Exploring Change in Children’s and Art Therapists’ Behavior during ‘Images of Self’, an Art Therapy Program for Children Diagnosed with Autism Spectrum Disorders: A Repeated Case Study Design
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measurement Instruments
2.3. Procedure
2.4. Analysis
3. Results
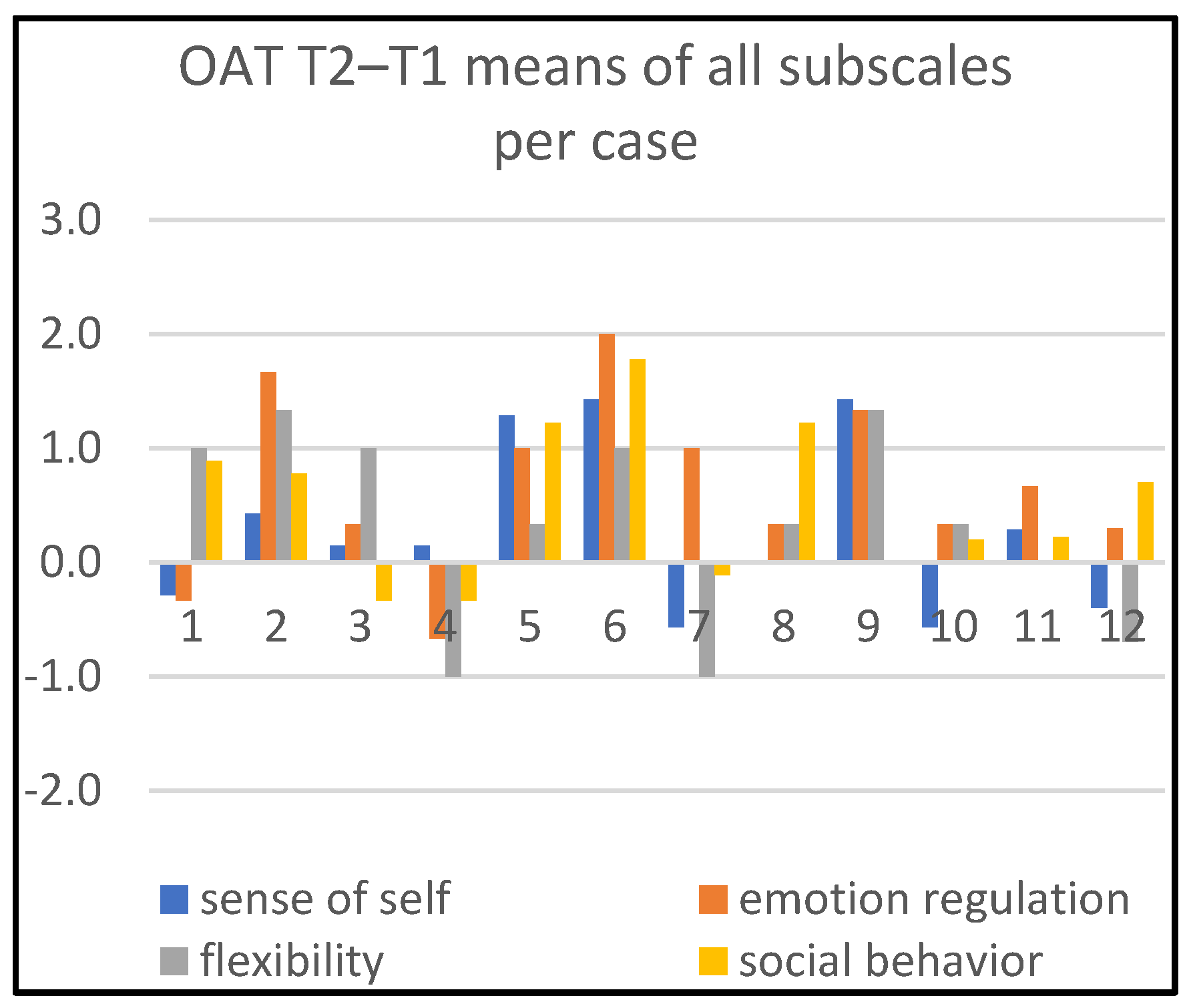
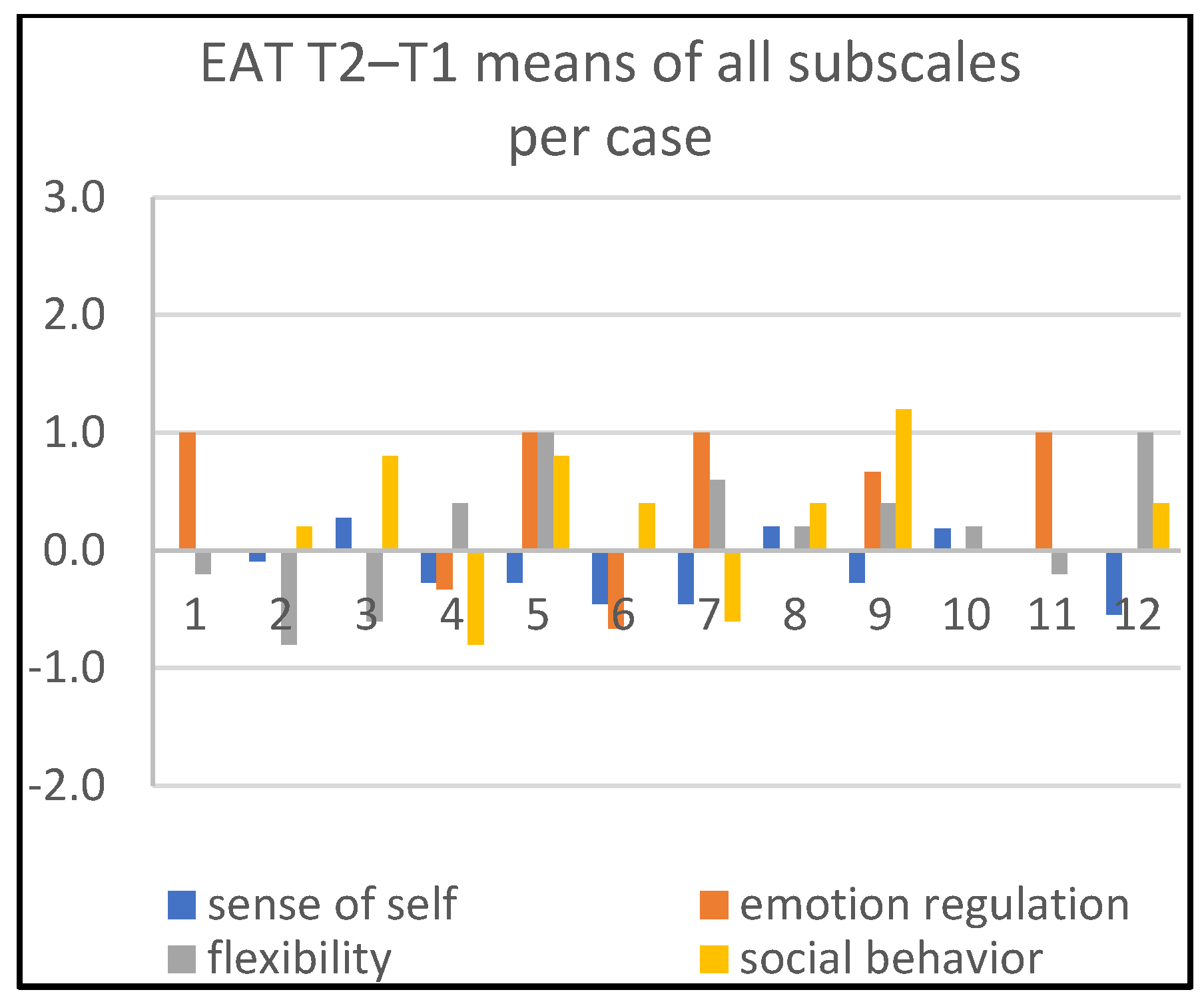
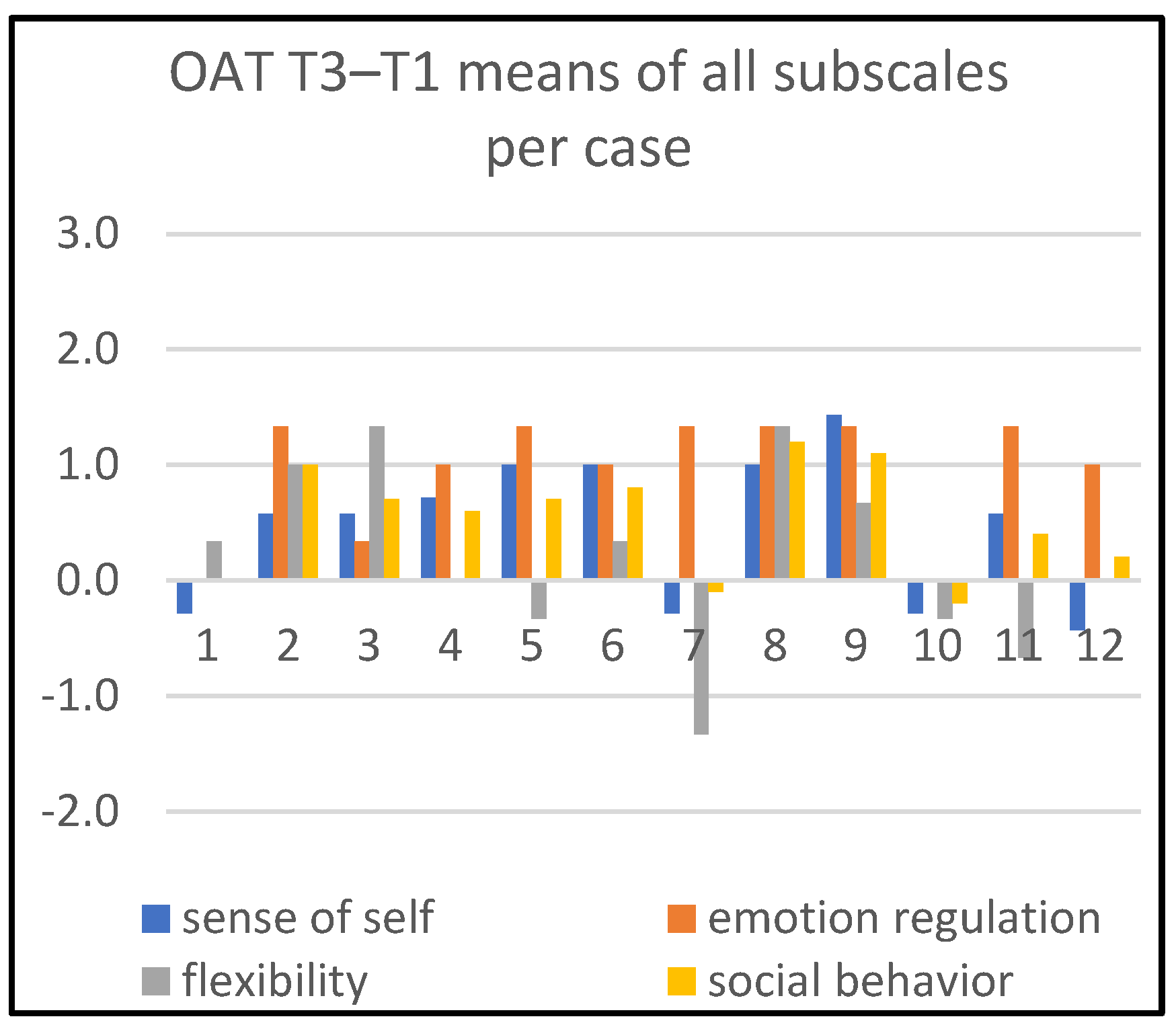
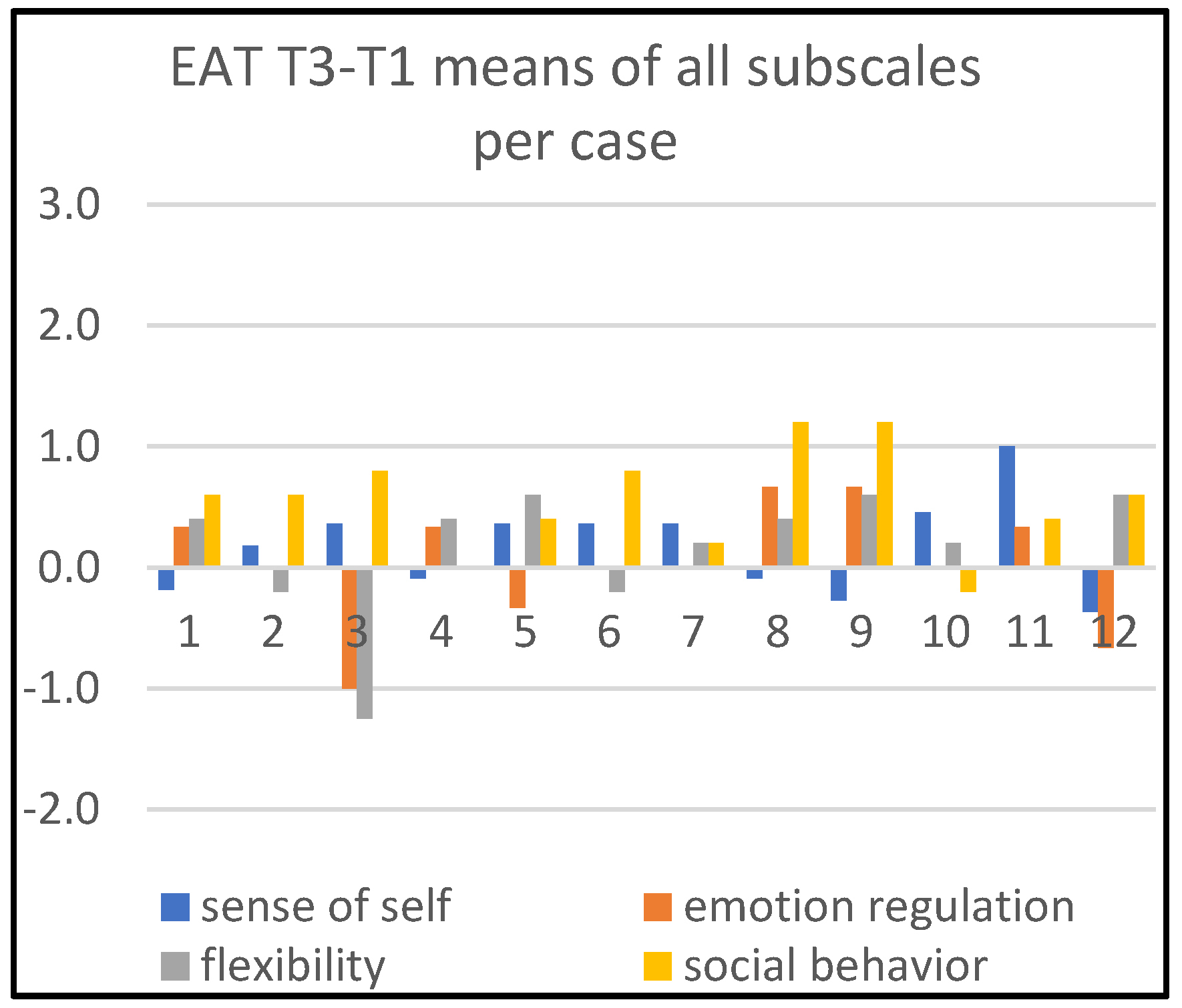
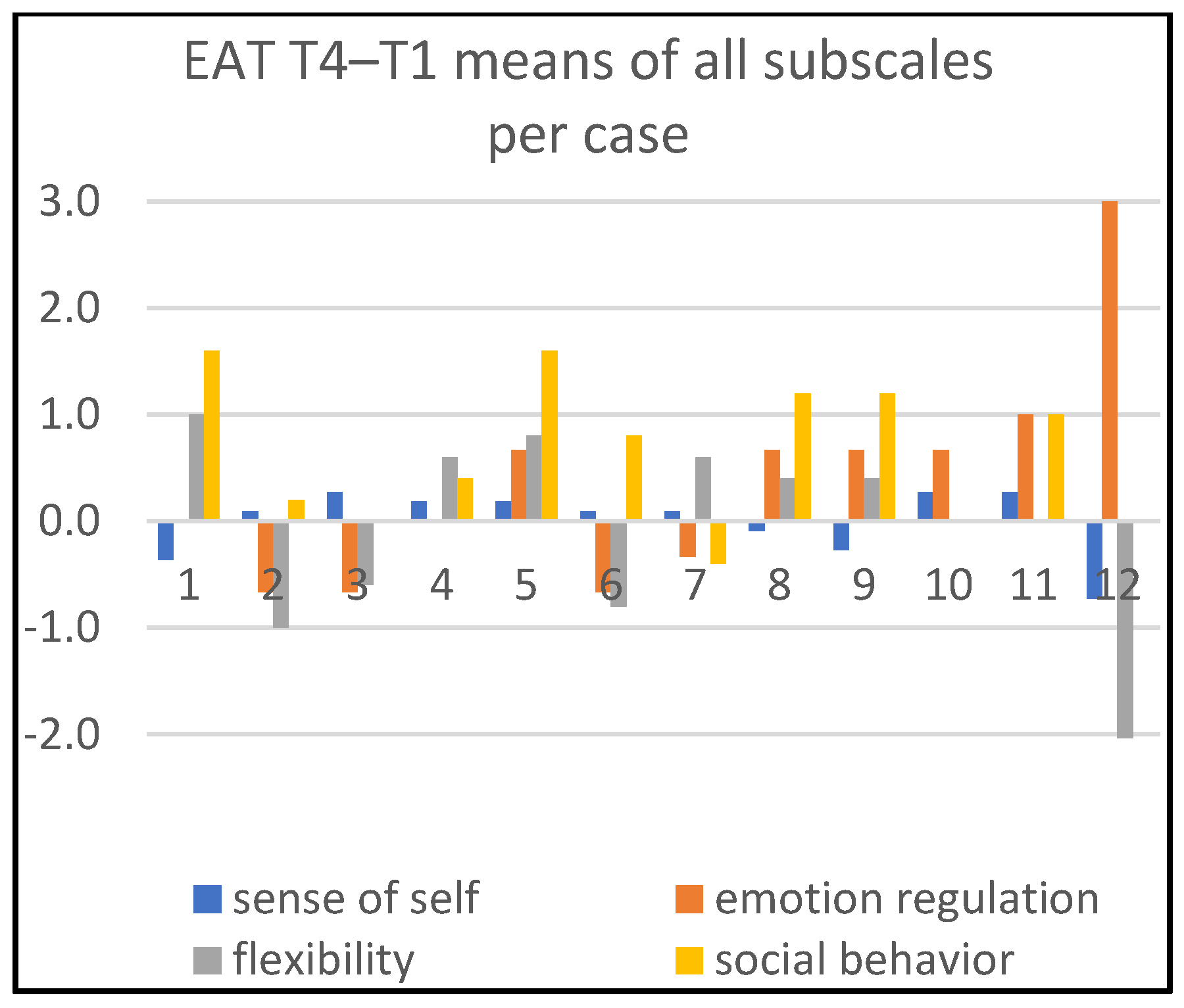
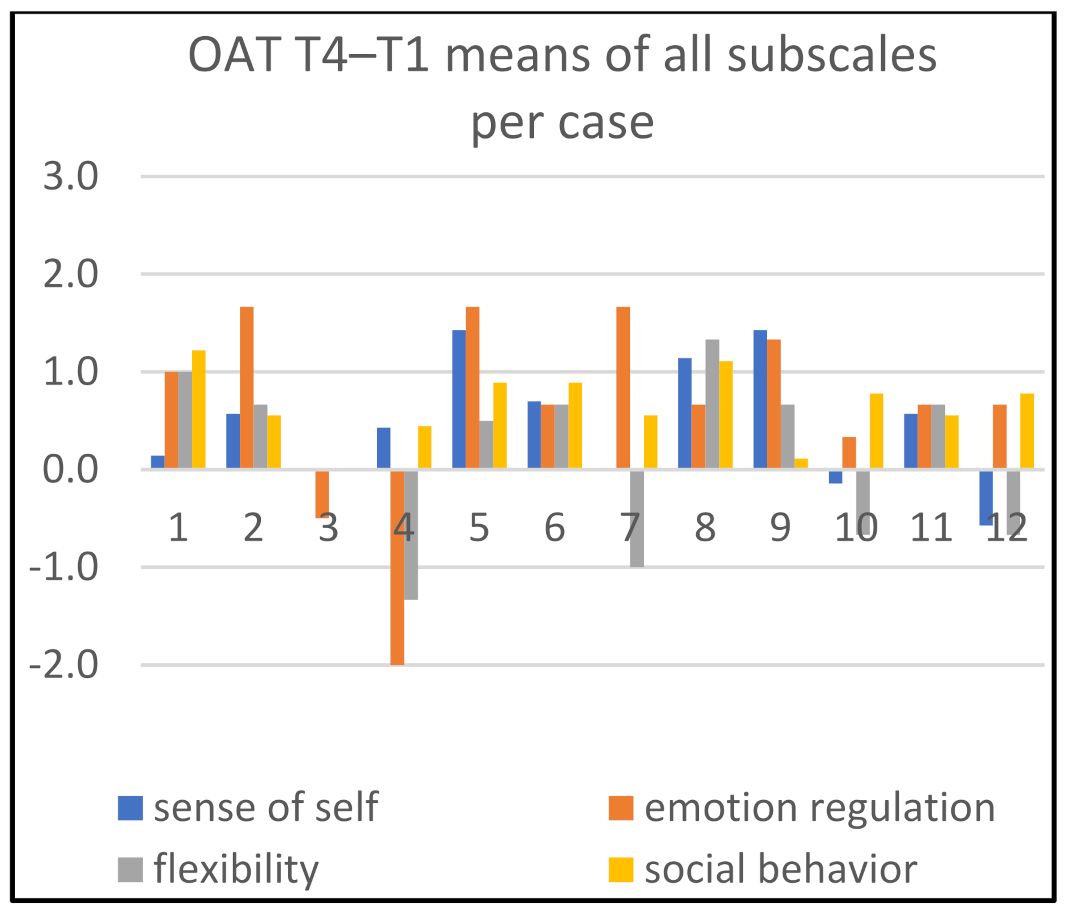
3.1. Individual Analyses
3.2. Change in Children’s Behavior with Respect to Therapists’ Behavior
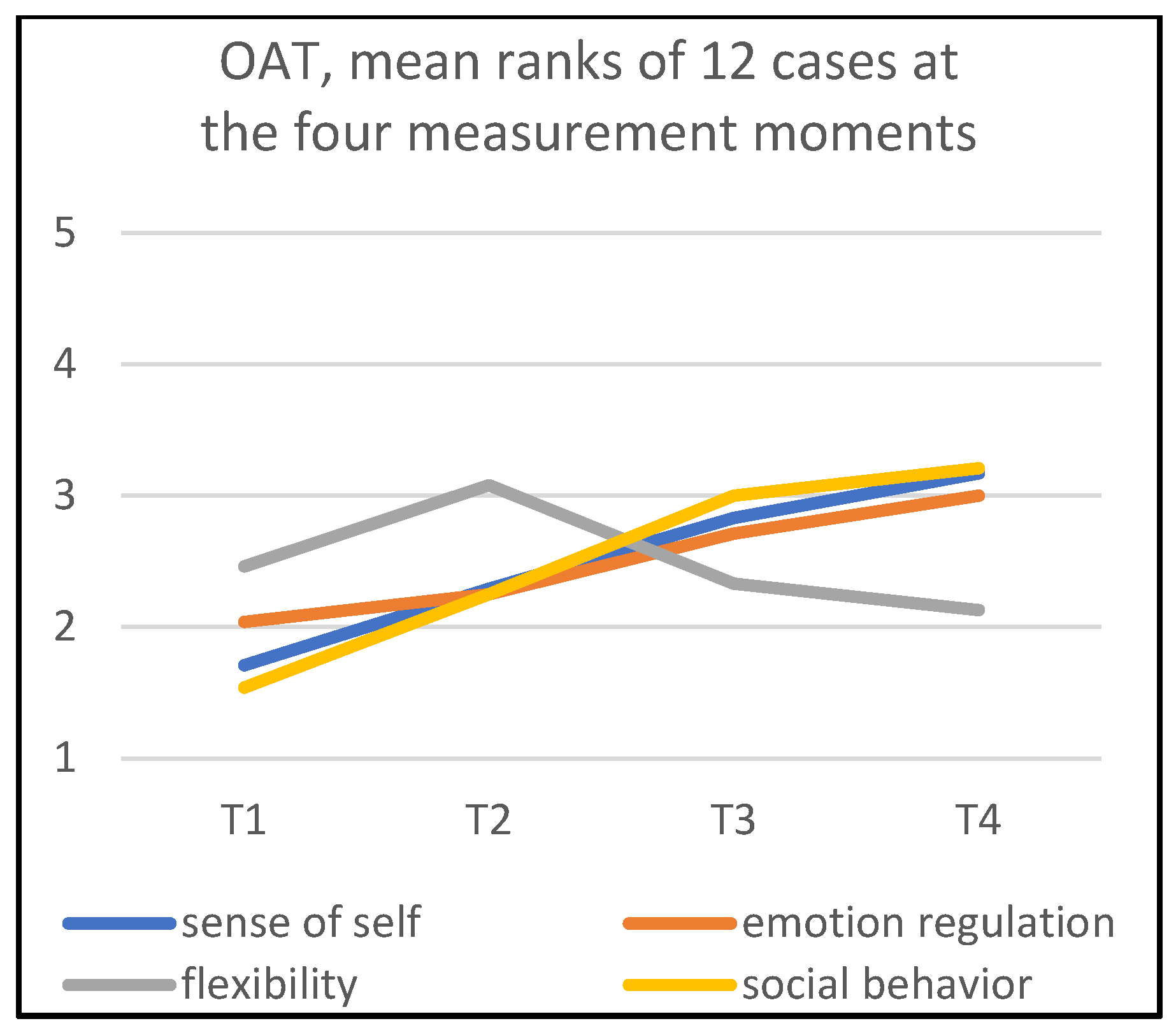
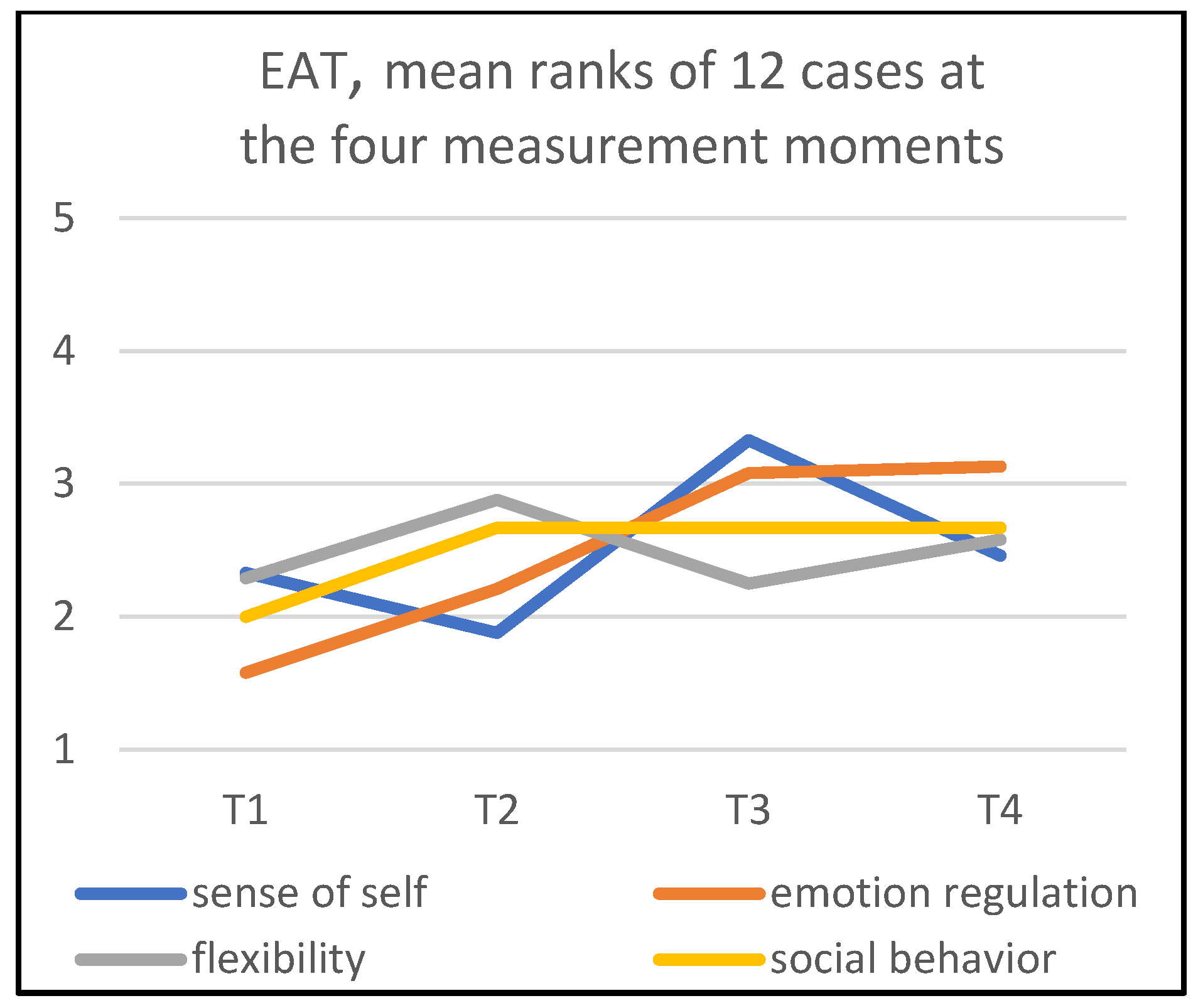
3.3. Group Analyses
3.4. Patterns in Mean Ranks
4. Discussion
4.1. Strengths and Limitations
4.2. Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Child. | Gender | Age | Art Therapist | Experience of Art Therapist (years) | Treatment Setting | Reason for Referral | Medication | Context Information |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 6 | 1 | 13 | Ambulant mental health care organization | Not going to school at start AT. Heavy emotion regulation problems and inflexible behavior in classroom. | Vitamin B injections | After eight weeks she is part-time visiting school. Mother tells that the teacher does not understand her child. |
| 2 | F | 9 | 2 | 40 | (Semi)residential psychiatric center for children and youth | Social communication problems: isolated; what is she thinking/feeling? | No | Philippine background with Asian values about behavior and education. Mother has a burn-out and is in a divorce. |
| 3 | F | 12 | 3 | 8 | School for special education | Emotion regulation problems in classroom (crying); negative self-image; oversensitivity. | Methyl phenidate for oversensitivity | Extra psycho- education for child, to improve her understanding of ASD. |
| 4 | M | 10 | 4 | 13 | (Semi)residential psychiatric center for children and youth | Child shows severe depressed feelings at home. Negative self-image. Emotion regulation problems in classroom (anxiety problems and anger outbursts). | Methyl phenidate | Parent training to improve understanding of ASD. |
| 5 | F | 11 | 5 | 40 | School for special education | Negative self-image. Severe depressed feelings at home. Emotion regulation problems in classroom (anxiety problems). Social communication problems at home and in school (hardly talks). | No | At the end of AT she went to a lower class grade. |
| 6 | M | 9 | 5 | 40 | School for special education | Negative self-image. Emotion regulation problems at home and in classroom (anxiety problems and anger outbursts). | Yes, for the anxiety and emotion regulation, but no specific information what it is. | After 10 weeks, mother severely ill. Child has problems with teacher. |
| 7 | M | 10 | 5 | 40 | School for special education | Negative self-image. Flexibility problems at home. | No | |
| 8 | M | 12 | 6 | 20 | (Semi)residential psychiatric center for children and youth | Negative self-image. Flexibility problems. Social communication problems (what is she thinking/feeling?). Anxiety problems. | No | Parent training to improve understanding of ASD. |
| 9 | M | 12 | 6 | 20 | (Semi)residential psychiatric center for children and youth | Negative self-image. Emotion regulation problems at home and in classroom (anger outbursts). | No | Parent training to improve understanding of ASD. Stop-think-do method is used in school. |
| 10 | M | 11 | 1 | 13 | Ambulant mental health care organization | Negative self-image. Emotion regulation problems at home (anger outbursts). Social communication problems (what is he thinking/feeling?). | No | Parent training to improve understanding of ASD. |
| 11 | F | 11 | 7 | 9 | Ambulant mental health care organization | Negative self-image. Social communication problems. | Methyl phenidate for ADHD | |
| 12 | M | 12 | 1 | 13 | Ambulant mental health care organization | Negative self-image. Very depressed feelings. Social communication problems (what is he thinking/feeling?). | No | Parent training to improve understanding of ASD. Divorce of parents during treatment. |
References
- Teeuw, H. Resultaten in Beeld. Een Onderzoek naar Resultaten die Beeldend Therapeuten Behalen bij Kinderen met PDDnos van 8–12 Jaar [Outcomes in the Picture. A study into the Results of Art Therapists Working with Children 8–12 Years of Age with PDDnos]. Bachelor’s Thesis, NHL Stenden University of Applied Sciences, Leeuwarden, The Netherlands, 2011. [Google Scholar]
- AKWA-GGZ. Zorgstandaard Autisme [Care Standards Autism]. 2018. Available online: https://www.ggzstandaarden.nl/zorgstandaarden/autisme (accessed on 2 January 2019).
- American Art Therapy Association. About Art Therapy. 2014. Available online: https://www.arttherapy.org (accessed on 2 January 2014).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Bosgraaf, L.; Spreen, M.; Pattiselanno, K.; Van Hooren, S. Art therapy for psychosocial problems in children and adolescents: A systematic narrative review on art therapeutic means and forms of expression, therapist behavior and supposed mechanisms of change. Front. Psychol. 2020, 11, 2389. [Google Scholar] [CrossRef] [PubMed]
- Hauck, M.; Fein, D.; Waterhouse, L.; Feinstein, C. Social initiations by autistic children to adults and other children. J. Autism Other Dev. Disord. 1995, 25, 579–595. [Google Scholar] [CrossRef]
- Rozga, A.; Anderson, S.; Robins, D.L. Major current neuropsychological theories of ASD. In The Neuropsychology of Autism; Fein, D.A., Ed.; Oxford University Press: Oxford, UK, 2011; pp. 97–137. [Google Scholar]
- Waterhouse, L.; Gillberg, C. Why autism must be taken apart. J. Autism Dev. Disord. 2014, 44, 1788–1792. [Google Scholar] [CrossRef]
- Gillberg, C.; Fernell, E. Autism plus versus autism pure. J. Autism Dev. Disord. 2014, 44, 3274–3276. [Google Scholar] [CrossRef]
- Durrani, H. Sensory-Based Relational Art Therapy Approach (S-GRATA). Supporting Psycho-Emotional Needs in Children with Autism; Routledge: Milton Park, UK, 2021. [Google Scholar]
- Regev, D.; Snir, S. Art therapy for treating children with Autism Spectrum Disorders (ASD): The unique contribution of art materials. Acad. J. Creat. Art Ther. 2013, 3, 251–260. [Google Scholar]
- Van Lith, T.; Woolhiser Stallings, J.; Harris, C.E. Discovering good practice for children who have Autism Spectrum Disorder: The results of a small scale survey. Arts Psychother. 2017, 54, 78–84. [Google Scholar] [CrossRef]
- Begeer, M.; Poortland, B.; Mataw, K.J.S.; Begeer, S. Interventies voor kinderen met autisme: Wat bepaalt de keuze? Interventions for children with autism: What determines the choice? Wet. Tijdschr. Autisme 2019, 18, 40–53. [Google Scholar]
- Martin, N. Art as an Early Intervention Tool for Children with Autism; Jessica Kingsley: London, UK, 2009. [Google Scholar]
- Schweizer, C.; Knorth, E.J.; Spreen, M. Art therapy with children with Autism Spectrum Disorders: A review of clinical case descriptions on ‘what works’. Arts Psychother. 2014, 41, 577–593. [Google Scholar] [CrossRef]
- Schweizer, C.; Spreen, M.; Knorth, E.J. Exploring what works in art therapy with children with autism: Tacit knowledge of art therapists. Art Ther. 2017, 34, 183–191. [Google Scholar] [CrossRef]
- Schweizer, C.; Knorth, E.J.; Van Yperen, T.A.; Spreen, M. Consensus-based typical elements of art therapy with children with Autism Spectrum Disorders. Int. J. Art Ther. 2019, 24, 181–191. [Google Scholar] [CrossRef]
- Schweizer, C. Art Therapy for Children Diagnosed with Autism Spectrum Disorders: Development and First Evaluation of a Treatment Programme. Ph.D. Thesis, University of Groningen, Groningen, The Netherlands, 2020. [Google Scholar] [CrossRef]
- Schweizer, C.; Knorth, E.J.; Van Yperen, T.A.; Spreen, M. Evaluation of ‘Images of Self’, an art therapy program for children diagnosed with autism spectrum disorders (ASD). Child. Youth Serv. Rev. 2020, 116, 1–10. [Google Scholar] [CrossRef]
- Hartman, C.A.; Luteijn, E.; Moorlag, H.; De Bildt, A.; Minderaa, R.B. Vragenlijst voor Inventarisatie van Sociaal Gedrag van Kinderen (VISK). Handleiding [Questionnaire for Mapping of ‘Social Behavior’ of Children (VISK). Manual]; Boom: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Veerman, J.W.; Straathof, M.A.E.; Treffers, D.A.; Van den Bergh, B.R.H.; Ten Brink, L.T. Competentie Belevingsschaal voor Kinderen (CBSK), Handleiding; Pearson: London, UK, 2004. [Google Scholar]
- Jörg, F.; Ormel, J.; Reijneveld, S.A.; Jansen, D.E.M.C.; Verhulst, F.C.; Oldehinkel, A.J. Puzzling findings in studying the outcome of ‘real world’ adolescent mental health services: The TRAILS Study. PLoS ONE 2012, 7, e44704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nanninga, M.; Jansen, D.E.M.C.; Knorth, E.J.; Reijneveld, S.A. Enrolment of children in psychosocial care: Problems upon entry, care received, and outcomes achieved. Eur. Child Adolesc. Psychiatry 2016, 27, 625–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heynen, E.; Roest, J.; Willemars, G.; Van Hooren, S. Therapeutic alliance is a factor of change in arts therapies and psychomotor therapy with adults who have mental health problems. Arts Psychother. 2017, 55, 111–115. [Google Scholar] [CrossRef]
- Schweizer, C.; De Bruin, J.; Haeyen, S.; Henskens, B.; Rutten-Saris, M.; Visser, H. (Eds.) Handboek Beeldende Therapie. Uit de Verf. [Handbook Art Therapy. Paint It out]; Bohn Stafleu van Loghum: Houten, The Netherlands, 2009. [Google Scholar]
- Schweizer, C.; Knorth, E.J.; Van Yperen, T.A.; Spreen, M. Evaluating art therapeutic processes with children diagnosed with Autism Spectrum Disorders: Development and testing of two observation instruments for evaluating children’s and therapists’ behavior. Arts Psychother. 2019, 66, 1–9. [Google Scholar] [CrossRef]
- Pater, M.; Spreen, M.; Van Yperen, T. The developmental process in social behavior of children with Autism Spectrum Disorder getting music therapy. A multiple case study. Child. Youth Serv. Rev. 2021, 120, 1–8. [Google Scholar] [CrossRef]
- Gioia, G.A.; Isquith, P.K.; Guy, S.C.; Kenworthy, L. Behavior Rating Instrument for Executive Functions (BRIEF); Psychological Assessment Resources (PAR): Lutz, FL, USA, 2000. [Google Scholar]
- .Hartman, C.A.; Luteijn, E.; Serra, M.; Minderaa, R. Refinement of the Children’s ‘Social Behavior’ Questionnaire (CSBQ): An instrument that describes the diverse problems seen in milder forms of PDD. J. Autism Dev. Disord. 2006, 36, 325–342. [Google Scholar] [CrossRef]
- Harter, S. Self-Perception Profile for Children: Manual and Questionnaires (Grades 3–8); University of Denver: Denver, CO, USA, 2012. [Google Scholar]
- Stern, D.N. The Interpersonal World of the Infant. A View from Psycho Analysis and Developmental Psychology; Basic Books: New York, NY, USA, 1985. [Google Scholar]
- Van Heusden, B. Arts education ‘After the End of Art’. Towards a new framework for arts education. In Arts Education beyond Art: Teaching Art in Times of Change; van Heusden, B., Gielen, P., Eds.; Valiz: Amsterdam, The Netherlands, 2015; pp. 153–164. [Google Scholar]
- Schweizer, C. Ik zie ik zie wat jij niet ziet. Behandelresultaten van beeldende therapie bij cliënten met autisme spectrum stoornissen [I spy with my little eye. Treatment results of art therapy with clients with autism spectrum disorders]. Tijdschr. Voor Vaktherapie 2016, 12, 13–17. [Google Scholar]
- Lambie, J.A.; Marcel, A.J. Consciousness and the varieties of emotion experience: A theoretical framework. Psychol. Rev. 2002, 109, 219–259. [Google Scholar] [CrossRef]
- Gross, J.J.; John, O.P. Individual differences in two ‘emotion regulation’ processes: Implications for affect, relationships, and well-being. J. Personal. Soc. Psychol. 2003, 85, 348–362. [Google Scholar] [CrossRef]
- Gruber, H.; Oepen, R. Emotion regulation strategies and effects in art-making: A narrative synthesis. Arts Psychother. 2018, 59, 65–74. [Google Scholar] [CrossRef]
- Webb, T.L.; Miles, E.; Sheeran, P. Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of ‘emotion regulation’. Psychol. Bull. 2012, 138, 775–808. [Google Scholar] [CrossRef] [PubMed]
- Huizinga, M.; Smidts, D.P. BRIEF. Vragenlijst Executieve Functies voor 5- tot 18-Jarigen: Handleiding. [BRIEF. Questionnaire on Executive Functions for the 5–18 Age Group: Manual]; Hogrefe: Boston, MA, USA, 2012. [Google Scholar]
- Isserow, J. Looking together: Joint attention in art therapy. Int. J. Art Ther. 2008, 13, 34–42. [Google Scholar] [CrossRef]
- Murza, K.A.; Schwartz, J.B.; Hahs-Vaughn, D.H.; Nye, C. Joint attention interventions for children with autism spectrum disorder: A systematic review and meta-analysis. Int. J. Lang. Commun. Disord. 2015, 51, 236–251. [Google Scholar] [CrossRef]
- Lavrakas, P.J. (Ed.) Encyclopedia of Survey Research Methods; Sage Publications Inc.: Newbury Park, CA, USA, 2008. [Google Scholar]
- Kern Koegel, L.; Brown, F. Autism Spectrum Disorders: Trends, treatments, and diversity. Res. Pract. Pers. Sev. Disabil. 2007, 32, 87–88. [Google Scholar] [CrossRef]
- Stemler, S.E. A comparison of consensus, consistency, and measurement approaches to estimating interrater reliability. Pract. Assess. Res. Eval. 2004, 9, 1–11. [Google Scholar] [CrossRef]
- Artz, P. Bundeling van Deelonderzoeken over de Werkalliantie Binnen Vaktherapie. 2016. Available online: https://kenvak.nl/wp-content/uploads/2015/10/E-book-Zuyd_Boek_StayTuned_digitaal.pdf (accessed on 5 May 2022).
- Van den Hoek, W.; Vanuit Autisme Bekeken (VAB). Rapport Autisme en Levensloop Begeleiding. [From an Autism Perspective. Autism and Life Course Guidance Report]. 2019. Available online: https://www.vanuitautismebekeken.nl (accessed on 5 May 2022).
- Ferris Richardson, J. Art therapy on the autism spectrum: Engaging the mind, brain and senses. In The Wiley Handbook of Art Therapy; Gussak, D.E., Rosal, M.L., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2016; pp. 306–316. [Google Scholar]
- De Los Reyes, A.; Thomas, S.A.; Goodman, K.L.; Kundey, S.M.A. Principles underlying the use of multiple informants’ reports. Annu. Rev. Clin. Psychol. 2013, 9, 123–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, J.; Thomas, E. Art therapy for children with autism spectrum disorder in India. Art Ther. 2019, 36, 209–214. [Google Scholar] [CrossRef]
- Cummings, S.; Bridgmen, T.; Brown, K.G. Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Hum. Relat. 2016, 69, 33–60. [Google Scholar] [CrossRef] [Green Version]
- De Jong, R.K.; Snoek, H.; Staal, W.G.; Klip, H. The effect of patients’ feedback on treatment outcome in a child and adolescent psychiatric sample: A randomized controlled trial. Eur. Child Adolesc. Psychiatry 2019, 28, 819–834. [Google Scholar] [CrossRef] [Green Version]
- Hall, A.; Finch, T.; Kolehmainen, N.; James, D. Implementing a video-based intervention to empower staff members in an autism care organization: A qualitative study. BMC Health Serv. Res. 2016, 16, 608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poslawsky, I.E.; Naber, F.B.A.; Bakermans-Kranenburg, M.J.; De Jonge, M.V.; Van Engeland, H.; Van IJzendoorn, M.H. Development of a video-feedback intervention to promote Positive Parenting for children with autism (VIPP-AUTI). Attach. Hum. Dev. 2014, 16, 343–355. [Google Scholar] [CrossRef] [PubMed]
- Walfish, S.; McAlister, B.; O’Donnell, P.; Lambert, M.J. An investigation of self-assessment bias in mental health providers. Psychol. Rep. 2012, 10, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Bijl, B.; Van Yperen, T.; Veerman, J.W. Een kwestie van bewijzen … [The issue of proving …]. In Zicht op Effectiviteit. Handboek voor Resultaatgerichte Ontwikkeling van Interventies in de Jeugdsector; van Yperen, T., Veerman, J.W., Bijl, B., Eds.; Lemniscaat: Rotterdam, The Netherlands, 2017; pp. 115–140. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schweizer, C.; Knorth, E.J.; Van Yperen, T.A.; Spreen, M. Exploring Change in Children’s and Art Therapists’ Behavior during ‘Images of Self’, an Art Therapy Program for Children Diagnosed with Autism Spectrum Disorders: A Repeated Case Study Design. Children 2022, 9, 1036. https://doi.org/10.3390/children9071036
Schweizer C, Knorth EJ, Van Yperen TA, Spreen M. Exploring Change in Children’s and Art Therapists’ Behavior during ‘Images of Self’, an Art Therapy Program for Children Diagnosed with Autism Spectrum Disorders: A Repeated Case Study Design. Children. 2022; 9(7):1036. https://doi.org/10.3390/children9071036
Chicago/Turabian StyleSchweizer, Celine, Erik J. Knorth, Tom A. Van Yperen, and Marinus Spreen. 2022. "Exploring Change in Children’s and Art Therapists’ Behavior during ‘Images of Self’, an Art Therapy Program for Children Diagnosed with Autism Spectrum Disorders: A Repeated Case Study Design" Children 9, no. 7: 1036. https://doi.org/10.3390/children9071036
APA StyleSchweizer, C., Knorth, E. J., Van Yperen, T. A., & Spreen, M. (2022). Exploring Change in Children’s and Art Therapists’ Behavior during ‘Images of Self’, an Art Therapy Program for Children Diagnosed with Autism Spectrum Disorders: A Repeated Case Study Design. Children, 9(7), 1036. https://doi.org/10.3390/children9071036





