Craniofacial Growth at Age 6–11 Years after One-Stage Cleft Lip and Palate Repair: A Retrospective Comparative Study with Historical Controls
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants and Procedures
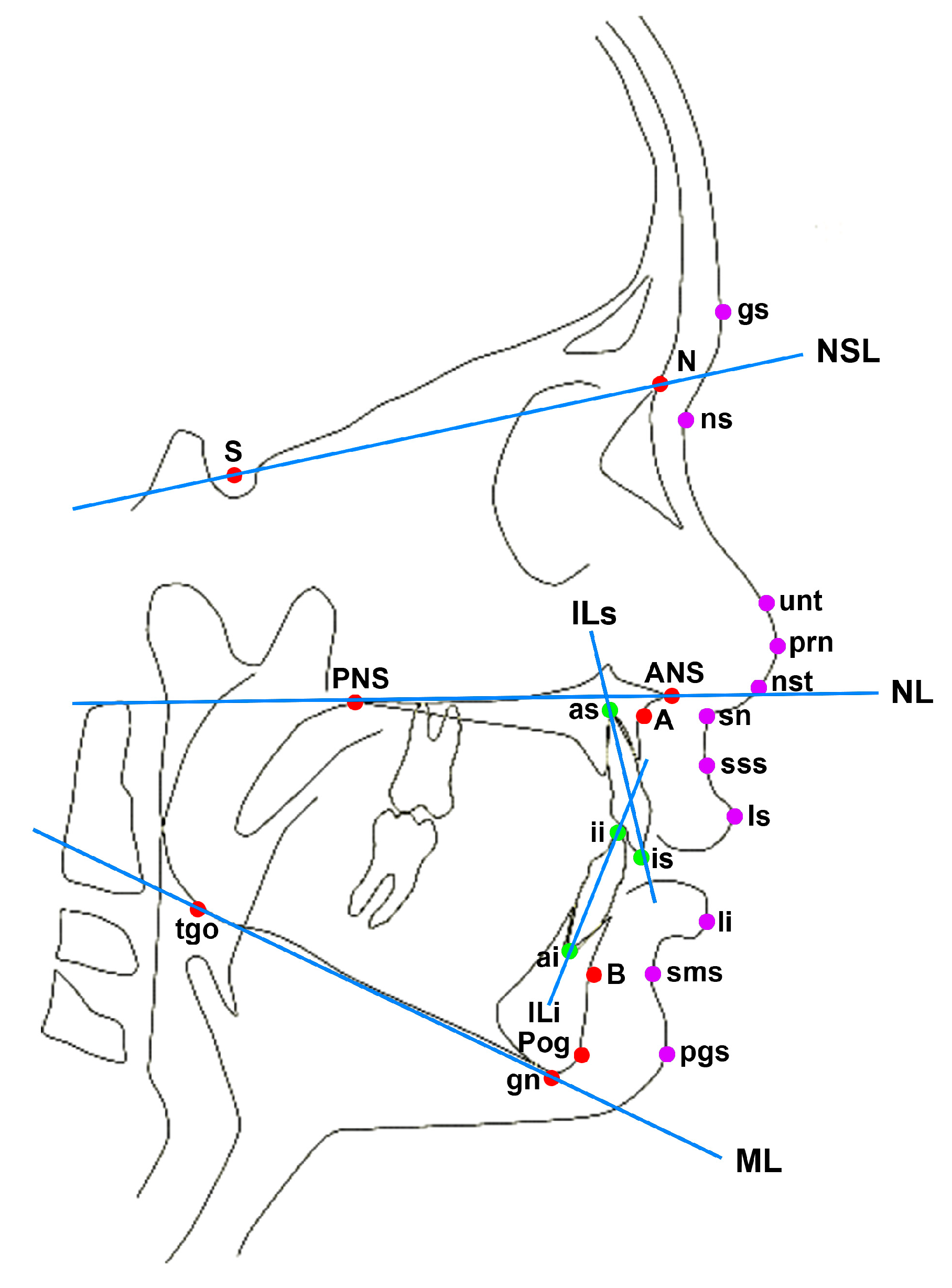
2.3. Outcome Variables, Data Sources and Measurements
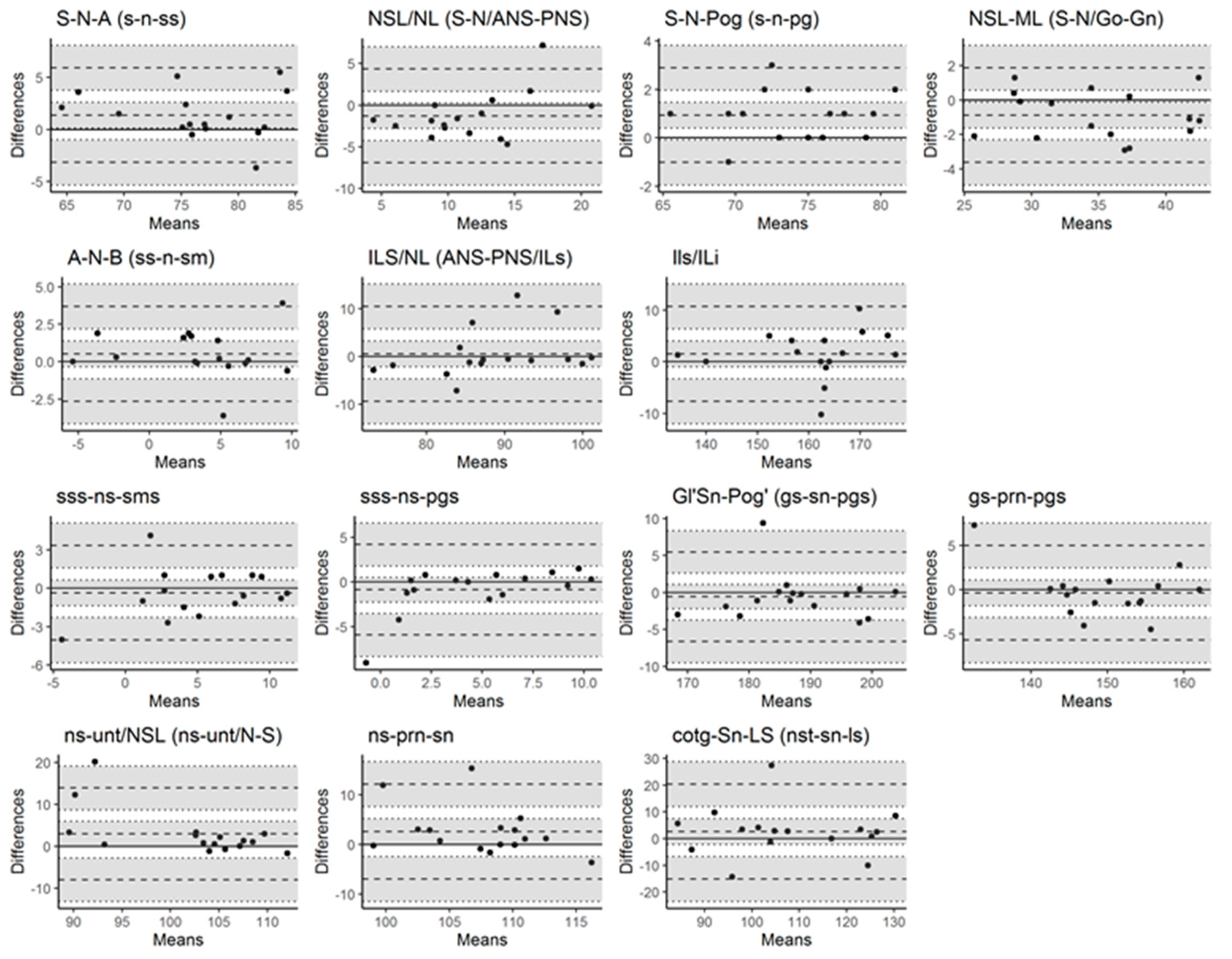
2.4. Statistical Methods
3. Results
3.1. Dental Arch Relationship and Palatal Morphology
3.2. Craniofacial Growth
4. Discussion
4.1. Clinical Relevance
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Group A (2003–2014) | Group B (1991–2002) | Group S (Slav-Cleft) | Healthy Control | |
|---|---|---|---|---|
| Hard tissue | ||||
| maxilla | S-N-A | S-N-A | s-n-ss (SNA) | A-N-S |
| NSL/NL | S-N/ANS-PNS | NSL/NL | N-S/ANS-PNS | |
| mandible | S-N-Pog | S-N-Pog | s-n-pg | PG-N-S |
| NSL/ML | S-N/Go-Gn | NSL/ML | N-S/GN-GO | |
| maxillomandibular | A-N-B | A-N-B | ss-n-sm (ANB) | A-N-B |
| ILs/NL | ANS-PNS/ILs | Ils/NL | UIE-UIA/PNS-ANS | |
| ILs/ILi | ILs/ILi | Ils/Ili | LIA -LIE/UIA -UIE | |
| Soft tissue | ||||
| maxillomandibular | sss-ns-sms | sss-ns-sms | sss-ns-sms | n/a |
| sss-ns-pgs | sss-ns-pgs | sss-ns-pgs | n/a | |
| gs-sn-pgs | gs-sn-pgs | gs-sn-pgs | n/a | |
| nasal profile | gs-prn-pgs | gs-prn-pgs | gs-prn-pgs | n/a |
| ns-unt/NSL | ns-unt/N-S | ns-unt/NSL | n/a | |
| ns-prn-sn | ns-prn-sn | ns-prn-sn | n/a | |
| nst-sn-ls | nst-sn-ls | nst-sn-ls | n/a | |
| ICC (95% CI) | ||
|---|---|---|
| Hard tissue | ||
| maxilla | S-N-A | 0.92 (0.8–0.97) |
| NSL/NL | 0.79 (0.5–0.92) | |
| mandible | S-N-Pog | 0.97 (0.92–0.99) |
| NSL/ML | 0.97 (0.91–0.99) | |
| maxillomandibular | A-N-B | 0.93 (0.81–0.98) |
| ILs/NL | 0.82 (0.56–0.93) | |
| ILs/ILi | 0.92 (0.78–0.97) | |
| Soft tissue | ||
| maxillomandibular | sss-ns-sms | 0.9 (0.74–0.96) |
| sss-ns-pgs | 0.76 (0.44–0.91) | |
| gs-sn-pgs | 0.95 (0.86–0.98) | |
| nasal profile | gs-prn-pgs | 0.93 (0.82–0.98) |
| ns-unt/NSL | 0.73 (0.39–0.9) | |
| ns-prn-sn | 0.57 (0.13–0.83) | |
| nst-sn-ls | 0.83 (0.58–0.94) | |
| n | Mean | n | Mean | Difference | p-Value | |
|---|---|---|---|---|---|---|
| S-N-A | ||||||
| Group A vs. Group B | 16 | 76.49 | 15 | 76 | 0.49 (−2.62–3.60) | 0.98 |
| Group A vs. Group S | 16 | 76.49 | 35 | 75.66 | 0.83 (−1.79–3.45) | 0.85 |
| Group A vs. Healthy control | 16 | 76.49 | 295 | 81.05 | −4.55 (−6.78–−2.33) | <0.001 |
| Group B vs. Group S | 15 | 76 | 35 | 75.66 | 0.34 (−2.34–3.02) | 0.99 |
| Group B vs. Healthy control | 15 | 76 | 295 | 81.05 | −5.05 (−7.34–−2.75) | <0.001 |
| Group S vs. Healthy control | 35 | 75.66 | 295 | 81.05 | −5.39 (−6.94–−3.83) | <0.001 |
| NSL/NL | ||||||
| Group A vs. Group B | 16 | 11.68 | 15 | 14 | −2.32 (−4.99–0.34) | 0.11 |
| Group A vs. Group S | 16 | 11.68 | 35 | 11.24 | 0.44 (−1.80–2.68) | 0.96 |
| Group A vs. Healthy control | 16 | 11.68 | 294 | 6.38 | 5.3 (3.40–7.20) | <0.001 |
| Group B vs. Group S | 15 | 14 | 35 | 11.24 | 2.76 (0.47–5.05) | 0.01 |
| Group B vs. Healthy control | 15 | 14 | 294 | 6.38 | 7.62 (5.66–9.58) | <0.001 |
| Group S vs. Healthy control | 35 | 11.24 | 294 | 6.38 | 4.86 (3.54–6.19) | <0.001 |
| S-N-Pog | ||||||
| Group A vs. Group B | 16 | 73.91 | 15 | 75 | −1.09 (−4.01–1.82) | 0.77 |
| Group A vs. Group S | 16 | 73.91 | 35 | 75.41 | −1.5 (−3.95–0.94) | 0.39 |
| Group A vs. Healthy control | 16 | 73.91 | 294 | 76.1 | −2.2 (−4.28–0.12) | 0.03 |
| Group B vs. Group S | 15 | 75 | 35 | 75.41 | −0.41 (−2.91–2.09) | 0.97 |
| Group B vs. Healthy control | 15 | 75 | 294 | 76.1 | −1.1 (−3.25–1.04) | 0.55 |
| Group S vs. Healthy control | 35 | 75.41 | 294 | 76.1 | −0.69 (−2.14–0.76) | 0.61 |
| A-N-B | ||||||
| Group A vs. Group B | 16 | 3.53 | 15 | 3 | 0.53 (−1.78–2.84) | 0.94 |
| Group A vs. Group S | 16 | 3.53 | 35 | 1.33 | 2.2 (0.26–4.14) | 0.02 |
| Group A vs. Healthy control | 16 | 3.53 | 294 | 4.78 | −1.25 (−2.90–0.40) | 0.21 |
| Group B vs. Group S | 15 | 3 | 35 | 1.33 | 1.67 (−0.31–3.65) | 0.13 |
| Group B vs. Healthy control | 15 | 3 | 294 | 4.78 | −1.78 (−3.48–0.08) | 0.04 |
| Group S vs. Healthy control | 35 | 1.33 | 294 | 4.78 | −3.45 (−4.60–−2.30) | <0.001 |
| ILs/NL | ||||||
| Group A vs. Group B | 16 | 88.53 | 15 | 103 | −14.47 (−21.96–−6.97) | <0.001 |
| Group A vs. Group S | 16 | 88.53 | 35 | 105.02 | −16.49 (−22.78–−10.20) | <0.001 |
| Group A vs. Healthy control | 16 | 88.53 | 294 | 107.25 | −18.72 (−24.07–−13.37) | <0.001 |
| Group B vs. Group S | 15 | 103 | 35 | 105.02 | −2.02 (−8.46–4.42) | 0.85 |
| Group B vs. Healthy control | 15 | 103 | 294 | 107.25 | −4.25 (−9.77–1.27) | 0.19 |
| Group S vs. Healthy control | 35 | 105.02 | 294 | 107.25 | −2.23 (−5.67–1.50) | 0.41 |
| ILs/ILi | ||||||
| Group A vs. Group B | 16 | 161.15 | 15 | 154 | 7.15 (−3.73–18.02) | 0.33 |
| Group A vs. Group S | 16 | 161.15 | 35 | 143.03 | 18.12 (8.98–27.25) | <0.001 |
| Group A vs. Healthy control | 16 | 161.15 | 293 | 131.75 | 29.4 (21.63–37.17) | <0.001 |
| Group B vs. Group S | 15 | 154 | 35 | 143.03 | 10.97 (1.63–20.31) | 0.01 |
| Group B vs. Healthy control | 15 | 154 | 293 | 131.75 | 22.25 (14.24–30.27) | <0.001 |
| Group S vs. Healthy control | 35 | 143.03 | 293 | 131.75 | 11.28 (5.87–16.70) | <0.001 |
| n | Mean | n | Mean | Difference | p-Value | |
|---|---|---|---|---|---|---|
| gs-sn-pgs | ||||||
| Group A vs. Group B | 16 | 187.87 | 15 | 187 | 0.87 (−5.57–7.40) | 0.95 |
| Group A vs. Group S | 16 | 187.87 | 35 | 173.54 | 14.33 (8.84–19.81) | <0.001 |
| Group B vs. Group S | 15 | 187 | 35 | 173.54 | 13.46 (7.85–19.07) | <0.001 |
| ns-unt/NSL | ||||||
| Group A vs. Group B | 16 | 102.38 | 15 | 107 | −4.63 (−9.15–0.10) | 0.044 |
| Group A vs. Group S | 16 | 102.38 | 35 | 105.91 | −3.54 (−7.33–0.26) | 0.07 |
| Group B vs. Group S | 15 | 107 | 35 | 105.91 | 1.09 (−2.79–4.97) | 0.78 |
References
- ReferencesShetye, P.R. Facial growth of adults with unoperated clefts. Clin. Plast. Surg. 2004, 31, 361–371. [Google Scholar] [CrossRef]
- Ross, R.B. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part 1: Treatment affecting growth. Cleft. Palate J. 1987, 24, 5–23. [Google Scholar]
- Markus, A.F.; Smith, W.P.; Delaire, J. Primary closure of cleft palate: A functional approach. Br. J. Oral. Maxillofac. Surg. 1993, 31, 71–77. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategies to Reduce the Health-Care Burden of Craniofacial Anomalies: Report of WHO Meetings on International Collaborative Research on Craniofacial Anomalies; World Health Organization: Geneva, Switzerland, 2002; pp. 1–148. [Google Scholar]
- Davila, A.A.; Holzmer, S.W.; Kubiak, J.; Martin, M.C. Anesthetic Exposure in Staged Versus Single-Stage Cleft Lip and Palate Repair. J. Craniofac. Surg. 2021, 32, 521–524. [Google Scholar] [CrossRef]
- Honigmann, K. One-stage closure of uni- and bilateral cleft lip and palate. Br. J. Oral. Maxillofac. Surg. 1996, 34, 214–219. [Google Scholar] [CrossRef]
- Benitez, B.K.; Brudnicki, A.; Surowiec, Z.; Singh, R.K.; Nalabothu, P.; Schumann, D.; Mueller, A.A. Continuous Circular Closure in Unilateral Cleft Lip and Plate Repair in One Surgery. J. Cranio Maxillofac. Surg. 2022, 50, 76–85. [Google Scholar] [CrossRef]
- Pickrell, K.; Quinn, G.; Massengill, R. Primary bone grafting of the maxilla in clefts of the lip and palate: A four year study. Plast. Reconstr. Surg. 1968, 41, 438–443. [Google Scholar] [CrossRef]
- Rehrmann, A.H.; Koberg, W.R.; Koch, H. Long-term postoperative results of primary and secondary bone grafting in complete clefts of lip and palate. Cleft Palate J. 1970, 7, 206–221. [Google Scholar]
- Carbullido, M.K.; Dean, R.A.; Kamel, G.N.; Davis, G.L.; Hornacek, M.; Segal, R.M.; Ewing, E.; Lance, S.H.; Gosman, A.A. Long-Term Treatment Outcomes of Primary Alveolar Bone Grafts for Alveolar Clefts: A Qualitative Systematic Review. Cleft Palate Craniofac. J. 2022, 59, 86–97. [Google Scholar] [CrossRef]
- Eppley, B.L. Alveolar cleft bone grafting (Part I): Primary bone grafting. J. Oral. Maxillofac. Surg. 1996, 54, 74–82. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Mueller, A.A.; Zschokke, I.; Brand, S.; Hockenjos, C.; Zeilhofer, H.-F.; Schwenzer-Zimmerer, K. One-stage cleft repair outcome at age 6- to 18-years -- a comparison to the Eurocleft study data. Br. J. Oral. Maxillofac. Surg. 2012, 50, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Urbanova, W.; Klimova, I.; Brudnicki, A.; Polackova, P.; Kroupova, D.; Dubovska, I.; Rachwalski, M.; Fudalej, P.S. The Slav-cleft: A three-center study of the outcome of treatment of cleft lip and palate. Part 1: Craniofacial morphology. J. Cranio Maxillofac. Surg. 2016, 44, 1767–1776. [Google Scholar] [CrossRef] [PubMed]
- Riolo, M.L.; Moyers, R.E.; McNamara, J.A.; Hunter, S.W. An Atlas of Craniofacial Growth: Cephalometric Standards from the University School Growth Study; The University of Michigan: Ann Arbor, MI, USA, 1979; pp. 219–280. [Google Scholar]
- Nalabothu, P.; Benitez, B.K.; Dalstra, M.; Verna, C.; Mueller, A.A. Three-Dimensional Morphological Changes of the True Cleft under Passive Presurgical Orthopaedics in Unilateral Cleft Lip and Palate: A Retrospective Cohort Study. J. Clin. Med. 2020, 9, 962. [Google Scholar] [CrossRef] [PubMed]
- Fudalej, P.S.; Hortis-Dzierzbicka, M.; Dudkiewicz, Z.; Semb, G. Dental arch relationship in children with complete unilateral cleft lip and palate following Warsaw (one-stage repair) and Oslo protocols. Cleft Palate Craniofac. J. 2009, 46, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Brattström, V.; Mølsted, K.; Prahl-Andersen, B.; Semb, G.; Shaw, W.C. The Eurocleft study: Intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 2: Craniofacial form and nasolabial appearance. Cleft Palate Craniofac. J. 2005, 42, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Sabelis, A.J.; Kuijpers, M.A.R.; Nada, R.M.; Chiu, Y.T.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Fudalej, P.S. Rating dental arch relationships and palatal morphology with the EUROCRAN index on three different formats of dental casts in children with unilateral cleft lip and palate. Clin. Oral. Investig. 2016, 20, 943–950. [Google Scholar] [CrossRef][Green Version]
- Fudalej, P.; Katsaros, C.; Dudkiewicz, Z.; Offert, B.; Piwowar, W.; Kuijpers, M.; Kuijpers-Jagtman, A.M. Dental arch relationships following palatoplasty for cleft lip and palate repair. J. Dent. Res. 2012, 91, 47–51. [Google Scholar] [CrossRef]
- Gross Portney, L.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; Prentice Hall: Hoboken, NJ, USA, 2000. [Google Scholar]
- McCance, A.M.; Roberts-Harry, D.; Sherriff, M.; Mars, M.; Houston, W.J.B. A study model analysis of adult unoperated Sri Lankans with unilateral cleft lip and palate. Cleft Palate J. 1990, 27, 146–154. [Google Scholar] [CrossRef]
- Ranta, R. A review of tooth formation in children with cleft lip/palate. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 11–18. [Google Scholar] [CrossRef]
- Lekkas, C.; Latief, B.S.; ter Rahe, S.P.; Kuijpers-Jagtman, A.M. The adult unoperated cleft patient: Absence of maxillary teeth outside the cleft area. Cleft Palate Craniofac. J. 2000, 37, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Swarnalatha, C.; Paruchuri, U.; Babu, J.S.; Alquraishi, M.A.; Almalaq, S.A.; Alnasrallah, F.A.; Nayyar, A.S. Prevalence of congenitally missing upper lateral incisors in an orthodontic adolescent population. J. Orthod. Sci. 2020, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Cao, C.; Zheng, Q.; Shi, B. The Influence of Four Different Treatment Protocols on Maxillofacial Growth in Patients with Unilateral Complete Cleft Lip, Palate, and Alveolus. Plast Reconstr. Surg. 2019, 144, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Santiago, P.E.; Grayson, B.H.; Cutting, C.B.; Gianoutsos, M.P.; Brecht, L.E.; Kwon, S.M. Reduced need for alveolar bone grafting by presurgical orthopedics and primary gingivoperiosteoplasty. Cleft Palate Craniofac. J. 1998, 35, 77–80. [Google Scholar] [CrossRef]
- Hathaway, R.R.; Eppley, B.L.; Hennon, D.K.; Nelson, C.L.; Sadove, A.M. Primary alveolar cleft bone grafting in unilateral cleft lip and palate: Arch dimensions at age 8. J. Craniofacial Surg. 1999, 10, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Grisius, T.M.; Spolyar, J.; Jackson, I.T.; Bello-Rojas, G.; Dajani, K. Assessment of cleft lip and palate patients treated with presurgical orthopedic correction and either primary bone grafts, gingivoperiosteoplasty, or without alveolar grafting procedures. J. Craniofacial Surg. 2006, 17, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Kyung, H.; Kang, N. Management of alveolar cleft. Arch. Craniofacial Surg. 2015, 16, 49. [Google Scholar] [CrossRef] [PubMed]
- Savaci, N.; Hoşnuter, M.; Tosun, Z.; Demir, A. Maxillofacial morphology in children with complete unilateral cleft lip and palate treated by one-stage simultaneous repair. Plast. Reconstr. Surg. 2005, 115, 1509–1517. [Google Scholar] [CrossRef] [PubMed]
- De Mey, A.; Franck, D.; Cuylits, N.; Swennen, G.; Malevez, C.; Lejour, M. Early one-stage repair of complete unilateral cleft lip and palate. J. Craniofacial Surg. 2009, 20, 1723–1728. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.R.; Gosla Reddy, S.; Vaidhyanathan, A.; Bergé, S.J.; Kuijpers-Jagtman, A.M. Maxillofacial growth and speech outcome after one-stage or two-stage palatoplasty in unilateral cleft lip and palate. A systematic review. J. Cranio Maxillofac. Surg. 2017, 45, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Kantar, R.S.; Rifkin, W.J.; Cammarata, M.J.; Maliha, S.G.; Diaz-Siso, J.R.; Farber, S.J.; Flores, R.L. Single-Stage Primary Cleft Lip and Palate Repair: A Review of the Literature. Ann. Plast. Surg. 2018, 81, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Rohrich, R.J.; Love, E.J.; Byrd, H.S.; Johns, D.F. Optimal timing of cleft palate closure. Plast. Reconstr. Surg. 2000, 106, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Brudnicki, A.; Sawicka, E.; Fudalej, P.S. Maxillofacial morphology in post-pubertal patients with unilateral cleft lip and palate following early vs. late secondary alveolar bone grafting. J. Cranio Maxillofac. Surg. 2021, 49, 809–814. [Google Scholar] [CrossRef] [PubMed]

| Study Population (Publication) | Description | n | Age Range [Years] | Treatment Protocol |
|---|---|---|---|---|
| 2003–2014 | Group A | 16 | 6–9 | One-stage cleft repair: lip, vomer flap and two-flap palatoplasty at 6 months |
| 1991–2002 (Group 1) [13] | Group B | 15 | 6–11 | One-stage cleft repair: lip, vomer flap and two-flap palatoplasty with primary rib bone grafting at 6 months |
| Slav-Cleft (Warsaw) [14] | Group S | 35 | 8–13.6 | One-stage cleft repair: lip, vomer flap and bipedicled hard and soft palate repair at 9 months |
| Healthy control group [15] | Group H | 83 | 6–9 | N/A |
| Group A (2003–2014) n (%) | Group B (1991–2002) n (%) | Group S (1994–1996) n (%) | |
|---|---|---|---|
| Total patients per group | 16 | 15 | 35 |
| Female | 5 (31.25%) | 4 (26.67%) | 10 (28.57%) |
| Male | 11 (68.75%) | 11 (73.33%) | 25 (71.43%) |
| Cleft | |||
| Left | 11 (68.75%) | 9 (60%) | N/A |
| Right | 5 (31.25%) | 6 (40%) | N/A |
| Age at study (years) [mean (SD)] | 6.8 (0.83) | 9 (2) | 10.6 (1.2) |
| Age at cleft repair (months) [mean (SD)] | 3.9 (0.62) | 6 (1) | 9 |
| Group A (2003–2014) n = 16 | Group B (1991–2002) n = 15 | |
|---|---|---|
| EUROCRAN dental grade a | ||
| 1 | 2 (12.5%) | 3 (20%) |
| 2 | 2 (12.5%) | 5 (33%) |
| 3 | 5 (31.25%) | 5 (33%) |
| 4a | 6 (37.5%) | 2 (13%) |
| 4b | 1 (6.25%) | |
| Mean (SD) | 3 (1.0) | 2.4 (1.0) |
| EUROCRAN palatal morphology grade b | ||
| 1 | 5 (31.25%) | 3 (20%) |
| 2 | 8 (50%) | 7 (47%) |
| 3 | 3 (18.75%) | 5 (33%) |
| Mean (SD) | 1.9 (0.7) | 2.1 (0.7) |
| Missing lateral incisors—Cleft side [n (%)] | ||
| Yes | 8 (50%) | 11 (73%) |
| No | 8 (50%) | 4 (27%) |
| Missing lateral incisors—Non-cleft side [n (%)] | ||
| Yes | 9 (56.25%) | 6 (40%) |
| No | 7 (43.75%) | 9 (60%) |
| Missing lateral incisors—Bilateral [n (%)] | ||
| Yes | 6 (37.5%) | 5 (33%) |
| No | 10 (62.5%) | 10 (67%) |
| Group A (2003–2014) | Group B (1991–2002) | Group S (Slav-Cleft) | Healthy Control | ||||
|---|---|---|---|---|---|---|---|
| (n = 16) | Group 1 (n = 15) | Warsaw (n = 35) | (n = 83) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-Value # | Differences * | ||
| Hard tissue | |||||||
| maxilla | S-N-A | 76.5 (5.9) | 76 (4) | 75.7 (3.6) | 81 (3.1) | <0.001 | A-H, B-H, S-H |
| NSL/NL | 11.7 (4.2) | 14 (4) | 11.2 (4.3) | 6.4 (2.5) | <0.001 | A-H, B-S, B-H, S-H | |
| mandible | S-N-Pog | 73.9 (4.3) | 75 (4) | 75.4 (4) | 76.1 (2.9) | 0.022 | A-H |
| NSL/ML | 34.9 (5.5) | 35 (4) | 37.3 (5.6) | 35.1 (4.6) | 0.076 | - | |
| maxillomandibular | A-N-B | 3.5 (4.3) | 3 (3) | 1.3 (2.8) | 4.8 (2.3) | <0.001 | A-S, B-H S-H |
| ILs/NL | 88.5 (8.1) | 103 (15) | 105 (8.2) | 107.3 (7.6) | <0.001 | A-B, A-S, A-H | |
| ILs/ILi | 161.1 (11.4) | 154 (12) | 143 (10.9) | 131.7 (11.8) | <0.001 | A-S, A-H, B-S, B-H, S-H | |
| Soft tissue | |||||||
| maxillomandibular | sss-ns-sms | 5.3 (4.1) | 6 (3) | 5.9 (2.7) | - | 0.79 | - |
| sss-ns-pgs | 4.8 (3.5) | 5 (3) | 4.5 (3.1) | - | 0.86 | - | |
| gs-sn-pgs | 187.9 (9.5) | 187 (7) | 173.5 (6.8) | - | <0.001 | A-S, B-S | |
| nasal profile | gs-prn-pgs | 149.7 (7.4) | 150 (5) | 147.8 (5.8) | - | 0.38 | - |
| ns-unt/NSL | 102.4 (7.1) | 107 (4) | 105.9 (4.7) | - | 0.036 | A-B | |
| ns-prn-sn | 107.5 (4.7) | 105 (6) | 104.5 (5.9) | - | 0.22 | - | |
| nst-sn-ls | 107.8 (14.8) | 102 (11) | 101.6 (12.8) | - | 0.27 | - | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benitez, B.K.; Weibel, S.K.; Halbeisen, F.S.; Lill, Y.; Nalabothu, P.; Tache, A.; Mueller, A.A. Craniofacial Growth at Age 6–11 Years after One-Stage Cleft Lip and Palate Repair: A Retrospective Comparative Study with Historical Controls. Children 2022, 9, 1228. https://doi.org/10.3390/children9081228
Benitez BK, Weibel SK, Halbeisen FS, Lill Y, Nalabothu P, Tache A, Mueller AA. Craniofacial Growth at Age 6–11 Years after One-Stage Cleft Lip and Palate Repair: A Retrospective Comparative Study with Historical Controls. Children. 2022; 9(8):1228. https://doi.org/10.3390/children9081228
Chicago/Turabian StyleBenitez, Benito K., Seraina K. Weibel, Florian S. Halbeisen, Yoriko Lill, Prasad Nalabothu, Ana Tache, and Andreas A. Mueller. 2022. "Craniofacial Growth at Age 6–11 Years after One-Stage Cleft Lip and Palate Repair: A Retrospective Comparative Study with Historical Controls" Children 9, no. 8: 1228. https://doi.org/10.3390/children9081228
APA StyleBenitez, B. K., Weibel, S. K., Halbeisen, F. S., Lill, Y., Nalabothu, P., Tache, A., & Mueller, A. A. (2022). Craniofacial Growth at Age 6–11 Years after One-Stage Cleft Lip and Palate Repair: A Retrospective Comparative Study with Historical Controls. Children, 9(8), 1228. https://doi.org/10.3390/children9081228






