1. Introduction
Medical error has been identified as a leading cause of avoidable harm [
1,
2], and patients outside hospitals have been shown at particular risk of drug-related medical errors [
3]. Failure to prescribe necessary drugs, patients failing to adhere to drug treatment, or intoxication caused by drug interactions are all examples of such errors. Many of these errors are preventable, and nearly half of all preventable adverse drug effects have been shown to be serious enough to cause hospitalization. The errors frequently occur in phases of prescribing or monitoring drug use. This highlights the importance of safety interventions in these stages of outpatient care [
2,
3].
Drug interactions are when concurrent use of multiple drugs, a drug and a food, or a drug and a beverage causes changes in the effects of a drug. Such changes may consist of the appearance of side effects, or in the suppression of desirable effects. The likelihood of drug interactions increases with the number of drugs taken. This also often correlates with age. Up to 7% of hospitalizations have been shown attributable to drug interactions [
4].
Polypharmacy means concurrent use of multiple drugs, which also applies to taking more than one drug for a single condition. Increased use of drugs has important health benefits, but polypharmacy increases risk of drug interactions. Åstrand et al. [
5] conducted a cross-sectional study of drug prescriptions in Jämtland, Sweden, over a period of 30 years. They found a pronounced 61% increase in polypharmacy, and found the risk of potentially interacting drugs strongly correlated with this increase. Hovstadius et al. [
6] looked at the development of polypharmacy in a 4-year period between 2005 and 2008. Using the Swedish Prescribed Drug Register they were able to analyze data over the entire Swedish population according to drugs prescribed per individual. Applying a definition of polypharmacy as receiving five or more prescription drugs during a three-month period, and of excessive polypharmacy as receiving ten or more drugs within the same period, they found an 8% increase in polypharmacy, and a 16% increase in excessive polypharmacy. The study showed a steady increase in polypharmacy, excessive polypharmacy, and drug use in general, in spite of the well-known risks to patient health [
6].
Lack of adherence to treatment is a frequent source of drug-related medical error. Non-hospitalized patients have greater influence over their adherence to drug treatment, making them central in the prevention of medical errors [
3]. Patient-centered care and patient participation have been recognized as important means of improving adherence, and have also been recognized as means of increasing health-literacy and improving patient safety and satisfaction. When patients are able to self-manage their symptoms, this leads to more efficient healthcare, and also improves the quality of life. Participation is achieved by facilitating active engagement in decision-making. Achieving this requires that caregivers respect patients’ knowledge of their own bodies, and regard this knowledge as complementary to their professional knowledge. Participation also requires empowering patients with the information and the resources that enable them to participate [
7].
Assuming a patient-centered perspective on drug treatment suggests exploring patient needs for information regarding drugs. Kusch, Haefeli and Seidling [
8] investigated patients’ desires for drug information through a systematic literature review sourcing studies on patients’ drug information needs as well as studies on patient inquiries to drug information services. Topics were identified, and their frequency of occurrence was calculated. The results consistently showed adverse drug reactions and drug–drug interactions as the most desired topics. Discussing their findings, Kusch et al. [
8] indicated the need for making drug information more accessible to patients. To do so, they suggested building information databases based on patient-oriented topics, such as those identified by themselves.
In Scandinavia, much work has been undertaken to develop information systems for drug information and drug interactions. Such systems help healthcare professionals navigate large and constantly revised amounts of drug information. Böttiger et al. [
9] discussed the Swedish Finnish Interaction X-referencing database (SFINX), a predecessor of the current Janusmed [
10], describing the integration of its database with Swedish and Finnish healthcare systems to serve thousands of physicians and pharmacists. A subsequent study [
11] looked at the impact of SFINX in primary healthcare centers. The study compared 15 centers where the SFINX system had been implemented with 5 centers where it had not. The centers where the system had been implemented showed a significant reduction in prescriptions leading to serious drug interactions [
11].
Janusmed is today freely available as a web-based service. Although developed for a professional audience, rumors caught the attention of Nörby et al. [
12] that pregnant women had also adopted the site. This prompted them to investigate the pregnant women’s experiences of using the Drugs and Birth Defects section of the service. The findings showed that 11% of the women were already familiar with the service in advance of their participation in the study. They also reported using several other information resources about drugs related to pregnancy. Some became more anxious from accessing the content, but the vast majority found the information valuable and easy to understand. They also found it to confirm and support information provided by healthcare professionals. Nörby et al. went on to suggest that communication and patient compliance might improve if patients and professionals referred to the same sources [
12].
mHealth is meanwhile emerging as a promising means of delivering patient-oriented healthcare outside hospitals. mHealth is short for mobile healthcare, meaning the delivery of healthcare services and information through mobile devices. The mobile platform allows flexible and ubiquitous access to online and offline services and information. It therefore lends itself in particular to outpatient needs, and to individualized and patient-oriented services [
13]. mHealth applications have been found to have been implemented predominantly through experimentation with technology rather than through strategic planning [
14]. At the same time, these systems impact human lives on a large scale, potentially reaching millions of users and directly affecting their health. Just as it is imperative that information be accurate, it is also imperative that mHealth services not lead to user error, and thereby to adverse health effects [
13].
Usability in critical systems can be a matter of life or death. Nielsen [
15] commented on Koppel et al. [
16], identifying 22 ways that automated hospital systems could result in the wrong medication being dispensed to patients. Nielsen [
15] identified most of the problems as well-known usability issues that had been understood for decades. In a similar vein, Reolon et al. [
13] showed that studies on healthcare systems have found significant usability problems inviting a range of human errors. These were found to have the potential to lead to injury or even death. Within mHealth they likewise found a range of usability problems as well as a lack of user-centered design. They argued that patient-oriented systems would likely be in particular need for usability due to a lack of training as well as a significant proportion of elderly users.
Research Objective
Usability studies have begun to appear within eHealth and mHealth [
13,
15]. More recent advances [
17,
18] have developed and validated instruments for self-reported usability. To some extent, these have also been adopted in practice [
19,
20]. The usability testing that is needed to collect self-reported metrics is, however, known to be resource intensive. Heuristic evaluations have meanwhile proven to be particularly cost-efficient in driving the design improvement [
21]. Research on the use of heuristic evaluations within mHealth shows papers on the topic to be sparse [
13]. Adam and Vang [
22], meanwhile, conducted an expert-based checklist evaluation on drug–drug interaction websites, measuring information capacity, patient usability and readability. No studies appear to have been conducted specifically on the quality of user interfaces in terms of usability for patient-oriented drug interaction checkers. The objective of this paper has therefore been to explore the prevalence and characteristics of usability issues facing patients using publicly available drug interaction checkers in the Scandinavian market. This was conducted to facilitate future improvements to this emerging market, and to raise awareness of the usability issues users face today.
Two research questions have guided the study:
We delimited the context of exploration to the Scandinavian market in order to facilitate relevant and actionable insights. We also delimited it to drug interaction checkers accessible on mobile platform in order to appreciate the promise of mHealth for patient-oriented and outpatient uses. We did so also to stress usability requirements, seeing that mobile platforms place additional demands on usability.
6. Discussion
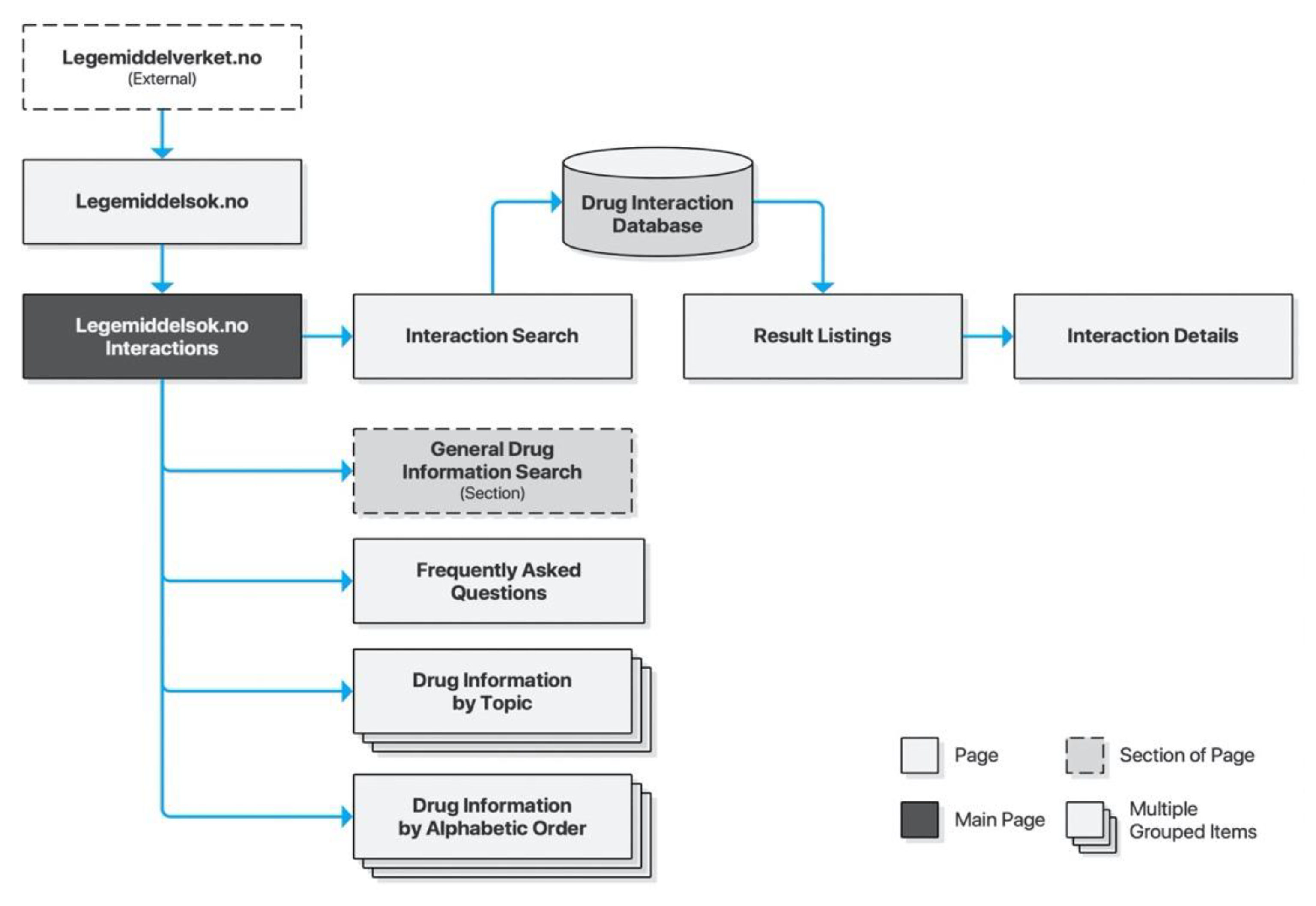
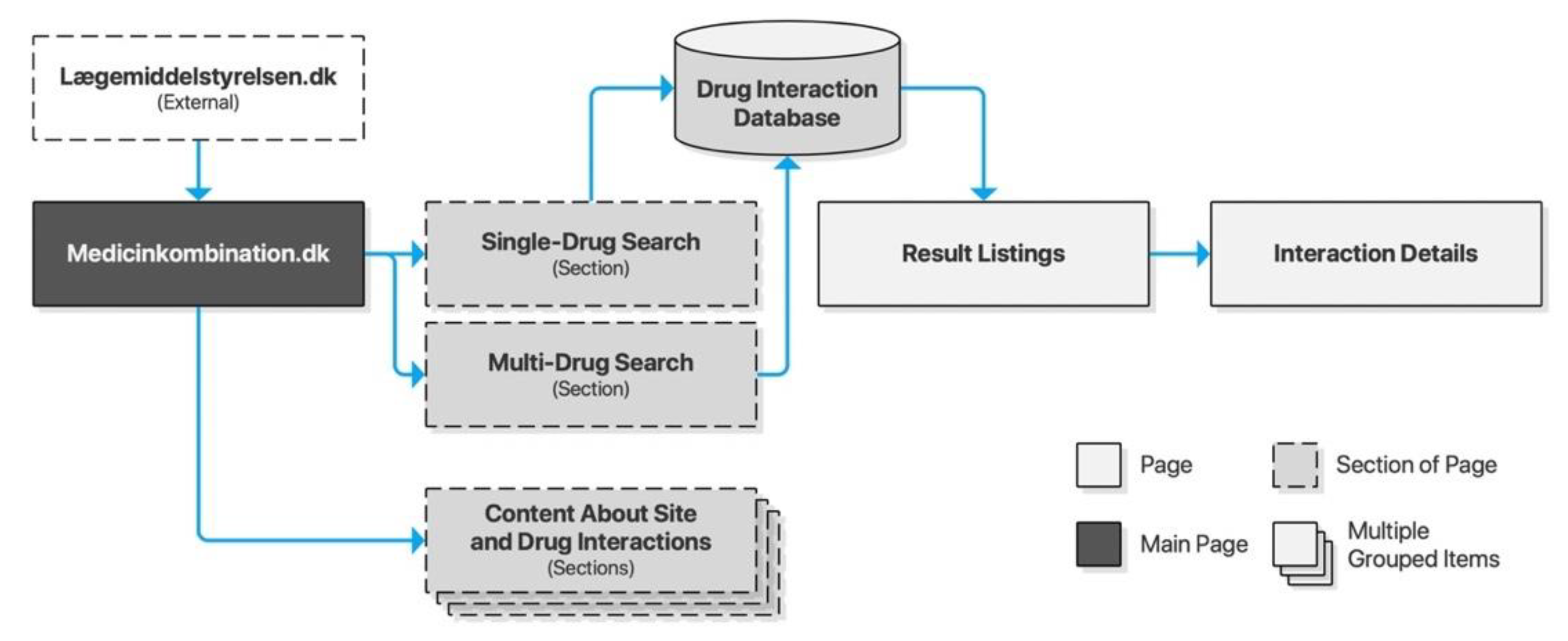
Allowing patients to act as decision-makers regarding their own health requires empowering them with information. The systems conveying this information must be usable in order for empowerment to take place. In this paper, we identified six drug interaction checkers publicly available to Scandinavian audiences: three in Norway, two in Denmark, and one in Sweden. The Norwegian checkers all utilized the same professionally oriented database. The two Danish checkers, on the other hand, utilized the same interface to serve content from different databases—one professionally oriented and one patient-oriented. The Swedish checker served only professionally oriented content and did so using multiple topically oriented databases. The service providers were national authorities, drug industry associations and private eHealth businesses. All of them served content from national authoritative sources, however. All except one of the checkers primarily targeted professional audiences as a means of clinical decision support, while at the same time allowing public access. Only Medicinkombination.dk targeted patient audiences with highly readable patient-oriented content. This constitutes an important contribution to patient-oriented healthcare in Denmark.
Although this paper has not aimed to investigate content specifically, it was noted that checkers targeting professional audiences did so frequently using acronyms and technical terminology. Acronyms are particularly difficult for laypersons to interpret as web searches for their meaning will often yield incorrect or poorly targeted results. Content will consequently not only be hard to read, but sometimes even inaccessible. As Nörby et al. [
12] have shown, this does not stop patients from using these checkers, but is suggested to cause anxiety for some users. It also prevents the benefits of empowering and engaging patients in regard to their health.
The heuristic evaluations showed all of the checkers applying patterns of progressive disclosure, from summarized listings of drug interactions to detailed descriptions and even external links for further reading. This might seem an appropriate pattern to preserve in order to accommodate patients’ varying attitudes towards supplementary drug information, as identified by Kusch, Haefeli and Seidling [
8]. Although the content of Medicinkombination.dk was very readable, it was also very brief. This may represent a precautious approach to provide content without causing anxiety. It may, however, also limit the positive effects of improved communication with professionals and improved compliance, as suggested by Nörby et al. [
12].
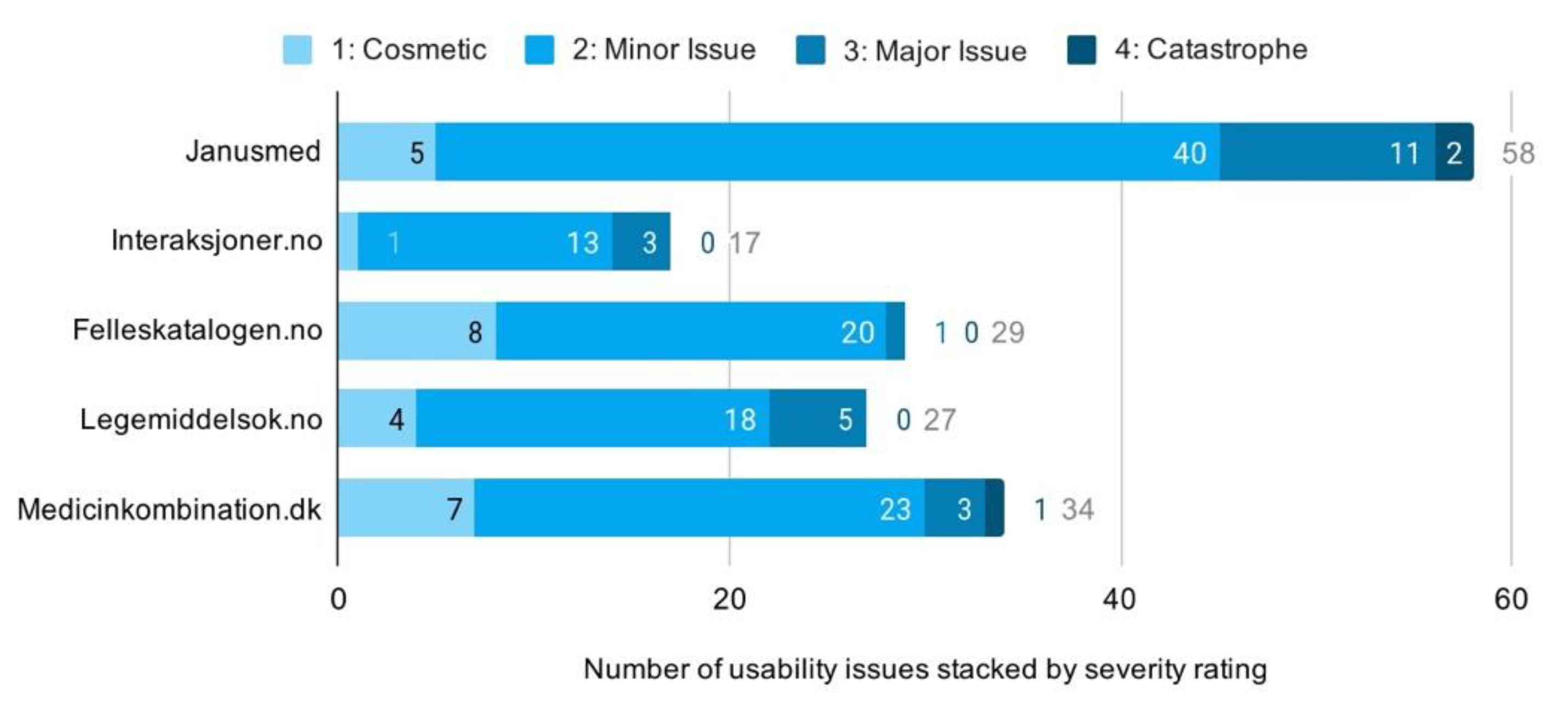
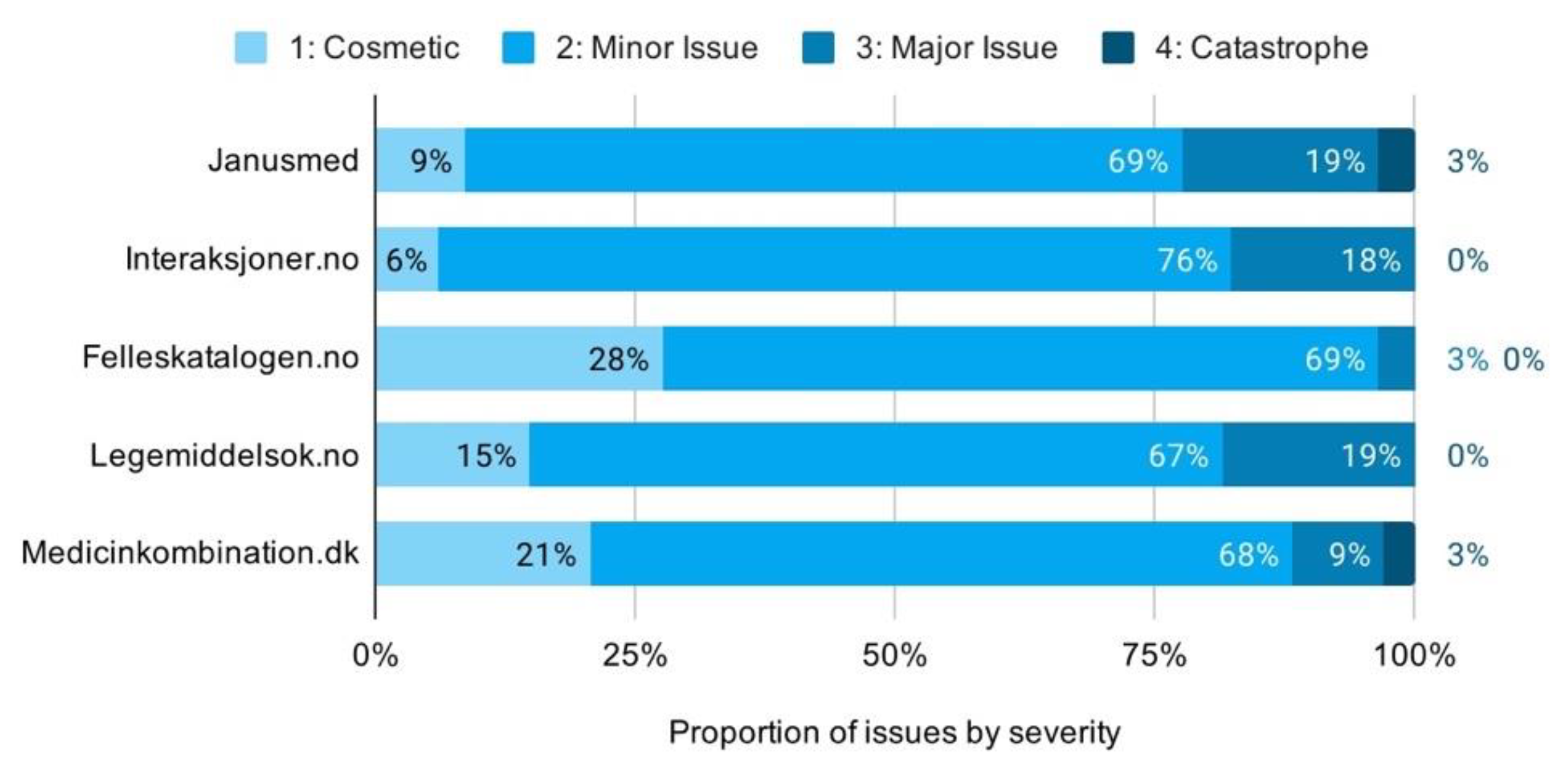
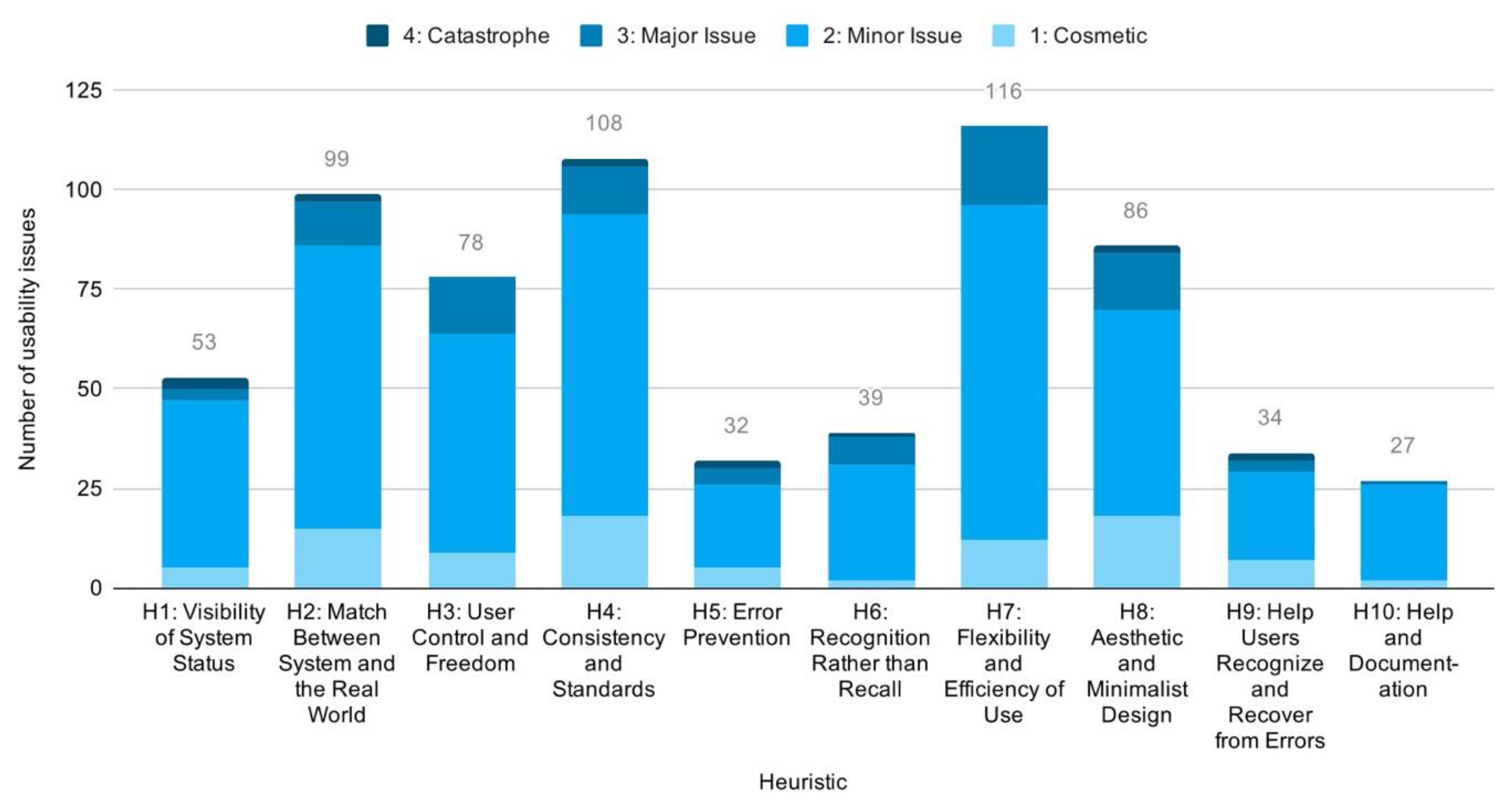
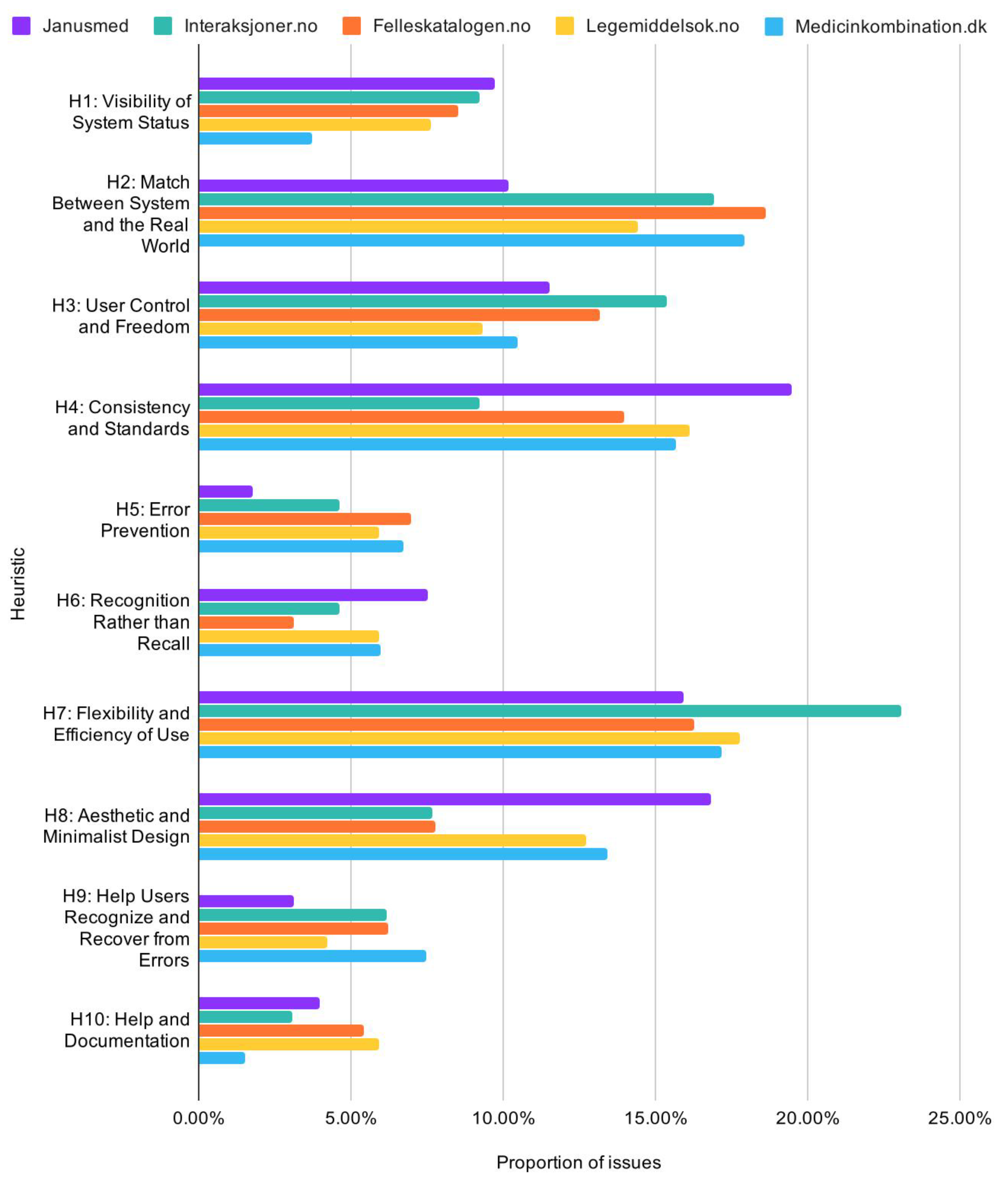
6.1. Prevalence and Characteristics of Usability Issues
In terms of usability issues and their characteristics, a large number of issues were detected across all of the drug interaction checkers. These were predominantly minor issues, but a considerable number of major issues were found in all but one of the checkers. Numbers of issues cannot be compared across studies, but we regard these as high numbers in view of the limited extent of the tasks applied. Qualitative analyses identified a positive correlation between the number of usability issues and the complexity of a checker. Care should be taken not to interpret this as a causal relation justifying more usability issues as a tradeoff for providing functionality. One would rather expect the basics to precede the extras. Considering their relation to basic design principles, an argument could be made that the high number of usability issues may indicate lack of systematic user-centered development. It could also result from losing track of user goals over time through incremental addition of features. Addition of features will at some point warrant redesign of a system, but limited resources may instead lead to shortsighted solutions being implemented. These can then accumulate to reduce usability and system quality. We suggest these as the most likely culprits worth examining for those drug interaction checkers identified in this paper with high numbers of usability issues.
Analyses, moreover, showed a very low degree of mobile-adaptive design. Three out of five of the checkers were essentially non-supportive of mobile devices. Adaptive design may have been a premium in the past, but is today an essential component of system quality for the Web. The proportion of mobile users on the Web is steadily increasing, at this point matching desktop users in Sweden [
33]. Intermittent tasks, such as checking drug interactions, lend themselves in particular to mobile use, making it readily apparent that service providers cannot afford to ignore this segment of users. Lack of adaptive design forces users to handle zooming and repositioning of the viewport. This causes a constant strain on efficiency, effectiveness, and satisfaction of use, rapidly convincing users to leave and never return.
Many of the checkers also showed poor leverage of basic design principles such as visual and typographic hierarchies to guide users through the interface. Minimalist and aesthetic design utilizes consistency to highlight important information through purposefully breaking this consistency. This is a way of guiding users through complex information environments. Lack of consistency generates noise, and this noise prevents anything from standing out to the user. Usability issues relating to lack of minimalist and aesthetic design thus causes unnecessary cognitive efforts spent at interpreting the interface as opposed to attaining user goals. This leads to user dissatisfaction.
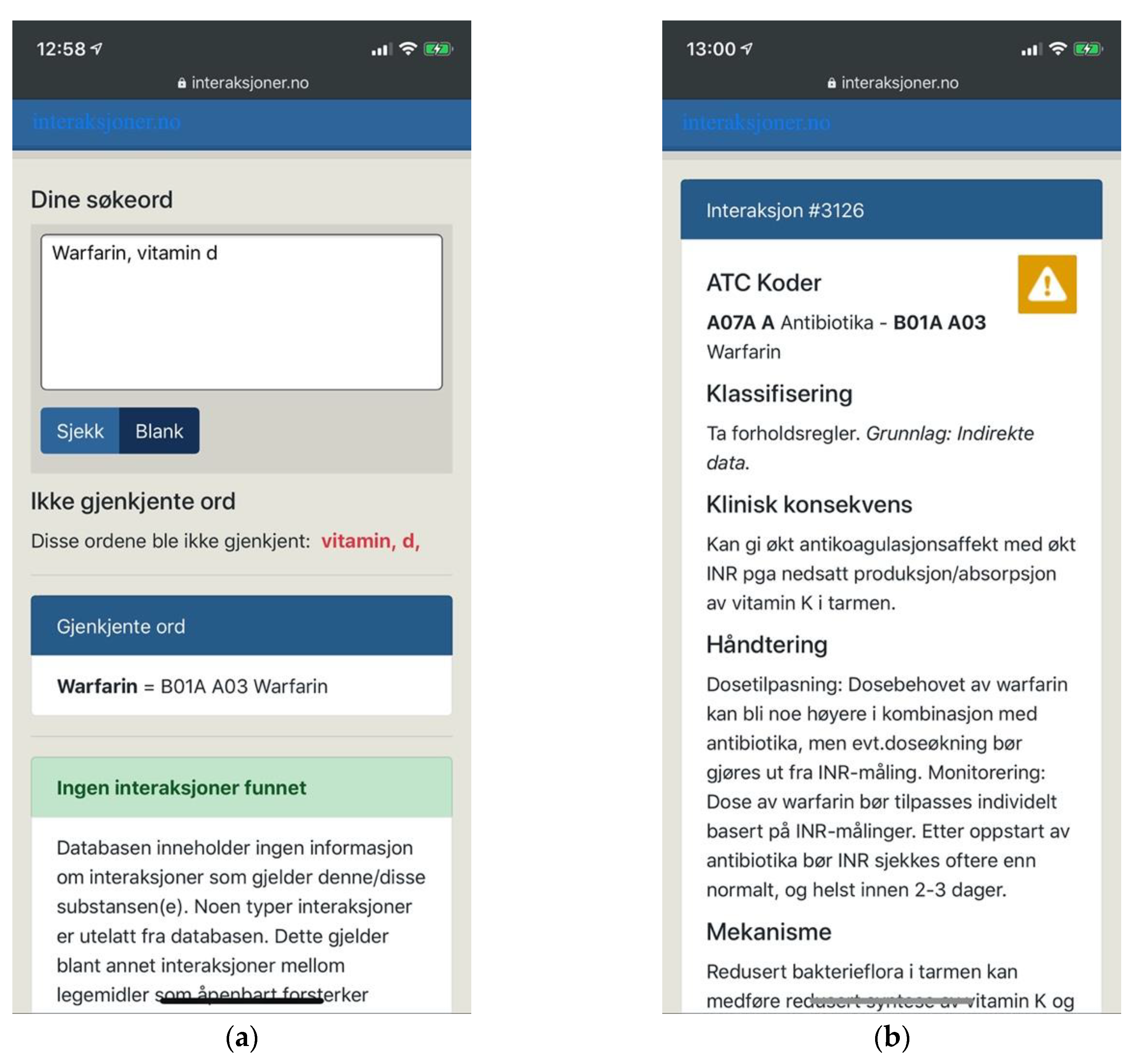
Supporting users through search suggestions, thesauri and means of managing search results was also identified as particularly important for this context. All but one of the checkers already provided search suggestions. In the only case where this was not provided, we noted this as a major usability issue in view of users having to type unfamiliar and hard-to-spell drug names without any help. Without search suggestions users would also not get early feedback that their search terms would not be recognized, and as such not yield any results. These findings of ours support Adam and Vang’s [
22] inclusion of search suggestions (medication pick list) as a criterion for patient usability. A natural extension of helping users type their intended queries is to help them attain the intended results even when they provide inaccurate input. In this respect we noted a lack of thesauri in all of the systems. Thesauri would be particularly useful due to the need for spelling unfamiliar words with multiple plausible spellings. As an example, the term “thyroxine” may reasonably be spelled as “thyroxin”, “tyroxin”, or “tyroksin” in Scandinavian languages. In addition, it would be reasonable to accept English spellings as well as popular terms such as “vitamin d” for technical terms such as “kolekalsiferol”. Thesauri were not considered by Adam and Vang [
22]. These means of user support are particularly important as they affect not only long-term satisfaction, but even short-term ability to retrieve information at all.
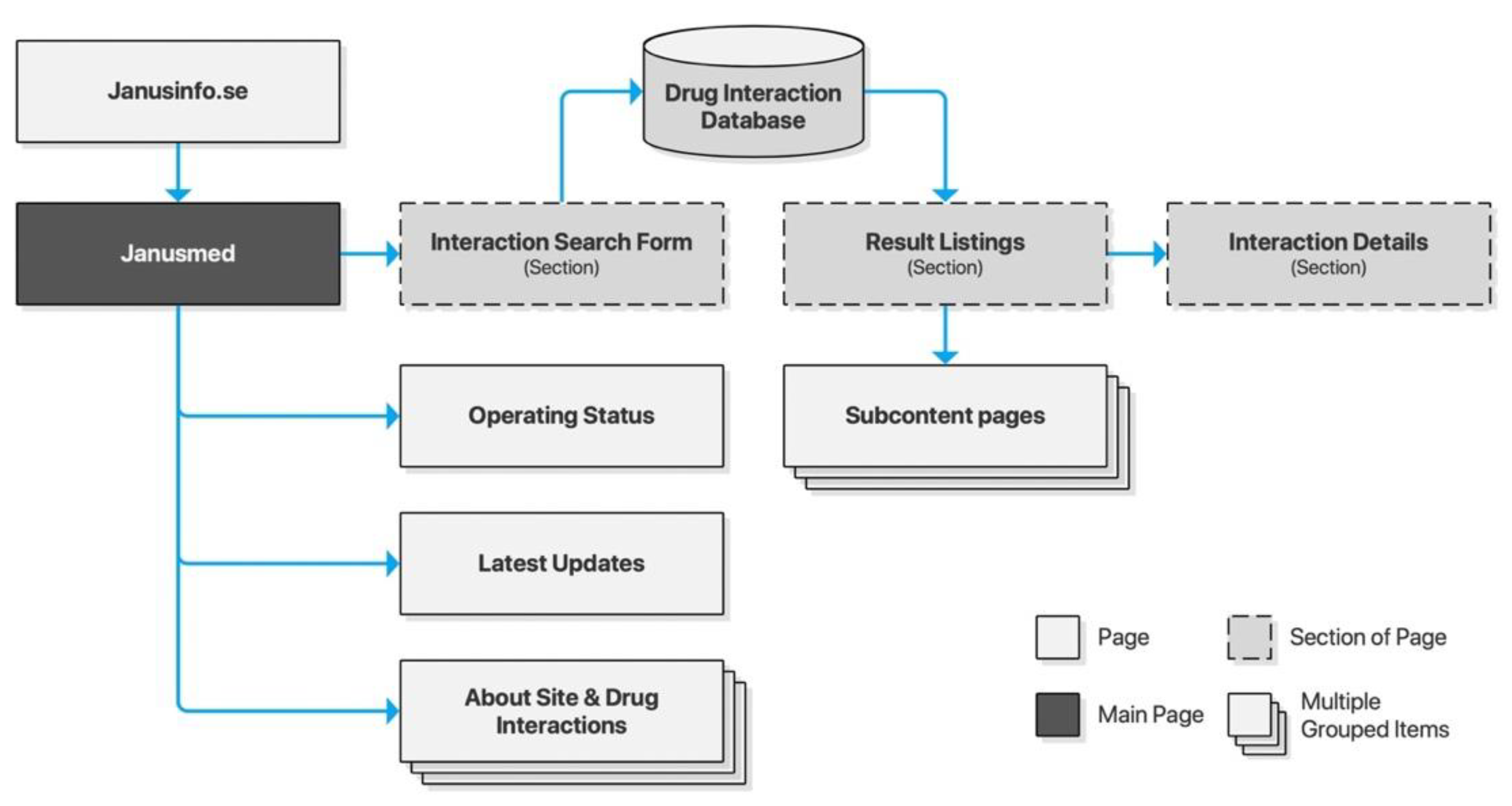
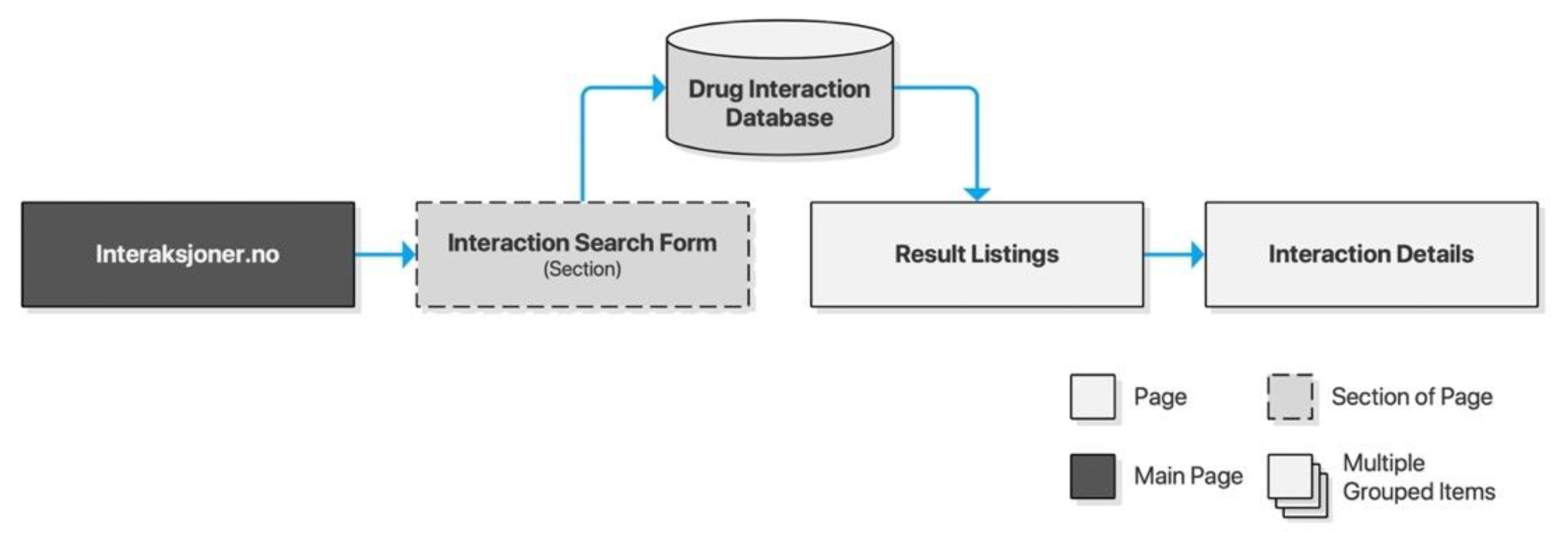
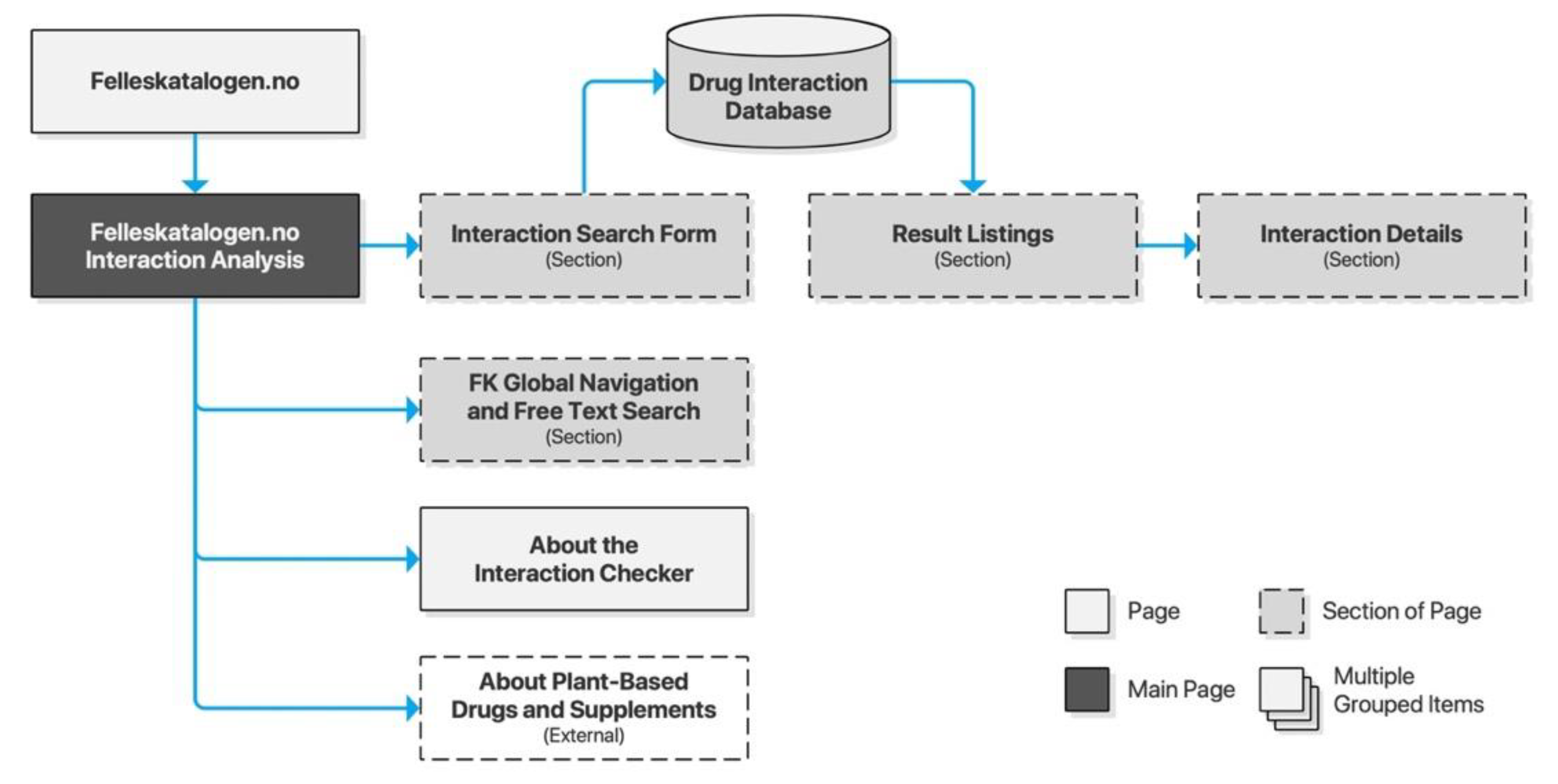
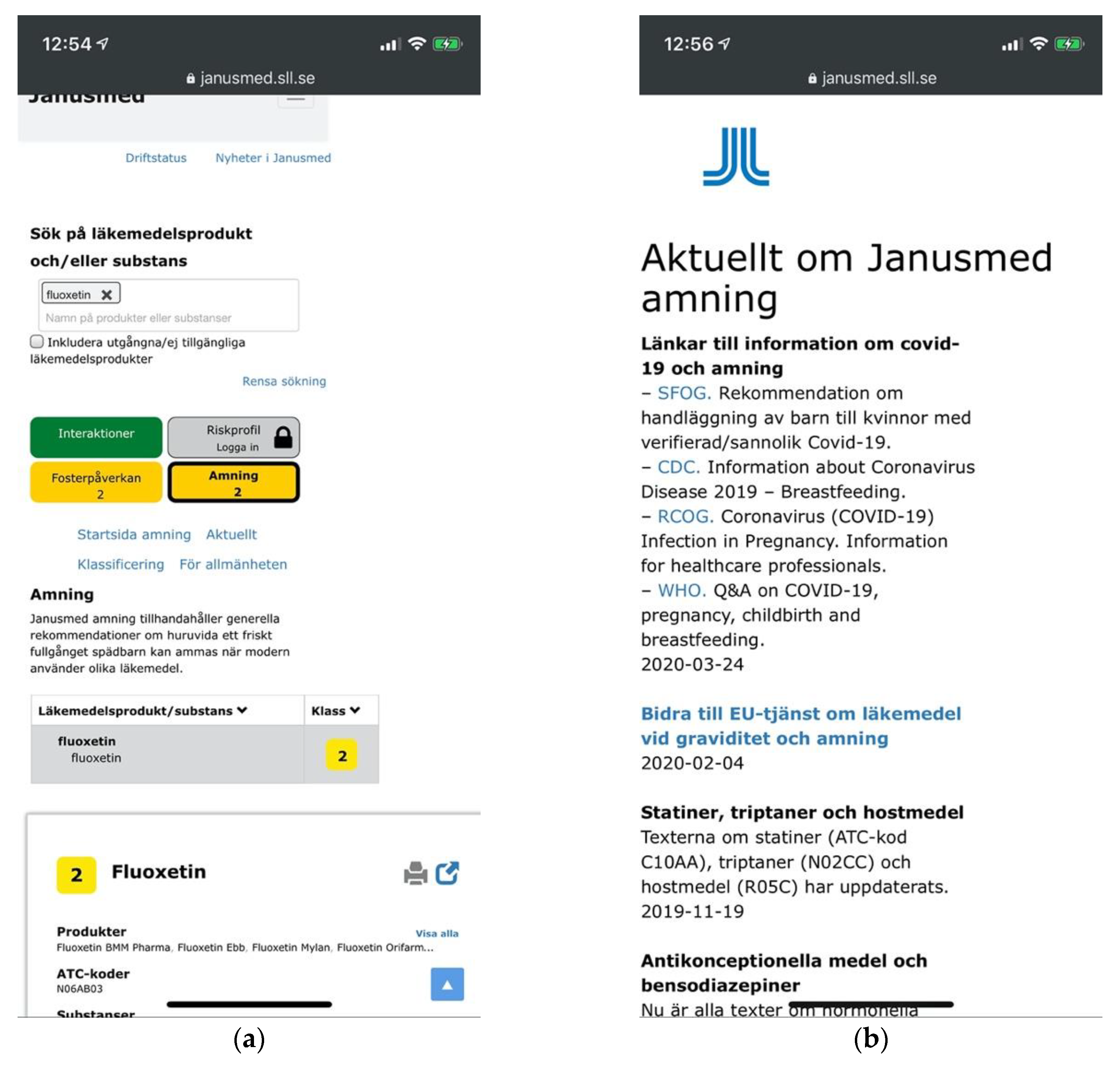
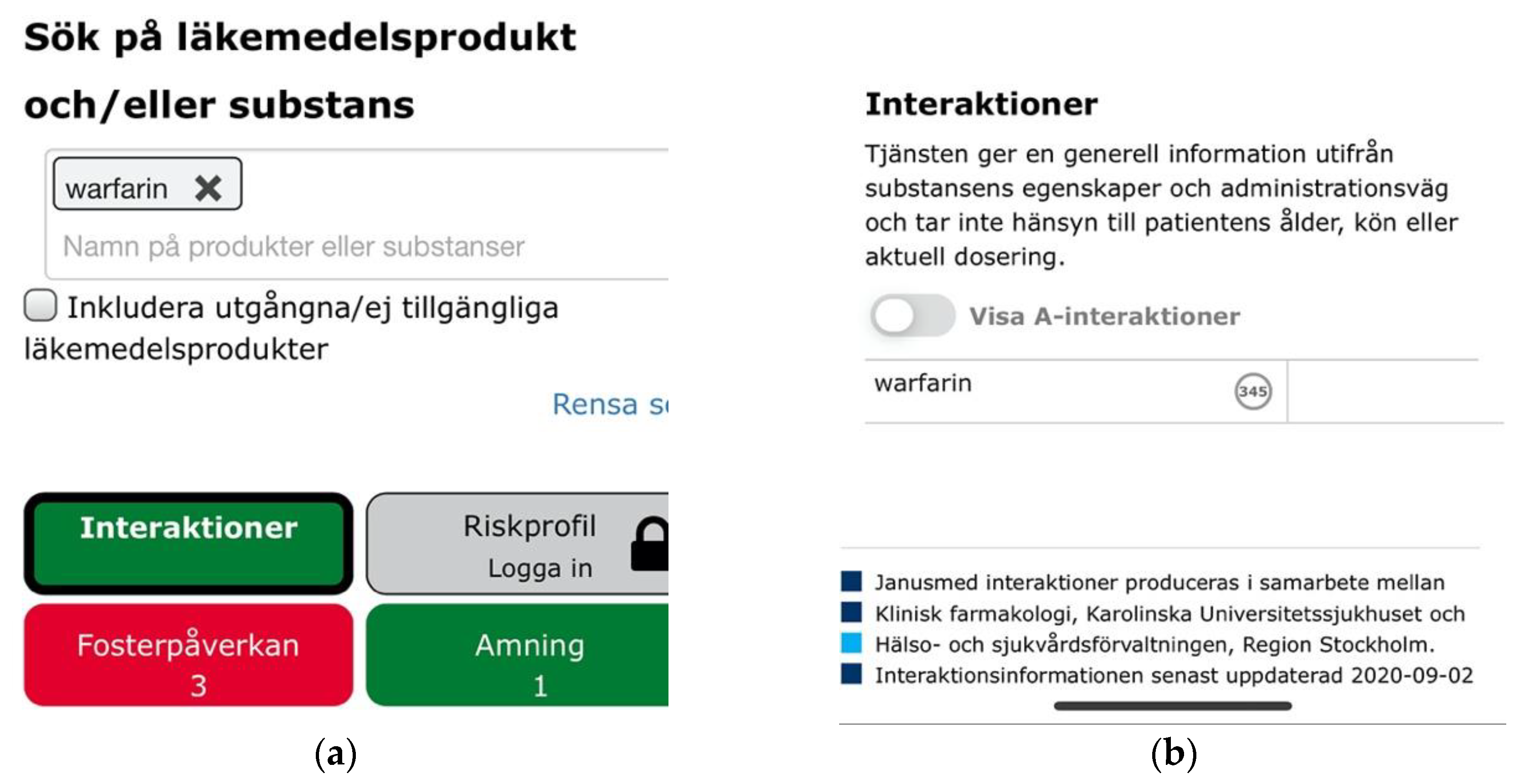
In terms of single-case analyses, nearly twice the mean number of usability issues were identified for the Swedish checker Janusmed. Even catastrophic issues were identified related to basic design principles such as providing appropriate feedback to users. The structure of the service was especially complex and incoherent. This may suggest organic growth insufficiently supported by goal-oriented and user-centered approaches. Janusmed on the other hand did provide more utility in terms of both content and functionality, employing promising interaction idioms for constructing queries. The Norwegian Interaksjoner.no took a minimalist approach, providing core functionality accompanied by clear and coherent feedback and visual hierarchy. This resulted in a particularly low number of usability issues. It failed, however, at providing patients with much-needed support in spelling difficult drug names, resulting in major usability issues in that area. Felleskatalogen.no represented a middle ground of functionality and coherence. It was one of only two services providing mobile-adaptive design. Providing necessary user support also resulted in an average amount of usability issues, but with a notable distribution towards the lower end of the severity spectrum. Legemiddelsok.no had particular issues with adaptive design, causing excessive viewport handling. The most notable trend beyond that was a complete lack of basic information welcoming users, explaining the purpose of the service, or how to use it. Medicinkombination.dk distinguished itself by providing highly accessible patient-oriented content. Its complete lack of adaptive design did not however help in providing accessibility for public audiences on mobile devices. A catastrophic issue was also identified where users might be presented with results for the previous query rather than the current. This could potentially lead to serious medical error.
Author Contributions
Conceptualization, D.V., E.J.A. and M.F.; methodology, investigation and data curation, D.V. and E.J.A.; formal analysis, D.V.; writing—original draft preparation, D.V. and E.J.A.; writing—review and editing, D.V.; visualization, D.V. and E.J.A.; supervision, M.F.; project administration, E.J.A., D.V. and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Patient Safety—Data and Statistics. Available online: https://www.euro.who.int/en/health-topics/Health-systems/patient-safety/data-and-statistics (accessed on 10 September 2020).
- Säfholm, S.; Bondesson, Å.; Modig, S. Medication Errors in Primary Health Care Records; a Cross-Sectional Study in Southern Sweden. BMC Fam. Pract. 2019, 20, 110. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, L.A.; Winterstein, A.G.; Søndergaard, B.; Haugbølle, L.S.; Melander, A. Systematic Review of the Incidence and Characteristics of Preventable Adverse Drug Events in Ambulatory Care. Ann. Pharmacother. 2007, 41, 1411–1426. [Google Scholar] [CrossRef] [PubMed]
- Cascorbi, I. Drug Interactions—Principles, Examples and Clinical Consequences. Dtsch. Ärzteblatt Int. 2012, 109, 546–556. [Google Scholar]
- Åstrand, E.; Åstrand, B.; Antonov, K.; Petersson, G. Potential Drug Interactions During a Three-Decade Study Period: A Cross-Sectional Study of a Prescription Register. Eur. J. Clin. Pharmacol. 2007, 63, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Hovstadius, B.; Hovstadius, K.; Åstrand, B.; Petersson, G. Increasing Polypharmacy—An Individual-Based Study of the Swedish Population 2005–2008. BMC Clin. Pharmacol. 2010, 10, 1–8. [Google Scholar] [CrossRef]
- Castro, E.M.; Van Regenmortel, T.; Vanhaecht, K.; Sermeus, W.; Van Hecke, A. Patient Empowerment, Patient Participation and Patient—Centeredness in Hospital Care: A Concept Analysis Based on a Literature Review. Patient Educ. Couns. 2016, 99, 1923–1939. [Google Scholar] [CrossRef] [PubMed]
- Kusch, M.K.P.; Haefeli, W.E.; Seidling, H.M. How to Meet Patients’ Individual Needs for Drug Information—A Scoping Review. Patient Prefer. Adherence 2018, 12, 2339–2355. [Google Scholar] [CrossRef] [PubMed]
- Böttiger, Y.; Laine, K.; Andersson, M.L.; Korhonen, T.; Molin, B.; Ovesjö, M.-L.; Tirkkonen, T.; Rane, A.; Gustafsson, L.L.; Eiermann, B. SFINX—A Drug-Drug Interaction Database Designed for Clinical Decision Support Systems. Eur. J. Clin. Pharmacol. 2009, 65, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Janusmed. Available online: https://janusmed.sll.se (accessed on 1 June 2020).
- Andersson, M.L.; Böttiger, Y.; Lindh, J.D.; Wettermark, B.; Eiermann, B. Impact of the Drug-Drug Interaction Database SFINX on Prevalence of Potentially Serious Drug—Drug Interactions in Primary Health Care. Eur. J. Clin. Pharmacol. 2013, 69, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Nörby, U.; Källén, K.; Shemeikka, T.; Korkmaz, S.; Winbladh, B. Pregnant Women’s View on the Swedish Internet Resource Drugs and Birth Defects Intended for Health Care Professionals. Acta Obstet. Gynecol. Scand. 2015, 94, 960–968. [Google Scholar] [CrossRef] [PubMed]
- Reolon, M.; Lacerda, T.; Krone, C.; Gresse von Wangenheim, C.; Xafranski, J.; Nunes, J.; Von Wangenheim, A. Usability Heuristics for Evaluating Healthcare Applications for Smartphones: A Systematic Literature Review; Technical Report INCoD/GQS.01.2016.E.; INCoD—Brazilian Institute for Digital Convergence: Campinas, Brazil, 2016. [Google Scholar]
- World Health Organization. mHealth: New Horizons for Health through Mobile Technologies: Second Global Survey on eHealth; Global Observatory for eHealth Series Volume 3; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- How to Kill Patients Through Bad Design. Available online: https://www.nngroup.com/articles/medical-usability/ (accessed on 29 May 2020).
- Koppel, R.; Metlay, J.P.; Cohen, A.; Abaluck, B.; Localio, A.R.; Kimmel, S.E.; Strom, B.L. Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors. JAMA 2005, 293, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Schnall, R.; Cho, H.; Liu, J. Health Information Technology Usability Evaluation Scale (Health-ITUES) for Usability Assessment of Mobile Health Technology: Validation Study. JMIR Mhealth Uhealth 2018, 6, e4. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Bao, J.; Setiawan, I.; Saptono, A.; Parmanto, B. The mHealth App Usability Questionnaire (MAUQ): Development and Validation Study. JMIR Mhealth Uhealth 2019, 7, e11500. [Google Scholar] [CrossRef] [PubMed]
- Beauchemin, M.; Gradilla, M.; Baik, D.; Cho, H.; Schnall, R. A Multi-step Usability Evaluation of a Self-Management App to Support Medication Adherence in Persons Living with HIV. Int. J. Med. Inform. 2019, 122, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Stonbraker, S.; Cho, H.; Hermosi, G.; Pichon, A.; Schnall, R. Usability Testing of a mHealth App to Support Self-Management of HIV-Associated Non-AIDS Related Symptoms. Stud. Health Technol. Inform. 2018, 250, 106–110. [Google Scholar]
- Jaspers, M.W. A Comparison of Usability Methods for Testing Interactive Health Technologies: Methodological Aspects and Empirical Evidence. Int. J. Med Inform. 2009, 78, 340–353. [Google Scholar] [CrossRef]
- Adam, T.J.; Vang, J. Content and Usability Evaluation of Patient Oriented Drug—Drug Interaction Websites. Amia Annu. Symp. Proc. 2015, 2015, 287–296. [Google Scholar]
- 10 Usability Heuristics for User Interface Design. Available online: https://www.nngroup.com/articles/ten-usability-heuristics/ (accessed on 1 July 2020).
- Monkman, H.; Kushniruk, A. A Health Literacy and Usability Heuristic Evaluation of a Mobile Consumer Health Application. Stud. Health Technol. Inform. 2013, 192, 724–728. [Google Scholar]
- Bertini, E.; Catarci, T.; Dix, A.; Gabrielli, S.; Kimani, S.; Santucci, G. Appropriating Heuristic Evaluation for Mobile Computing. Int. J. Mob. Hum. Comput. Interact 2009, 1, 20–41. [Google Scholar] [CrossRef]
- Tullis, T.; Albert, B. Measuring the User Experience, 2nd ed.; Morgan Kaufmann: Waltham, MA, USA, 2013. [Google Scholar]
- Sharp, H.; Preece, J.; Rogers, Y. Interaction Design: Beyond Human-Computer Interaction, 5th ed.; Wiley: Indianapolis, IN, USA, 2019. [Google Scholar]
- Wilson, C. User Interface Inspection Methods: A User-Centered Design Method; Morgan Kaufmann: San Francisco, CA, USA, 2014. [Google Scholar]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative & Mixed Methods Approaches, 5th ed.; Sage: Los Angeles, CA, USA, 2018. [Google Scholar]
- Similarsites.com—Easily Explore Alternative Websites. Available online: https://www.similarsites.com/ (accessed on 22 May 2020).
- Nielsen, J.; Molich, R. Heuristic Evaluation of User Interfaces. In Proceedings of the SIGCHI Conference on Human Factors in Computing. Systems, Seattle, WA, USA, 1–5 April 1990; pp. 249–256. [Google Scholar]
- Nielsen, J. Enhancing the Explanatory Power of Usability Heuristics. In Proceedings of the SIGCHI Conference on Human Factors in Computing. Systems, Boston, MA, USA, 24–28 April 1994; pp. 152–158. [Google Scholar]
- Desktop vs Mobile vs Tablet Market Share Sweden | StatCounter Global Stats. Available online: https://gs.statcounter.com/platform-market-share/desktop-mobile-tablet/sweden/#monthly-201504-202004 (accessed on 1 June 2020).
- Nielsen, J.; Landauer, T. A Mathematical Model of the Finding of Usability Problems. In Proceedings of the SIGCHI Conference on Human Factors in Computing. Systems, Amsterdam, The Netherlands, 24–29 April 1993; pp. 206–213. [Google Scholar]
- How Many Test Users in a Usability Study? Available online: https://www.nngroup.com/articles/how-many-test-users/ (accessed on 1 July 2020).
- Molich, R. Are Usability Evaluations Reproducible? Interactions 2018, 25, 82–85. [Google Scholar] [CrossRef]
- Law, L.C.; Hvannberg, E.T. Complementarity and Convergence of Heuristic Evaluation and Usability Test: A Case Study of UNIVERSAL Brokerage Platform. In Proceedings of the Second Nordic Conference on Human-Computer Interaction, Aarhus, Denmark, 19–23 October 2002; pp. 71–80. [Google Scholar]
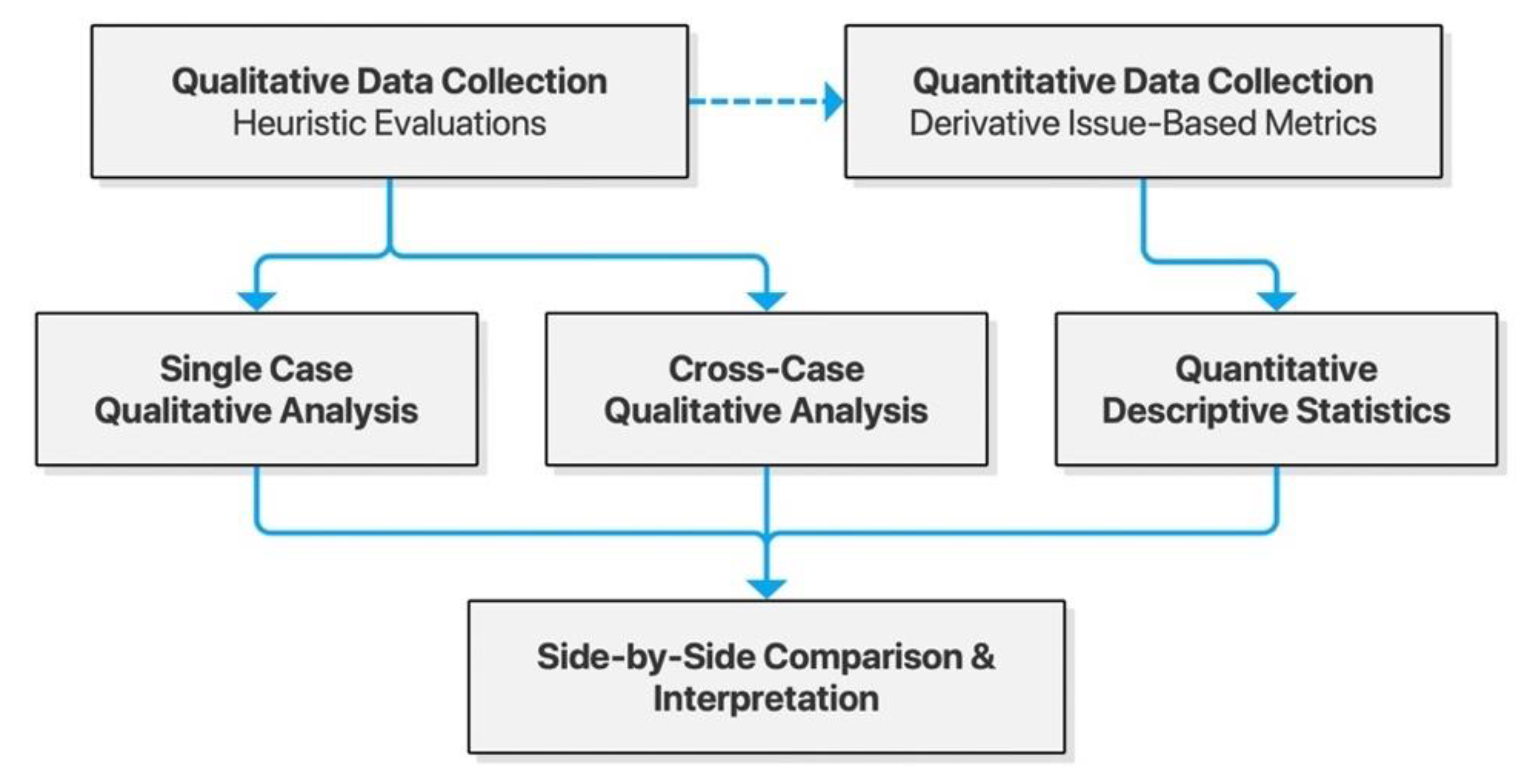
Figure 1.
Model of the convergent mixed-methods study design.
Figure 2.
Sitemap for Janusinfo.se.
Figure 3.
Sitemap for Interaksjoner.no.
Figure 4.
Sitemap for Felleskatalogen.no.
Figure 5.
Sitemap for Legemiddelsok.no.
Figure 6.
Sitemap for Medicinkombination.dk.
Figure 7.
Distribution of usability issues across services.
Figure 8.
Proportion of usability issues by severity across services.
Figure 9.
Distribution of issues by heuristic.
Figure 10.
Proportion of usability issues by heuristic across services.
Figure 11.
(a) Visual and typographic hierarchies at Janusmed are broken across sections of the page; (b) Current news for the breastfeeding section opens in a new tab without means of navigation.
Figure 12.
(a) Interaksjoner.no with an adaptive layout, a clear visual hierarchy and clear feedback; (b) Drug interaction details open on a new page in the same browser tab.
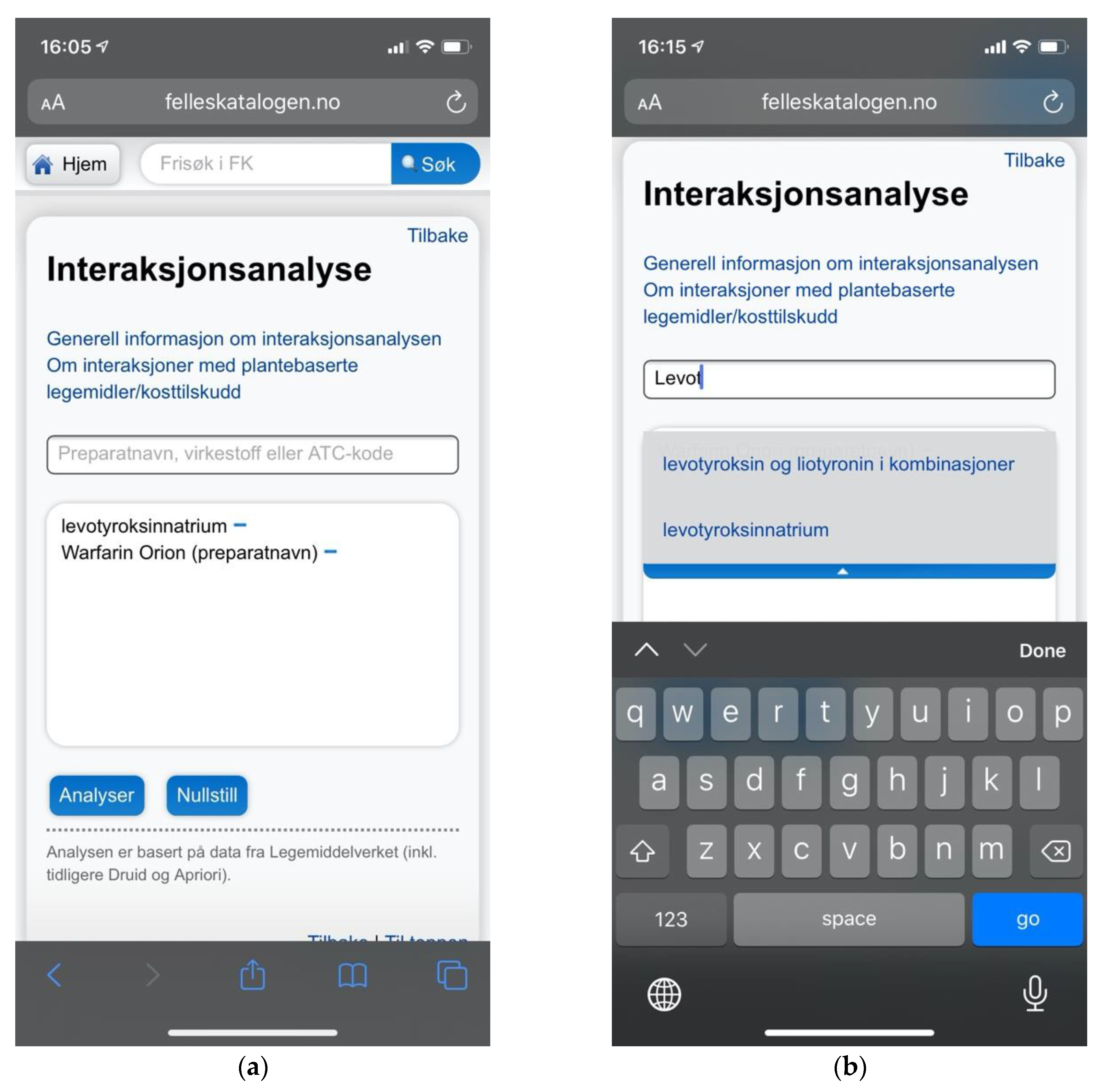
Figure 13.
(a) Felleskatalogen.no providing a mobile adaptive layout avoiding issues with zoom and viewport handling; (b) Felleskatalogen.no did provide search suggestions to help users choose the appropriate search terms.
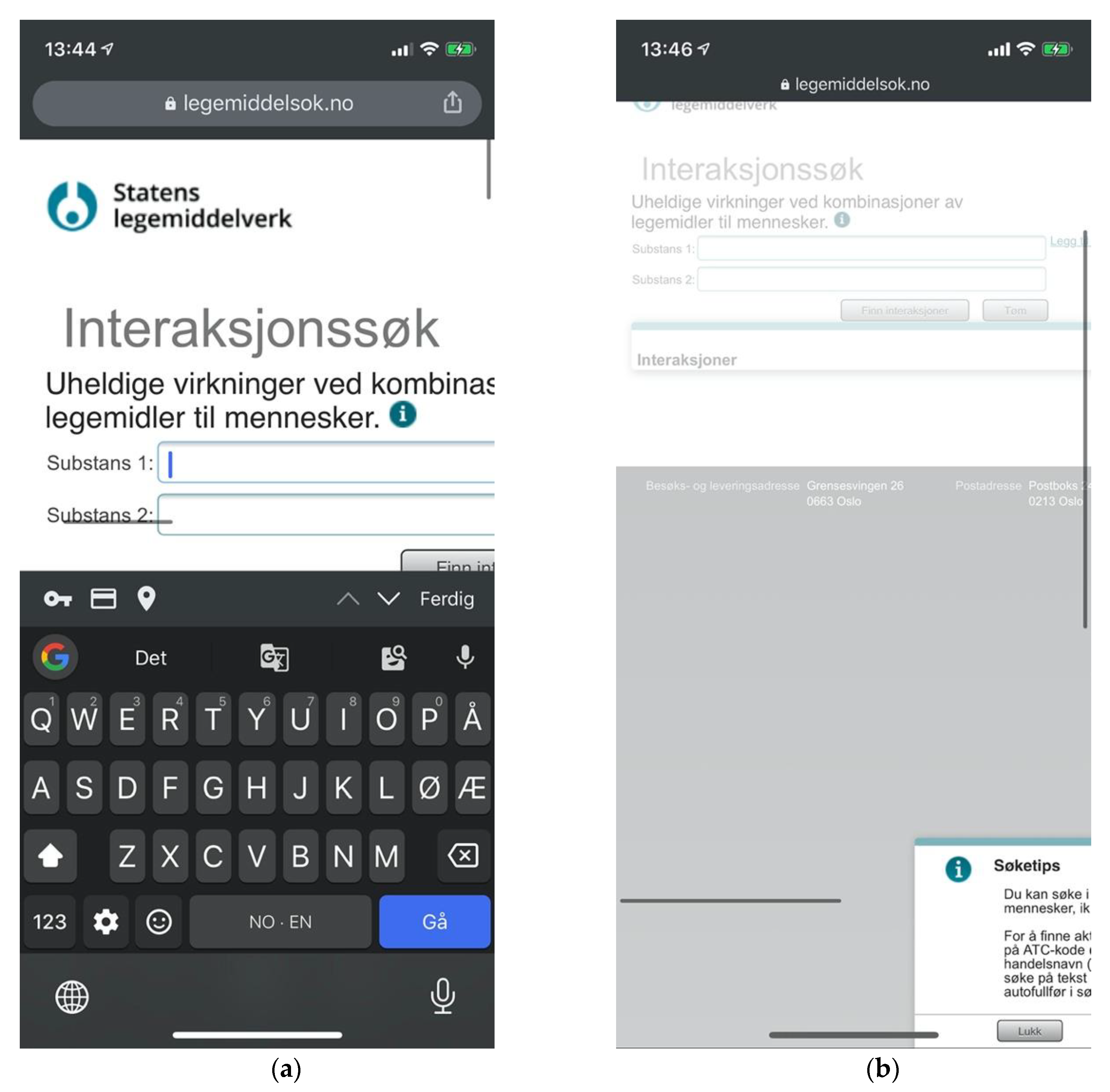
Figure 14.
(a) Issues of viewport handling prevent usability at Legemiddelsok.no, and no welcoming instructions are provided; (b) “Search tips” modal panel sticking outside the viewport.
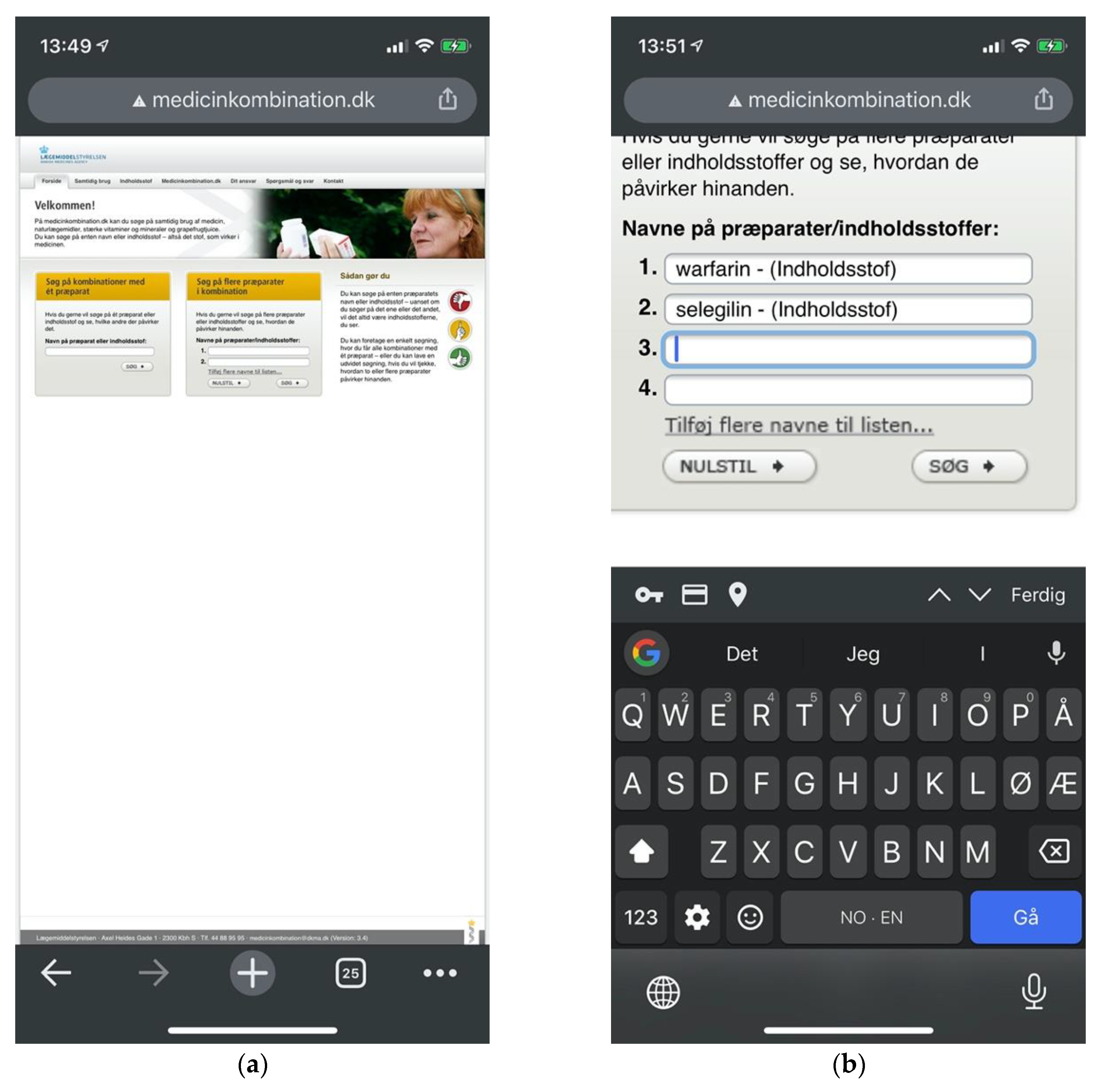
Figure 15.
(a) Medicinkombination.dk lacking adaptive design in spite of an explicit layperson audience; (b) Multi-drug searches require users to manually add input fields one by one.
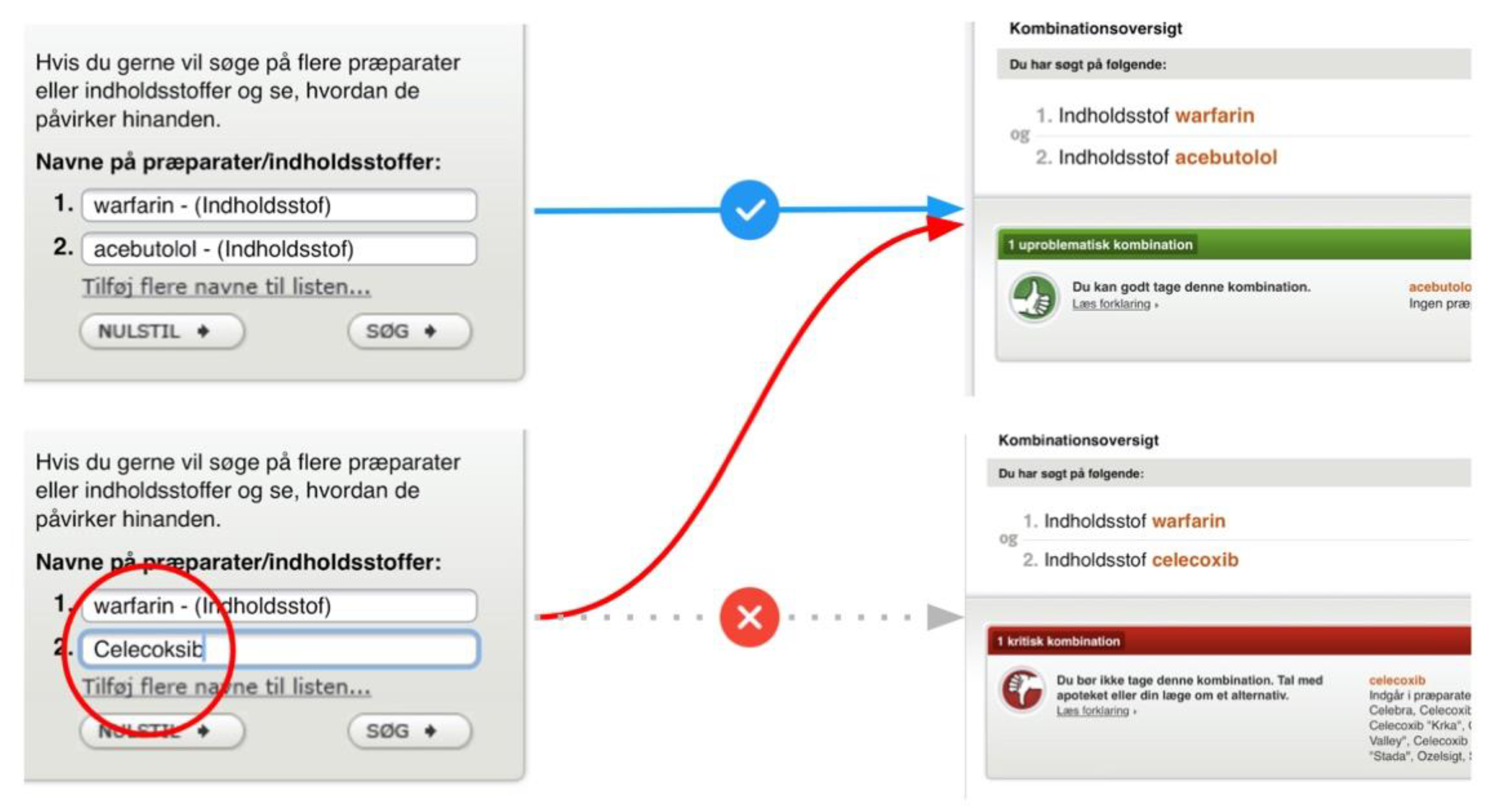
Figure 16.
(a) A green indicator for interaction analysis of warfarin indicating its safety; (b) Visually de-emphasized and unlabeled indicator for 347 drug interactions pertaining to warfarin.
Figure 17.
Medicinkombination.dk providing previous results for a current search.
Table 1.
Goal-oriented tasks applied in heuristic evaluations.
| Task No. | Description |
|---|
| Task 1 | Find out whether drug X and drug Y produce adverse interactions. |
| Task 2 | Find out which adverse reactions drug X may produce.
(i.e., with or without any other drug or substance.) |
| Task 3 | Find out which adverse drug interactions a patient is exposed to, based on a list of multiple drugs. |
Table 2.
Drug pairs applied in evaluated tasks.
| Pair No. | Drug X | Drug Y |
|---|
| Pair 1: | Simvastatin | Itraconazole |
| Pair 2: | Warfarin | Gemfibrozil |
| Pair 3: | Levothyroxine | Warfarin |
| Pair 4: | Fluoxetine | Selegiline |
| Pair 5: | Selegiline | Phenelzine |
| Pair 6: | Cholecalciferol | Paracetamol |
Table 3.
Nielsen’s Usability Heuristics, based on Nielsen [
23].
| Identifier | Description |
|---|
| H1 | Visibility of System Status |
| H2 | Match Between System and the Real World |
| H3 | User Control and Freedom |
| H4 | Consistency and Standards |
| H5 | Error Prevention |
| H6 | Recognition Rather than Recall |
| H7 | Flexibility and Efficiency of Use |
| H8 | Aesthetic and Minimalist Design |
| H9 | Help Users Recognize, Diagnose, and Recover from Errors |
| H10 | Help and Documentation |
Table 4.
Scheme of severity rating applied, following Nielsen [
32].
| Rating | Description |
|---|
| 0 | I don’t agree that this is a usability problem at all. |
| 1 | Cosmetic problem only: need not be fixed unless extra time is available. |
| 2 | Minor usability problem: fixing this should be given low priority. |
| 3 | Major usability problem: important to fix, so should be given high priority. |
| 4 | Usability catastrophe: imperative to fix this before product can be released. |
Table 5.
The drug interaction checkers sampled for the study.
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).