Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review
Abstract
:1. Introduction
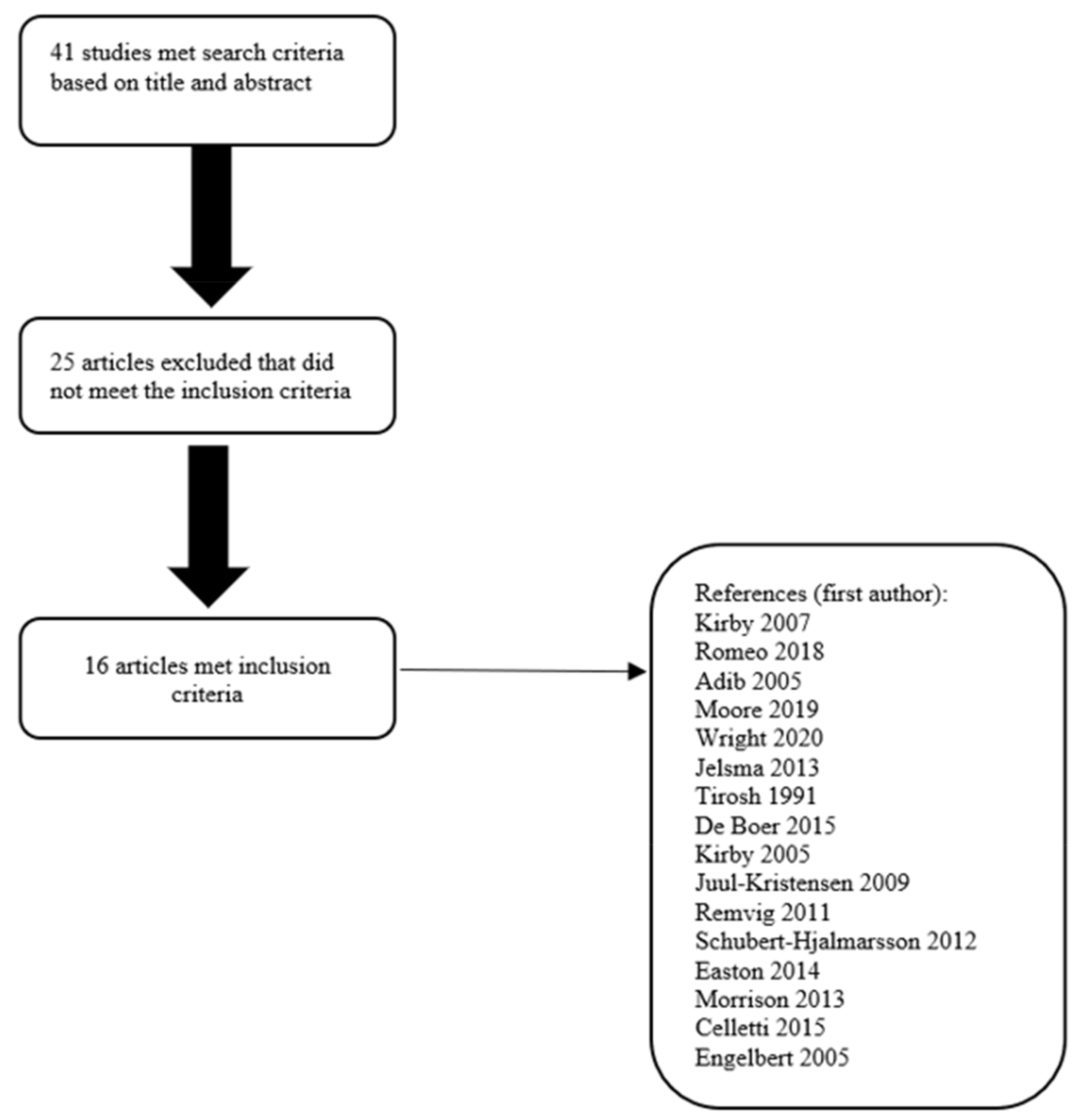
2. Methods
2.1. Search Criteria
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction and Analysis
3. Results
3.1. Studies Assessing Joint Hypermobility and Motor Performance/Coordination by Using the M-ABC
3.2. Studies Assessing Joint Hypermobility and Motor Performance by Using Different Kinds of Evaluations
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blank, R.; Smits-Engelsman, B.; Polatajko, H.; Wilson, P. European Academy for Childhood Disability (EACD): Recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version)*: EACD Recommendations. Dev. Med. Child Neurol. 2012, 54, 54–93. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Miyahara, M.; Möbs, I. Developmental dyspraxia and developmental coordination disorder. Neuropsychol. Rev. 1995, 5, 245–268. [Google Scholar] [CrossRef] [PubMed]
- Harris, S.R.; Mickelson, E.C.R.; Zwicker, J.G. Diagnosis and management of developmental coordination disorder. CMAJ 2015, 187, 659–665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wuang, Y.P.; Su, J.H.; Su, C.Y. Reliability and responsiveness of the Movement Assessment Battery for Children-Second Edition Test in children with developmental coordination disorder. Dev. Med. Child Neurol. 2012, 54, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.H. Practitioner review: Approaches to assessment and treatment of children with DCD: An evaluative review. J. Child Psychol. Psychiatry 2005, 46, 806–823. [Google Scholar] [CrossRef]
- Engelbert, R.H.H.; Juul-Kristensen, B.; Pacey, V.; de Wandele, I.; Smeenk, S.; Woinarosky, N.; Sabo, S.; Scheper, M.C.; Russek, L.; Simmonds, J.V. The evidence-based rationale for physical therapy treatment of children, adolescents, and adults diagnosed with joint hypermobility syndrome/hypermobile Ehlers Danlos syndrome. Am. J. Med. Genet. Part C Semin. Med. Genet. 2017, 175, 158–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirby, A.; Davies, R. Developmental Coordination Disorder and Joint Hypermobility Syndrome?—Overlapping disorders? Implications for research and clinical practice. Child Care Health Dev. 2007, 33, 513–519. [Google Scholar] [CrossRef]
- Clark, C.J.; Khattab, A.D. Association between Joint Hypermobility Syndrome and Developmental Coordination Disorder—A Review. J. Sports Med. Doping Stud. 2012, S4. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Klerks, M.; Kirby, A. Beighton Score: A Valid Measure for Generalized Hypermobility in Children. J. Pediatrics 2011, 158, 119–123.e4. [Google Scholar] [CrossRef]
- Murray, K.J. Benign joint hypermobility in childhood. Rheumatology 2001, 40, 489–491. [Google Scholar] [CrossRef]
- Bird, H.A. Joint hypermobility in children. Rheumatology 2005, 44, 703–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lephart, S.M.; Pincivero, D.M.; Giraido, J.L.; Fu, F.H. The Role of Proprioception in the Management and Rehabilitation of Athletic Injuries. Am. J. Sports Med. 1997, 25, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Sainburg, R.L.; Poizner, H.; Ghez, C. Loss of proprioception produces deficits in interjoint coordination. J. Neurophysiol. 1993, 70, 2136–2147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, M.G.; Ferrell, W.R.; Sturrock, R.D.; Hamblen, D.L.; Baxendale, R.H. The Effect of The Hypermobility Syndrome on Knee Joint Proprioception. Rheumatology 1995, 34, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.N.; Ko, J.; Rosen, A.B.; Hsieh, K. Individuals with both perceived ankle instability and mechanical laxity demonstrate dynamic postural stability deficits. Clin. Biomech. 2015, 30, 1170–1174. [Google Scholar] [CrossRef] [PubMed]
- Geuze, R.H. Postural Control in Children with Developmental Coordination Disorder. Neural Plast. 2005, 12, 183–196. [Google Scholar] [CrossRef] [Green Version]
- Johnston, L.M.; Burns, Y.R.; Brauer, S.G.; Richardson, C.A. Differences in postural control and movement performance during goal directed reaching in children with developmental coordination disorder. Hum. Mov. Sci. 2002, 21, 583–601. [Google Scholar] [CrossRef]
- Romeo, D.M.; Velli, C.; Lucibello, S.; Ferrantini, G.; Leo, G.; Brogna, C.; Cota, F.; Ricci, D.; Gallini, F.; Romagnoli, C.; et al. Joint Laxity in Preschool Children Born Preterm. J. Pediatr. 2018, 197, 104–108. [Google Scholar] [CrossRef]
- Adib, N.; Davies, K.; Grahame, R.; Woo, P.; Murray, K.J. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology 2005, 44, 744–750. [Google Scholar] [CrossRef] [Green Version]
- Moore, N.; Rand, S.; Simmonds, J. Hypermobility, developmental coordination disorder and physical activity in an Irish paediatric population. Musculoskelet. Care 2019, 17, 261–269. [Google Scholar] [CrossRef] [Green Version]
- Wright, K.E.; Furzer, B.J.; Licari, M.K.; Dimmock, J.A.; Jackson, B.; Thornton, A.L. Exploring associations between neuromuscular performance, hypermobility, and children’s motor competence. J. Sci. Med. Sport 2020, 23, 1080–1085. [Google Scholar] [CrossRef]
- Jelsma, L.D.; Geuze, R.H.; Klerks, M.H.; Niemeijer, A.S.; Smits-Engelsman, B.C. The relationship between joint mobility and motor performance in children with and without the diagnosis of developmental coordination disorder. BMC Pediatr. 2013, 13, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tirosh, E.; Jaffe, M.; Marmur, R.; Taub, Y.; Rosenberg, Z. Prognosis of motor development and joint hypermobility. Arch. Dis. Child 1991, 66, 931–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Boer, R.M.; van Vlimmeren, L.A.; Scheper, M.C.; Nijhuis-van der Sanden, M.W.G.; Engelbert, R.H.H. Is Motor Performance in 5.5-Year-Old Children Associated with the Presence of Generalized Joint Hypermobility? J. Pediatrics 2015, 167, 694–701.e1. [Google Scholar] [CrossRef]
- Kirby, A.; Davies, R.; Bryant, A. Hypermobility syndrome and developmental coordination disorder: Similarities and features. Int. J. Ther. Rehabil. 2005, 12, 431–437. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Kristensen, J.H.; Frausing, B.; Jensen, D.V.; Røgind, H.; Remvig, L. Motor competence and physical activity in 8-year-old school children with generalized joint hypermobility. Pediatrics 2009, 124, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Remvig, L.; Kümmel, C.; Kristensen, J.H.; Boas, G.; Juul-Kristensen, B. Prevalence of generalized joint hypermobility, arthralgia and motor competence in 10-year-old school children. Int. Musculoskelet. Med. 2011, 33, 137–145. [Google Scholar] [CrossRef]
- Schubert-Hjalmarsson, E.; Öhman, A.; Kyllerman, M.; Beckung, E. Pain, balance, activity, and participation in children with hypermobility syndrome. Pediatr. Phys. Ther. 2012, 24, 339–344. [Google Scholar] [CrossRef] [Green Version]
- Easton, V.; Bale, P.; Bacon, H.; Jerman, E.; Armon, K.; Macgregor, A.J. The relationship between benign joint hypermobility syndrome and developmental coordination disorders in children. Arthritis Rheumatol. 2014, 66, S124. [Google Scholar] [CrossRef]
- Morrison, S.C.; Ferrari, J.; Smillie, S. Assessment of gait characteristics and orthotic management in children with Developmental Coordination Disorder: Preliminary findings to inform multidisciplinary care. Res. Dev. Disabil. 2013, 34, 3197–3201. [Google Scholar] [CrossRef]
- Celletti, C.; Mari, G.; Ghibellini, G.; Celli, M.; Castori, M.; Camerota, F. Phenotypic variability in developmental coordination disorder: Clustering of generalized joint hypermobility with attention deficit/hyperactivity disorder, atypical swallowing and narrative difficulties. Am. J. Med. Genet. Part C Semin. Med. Genet. 2015, 169C, 117–122. [Google Scholar] [CrossRef]
- Engelbert, R.H.; Kooijmans, F.T.; van Riet, A.M.; Feitsma, T.M.; Uiterwaal, C.S.; Helders, P.J. The relationship between generalized joint hypermobility and motor development. Pediatric Phys. Ther. 2005, 17, 258–263. [Google Scholar] [CrossRef]
- Fawcett, A.J.; Nicolson, R.I. Automatisation deficits in balance for dyslexic children. Percept. Mot. Skills 1992, 75, 507–529. [Google Scholar] [CrossRef]
- Laszlo, J.I.; Sainsbury, K.M. Perceptual-motor development and prevention of clumsiness. Psychol. Res. 1993, 55, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.H.; McKenzie, B.E. Information processing deficits associated with developmental coordination disorder: A meta-analysis of research findings. J. Child Psychol. Psychiatry 1998, 39, 829–840. [Google Scholar] [PubMed]
- Ekelund, U.; Sardinha, L.B.; Anderssen, S.A.; Harro, M.; Franks, P.W.; Brage, S.; Cooper, A.R.; Andersen, L.B.; Riddoch, C.; Froberg, K. Associations between objectively assessed physical activity and indicators of body fatness in 9- to 10-y-old European children: A population-based study from 4 distinct regions in Europe (the European Youth Heart Study). Am. J. Clin. Nutr. 2004, 80, 584–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Ref. | Author, Year | Type of Study | Sample N | Age of Assessment in Months (m) or Years (y) | Joint Hypermobility and Developmental Coordination Disorder | Assessment for DCD/Motor Performance | Assessment for Hypermobility | Others Instruments Used |
|---|---|---|---|---|---|---|---|---|
| [8] | Kirby, A. et al., 2007 | Case-Control | 54 | Control group: 5–18 years Case group: 9–17 years | Similar clinical features between JHS and DCD | M-ABC | Questionnaire | Questionnaire covering a range of symptoms consistent with a diagnosis of JHS and related autonomic nervous systemic symptoms |
| [19] | Romeo et al., 2018 | Longitudinal | 132 | From 12 months to 4 years | Children with joint laxity had lower scores than those without joint laxity on both total scores and subscores of M-ABC-2. | M-ABC-2 | Beighton Score (>4) | Touwen Infant Neurological Examination |
| [20] | Adib, N. et al., 2005 | Prospective and Retrospective | 125 | 3–17 years | Children with JHS present Joint pain and coordination problems in 36% | Clinical history | Beighton Score (≥4) | - |
| [21] | Moore, N. et al., 2019 | Cross-sectional, case-control, observational | 73 | 6–12 years | No significant difference in the number of children with pDCD in those with and without GJH. | Self-reported questionnaires Children: Physical Activity Questionnaire for older children Parent: Developmental Coordination Disorder Questionnaire | Beighton Score (≥6) | - |
| [22] | Wright, K.E. et al., 2020 | Cross-sectional observation | 60 | 6–12 years | Hypermobility failed to explain significant variance in motor competence beyond that explained by neuromuscular performance. | M-ABC-2 | Beighton score (>7) Lower Limb Assessment Score | Resistance Training Skills Battery for Children (RTSBc), 5-repetition maximum (5RM) leg press and Biodex dynamometry |
| [23] | Jelsma et al., 2013 | Case-control | Case group: 36 Control group: 352 | Case group 7–10 years Control group 3–16 years | In the DCD group the prevalence of hypermobility was higher and there was a significant negative correlation between the m-ABC total score and the degree of hyperextension of the knees. | M-ABC M-ABC-2 | Beighton score (≥5 for 3–9 years; ≥4 for >10 years) | - |
| [24] | Tirosh et al., 1991 | Longitudinal | 59 | 54–60 months | Both gross and fine motor performance were significantly delayed in the group of children with joint hypermobility and motor delay. | Gross motor performance. Parent perception of motor proficiency: | Clinical evaluation of the mobility of joints | - |
| [25] | De Boer et al., 2015 | Prospective | 249 | Mean 5.5 years | No significant association was found between GJH and total motor performance. | Bayley Scales of Infant Development, Second Edition M-ABC-2 | Beighton Score (≥4; ≥5; ≥6) | |
| [26] | Kirby et al., 2005 | Cohort | 126 | 8–9 years | Children with BJHS present functional difficulties that impact on fine and gross motor function. Children with BJHS and DCD have a similar range of functional difficulties. | M-ABC | Questionnaire | Hypermobility Syndrome Association developmental coordination disorder questionnaire |
| [27] | Juul-Kristensen, B. et al., 2009 | Cross-sectional | 349 | (8.40 ± 0.52) years | Static balance and speed reaction tests better in children with GJH The BJHS group did not perform worse than the non-BJHS group in any of the motor competence tests. There was no significant effect of any of the GJH groups in the parameters of PAL; no correlation between number of positive Beighton tests and PAL. | Clinical examination and motor competence tests | Questionnaire Beighton score (>4; >5; >6) Brighton Tests | Questionnaire with 75 items on health and physical activity |
| [28] | Remvig, L. et al., 2011 | Cohort | 315 | 10 years | Increased pain or frequency of injures were not related to GJH. Insignificant increased jump height by girls with joint hypermobility. Significant shorter hand reaction time in boys with GJH6. | Motor competence tests: | Beighton score (>4; >5; >6)Brighton Tests | Questionnaire with 75 items on health and physical activity |
| [29] | Schubert-Hjalmarsson et al., 2012 | Cross-sectional | Case group: 20 Control group: 24 | 8–15 years (11.2 ± 1.9) 8–15 years (11.4 ± 2) | Balance is decreased in children with HMS compared with healthy controls. | Bruininks-Oseretsky test of motor proficiency (balance) Positive association | Del Mar scale | Frequency of Partic- ipation Questionnaire Physical activity was reported in an activity diary |
| [30] | Easton, V. et al., 2014 | Interventional | 119 | 5–16 years | Among the children with BJHS assessed, 32.8% scored ≤15 percentile on the M-ABC (p < 0.001). | M-ABC-2 | Clinical evaluation | Childhood Health Assess- ment Questionnaire |
| [31] | Morrison, S.C. et al., 2013 | Interventional | 14 (14/0) | 6–11 years | Children with DCD were at the top end of the scale for lower limb hypermobility. | Not specified | Lower Limb Assessment Score Foot Posture Index | 6-Minute Walk Test GAITRite walkway |
| [32] | Celletti, C. et al., 2015 | Observational | 41 | Mean age 8 ± 3 years | Children with DCD and GJH showed a significant excess of frequent falls, easy bruising, motor impersistence. | M-ABC VMI | Beighton score (≥5 for 3–9 years; ≥4 for >10 years) | Linguistic Comprehension Test, Peabody Picture Vocabulary Test, Boston Naming Test, Bus Story Test, and Memoria-Training tests WISC-IV |
| [33] | Engelbert et al., 2005 | observational | 56 | 4–12 years | No significant association between the presence of a delay in motor development and joint hypermobility | M-ABC | Bulbena criteria | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romeo, D.M.; Venezia, I.; De Biase, M.; Ascione, F.; Lala, M.R.; Arcangeli, V.; Mercuri, E.; Brogna, C. Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review. Children 2022, 9, 1011. https://doi.org/10.3390/children9071011
Romeo DM, Venezia I, De Biase M, Ascione F, Lala MR, Arcangeli V, Mercuri E, Brogna C. Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review. Children. 2022; 9(7):1011. https://doi.org/10.3390/children9071011
Chicago/Turabian StyleRomeo, Domenico M., Ilaria Venezia, Margherita De Biase, Federica Ascione, Maria Rosaria Lala, Valentina Arcangeli, Eugenio Mercuri, and Claudia Brogna. 2022. "Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review" Children 9, no. 7: 1011. https://doi.org/10.3390/children9071011
APA StyleRomeo, D. M., Venezia, I., De Biase, M., Ascione, F., Lala, M. R., Arcangeli, V., Mercuri, E., & Brogna, C. (2022). Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review. Children, 9(7), 1011. https://doi.org/10.3390/children9071011







