Social Media Adoption by Health Professionals: A TAM-Based Study
Abstract
:1. Introduction
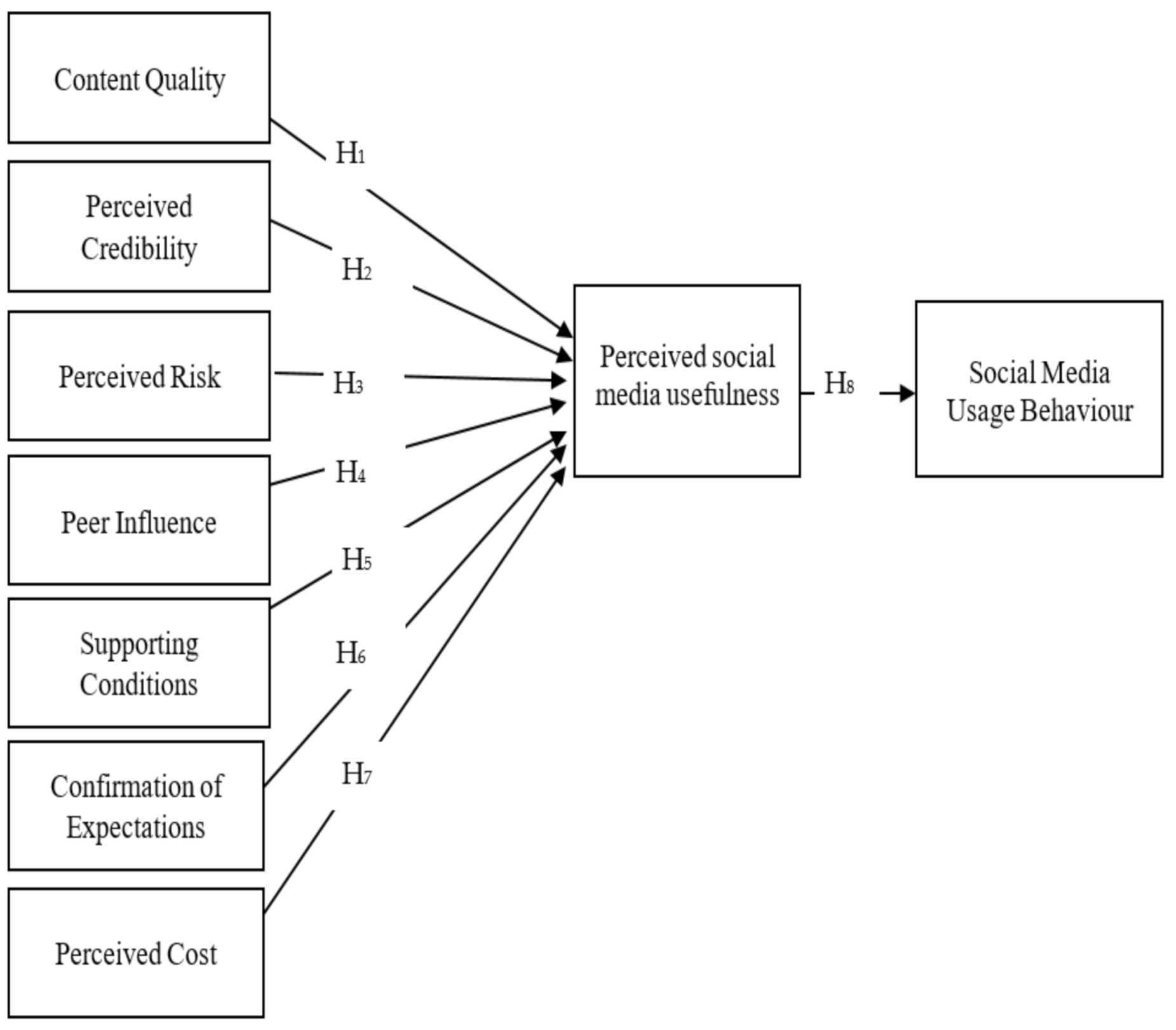
1.1. Theoretical Background and Research Model
1.2. Hypothesis Development
1.2.1. A. Content Quality
1.2.2. B. Perceived Credibility
1.2.3. C. Perceived Risk
1.2.4. D. Peer Influence
1.2.5. E. Supporting Conditions
1.2.6. F. Confirmation of Expectations
1.2.7. G. Perceived Cost
1.2.8. H. Perceived Usefulness and Usage Behaviour
2. Methods
2.1. Data Collection
2.2. Data Analysis
2.3. Construct Measures
2.4. The Demographic Profile
3. Results
Hypothesis Testing
4. Discussion
5. Conclusions and Implications
6. Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernández-Luque, L.; Bau, T. Health and social media: Perfect storm of information. Healthc. Inform. Res. 2015, 21, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Leary, V.G.; Grant, G. Social media in healthcare. In Proceedings of the 50th Hawaii International Conference on System Sciences, Puako, HI, USA, 4–7 January 2017. [Google Scholar]
- Park, A.; Bowling, J.; Shaw, G., Jr.; Li, C.; Chen, S. Adopting social media for improving health opportunities and challenges. North Carol. Med. J. 2019, 80, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Gabarron, E.; Bradway, M.; Fernandez-Luque, L.; Chomutare, T.; Hansen, A.H.; Wynn, R.; Årsand, E. Social media for health promotion in diabetes: Study protocol for a participatory public health intervention design. BMC Health Serv. Res. 2018, 18, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Barnes, S.S.; Kaul, V.; Kudchadkar, S.R. Social media engagement and the critical care medicine community. J. Intensive Care Med. 2019, 34, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Moorhead, S.A.; Hazlett, D.E.; Harrison, L.; Carroll, J.K.; Irwin, A.; Hoving, C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Internet Res. 2013, 15, 4. [Google Scholar] [CrossRef] [Green Version]
- Korda, H.; Itani, Z. Harnessing social media for health promotion and behavior change. Health Promot. Pract. 2013, 14, 15–23. [Google Scholar] [CrossRef]
- Sarasohn-Kahn, J. The Wisdom of Patients: Health Care Meets Online Social Media; California HealthCare Foundation: Oakland, CA, USA, 2008. [Google Scholar]
- Sarringhaus, M.M. The great divide: Social media’s role in bridging healthcare’s generational shift. J. Healthc. Manag. 2011, 56, 235–244. [Google Scholar]
- Fisher, J.; Clayton, M. Who gives a tweet: Assessing patients’ interest in the use of social media for health care. Worldviews Evid. Based Nurs. 2012, 9, 100–108. [Google Scholar] [CrossRef]
- Lambert, K.M.; Barry, P.; Stokes, G. Risk management and legal issues with the use of social media in the healthcare setting. J. Healthc. Risk Manag. 2012, 31, 41–47. [Google Scholar] [CrossRef]
- Andersen, K.N.; Medaglia, R.; Henriksen, H.Z. Social media in public health care: Impact domain propositions. Gov. Inf. Q. 2012, 29, 462–469. [Google Scholar] [CrossRef]
- Wicks, P.; Massagli, M.; Frost, J.; Brownstein, C.; Okun, S.; Vaughan, T.; Bradley, R.; Heywood, J. Sharing health data for better outcomes on PatientsLikeMe. J. Med. Internet Res. 2010, 12, e19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, A.R.; Tucker, C. Active social media management: The case of health care. Inf. Syst. Res. 2013, 24, 52–70. [Google Scholar] [CrossRef] [Green Version]
- Chretien, K.C.; Greysen, S.R.; Chretien, J.P.; Kind, T. Online posting of unprofessional content by medical students. JAMA 2009, 302, 1309–1315. [Google Scholar] [CrossRef] [Green Version]
- McKee, R. Ethical issues in using social media for health and health care research. Health Policy 2013, 110, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Grobler, C.; Dhai, A. Social media in the healthcare context: Ethical challenges and recommendations. S. Afr. J. Bioeth. Law 2016, 9, 22–25. [Google Scholar] [CrossRef]
- Sahin, I. Detailed review of Rogers’ diffusion of innovations theory and educational technology-related studies based on Rogers’ theory. Turk. Online J. Educ. Technol.-TOJET 2006, 5, 14–23. [Google Scholar]
- Antheunis, M.L.; Tates, K.; Nieboer, T.E. Patients’ and health professionals’ use of social media in health care: Motives, barriers and expectations. Patient Educ. Couns. 2013, 92, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Cuan-Baltazar, J.Y.; Muñoz-Perez, M.J.; Robledo-Vega, C.; Pérez-Zepeda, M.F.; Soto-Vega, E. Misinformation of COVID-19 on the internet: Infodemiology study. JMIR Public Health Surveill. 2020, 6, e18444. [Google Scholar] [CrossRef] [Green Version]
- Kasemsap, K. Professional and business applications of social media platforms. In Social Entrepreneurship: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2019; pp. 824–847. [Google Scholar]
- Kouzy, R.; Abi Jaoude, J.; Kraitem, A.; El Alam, M.B.; Karam, B.; Adib, E.; Zarka, J.; Traboulsi, C.; Akl, E.W.; Baddour, K. Coronavirus goes viral: Quantifying the COVID-19 misinformation epidemic on Twitter. Cureus 2020, 12, e7255. [Google Scholar] [CrossRef] [Green Version]
- Smailhodzic, E.; Hooijsma, W.; Boonstra, A.; Langley, D.J. Social media use in healthcare: A systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Serv. Res. 2016, 16, 442. [Google Scholar] [CrossRef] [Green Version]
- Kind, T.; Greysen, S.R.; Chretien, K.C. Pediatric clerkship directors’ social networking use and perceptions of online professionalism. Acad. Pediatrics 2012, 12, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Ryan, C.; Harris, A. How doctors view and use social media: A national survey. J. Med. Internet Res. 2014, 16, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Usher, W. Types of social media (Web 2.0) used by Australian allied health professionals to deliver early twenty-first-century practice promotion and health care. Social Work Health Care 2011, 50, 305–329. [Google Scholar] [CrossRef]
- McGowan, B.S.; Wasko, M.; Vartabedian, B.S.; Miller, R.S.; Freiherr, D.D.; Abdolrasulnia, M. Understanding the factors that influence the adoption and meaningful use of social media by physicians to share medical information. J. Med. Internet Res. 2012, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- Šumak, B.; Heričko, V.; PušNik, M. A meta-analysis of e-learning technology acceptance: The role of user types and e-learning technology types. Comput. Hum. Behav. 2011, 27, 2067–2077. [Google Scholar] [CrossRef]
- Scherer, R.; Siddiq, F.; Tondeur, J. The technology acceptance model (TAM): A meta-analytic structural equation modeling approach to explaining teachers’ adoption of digital technology in education. Comput. Educ. 2019, 128, 13–35. [Google Scholar] [CrossRef]
- Nadri, H.; Rahimi, B.; Lotfnezhad, A.H.; Samadbeik, M.; Garavand, A. Factors affecting acceptance of hospital information systems based on extended technology acceptance model: A case study in three paraclinical departments. Appl. Clin. Inform. 2018, 9, 238. [Google Scholar] [CrossRef] [Green Version]
- Palos-Sanchez, P.R.; Hernandez-Mogollon, J.M.; Campon-Cerro, A.M. The behavioral response to location-based services: An examination of the influence of social and environmental benefits, and privacy. Sustainability 2017, 9, 1988. [Google Scholar] [CrossRef] [Green Version]
- Ajzen, I.; Fishbein, M. Understanding Attitudes and Predicting Social Behavior; Pearson: London, UK, 1980. [Google Scholar]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef] [Green Version]
- Venkatesh, V.; Davis, F.D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef] [Green Version]
- Koh, C.E.; Prybutok, V.R.; Ryan, S.D.; Wu, Y. A model for mandatory use of software technologies: An integrative approach by applying multiple levels of abstraction of informing science. Inf. Sci. 2010, 13, 177–203. [Google Scholar]
- Yang, H.-D.; Yoo, Y. It’s all about attitude: Revisiting the technology acceptance model. Decis. Support Syst. 2004, 38, 19–31. [Google Scholar] [CrossRef]
- Abdullah, F.; Ward, R.; Ahmed, E. Investigating the influence of the most commonly used external variables of TAM on students’ Perceived Ease of Use (PEOU) and Perceived Usefulness (PU) of e-portfolios. Comput. Hum. Behav. 2016, 63, 75–90. [Google Scholar] [CrossRef]
- Kucukusta, D.; Law, R.; Besbes, A.; Legohérel, P. Re-examining perceived usefulness and ease of use in online booking. Int. J. Contemp. Hosp. Manag. 2015, 27, 185–198. [Google Scholar] [CrossRef]
- Ong, C.S.; Lai, J.Y.; Wang, Y.S. Factors affecting engineers’ acceptance of asynchronous e-learning systems in high-tech companies. Inform. Manag. 2004, 41, 795–804. [Google Scholar] [CrossRef]
- Chismar, W.G.; Wiley-Patton, S. Does the extended technology acceptance model apply to physicians. In Proceedings of the 36th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 6–9 January 2003. [Google Scholar]
- Lin, C.; Lin, I.-C.; Roan, J. Barriers to physicians’ adoption of healthcare information technology: An empirical study on multiple hospitals. J. Med. Syst. 2012, 36, 1965–1977. [Google Scholar] [CrossRef]
- Phang, C.W.; Li, Y.; Sutanto, J.; Kankanhalli, A. Senior citizens’ adoption of e-government: In quest of the antecedents of perceived usefulness. In Proceedings of the 38th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 6 January 2005; p. 130a. [Google Scholar]
- Davis, F.D. User acceptance of information technology: System characteristics, user perceptions and behavioral impacts. Int. J. Man Mach. Stud. 1993, 38, 475–487. [Google Scholar] [CrossRef] [Green Version]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [Green Version]
- Holden, R.J.; Karsh, B.-T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [Green Version]
- Delone, W.H.; McLean, E.R. The DeLone and McLean model of information systems success: A ten-year update. J. Manag. Inf. Syst. 2003, 19, 9–30. [Google Scholar]
- DeLone, W.H.; McLean, E.R. Information systems success: The quest for the dependent variable. Inf. Syst. Res. 1992, 3, 60–95. [Google Scholar] [CrossRef]
- Al-Gahtani, S.S. Modeling the electronic transactions acceptance using an extended technology acceptance model. Appl. Comput. Inform. 2011, 9, 47–77. [Google Scholar] [CrossRef] [Green Version]
- Lopez, D.; Blobel, B.; Gonzalez, C. Information quality in healthcare social media—An architectural approach. Health Technol. 2016, 6, 17–25. [Google Scholar] [CrossRef]
- Gutierrez, N.; Kindratt, T.B.; Pagels, P.; Foster, B.; Gimpel, N.E. Health literacy, health information seeking behaviors and internet use among patients attending a private and public clinic in the same geographic area. J. Community Health 2014, 39, 83–89. [Google Scholar] [CrossRef]
- Mohammadi, F.; Abrizah, A.; Nazari, M. Is the information fit for use? Exploring teachers perceived information quality indicators for Farsi web-based learning resources. Malays. J. Libr. Inf. Sci. 2017, 20, 1. [Google Scholar]
- Alsabawy, A.Y.; Cater-Steel, A.; Soar, J. Soar. Determinants of perceived usefulness of e-learning systems. Comput. Hum. Behav. 2016, 64, 843–858. [Google Scholar] [CrossRef]
- Considine, D.M. Social Media for Health Professionals—Benefits and Pitfalls. Available online: https://www.doctorportal.com.au/social-media-for-health-professionals-benefits-and-pitfalls/ (accessed on 17 March 2018).
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in online shopping: An integrated model. MIS Q. 2003, 27, 51–90. [Google Scholar] [CrossRef]
- Hou, J.; Shim, M. The role of provider–patient communication and trust in online sources in Internet use for health-related activities. J. Health Commun. 2010, 15, 186–199. [Google Scholar] [CrossRef]
- Bansal, G.; Gefen, D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis. Support Syst. 2010, 49, 138–150. [Google Scholar] [CrossRef]
- Van Der Velden, M.; El Emam, K. Not all my friends need to know: A qualitative study of teenage patients, privacy, and social media. J. Am. Med. Inform. Assoc. 2013, 20, 16–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, W.-Y.; Zhang, X.; Song, H.; Omori, K. Health information seeking in the Web 2.0 age: Trust in social media, uncertainty reduction, and self-disclosure. Comput. Hum. Behav. 2016, 56, 289–294. [Google Scholar] [CrossRef]
- Jacoby, J.; Kaplan, L.B. The components of perceived risk. In Proceedings of the Third Annual Conference of the Association for Consumer Research, Chicago, IL, USA, 3–5 November 1972. [Google Scholar]
- Stone, R.N.; Grønhaug, K. Perceived risk: Further considerations for the marketing discipline. Eur. J. Mark. 1993, 27, 39–50. [Google Scholar] [CrossRef]
- Mitra, K.; Reiss, M.C.; Capella, L.M. An examination of perceived risk, information search and behavioral intentions in search, experience and credence services. J. Serv. Mark. 1999, 13, 208–228. [Google Scholar] [CrossRef]
- Rahman, M.M.; Sloan, T. User adoption of mobile commerce in Bangladesh: Integrating perceived risk, perceived cost and personal awareness with TAM. Int. Technol. Manag. Rev. 2017, 6, 103–124. [Google Scholar] [CrossRef] [Green Version]
- Crane, G.M.; Gardner, J.M. Pathology image-sharing on social media: Recommendations for protecting privacy while motivating education. AMA J. Ethics 2016, 18, 817. [Google Scholar]
- Melnik, T. Avoiding violations of patient privacy with social media. J. Nurs. Regul. 2013, 3, 39–46. [Google Scholar] [CrossRef]
- Al-Muhtadi, J.; Shahzad, B.; Saleem, K.; Jameel, W.; Orgun, M.A. Cybersecurity and privacy issues for socially integrated mobile healthcare applications operating in a multi-cloud environment. Health Inform. J. 2019, 25, 315–329. [Google Scholar] [CrossRef]
- Hader, A.L.; Brown, E.D. LEGAL BRIEFS. Patient Privacy and Social Media. AANA J. 2010, 78, 270–274. [Google Scholar]
- Hawn, C. Take two aspirin and tweet me in the morning: How Twitter, Facebook, and other social media are reshaping health care. Health Aff. 2009, 28, 361–368. [Google Scholar] [CrossRef]
- Cain, J. Social media in health care: The case for organizational policy and employee education. Am. J. Health Syst. Pharm. 2011, 68, 1036–1040. [Google Scholar] [CrossRef] [PubMed]
- Lagu, T.; Kaufman, E.J.; Asch, D.A.; Armstrong, K. Content of weblogs written by health professionals. J. Gen. Intern. Med. 2008, 23, 1642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chretien, K.C.; Azar, J.; Kind, T. Physicians on twitter. JAMA 2011, 305, 566–568. [Google Scholar] [PubMed]
- Thompson, L.A.; Black, E.; Duff, W.P.; Black, N.P.; Saliba, H.; Dawson, K. Protected health information on social networking sites: Ethical and legal considerations. J. Med. Internet Res. 2011, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Farnan, J.M.; Snyder Sulmasy, L.; Worster, B.K.; Chaudhry, H.J.; Rhyne, J.A.; Arora, V.M.; American College of Physicians Ethics; Professionalism and Human Rights Committee, American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: Patient and public relationships: Policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann. Intern. Med. 2013, 158, 620–627. [Google Scholar] [CrossRef]
- Vanneste, D.; Vermeulen, B.; Declercq, A. Healthcare professionals’ acceptance of BelRAI, a web-based system enabling person-centred recording and data sharing across care settings with interRAI instruments: A UTAUT analysis. BMC Med. Inform. Decis. Mak. 2013, 13, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Panahi, S.; Watson, J.; Partridge, H. Social media and physicians: Exploring the benefits and challenges. Health Inform. J. 2016, 22, 99–112. [Google Scholar] [CrossRef] [Green Version]
- Martinasek, M.P.; Panzera, A.D.; Schneider, T.; Lindenberger, J.H.; Bryant, C.A.; McDermott, R.J.; Couluris, M. Benefits and barriers of pediatric healthcare providers toward using social media in asthma care. Am. J. Health Educ. 2011, 42, 213–221. [Google Scholar] [CrossRef]
- Vitak, J.; Ellison, N.B. There’sa network out there you might as well tap’: Exploring the benefits of and barriers to exchanging informational and support-based resources on Facebook. New Media Soc. 2013, 15, 243–259. [Google Scholar] [CrossRef]
- Kamal, S.; Ayesha, M.S.; Priyanka, K. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Surani, Z.; Hirani, R.; Elias, A.; Quisenberry, L.; Varon, J.; Surani, S.; Surani, S. Social media usage among health care providers. BMC Res. Notes 2017, 10, 654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murire, O.T.; Cilliers, L. Social media adoption among lecturers at a traditional university in Eastern Cape Province of South Africa. SA J. Inform. Manag. 2017, 19, 6. [Google Scholar] [CrossRef] [Green Version]
- Puspitasari, I.; Firdauzy, A. Characterizing consumer behavior in leveraging social media for e-patient and health-related activities. Int. J. Environ. Res. Public Health 2019, 16, 3348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peñarroja, V.; Sánchez, J.; Gamero, N.; Orengo, V.; Zornoza, A.M. The influence of organizational facilitating conditions and technology acceptance factors on the effectiveness of virtual communities of practice. Behav. Inf. Technol. 2019, 38, 845–857. [Google Scholar] [CrossRef]
- Brown, S.A.; Venkatesh, V.; Kuruzovich, J.; Massey, A.P. Expectation confirmation: An examination of three competing models. Organ. Behav. Hum. Decis. Process. 2008, 105, 52–66. [Google Scholar] [CrossRef] [Green Version]
- Wijaya, I.; Rai, A.; Hariguna, T. The impact of customer experience on customer behavior intention use in social media commerce, an extended expectation confirmation model: An empirical study. Manag. Sci. Lett. 2019, 12, 2009–2020. [Google Scholar] [CrossRef]
- Bhattacherjee, A. Understanding information systems continuance: An expectation-confirmation model. MIS Q. 2001, 351–370. [Google Scholar] [CrossRef]
- Hew, J.J.; Lee, V.H.; Ooi, K.B.; Lin, B. Mobile social commerce: The booster for brand loyalty? Comput. Hum. Behav. 2016, 59, 142–154. [Google Scholar] [CrossRef]
- Kim, B. An empirical investigation of mobile data service continuance: Incorporating the theory of planned behavior into the expectation–confirmation model. Expert Syst. Appl. 2010, 37, 7033–7039. [Google Scholar] [CrossRef]
- Hariguna, T.; Lai, M.T.; Hung, C.W.; Chen, S.C. Understanding information system quality on public e-government service intention: An empirical study. Int. J. Innov. Sustain. Dev. 2017, 11, 271–290. [Google Scholar] [CrossRef]
- Park, E. User acceptance of smart wearable devices: An expectation-confirmation model approach. Telemat. Inform. 2020, 47, 101318. [Google Scholar] [CrossRef]
- Chow, W.S.; Shi, S. Investigating students’ satisfaction and continuance intention toward e-learning: An Extension of the expectation–confirmation model. Procedia-Soc. Behav. Sci. 2014, 141, 1145–1149. [Google Scholar] [CrossRef] [Green Version]
- Wixom, B.H.; Todd, P.A. A theoretical integration of user satisfaction and technology acceptance. Inform. Syst. Res. 2005, 16, 85–102. [Google Scholar] [CrossRef]
- Chuttur, M.Y. Overview of the technology acceptance model: Origins, developments and future directions. Work. Pap. Inform. Syst. 2009, 37, 9–37. [Google Scholar]
- Kim, S.H. Moderating effects of job relevance and experience on mobile wireless technology acceptance: Adoption of a smartphone by individuals. Inf. Manag. 2008, 45, 387–393. [Google Scholar] [CrossRef]
- Roger, E. Diffusion of Innovations; The Free Press: New York, NY, USA, 1995. [Google Scholar]
- Pearson, A.; Suresh, T.; Chris, G. The role of e-service quality and information quality in creating perceived value: Antecedents to web site loyalty. Inf. Syst. Manag. 2012, 29, 201–215. [Google Scholar] [CrossRef]
- Sripalawat, J.; Thongmak, M.; Ngramyarn, A. M-banking in metropolitan Bangkok and a comparison with other countries. J. Comput. Inf. Syst. 2011, 51, 67–76. [Google Scholar]
- Yarbrough, A.K.; Smith, T.B. Technology acceptance among physicians: A new take on TAM. Med. Care Res. Rev. 2007, 64, 650–672. [Google Scholar] [CrossRef]
- Burton-Jones, A.; Straub, D.W., Jr. Reconceptualizing system usage: An approach and empirical test. Inf. Syst. Res. 2006, 17, 228–246. [Google Scholar] [CrossRef]
- Legris, P.; Ingham, J.; Collerette, P. Why do people use information technology? A critical review of the technology acceptance model. Inform. Manag. 2003, 40, 191–204. [Google Scholar] [CrossRef]
- Aluri, A.; Tucker, E. Social influence and technology acceptance: The use of personal social media as a career enhancement tool among college students. J. Hosp. Tour. Educ. 2015, 27, 48–59. [Google Scholar] [CrossRef]
- Westin, A.F. Privacy and freedom. Wash. Lee Law Rev. 1968, 25, 166. [Google Scholar]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Consumer acceptance and use of information technology: Extending the unified theory of acceptance and use of technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.C. Explaining and predicting users’ continuance intention toward e-learning: An extension of the expectation–confirmation model. Comput. Educ. 2010, 54, 506–516. [Google Scholar] [CrossRef]
- Wei, T.T.; Marthandan, G.; Chong, A.Y.L.; Ooi, K.B.; Arumugam, S. What drives Malaysian m-commerce adoption? An empirical analysis. Ind. Manag. Data Syst. 2009, 109, 370–388. [Google Scholar]
- Chang, I.-C.; Hwang, H.-G.; Hung, W.-F.; Li, Y.-C. Physicians’ acceptance of pharmacokinetics-based clinical decision support systems. Expert Syst. Appl. 2007, 33, 296–303. [Google Scholar] [CrossRef]
- Bryman, A.; Bell, E. Business Research Methods; Oxford University Press: New York, NY, USA, 2015. [Google Scholar]
- Ryan, G.W.; Bernard, H.R. Techniques to identify themes. Field Methods 2003, 15, 85–109. [Google Scholar] [CrossRef] [Green Version]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: London, UK, 2007. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis, 6th ed.; Pearson: London, UK, 2006. [Google Scholar]
- Reyes-Menendez, A.; Saura, J.R.; Palos-Sanchez, P.R.; Alvarez-Garcia, J. Understanding user behavioral intention to adopt a search engine that promotes sustainable water management. Symmetry 2018, 10, 584. [Google Scholar] [CrossRef] [Green Version]
- Chin, W.W.; Todd, P.A. On the use, usefulness, and ease of use of structural equation modeling in MIS research: A note of caution. MIS Q. 1995, 19, 237–246. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming (Multivariate Applications Series); Taylor and Francis: Oxfordshire, UK, 2010; Volume 396, p. 7384. [Google Scholar]
- Cummins, R.A.; Gullone, E. Why we should not use 5-point Likert scales: The case for subjective quality of life measurement. Proc. Second. Int. Conf. Qual. Life Cities 2000, 74, 93. [Google Scholar]
- Finstad, K. Response interpolation and scale sensitivity: Evidence against 5-point scales. J. Usability Stud. 2010, 5, 104–110. [Google Scholar]
- Featherman, M.S.; Pavlou, P.A. Predicting e-services adoption: A perceived risk facets perspective. Int. J. Hum.-Comput. Stud. 2003, 59, 451–474. [Google Scholar] [CrossRef] [Green Version]
- Duyck, P.; Pynoo, B.; Devolder, P.; Voet, T.; Adang, L.; Vercruysse, J. User acceptance of a picture archiving and communication system. Methods Inf. Med. 2008, 47, 149–156. [Google Scholar] [PubMed]
- Bhattacherjee, A.; Hikmet, N. Physicians’ resistance toward healthcare information technology: A theoretical model and empirical test. Eur. J. Inf. Syst. 2007, 16, 725–737. [Google Scholar] [CrossRef]
- De Kerviler, G.; Demoulin, N.T.; Zidda, P. Adoption of in-store mobile payment: Are perceived risk and convenience the only drivers? J. Retail. Consum. Serv. 2016, 31, 334–344. [Google Scholar] [CrossRef]
- Chau, P.Y.; Hu, P.J.-H. Investigating healthcare professionals’ decisions to accept telemedicine technology: An empirical test of competing theories. Inf. Manag. 2002, 39, 297–311. [Google Scholar] [CrossRef]
- Hair, J.F. Research Methods for Business; John Wiley & Sons: Hoboken, NJ, USA, 2007. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural equation modeling: Perspectives on the present and the future. Int. J. Test. 2001, 1, 327–334. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. J. Econom. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Machdar, N.M. The effect of information quality on Perceived usefulness and ease of ose. Bus. Entrep. Rev. 2019, 15, 131–146. [Google Scholar]
- Saeed, K.A.; Abdinnour-Helm, S. Examining the effects of information system characteristics and perceived usefulness on post adoption usage of information systems. Inf. Manag. Decis. 2008, 45, 376–386. [Google Scholar] [CrossRef]
- Fuller, M.A.; Serva, M.A.; Baroudi, J. Clarifying the integration of trust and TAM in e-commerce environments: Implications for systems design and management. IEEE Trans. Eng. Manag. 2010, 57, 380–393. [Google Scholar]
- Chaouali, W.; Yahia, I.B.; Souiden, N. The interplay of counter-conformity motivation, social influence, and trust in customers’ intention to adopt Internet banking services: The case of an emerging country. J. Retail. Consum. Serv. 2016, 28, 209–218. [Google Scholar] [CrossRef]
- Ranaweera, H. Perspective of trust towards e-government initiatives in Sri Lanka. SpringerPlus 2016, 5, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mou, J.; Shin, D.-H.; Cohen, J. Understanding trust and perceived usefulness in the consumer acceptance of an e-service: A longitudinal investigation. Behav. Inform. Technol. 2017, 36, 125–139. [Google Scholar] [CrossRef]
- Hanson, C.; West, J.; Neiger, B.; Thackeray, R.; Barnes, M.; Mcintyre, E. Use and acceptance of social media among health educators. Am. J. Health Educ. 2011, 42, 197–204. [Google Scholar] [CrossRef]
- Williams, M.; Rana, N.; Dwivedi, Y.; Lal, B. Is UTAUT really used or just cited for the sake of it? A systematic review of citations of UTAUT’s originating article. ECIS 2011 Proceedings 231.
- Teo, T. Modeling the determinants of pre-service teachers’ perceived usefulness of e-learning. Campus Wide Inf. Syst. 2011, 28, 124–140. [Google Scholar] [CrossRef]
- Chretien, K.C.; Kind, T. Social media and clinical care: Ethical, professional, and social implications. Circulation 2013, 127, 1413–1421. [Google Scholar] [CrossRef]
- Merolli, M.; Gray, K.; Martin-Sanchez, F. Health outcomes and related effects of using social media in chronic disease management: A literature review and analysis of affordances. J. Biomed. Inform. 2013, 46, 957–969. [Google Scholar] [CrossRef] [Green Version]
- Tao, D.; Wang, T.; Wang, T.; Zhang, T.; Zhang, X.; Qu, X. A systematic review and meta-analysis of user acceptance of consumer-oriented health information technologies. Comput. Hum. Behav. 2020, 104, 106147. [Google Scholar] [CrossRef]
| Construct | Definition | Source |
|---|---|---|
| Content quality | Inherent value and usefulness of the content provided by social media platforms. | [95] |
| Perceived credibility | Refers to the degree to which a person perceives that using a specific technology and system would be free of privacy and security related threats. | [47] |
| Peer influence | Behavioural intention to use a new technology/system is influenced by the perception of important others in their social circle. | [45,99,100] |
| Perceived risk | Refers to the degree to which the user perceives that it would be unsafe to utilise social media technologies. | [101] |
| Supporting conditions | Availability of required conditions to perform a specific task. | [102] |
| Confirmation of expectations | Refers to the degree to which the user perceives that actual performance is consistent with the expected performance of an information system/technology. | [103] |
| Perceived cost | The degree to which a user perceived that it is expensive to utilise a specific technology or system to perform a specific task. | [104] |
| Perceived usefulness | The extent to which a person believes that using the system will enhance his or her job performance. | [28] |
| Usage behaviour | Refers to the degree to which a user utilises one or more system features to complete a specific task. | [105] |
| Construct | Source | Measure | Std. Est. |
|---|---|---|---|
| Perceived Risk (α = 0.72, AVE = 0.72) | New measures based on [115,116,117,118] | Risky to share data | 0.8 |
| Information can be misused | 0.68 | ||
| Might not meet expectation | 0.66 | ||
| Concerned about the privacy settings | 0.74 | ||
| Content quality (α = 0.85, AVE = 0.83) | Adapted measures from [48] | Social media provides relevant information | 0.76 |
| Social media provides reliable information | 0.81 | ||
| Provide accurate content | 0.88 | ||
| Provide timely and complete health information | 0.87 | ||
| Perceived credibility (α = 0.88, AVE = 0.85) | Measures based on [55] | I am not worried about security issues | 0.82 |
| Health related social media sites are credible | 0.81 | ||
| I am confident in using online health platforms | 0.92 | ||
| I trust online health platforms | 0.84 | ||
| Peer Influence (α = 0.91, AVE = 0.88) | New measures based on [102] | Colleagues influence me to use social media | 0.87 |
| Patients influence me to use social media | 0.88 | ||
| Friends influence me to use social media | 0.9 | ||
| It is expected from healthcare professionals to use social media | 0.9 | ||
| Supporting conditions (α = 0.80, AVE = 0.78) | Adapted measure from [119] | I am encouraged participate actively in health communities | 0.72 |
| Can reach other healthcare professionals | 0.71 | ||
| Workplace encourages me to use social media | 0.81 | ||
| Industry practices influence me to use social media | 0.88 | ||
| Confirmation of expectations (α = 0.89, AVE = 0.89) | New measures based on [83,84,85] | Social media has improved relationships with patients | 0.83 |
| Saved time in professional interactions | 0.91 | ||
| Strengthened relationships with colleagues | 0.86 | ||
| Ensured better healthcare service | 0.94 | ||
| Perceived cost (α = 0.96, AVE = 0.93) | New measures based on [93] | Social media offers good value | 0.92 |
| Social media is cost-effective | 0.92 | ||
| Attractive in terms of cost | 0.91 | ||
| The cost of promotion is reasonable | 0.97 | ||
| Perceived usefulness (α = 0.89, AVE = 0.87) | New measures based on [28] | Social media enables me to communicate better with patients | 0.8 |
| Improves quality of patient care | 0.71 | ||
| Increases knowledge sharing | 0.67 | ||
| Improves job performance | 0.68 | ||
| Usage behaviour (α = 0.92, AVE = 0.87) | New measure developed based on [28] | I use social media to share medical knowledge with patients | 0.88 |
| I follow several health professionals in various social media | 0.91 | ||
| I share available medical information using social media platforms | 0.85 | ||
| I use social media for self-promotion | 0.85 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Content quality | 1 | ||||||||
| 2. Perceived risk | 0.297 ** | 1 | |||||||
| 3. Perceived credibility | 0.452 ** | 0.324 ** | 1 | ||||||
| 4. Peer influence | 0.496 ** | 0.223 ** | 0.391 ** | 1 | |||||
| 5. Supporting conditions | 0.243 ** | 0.092 | 0.192 * | 0.011 | 1 | ||||
| 6. Confirmation of expectations | 0.233 ** | 0.306 ** | 0.391 ** | 0.329 ** | 0.241 ** | 1 | |||
| 7. Perceived cost | 0.408 ** | 0.302 ** | 0.442 ** | 0.525 ** | 0.172 * | 0.532 ** | 1 | ||
| 8. Perceived usefulness | 0.250 ** | −0.216 ** | 0.238 ** | 0.325 ** | 0.334 * | 0.190 ** | −0.178 * | 1 | |
| 9. Usage behaviour | 0.364 ** | 0.201 ** | 0.323 ** | 0.561 ** | 0.189 * | 0.311 ** | 0.524 ** | 0.183 * | 1 |
| Type | Personal Use | Professional Use |
|---|---|---|
| 102/47% | 41/19% | |
| 55/25% | 27/12% | |
| 9/4% | 9/4% | |
| YouTube | 98/45% | 54/25% |
| Blogs | 17/8% | 15/7% |
| 47/21% | 47/21% | |
| Others | 33/15% | 23/11% |
| Path | Path Coefficient | S.E. | C.R. | P | ||
|---|---|---|---|---|---|---|
| H1: Content quality | → | Perceived usefulness | 0.360 | 0.160 | 2.752 | 0.012 |
| H2: Perceived credibility | → | Perceived usefulness | 0.423 | 0.117 | 3.274 | *** |
| H3: Perceived risks | → | Perceived usefulness | −0.600 | 0.103 | −5.849 | *** |
| H4: Peer influence | → | Perceived usefulness | 0.272 | 0.161 | 2.816 | *** |
| H5: Supporting conditions | → | Perceived usefulness | 0.428 | 0.199 | 2.062 | 0.019 |
| H6: Confirmation of expectations | → | Perceived usefulness | 0.282 | 0.087 | 3.620 | *** |
| H7: Perceived cost | → | Perceived usefulness | −0.201 | 0.093 | −2.164 | 0.020 |
| H8: Perceived usefulness | → | Usage behaviour | 0.142 | 0.063 | 2.241 | 0.022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, M.I.; Saleh, M.A.; Quazi, A. Social Media Adoption by Health Professionals: A TAM-Based Study. Informatics 2021, 8, 6. https://doi.org/10.3390/informatics8010006
Khan MI, Saleh MA, Quazi A. Social Media Adoption by Health Professionals: A TAM-Based Study. Informatics. 2021; 8(1):6. https://doi.org/10.3390/informatics8010006
Chicago/Turabian StyleKhan, Md Irfanuzzaman, M Abu Saleh, and Ali Quazi. 2021. "Social Media Adoption by Health Professionals: A TAM-Based Study" Informatics 8, no. 1: 6. https://doi.org/10.3390/informatics8010006
APA StyleKhan, M. I., Saleh, M. A., & Quazi, A. (2021). Social Media Adoption by Health Professionals: A TAM-Based Study. Informatics, 8(1), 6. https://doi.org/10.3390/informatics8010006





