Batchelor, H.K.; Orlu-Gul, M.; Ernest, T.B.; Thomas, I.W.; Flanagan, T.; Tuleu, C. Patient-Centered Pharmaceutical Design to Improve Acceptability of Medicines: Similarities and Differences in Paediatric and Geriatric Populations. Drugs 2014, 74, 1871–1889. [Google Scholar] [CrossRef]
- Hanning, S.M.; Lopez, F.L.; Wong, I.C.K.; Ernest, T.B.; Tuleu, C.; Orlu Gul, M. Patient Centric Formulations for Paediatrics and Geriatrics: Similarities and Differences. Int. J. Pharm. 2016, 512, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Lee, J.-J.; Kim, M.-G.; Kim, K.-T.; Cho, C.-W.; Kim, D.-D.; Lee, J.-Y. Sprinkle Formulations—A Review of Commercially Available Products. Asian J. Pharm. Sci. 2020, 15, 292–310. [Google Scholar] [CrossRef] [PubMed]
- Keppra 250 mg Film-Coated Tablets—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/2294/smpc (accessed on 15 September 2023).
- Silva, R.; Bicker, J.; Almeida, A.; Carona, A.; Silva, A.; Sales, F.; Santana, I.; Falcão, A.; Fortuna, A. Clinical Application of Pharmacokinetics to Appraise Adherence to Levetiracetam in Portuguese Epileptic Patients. Biomedicines 2022, 10, 2127. [Google Scholar] [CrossRef]
- FDA Approves the First 3D Printed Drug Product. Available online: https://www.aprecia.com/news/fda-approves-the-first-3d-printed-drug-product (accessed on 15 September 2023).
- ZipDose Technology. Available online: https://www.aprecia.com/technology/zipdose (accessed on 15 September 2023).
- Senapati, S.; Mahanta, A.K.; Kumar, S.; Maiti, P. Controlled Drug Delivery Vehicles for Cancer Treatment and Their Performance. Sig. Transduct. Target Ther. 2018, 3, 7. [Google Scholar] [CrossRef]
- Doxorubicin Solution for Injection—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/6184/smpc#gref (accessed on 9 July 2023).
- Thorn, C.F.; Oshiro, C.; Marsh, S.; Hernandez-Boussard, T.; McLeod, H.; Klein, T.E.; Altman, R.B. Doxorubicin Pathways: Pharmacodynamics and Adverse Effects. Pharmacogenet. Genom. 2011, 21, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, D.; Iacopo, F.; Cipolla, C.M. Cardiotoxicity of Anthracyclines. Front. Cardiovasc. Med. 2020, 7, 26. [Google Scholar] [CrossRef]
- Gabizon, A.; Martin, F. Polyethylene Glycol-Coated (Pegylated) Liposomal Doxorubicin—Rationale for Use in Solid Tumours. Drugs 1997, 54 (Suppl. S4), 15–21. [Google Scholar] [CrossRef] [PubMed]
- Gabizon, A.; Shmeeda, H.; Barenholz, Y. Pharmacokinetics of Pegylated Liposomal Doxorubicin: Review of Animal and Human Studies. Clin. Pharmacokinet. 2003, 42, 419–436. [Google Scholar] [CrossRef]
- Caelyx Pegylated Liposomal 2 mg/mL Concentrate for Solution for Infusion—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/12931/smpc#gref (accessed on 9 July 2023).
- Yildirim, Y.; Gultekin, E.; Avci, M.E.; Inal, M.M.; Yunus, S.; Tinar, S. Cardiac Safety Profile of Pegylated Liposomal Doxorubicin Reaching or Exceeding Lifetime Cumulative Doses of 550 mg/m2 in Patients with Recurrent Ovarian and Peritoneal Cancer. Int. J. Gynecol. Cancer 2008, 18, 223–227. [Google Scholar] [CrossRef]
- Gabizon, A.A.; Lyass, O.; Berry, G.J.; Wildgust, M. Cardiac Safety of Pegylated Liposomal Doxorubicin (Doxil/Caelyx) Demonstrated by Endomyocardial Biopsy in Patients with Advanced Malignancies. Cancer Investig. 2004, 22, 663–669. [Google Scholar] [CrossRef]
- O’Brien, M.E.R.; Wigler, N.; Inbar, M.; Rosso, R.; Grischke, E.; Santoro, A.; Catane, R.; Kieback, D.G.; Tomczak, P.; Ackland, S.P.; et al. Reduced Cardiotoxicity and Comparable Efficacy in a Phase III Trial of Pegylated Liposomal Doxorubicin HCl (CAELYX/Doxil) versus Conventional Doxorubicin for First-Line Treatment of Metastatic Breast Cancer. Ann. Oncol. 2004, 15, 440–449. [Google Scholar] [CrossRef]
- Hornberger, J.; Chhatwal, J. Opioid Misuse: A Global Crisis. Value Health 2021, 24, 145–146. [Google Scholar] [CrossRef]
- Alenezi, A.; Yahyouche, A.; Paudyal, V. Current Status of Opioid Epidemic in the United Kingdom and Strategies for Treatment Optimisation in Chronic Pain. Int. J. Clin. Pharm. 2021, 43, 318–322. [Google Scholar] [CrossRef]
- Iwanicki, J.L.; Severtson, S.G.; McDaniel, H.; Rosenblum, A.; Fong, C.; Cicero, T.J.; Ellis, M.S.; Kurtz, S.P.; Buttram, M.E.; Dart, R.C. Abuse and Diversion of Immediate Release Opioid Analgesics as Compared to Extended Release Formulations in the United States. PLoS ONE 2016, 11, e0167499. [Google Scholar] [CrossRef]
- Geoffrey Severtson, S.; Kreider, S.E.D.; Amioka, E.C.; Margolin, Z.R.; Iwanicki, J.L.; Dart, R.C. Postmarketing Analysis of Misuse, Abuse, and Diversion of Xtampza ER. Pain Med. 2020, 21, 3660–3668. [Google Scholar] [CrossRef]
- Argoff, C.E.; Kopecky, E.A. Patients with Chronic Pain and Dysphagia (CPD): Unmet Medical Needs and Pharmacologic Treatment Options. Curr. Med. Res. Opin. 2014, 30, 2543–2559. [Google Scholar] [CrossRef] [PubMed]
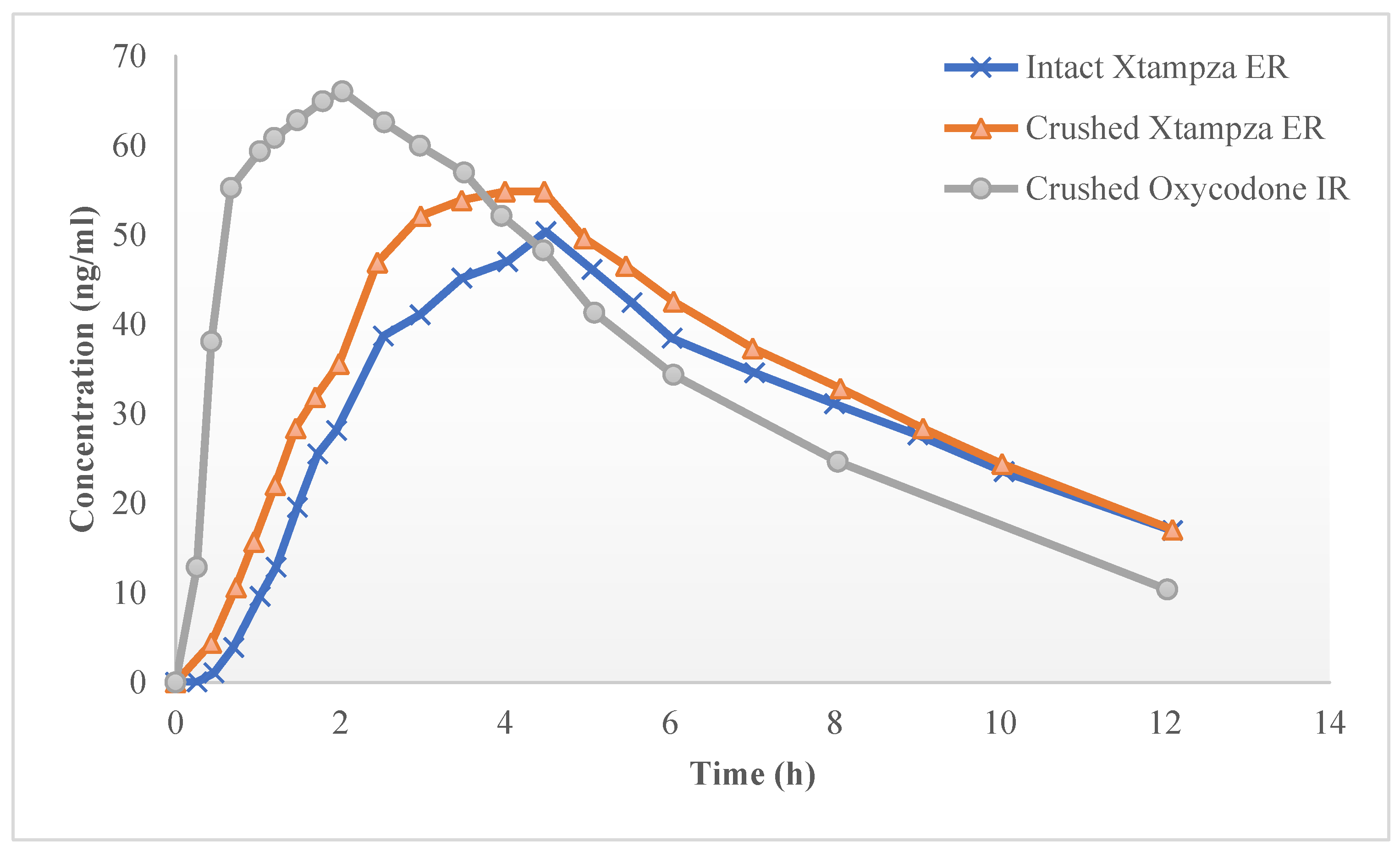
- Gudin, J. Effect of Physical Manipulation on the Oral Pharmacokinetic Profile of Xtampza® ER (Oxycodone DETERx® Formulation): A Review of Published Studies. J. Opioid Manag. 2020, 16, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.J.; Kopecky, E.A.; Marseilles, A.; O’Connor, M.; Fleming, A.B. The Comparative Pharmacokinetics of Physical Manipulation by Crushing of Xtampza® ER Compared with OxyContin®. Pain Manag. 2017, 7, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Webster, L.R.; Kopecky, E.A.; Smith, M.D.; Fleming, A.B. A Randomized, Double-Blind, Double-Dummy Study to Evaluate the Intranasal Human Abuse Potential and Pharmacokinetics of a Novel Extended-Release Abuse-Deterrent Formulation of Oxycodone. Pain Med. 2016, 17, 1112–1130. [Google Scholar] [CrossRef] [PubMed]
- Becker, W.C.; Fiellin, D.A. Abuse-Deterrent Opioid Formulations—Putting the Potential Benefits into Perspective. N. Engl. J. Med. 2017, 376, 2103–2105. [Google Scholar] [CrossRef] [PubMed]
- Abuse-Deterrent Opioid Analgesics. Available online: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/abuse-deterrent-opioid-analgesics (accessed on 29 September 2023).
- Paclitaxel 6 mg/mL Concentrate for Solution for Infusion—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/10076/smpc#gref (accessed on 9 July 2023).
- Sharma, U.S.; Balasubramanian, S.V.; Straubinger, R.M. Pharmaceutical and Physical Properties of Paclitaxel (Taxol) Complexes with Cyclodextrins. J. Pharm. Sci. 1995, 84, 1223–1230. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Aditya, K. Paclitaxel Hypersensitivity. Cancer Res. Stat. Treat. 2020, 3, 419. [Google Scholar] [CrossRef]
- Miele, E.; Spinelli, G.P.; Miele, E.; Tomao, F.; Tomao, S. Albumin-Bound Formulation of Paclitaxel (Abraxane ABI-007) in the Treatment of Breast Cancer. Int. J. Nanomed. 2009, 4, 99–105. [Google Scholar]
- Hama, M.; Ishima, Y.; Chuang, V.T.G.; Ando, H.; Shimizu, T.; Ishida, T. Evidence for Delivery of Abraxane via a Denatured-Albumin Transport System. ACS Appl. Mater Interfaces 2021, 13, 19736–19744. [Google Scholar] [CrossRef]
- Kratz, F. Albumin as a Drug Carrier: Design of Prodrugs, Drug Conjugates and Nanoparticles. J. Control Release 2008, 132, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Abraxane 5 mg/mL Powder for Dispersion for Infusion—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/6438/smpc#gref (accessed on 9 July 2023).
- Desai, N.; Trieu, V.; Yao, Z.; Louie, L.; Ci, S.; Yang, A.; Tao, C.; De, T.; Beals, B.; Dykes, D.; et al. Increased Antitumor Activity, Intratumor Paclitaxel Concentrations, and Endothelial Cell Transport of Cremophor-Free, Albumin-Bound Paclitaxel, ABI-007, Compared with Cremophor-Based Paclitaxel. Clin. Cancer Res. 2006, 12, 1317–1324. [Google Scholar] [CrossRef]
- Al Musaimi, O.; Al Shaer, D.; de la Torre, B.G.; Albericio, F. 2017 FDA Peptide Harvest. Pharmaceuticals 2018, 11, 42. [Google Scholar] [CrossRef]
- Ozempic 0.25 mg Solution for Injection in Pre-Filled Pen—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/9748/smpc (accessed on 20 September 2023).
- Maher, S.; Mrsny, R.J.; Brayden, D.J. Intestinal Permeation Enhancers for Oral Peptide Delivery. Adv. Drug Deliv. Rev. 2016, 106, 277–319. [Google Scholar] [CrossRef]
- Rybelsus 14 mg—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/14389 (accessed on 20 September 2023).
- Kim, J.C.; Park, E.J.; Na, D.H. Gastrointestinal Permeation Enhancers for the Development of Oral Peptide Pharmaceuticals. Pharmaceuticals 2022, 15, 1585. [Google Scholar] [CrossRef]
- Overgaard, R.V.; Navarria, A.; Ingwersen, S.H.; Bækdal, T.A.; Kildemoes, R.J. Clinical Pharmacokinetics of Oral Semaglutide: Analyses of Data from Clinical Pharmacology Trials. Clin. Pharmacokinet. 2021, 60, 1335–1348. [Google Scholar] [CrossRef] [PubMed]
- Aungst, B.J. Absorption Enhancers: Applications and Advances. AAPS J. 2012, 14, 10–18. [Google Scholar] [CrossRef] [PubMed]

| Antibiotic | Approved Indications | References |
|---|---|---|
| Amikacin (Arikayce®) | Treatment of non-tuberculous mycobacteria lung infections caused by Mycobacterium avium Complex in adults with limited treatment options who do not have cystic fibrosis | [12] |
| Aztreonam powder and solvent for nebuliser solution (Cayston®) | Therapy of chronic pulmonary infections due to P. aeruginosa in patients with cystic fibrosis aged 6 years and older | [13] |
| Colistimethate inhalation powder (Colobreathe®) | [14] | |
| Colistimethate powder for nebuliser solution (Promixin) | Management in adult and paediatric of chronic pulmonary infections due to P. aeruginosa in patients with cystic fibrosis | [15] |
| Levofloxacin nebuliser solution (Quinsair®) | Management of chronic pulmonary infections due to P. aeruginosa in adult patients with cystic fibrosis | [16] |
| Tobramycin nebuliser solution | Therapy of chronic pulmonary infections due to P. aeruginosa in patients with cystic fibrosis aged 6 years and older | [17] |
| Tobramycin inhalation powder (Tobi Podhaler®) | [18] |
| Formulation | Improved Acceptability | Examples |
|---|---|---|
| Fixed-dose combination | Reduction in complexity of treatment regimen and pill burden | Amlodipine/Valsartan tablets |
| Multiparticulates | Multi-unit systems of minitablets, pellets or granules that are filled into capsules or compressed into tablets. They can be swallowed as whole or may be sprinkled onto soft food. Good choice for the development of fixed-dose combination products | Pancreatin gastro-resistant granules |
| Orodispersible dosage forms | Rapid disintegration or dissolution in the oral cavity without the need for water. Ability to be administered to those with swallowing difficulties | Donepezil orodispersible tablets |
| Drug Product | Drug | Abuse-Deterrence Mechanism |
|---|---|---|
| OxyContinTM | Oxycodone | Upon dissolution, a viscous gel is formed that is difficult to inject through a hypodermic needle |
| HysinglaTM ER | Hydrocodone | |
| XtampzaTM ER | Oxycodone | Capsules containing microspheres formulated with oxycodone base and excipients that make the formulation harder to manipulate |
| RoxyBondTM | Contains excipients that make the tablet harder to misuse by physical manipulation and/or chemical extraction |
| Mechanism |
|---|
| Prevention of degradation/metabolism |
Enhancement of membrane permeability by:
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malamatari, M. The Importance of Drug Delivery in the Clinical Development and Lifecycle of Drug Products with Examples from Authorised Medicinal Products. Processes 2023, 11, 2919. https://doi.org/10.3390/pr11102919
Malamatari M. The Importance of Drug Delivery in the Clinical Development and Lifecycle of Drug Products with Examples from Authorised Medicinal Products. Processes. 2023; 11(10):2919. https://doi.org/10.3390/pr11102919
Chicago/Turabian StyleMalamatari, Maria. 2023. "The Importance of Drug Delivery in the Clinical Development and Lifecycle of Drug Products with Examples from Authorised Medicinal Products" Processes 11, no. 10: 2919. https://doi.org/10.3390/pr11102919
APA StyleMalamatari, M. (2023). The Importance of Drug Delivery in the Clinical Development and Lifecycle of Drug Products with Examples from Authorised Medicinal Products. Processes, 11(10), 2919. https://doi.org/10.3390/pr11102919





