Abstract
(1) Background: For decades, the temperaments of infants and small children have been a focus of studies in human development and been seen as a potential contributor to children’s developmental patterns. However, less is known about the interplay between the temperamental characteristics of mothers and their children in the context of explaining variations in developmental outcomes. The aim of our study was to explore the associations—with or without genetic links—of the temperaments and psychological distress of mothers and the temperaments of children with behavioral problems in a group of internationally adopted children and their adoptive mothers and in a group of non-adopted children and their mothers. (2) Methods: Data (n = 170) were derived from the ongoing Finnish Adoption (FinAdo) follow-up study. The children included were under the age of 7 years; 74 were adopted internationally through legal agencies between October 2010 and December 2016, and the remaining 96 were non-adopted children living with their birth parents (biological group) recruited from day-care centers. We used Mary Rothbart’s temperament questionnaires to assess temperament, the Child Behavior Checklist (CBCL) to obtain data on the children’s behavioral/emotional problems and competencies, and the General Health Questionnaire (GHQ) to assess parental psychological distress. The study was approved by the Ethics Committee of the Hospital District of Southwest Finland, and written informed consent was obtained from the parents and the children themselves. (3) Results: The negative affectivities of both mothers and children were associated with the total CBCL and with both internalizing and externalizing problem behaviors after adjusting for age, gender, and adoption status. Both relationships remained significant when tested simultaneously, suggesting additive effects. Maternal negative affect was associated with problem behavior irrespective of child extraversion/surgency. Child extraversion/surgency was associated with lower levels of all internalizing behavioral problems when adjusted for maternal sociability. Child negative affect was associated with all behavioral problem measures irrespective of maternal sociability or maternal psychological distress. Maternal distress was associated with child problem behaviors only in children with low extraversion/surgency. (4) Limitations: The sample size was relatively small, and the information was gathered solely with questionnaires. (5) Conclusions: The results of the study may be clinically significant. Child negative affect, maternal negative affect, and maternal experienced distress, combined with low child extraversion/surgency, may increase the risk of child problem behaviors in both adoptees and non-adoptees.
1. Introduction
Temperament has been described as individual differences in reactivity and self-regulation that are constitutionally based, appear early, and are influenced over time by heredity, maturation, and experience [1]. More recent research offers an alternative definition: “Temperament traits are early emerging basic dispositions in the domains of activity, affect, attention, and self-regulation, and these dispositions are the product of complex interactions among genetic, biological, and environmental factors across time” [2].
For decades, temperament in early life has been a focus of studies in human development and psychopathology in children and adolescents [3]. Individual differences in temperament reflect individual differences in central nervous system functioning and structure, and while there is a consistent body of evidence documenting the contributions of genotype to these differences, it has become increasingly clear that bioecological influences (e.g., nutrition) and environmental factors involving parenting styles and the nature of the home context can impose transgenerational effects [4,5].
Intergenerational transmission, a process through which an earlier generation influences parenting attitudes and behavior, genetically or otherwise, inevitably results in parent–offspring resemblance [6,7]. Although resemblance has been studied extensively in many areas of human functioning, studies into parent–offspring resemblance in personality are underrepresented [8], and resemblance has rarely been linked to underlying transmission mechanisms other than genetics [9,10].
Previous research has shown associations between child temperament, parenting, and child adjustment [11,12,13], and moreover, parental temperament traits have been found to predict especially externalizing problems in children [14,15,16]. In a recent study, Xing et al. assessed the combined effects of maternal personality and child temperamental reactivity on child externalizing behavioral problems [17]. In addition, disrupted attachment patterns and mismatches between behavioral expectations and the demands of peers or parents have been hypothesized to mediate the associations between child temperament and adjustment [12,18,19,20,21].
The mental well-being of adopted children has been addressed in previous studies; most adopted children are emotionally and behaviorally healthy but more likely than non-adoptees to receive mental health treatment. According to several studies, adopted children are referred for psychiatric treatment at a higher rate than their non-adopted peers [22,23], and in a meta-analysis of 11 studies, Askeland et al. [24] concluded that adopted adolescents experience more mental health problems.
The aim of our study was to explore the associations between child behavioral problems, the temperaments and psychological distress of mothers, and the temperaments of children. The study’s design, which included adoptees and biological children, enabled us to examine whether these associations depend on genetic links between mothers and children. We decided to focus on two temperamental characteristics, negative affect and extraversion/surgency, as these characteristics have been consistently associated with later psychological problems [25].
2. Methods
2.1. Participants
This study was part of the ongoing Finnish Adoption (FinAdo) study [26,27], which is a unique and extensive Finnish medical study of internationally adopted children. The aim is to produce new, nationally, and internationally significant information on the physical and mental health and psychosocial development of these children. This kind of study offers a distinctive view on the development of psychiatric and developmental disorders because an adopted child’s rearing environment is transformed, often drastically, after their early years, and the parents and children have no shared genes. The FinAdo 2 project is an ongoing, prospective clinical follow-up study, and invitations to participate were sent through the three legalized adoption agencies working in Finland to all families who had internationally adopted a child under the age of 7 years between October 2010 and December 2016. The non-adopted children were recruited from day-care centers in the cities of Turku and Kaarina in southwest Finland. This temperament sub-study was conducted using questionnaires that were completed by the adoptive and biological parents. Of the 170 children, 74 were adopted and 96 non-adopted; 98 were boys and 72 girls; and the mean age was 4.17 years (SD 1.62).
The current study was approved by the Ethics committee of the Hospital District of Southwest Finland, and written informed consent was obtained from the parents.
2.2. Measures
2.2.1. Temperament Characteristics
To assess child temperament, we used Mary Rothbart’s temperament questionnaires, specifically the Early Childhood Behavior Questionnaire (ECBQ) and the Children’s Behavior Questionnaire (CBQ) [28].
The ECBQ is a parent-report measure of temperament in children aged from 18 months to 3 years that assesses 18 dimensions of temperament (activity level/energy, attentional focusing, attentional shifting, cuddliness, discomfort, fear, frustration, high-intensity pleasure, impulsivity, inhibitory control, low-intensity pleasure, motor activation, perceptual sensitivity, positive anticipation, sadness, shyness, sociability, and soothability, which form three broad factors: surgency/extraversion, negative affect, and effortful control. A study by Putnam et al. [29] supports the reliability and validity of the ECBQ as a measure of varied and finely differentiated aspects of toddler temperament; the 18 scales were found to be internally consistent, and for most dimensions, different raters were consistent both with one another and across time. In our sample, the Cronbach’s’s alphas were 0.83 for negative affect and 0.79 for surgency/extraversion.
The CBQ was designed to measure temperament in children aged from 3 to 7 years and assesses 15 dimensions of temperament (activity level, anger/frustration, approach, attentional focusing, discomfort, falling reactivity and soothability, fear, high-intensity pleasure, impulsivity, inhibitory control, low-intensity pleasure, perceptual sensitivity, sadness, shyness, and smiling and laughter), which reliably form the same three factors as the ECBQ. Rothbart et al. [30] assessed the reliability and validity of the CBQ and concluded that its scales have adequate internal consistency and can be used in studies requiring a highly differentiated yet integrated measure of temperament. In our sample, the Cronbach’s’s alpha was 0.88 for negative affect and 0.91 for surgency/extraversion.
Maternal temperament was measured using the Emotionality–Activity–Sociability Temperament Survey [31] The questionnaire consists of 27 items on a 5-point scale of (1) totally disagree to (5) totally agree. Negative emotionality includes two components, anger and fear, which were measured with 12 items. Sociability was measured with five items. The Cronbach’s’s alphas were 0.81 for sociability and 0.78 for negative emotionality. Good psychometric properties have been reported in other studies [32,33].
2.2.2. Parental Psychological Distress
The General Health Questionnaire (GHQ) is a self-administered screening questionnaire designed for use in consulting settings to detect individuals with diagnosable psychiatric disorders [34]. The most extensively used screening instrument for common mental disorders is the 12-item GHQ (GHQ-12). Various versions of the GHQ-12 have been reported to be useful in determining the presence of depression and to have good constructive validity [35]. The Cronbach’s alpha for our sample was 0.87.
2.2.3. Behavioral Problems
To assess child behavioral problems, we used two CBCL questionnaires: the CBCL for ages 18 months to 5 years, which has 100 questions, and the CBCL for ages 6 to 18 years, which has 113 questions, excluding 5 open-ended questions. These questionnaires produce scores on the same dimensions and are thus comparable and age-adjusted. Each question is answered as (0) not true, (1) somewhat or sometimes true, or (2) very true or often true. The CBCL provides a total score for behavioral characteristics and separate scores for internalizing and externalizing behavioral symptoms. The total CBCL score was calculated by summing up all items. The higher a child’s scores on the CBCL, the more behavioral problems the child has [36]. The Cronbach’s alphas in our sample were as follows: CBCL total score, 0.93; internalizing problems, 0.82; externalizing problems, 0.88.
2.2.4. Child-Related Background Factors
The child-related variables included the child’s adoption status (internationally adopted or not adopted), gender, age at adoption (if applicable), and age at the date of completing the questionnaire.
2.2.5. Statistical Analyses
Differences in child and maternal temperamental characteristics, child problem behaviors, and maternal distress according to the adoption status were examined using Student’s t-test. The associations of child problem behaviors with maternal temperamental characteristics, maternal distress, and child temperamental characteristics were examined using linear regression analyses. Maternal temperamental characteristics, maternal distress, and child temperamental characteristics were inserted into the same regression model to test the possible additive nature of the associations. In a separate model, an interaction term between maternal temperamental characteristics or distress and child temperamental characteristics was inserted to examine possible interaction effects. In all analyses, adoption status, gender, and age were used as covariates. The associations are presented as regression coefficients (b) and standard errors (se). All analyses were performed using Stata 17.0. Mediation analyses were conducted using structural equation modeling and Medsem package [37].
3. Results
Descriptive statistics for the study sample are shown in Table 1.

Table 1.
Descriptive statistics.
There were no significant differences in the temperamental dimensions between adopted and non-adopted children. Mothers of adopted children reported more externalizing behaviors than mothers of non-adopted children. The effect sizes ranged from small (0.02) to moderate (0.49). These are shown in Table 2.

Table 2.
Comparison of descriptive statistics according to adoption status.
The coefficients of the correlations between maternal temperament, child temperament, and child problem behaviors are shown in Table 3. Child negative affect was associated with higher levels of behavioral problems, and there was a negative correlation between child extraversion/surgency and child internalizing symptoms. Higher maternal negative affect was associated with higher levels of maternal psychological distress.

Table 3.
Correlation coefficients between the dependent and independent study variables.
The associations of maternal negative affect and child temperament characteristics with child problem behavior are shown in Table 4. Maternal and child negative affect were associated with the total CBCL, internalizing problem behaviors, and externalizing problem behaviors, and the relationships with total and external problem behaviors remained significant when tested simultaneously, suggesting an additive effect. In the model in which the relationships of child problem behaviors with maternal negative affect and child extraversion/surgency were examined, higher maternal negative affect was again associated with higher total, internal, and external problem behaviors. Higher child extraversion/surgency was associated with lower internal, but not total or external, problem behaviors. Maternal negative affect was associated with all child problem behavior measurements irrespective of child extraversion/surgency. No interaction effects in the association of maternal negative affect and child temperament characteristics with child problem behaviors were found.

Table 4.
The associations between maternal and child negative affect and child problem behavior.
The simultaneous associations of child problem behaviors with maternal sociability and child temperament characteristics are shown in Table 5. Whereas maternal and child extraversion/surgency were not associated with the total CBCL, higher child extraversion/surgency was associated with lower internal problem behaviors, and higher maternal sociability was associated with lower child external problem behaviors. Higher maternal extraversion/surgency was associated with lower total and externalizing problem behaviors irrespective of child negative affect. Child negative affect was associated with all problem behavior measures irrespective of maternal sociability. No interaction effects between maternal sociability and child temperament characteristics were found.

Table 5.
The associations between maternal and child extraversion/surgency with child problem behavior.
The associations of child problem behaviors with maternal psychological distress and child temperament characteristics are shown in Table 6. Maternal distress was associated with all problem behavior measures irrespective of child extraversion/surgency, and child extraversion/surgency was associated with lower internalizing problems even when adjusted for maternal distress. Child negative affect was associated with all problem behavior measures irrespective of maternal distress, but in contrast, there was no association between maternal psychological distress and child problem behaviors when examined together with child negative affect. An interaction effect suggesting a cross-over interaction of child problem behavior with maternal psychological distress and child surgency was found (Figure 1), and maternal distress was thus associated with problem behavior only in children with low surgency.

Table 6.
The association between maternal psychological distress and child temperamental characteristics with child problem behavior.
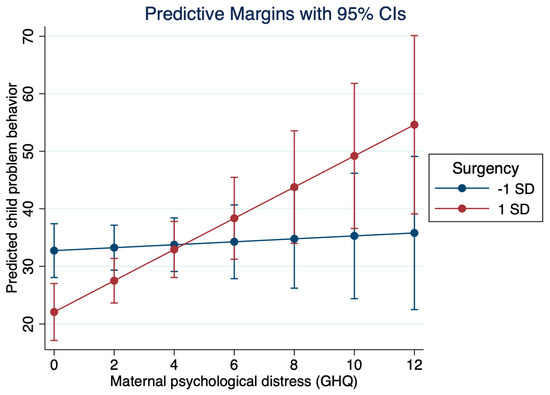
Figure 1.
Interaction of child problem behavior and maternal psychological distress.
Last, in a multivariate model, the associations between child and maternal temperamental characteristics and maternal distress with child problem behaviors were examined (Table 7). The results of these analyses showed that child negative affect was consistently associated with child problem behaviors. The interaction term between adoption status and the independent variables (child and maternal temperamental characteristics and maternal distress) was not statistically significant (p-values > 0.05) suggesting that the adoption status did not modify the associations of child and maternal temperamental characteristics and maternal distress with child problem behaviors.

Table 7.
The multivariate associations of child and maternal temperamental characteristics and maternal distress with child problem behaviors.
As sensitivity analyses, we tested whether child temperament traits would mediate the associations between maternal traits and child behavioral problems. Child negative affect mediated (z = 2.95, p < 0.01, 26% of total effect mediated) the association between maternal negative affect and child problem behavior (total score). None of the other mediation effects tested were statistically significant.
4. Discussion
The aim of our study was to explore the associations of child behavioral problems with the temperament and psychological distress of mothers and the temperament of children and to examine whether these associations are dependent on genetic links between mothers and children.
The results indicate that child temperamental traits are associated with behavioral problems in children, and controlling for adoption status did not change the results of the analyses, suggesting that the relationships apply equally to adopted children In univariable analyses, maternal negative affect and maternal distress also were associated with child problem behavior irrespective of child extraversion/surgency. However, in multivariable analyses, maternal psychological distress was associated with child problem behaviors only in children with low extraversion/surgency. In multivariable analyses, maternal lower sociability was associated with child externalizing behavioral problems, but maternal negative affect was not associated with child problem behavior. Low child extraversion/surgency was associated with internalizing behavioral problems Altogether, child negative affect, maternal low sociability, and low child extraversion/surgency may increase the risk of child problem behaviors in both adoptees and non-adoptees. Our sensitivity analyses suggested, however, that maternal negative affect may have an indirect effect on child problem behaviors through child negative affect.
Parents have an extensive influence on the children they raise. Parenting is culturally influenced, and therefore cultural differences in temperament can be anticipated [38], and in this regard, our study design is interesting: we could test whether the associations were affected by adoption status and thus explained by a shared genetic background. As stated earlier, individual differences in personality development have been shown to be predictive of the risk of and resilience to psychopathology [11,12,13], and Lunansky et al. [39] have proposed a personality–resilience–psychopathology model. Previous studies have shown that negative emotionality, effortful control, and surgency-related traits, such as impulsivity and behavioral inhibition, may contribute to the manifestation of both internalizing and externalizing problems in childhood [40,41,42,43]. The results of our study suggested the same, and moreover, the trait of extraversion/surgency seems to have a protective function.
Adoptees have often been exposed to childhood trauma, such as neglect, family violence, physical and sexual abuse, placement instability, and institutionalized care, which increase the risk for attachment difficulties, posttraumatic stress disorder, and other psychiatric disorders [24,44]. These early experiences of deprivation are strong predictors of later psychopathology [45,46], and it could therefore be argued that temperamental differences play a less significant role for adopted children, but our study suggests that the temperamental characteristics of adopted children and their adoptive mothers do influence the children’s mental health.
Numerous studies have examined personality similarities between peers and romantic partners (e.g., [47]), but little is known regarding personality similarities between parents and offspring [48], and few previous studies have examined those similarities and their role in child development [4,13,49]. Franken et al. [48] investigated the impact of parent–offspring personality similarities on adolescent externalizing problems and found that child and parent personalities equally impact the development of externalizing problems during late adolescence. Two earlier studies [4,49] suggested that parent and offspring personality similarities might play an important role in child development, and both studies indicated that when similarity was a significant factor, it was associated with fewer externalizing problems. n a study by Rettew et al. [13], who examined the goodness-of-fit hypothesis regarding child–parent temperament and psychopathology, the interactions of the child and parent temperament dimensions were noteworthy additional predictors of childhood psychopathology. The interactions between the child and parent temperament dimensions predicted higher levels of externalizing, internalizing, and attention problems beyond the effects of these dimensions alone, and the authors concluded that the effect of child temperament upon child psychopathology can be dependent on parent temperament and that the effect of parent temperament can be dependent on child temperament [13]. The results of our sensitivity analyses indicated an indirect effect of maternal negative affect on child problem behavior through child negative affect and thus support previous studies. Furthermore, we concluded that maternal lower sociability was associated with child externalizing behavior.
The fact that temperamental differences affect psychological development irrespective of a genetic link is of importance to adoptive parents and their children, and the results of our study can thus be considered clinically significant.
Strengths and Weaknesses
The major limitation of our study is the relatively small sample size (N = 170). An additional limitation is data collection using questionnaires, which meant that the assessments of behavioral problems, child temperament, maternal temperament, and maternal psychological distress were based solely on maternal reports. Furthermore, as the vast majority of the respondents were mothers, we were unable to assess any potential differences between mothers’ and fathers’ reports. Further studies would benefit from integrating the perspectives of multiple informants (e.g., fathers, teachers).
The major strengths of our study are the use of well-established and widely used measures (CBCL, GHQ, ECBQ, CBQ, and EAS) and the ability to consider the genetic links between parents and children. To our knowledge, this is the first study to assess the associations of child and maternal temperament with psychological well-being in both adoptive and non-adoptive families.
5. Conclusions
Our study suggests that certain temperamental features of children and mothers may impact the psychological development and well-being of children. Because adopted children are at a heightened risk of mental health problems, it is important to acknowledge any factors that may affect their psychological development.
The results of our study help to identify those children who are at risk to develop behavioral problems. The risk is increased when maternal psychological distress is combined with low extraversion/surgency in the child and in the case of maternal and child negative affect, especially when mother and child share this trait. We are unable to change a child’s temperament, but when there is a risk of externalizing behavior, early interventions, such as Incredible Years, are available. These interventions have been studied and shown to be effective [50].
Author Contributions
M.E. and H.L. were responsible for the study concept and design. M.E., H.L. and H.R. and contributed to the data acquisition. C.H. and M.E. performed the statistical analyses. K.L. provided the first version of the manuscript. All authors provided critical revision of the manuscript, reviewed the content, and approved the final version of this manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Krista Liskola received a grant of EUR 6000 from the Ane and Signe Gyllenberg Foundation in 2019, which partly relates to the research reported in this article. Krista Liskola also received a grant of EUR 8000 from the Päivikki and Sakari Sohlberg Foundation in 2021 and a grant of EUR 6000 from the Finnish Brain Foundation in 2021. The Ane and Signe Gyllenberg Foundation, Päivikki and Sakari Sohlberg Foundation, and Finnish Brain Foundation had no role in either the gathering or the interpretation of the data presented in this article. Marko Elovainio was supported by the Academy of Finland (339390). Helena Lapinleimu received support for all FinAdo study phases from the Foundation of Pediatric Research, Finland, the Signe and Ane Gyllenberg Foundation, and the EVO Grant from Turku University Hospital.
Institutional Review Board Statement
The study was approved by the Ethics Committee of the Hospital District of Southwest Finland (Dnro 102/180/2012), and written informed consent was obtained from the parents and the children themselves.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data and the analytical code are available from the corresponding author upon reasonable request.
Acknowledgments
The authors are thankful to all the internationally adopted children and their parents for their participation in this study. M.E. was supported by the Academy of Finland (339390). K.L. was supported by the Ane and Signe Gyllenberg Foundation, the Päivikki and Sakari Sohlberg Foundation and the Finnish Brain Foundation. H.L. received support for all FinAdo study phases from the Foundation of Pediatric Research, Finland, the Signe and Ane Gyllenberg Foundation, and the EVO Grant from Turku University Hospital.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rothbart, M.; Derryberry, D. Development of Individual Differences in Temperament. Adv. Dev. Psychol. 1981, 1, 37–86. [Google Scholar]
- Shiner, R.L.; Buss, K.A.; Mcclowry, S.G.; Putnam, S.P.; Saudino, K.J.; Zentner, M. What Is Temperament Now? Assessing Progress Temperament Research on the Twenty-Fifth Anniversary of Goldsmith et Al. Child Dev. Perspect. 2012, 6, 436–444. [Google Scholar] [CrossRef]
- de Pauw, S.S.W.; Mervielde, I. Temperament, Personality and Developmental Psychopathology: A Review Based on the Conceptual Dimensions Underlying Childhood Traits. Child Psychiatry Hum. Dev. 2010, 41, 313–329. [Google Scholar] [CrossRef]
- Langenhof, M.R.; Komdeur, J.; Oldehinkel, A.J. Effects of Parenting Quality on Adolescents’ Personality Resemblance to Their Parents. The TRAILS Study. J. Adolesc. 2016, 51, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Wachs, T.D. Relevance of Physical Environment Influences for Toddler Temperament. Infant Behav. Dev. 1988, 11, 431–445. [Google Scholar] [CrossRef]
- van Ijzendoorn, M.H. Intergenerational Transmission of Parenting: A Review of Studies in Nonclinical Populations. Dev. Rev. 1992, 12, 76–99. [Google Scholar] [CrossRef]
- Mameli, M. Nongenetic Selection and Nongenetic Inheritance. Br. J. Philos. Sci. 2004, 55, 35–71. [Google Scholar] [CrossRef]
- Eley, T.C.; McAdams, T.A.; Rijsdijk, F.V.; Lichtenstein, P.; Narusyte, J.; Reiss, D.; Spotts, E.L.; Ganiban, J.M.; Neiderhiser, J.M. The Intergenerational Transmission of Anxiety: A Children-of-Twins Study. Am. J. Psychiatry 2015, 172, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, T.J.; Loehlin, J.C. Genes, Evolution, and Personality. Behav. Genet. 2001, 31, 243–273. [Google Scholar] [CrossRef] [PubMed]
- Silberg, J.L.; Eaves, L.J. Analysing the Contributions of Genes and Parent-Child Interaction to Childhood Behavioral and Emotional Problems: A Model for the Children of Twins. Psychol. Med. 2004, 34, 347–356. [Google Scholar] [CrossRef]
- McFadyen-Ketchum, S.A.; Bates, J.E.; Dodge, K.A.; Pettit, G.S. Patterns of Change in Early Childhood Aggressive-Disruptive Behavior: Gender Differences in Predictions from Early Coercive and Affectionate Mother-Child Interactions. Child Dev. 1996, 67, 2417–2433. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.L.; Bates, J.E.; Sandy, J.M.; Lanthier, R. Early Developmental Precursors of Externalizing Behavior in Middle Childhood and Adolescence. J. Abnorm. Child Psychol. 2000, 28, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Rettew, D.C.; Stanger, C.; McKee, L.; Doyle, A.; Hudziak, J.J. Interactions between Child and Parent Temperament and Child Behavior Problems. Compr. Psychiatry 2006, 47, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Prinzie, P.; Onghena, P.; Hellinckx, W.; Grietens, H.; Ghesquière, P.; Colpin, H. Direct and Indirect Relationships between Parental Personality and Externalising Behaviour: The Role of Negative Parenting. Psychol. Belg. 2005, 45, 123–145. [Google Scholar] [CrossRef]
- Oliver, P.H.; Guerin, D.W.; Coffman, J.K. Big Five Parental Personality Traits, Parenting Behaviors, and Adolescent Behavior Problems: A Mediation Model. Personal. Individ. Differ. 2009, 47, 631–636. [Google Scholar] [CrossRef]
- Koutra, K.; Roumeliotaki, T.; Kyriklaki, A.; Kampouri, M.; Sarri, K.; Vassilaki, M.; Bitsios, P.; Kogevinas, M.; Chatzi, L. Maternal Depression and Personality Traits in Association with Child Neuropsychological and Behavioral Development in Preschool Years: Mother-Child Cohort (Rhea Study) in Crete, Greece. J. Affect. Disord. 2017, 217, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Xing, S.; Gao, X.; Liu, X.; Ma, Y.; Wang, Z. Maternal Personality and Child Temperamental Reactivity: Differential Susceptibility for Child Externalizing Behavioral Problems in China. Front. Psychol. 2018, 9, 1952. [Google Scholar] [CrossRef] [PubMed]
- Bates, J.E.; Bayles, K.; Bennett, D.S.; Ridge, B.; Brown, M.M. Origins of Externalizing Behavior Problems at Eight Years of Age. Dev. Treat. Child. Aggress. 1991, 17, 93–120. [Google Scholar]
- Clark, L.A.; Kochanska, G.; Ready, R. Mothers’ Personality and Its Interaction with Child Temperament as Predictors of Parenting Behavior. J. Personal. Soc. Psychol. 2000, 79, 274–285. [Google Scholar] [CrossRef]
- Hooley, J.M.; Hiller, J.B. Personality and Expressed Emotion. J. Abnorm. Psychol. 2000, 109, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Lieb, R.; Wittchen, H.U.; Höfler, M.; Fuetsch, M.; Stein, M.B.; Merikangas, K.R. Parental Psychopathology, Parenting Styles, and the Risk of Social Phobia in Offspring: A Prospective-Longitudinal Community Study. Arch. Gen. Psychiatry 2000, 57, 859–866. [Google Scholar] [CrossRef]
- Fisher, A.P. Still “Not Quite as Good as Having Your Own”? Toward a Sociology of Adoption. Annu. Rev. Sociol. 2003, 29, 335–361. [Google Scholar] [CrossRef]
- Graff, H.J.; Siersma, V.D.; Kragstrup, J.; Petersson, B. Increased Health-Care Utilisation in International Adoptees. Dan. Med. J. 2015, 62, A5111. [Google Scholar] [PubMed]
- Askeland, K.G.; Hysing, M.; la Greca, A.M.; Aarø, L.E.; Tell, G.S.; Sivertsen, B. Mental Health in Internationally Adopted Adolescents: A Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Rothbart, M.K.; Evans, D.E.; Ahadi, S.A. Temperament and Personality: Origins and Outcomes. J. Personal. Soc. Psychol. 2000, 78, 122–135. [Google Scholar] [CrossRef]
- Raaska, H.; Elovainio, M.; Sinkkonen, J.; Matomäki, J.; Mäkipää, S.; Lapinleimu, H. Internationally Adopted Children in Finland: Parental Evaluations of Symptoms of Reactive Attachment Disorder and Learning Difficulties—FINADO Study. Child Care Health Dev. 2012, 38, 697–705. [Google Scholar] [CrossRef]
- Raaska, H.; Lapinleimu, H.; Sinkkonen, J.; Salmivalli, C.; Matomäki, J.; Mäkipää, S.; Elovainio, M. Experiences of School Bullying among Internationally Adopted Children: Results from the Finnish Adoption (FINADO) Study. Child Psychiatry Hum. Dev. 2012, 43, 592–611. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.E.; Rothbart, M.K. Developing a Model for Adult Temperament. J. Res. Personal. 2007, 41, 868–888. [Google Scholar] [CrossRef]
- Putnam, S.P.; Gartstein, M.A.; Rothbart, M.K. Measurement of Fine-Grained Aspects of Toddler Temperament: The Early Childhood Behavior Questionnaire. Infant Behav. Dev. 2006, 29, 386–401. [Google Scholar] [CrossRef] [PubMed]
- Rothbart, M.K.; Ahadi, S.A.; Hershey, K.L.; Fisher, P. Investigations of Temperament at Three to Seven Years: The Children’s Behavior Questionnaire. Child Dev. 2001, 72, 1394–1408. [Google Scholar] [CrossRef] [PubMed]
- Strelau, J.; Angleitner, A. Explorations in Temperament: International Perspectives on Theory and Measurement. In Perspectives on Individual Differences; Springer: Berlin/Heidelberg, Germany, 1991. [Google Scholar]
- Nærde, A.; Røysamb, E.; Tambs, K. Temperament in Adults—Reliability, Stability, and Factor Structure of the EAS Temperament Survey. J. Personal. Assess. 2004, 82, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Elovainio, M.; Jokela, M.; Rosenström, T.; Pulkki-Råbäck, L.; Hakulinen, C.; Josefsson, K.; Hintsanen, M.; Hintsa, T.; Raitakari, O.T.; Keltikangas-Järvinen, L. Temperament and Depressive Symptoms: What Is the Direction of the Associatioň. J. Affect. Disord. 2015, 170, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.P.; Hillier, V.F. A Scaled Version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Elovanio, M.; Hakulinen, C.; Pulkki-Råback, L.; Aalto, A.M.; Virtanen, M.; Partonen, T.; Suvisaari, J. General Health Questionnaire (GHQ-12), Beck Depression Inventory (BDI-6), and Mental Health Index (MHI-5): Psychometric and Predictive Properties in a Finnish Population-Based Sample. Psychiatry Res. 2020, 289, 112973. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Ruffle, T.M. The Child Behavior Checklist and Related Forms for Assessing Behavioral/Emotional Problems and Competencies. Pediatr. Rev. 2000, 21, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Mehmetoglu, M. Medsem: A Stata Package for Statistical Mediation Analysis. Int. J. Comput. Econ. Econom. 2018, 8, 63. [Google Scholar] [CrossRef]
- Gartstein, M.A.; Gonzalez, C.; Carranza, J.A.; Ahadi, S.A.; Ye, R.; Rothbart, M.K.; Yang, S.W. Studying Cross-Cultural Differences in the Development of Infant Temperament: People’s Republic of China, the United States of America, and Spain. Child Psychiatry Hum. Dev. 2006, 37, 145–161. [Google Scholar] [CrossRef] [PubMed]
- Lunansky, G.; van Borkulo, C.; Borsboom, D. Personality, Resilience, and Psychopathology: A Model for the Interaction between Slow and Fast Network Processes in the Context of Mental Health. Eur. J. Personal. 2020, 34, 969–987. [Google Scholar] [CrossRef]
- Hankin, B.L.; Davis, E.P.; Snyder, H.; Young, J.F.; Glynn, L.M.; Sandman, C.A. Temperament Factors and Dimensional, Latent Bifactor Models of Child Psychopathology: Transdiagnostic and Specific Associations in Two Youth Samples. Psychiatry Res. 2017, 252, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Tackett, J.L.; Lahey, B.B.; van Hulle, C.; Waldman, I.; Krueger, R.F.; Rathouz, P.J. Common Genetic Influences on Negative Emotionality and a General Psychopathology Factor in Childhood and Adolescence. J. Abnorm. Psychol. 2013, 122, 1142–1153. [Google Scholar] [CrossRef]
- Shields, A.N.; Reardon, K.W.; Brandes, C.M.; Tackett, J.L. The p Factor in Children: Relationships with Executive Functions and Effortful Control. J. Res. Personal. 2019, 82, 103853. [Google Scholar] [CrossRef]
- Olino, T.M.; Dougherty, L.R.; Bufferd, S.J.; Carlson, G.A.; Klein, D.N. Testing Models of Psychopathology in Preschool-Aged Children Using a Structured Interview-Based Assessment. J. Abnorm. Child Psychol. 2014, 42, 1201–1211. [Google Scholar] [CrossRef] [PubMed]
- Brodzinsky, D.; Gunnar, M.; Palacios, J. Adoption and Trauma: Risks, Recovery, and the Lived Experience of Adoption. Child Abus. Negl. 2021, 130, 105309. [Google Scholar] [CrossRef]
- Becker-Weidman, A. Effects of Early Maltreatment on Development: A Descriptive Study Using the Vineland Adaptive Behavior Scales-II. Child Welf. 2009, 88, 137–161. [Google Scholar]
- Gunnar, M.R.; Fisher, P.A.; Dozier, M.; Fox, N.; Levine, S.; Neal, C.; Pollak, S.; Plotsky, P.; Sanchez, M.; Vazquez, D. Bringing Basic Research on Early Experience and Stress Neurobiology to Bear on Preventive Interventions for Neglected and Maltreated Children. Dev. Psychopathol. 2006, 18, 651–677. [Google Scholar] [CrossRef] [PubMed]
- Robins, R.W.; Caspi, A.; Moffitt, T.E. Two Personalities, One Relationship: Both Partners’ Personality Traits Shape the Quality of Their Relationship. J. Personal. Soc. Psychol. 2000, 79, 251–259. [Google Scholar] [CrossRef]
- Franken, A.; Laceulle, O.M.; van Aken, M.A.G.; Ormel, J. Using Response Surface Analysis to Interpret the Impact of Parent–Offspring Personality Similarity on Adolescent Externalizing Problems. Eur. J. Personal. 2017, 31, 104–117. [Google Scholar] [CrossRef]
- van Tuijl, C.; Branje, S.J.T.; Dubas, J.S.; Vermulst, A.D.A.; van Aken, M.A.G. Parent-Offspring Similarity in Personality and Adolescents’ Problem Behaviour. Eur. J. Personal. 2005, 19, 51–68. [Google Scholar] [CrossRef]
- Overbeek, G.; van Aar, J.; de Castro, B.O.; Matthys, W.; Weeland, J.; Chhangur, R.R.; Leijten, P. Longer-Term Outcomes of the Incredible Years Parenting Intervention. Prev. Sci. 2021, 22, 419–431. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).