Long-Term Outcomes of Congenital Diaphragmatic Hernia: Report of a Multicenter Study in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Patient Variables
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics and Mortality
3.2. Recurrence of CDH
3.3. Long-Term Cardiopulmonary Complications
3.4. Long-Term Gastrointestinal Complications
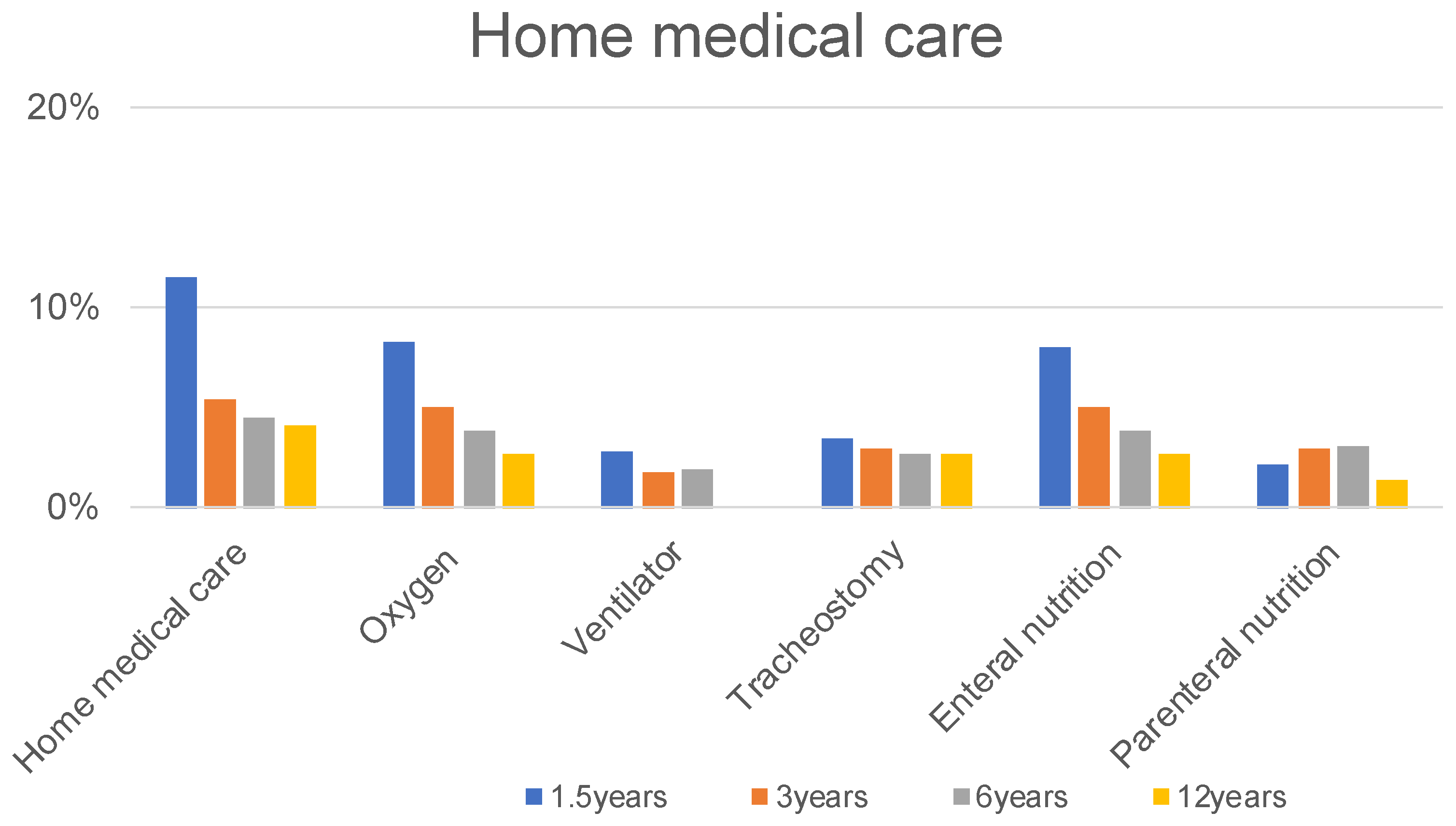
3.5. Long-Term Other Complications
4. Discussion
4.1. Recurrence
4.2. Cardiopulmonary Complications
4.2.1. PPH
4.2.2. Pneumonia
4.3. Gastrointestinal Complications
4.3.1. GERD
4.3.2. Intestinal Obstruction
4.4. Other Complications
4.4.1. Thoracic Deformity
4.4.2. Hearing Loss
4.4.3. Undescended Testis
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gischler, S.J.; Mazer, P.; Duivenvoorden, H.J.; van Dijk, M.; Bax, N.M.; Hazebroek, F.W.; Tibboel, D. Interdisciplinary structural follow-up of surgical newborns: A prospective evaluation. J. Pediatr. Surg. 2009, 44, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- Muratore, C.S.; Wilson, J.M. Congenital diaphragmatic hernia: Where are we and where do we go from here? Semin. Perinatol. 2000, 24, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Harting, M.T.; Lally, K.P. The Congenital Diaphragmatic Hernia Study Group registry update. Semin. Fetal Neonatal Med. 2014, 19, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Hollinger, L.E.; Harting, M.T.; Lally, K.P. Long-term follow-up of congenital diaphragmatic hernia. Semin. Pediatr. Surg. 2017, 26, 178–184. [Google Scholar] [CrossRef]
- Tan, J.K.; Banton, G.; Minutillo, C.; Hall, G.; Wilson, A.; Murray, C.; Nathan, E.A.; Verheggen, M.; Ramsay, J.; Samnakay, N.; et al. Long-term medical and psychosocial outcomes in congenital diaphragmatic hernia survivors. Arch. Dis. Child. 2019, 104, 761–767. [Google Scholar] [CrossRef]
- Gerall, C.D.; Stewart, L.A.; Price, J.; Kabagambe, S.; Sferra, S.R.; Schmaedick, M.J.; Hernan, R.; Khlevner, J.; Krishnan, U.S.; De, A.; et al. Long-term outcomes of congenital diaphragmatic hernia: A single institution experience. J. Pediatr. Surg. 2021, 57, 563–569. [Google Scholar] [CrossRef]
- Abramov, A.; Fan, W.; Hernan, R.; Zenilman, A.L.; Wynn, J.; Aspelund, G.; Khlevner, J.; Krishnan, U.; Lim, F.-Y.; Mychaliska, G.; et al. Comparative outcomes of right versus left congenital diaphragmatic hernia: A multicenter analysis. J. Pediatr. Surg. 2020, 55, 33–38. [Google Scholar] [CrossRef] [Green Version]
- Aydın, E.; Nolan, H.; Peiró, J.L.; Burns, P.; Rymeski, B.; Lim, F.-Y. When primary repair is not enough: A comparison of synthetic patch and muscle flap closure in congenital diaphragmatic hernia? Pediatr. Surg. Int. 2020, 36, 485–491. [Google Scholar] [CrossRef]
- Heiwegen, K.; van Rooij, I.A.L.M.; van Heijst, A.; de Blaauw, I.; Botden, S.M.B.I. Surgical Complications in Children with CDH: A Multivariate Analysis. World J. Surg. 2020, 44, 2042–2048. [Google Scholar] [CrossRef] [Green Version]
- Kamran, A.; Zendejas, B.; Demehri, F.R.; Nath, B.; Zurakowski, D.; Smithers, C.J. Risk factors for recurrence after thoracoscopic repair of congenital diaphragmatic hernia (CDH). J. Pediatr. Surg. 2018, 53, 2087–2091. [Google Scholar] [CrossRef]
- Kraemer, U.S.; Leeuwen, L.; Krasemann, T.B.; Wijnen, R.M.H.; Tibboel, D.; Ijsselstijn, H. Characteristics of Infants with Congenital Diaphragmatic Hernia Who Need Follow-Up of Pulmonary Hypertension. Pediatr. Crit. Care Med. 2018, 19, e219–e226. [Google Scholar] [CrossRef] [PubMed]
- Jancelewicz, T.; Vu, L.T.; Keller, R.L.; Bratton, B.; Lee, H.; Farmer, D.; Harrison, M.; Miniati, D.; Mackenzie, T.; Hirose, S.; et al. Long-term surgical outcomes in congenital diaphragmatic hernia: Observations from a single institution. J. Pediatr. Surg. 2010, 45, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Moss, R.; Chen, C.M.; Harrison, M.R. Prosthetic patch durability in congenital diaphragmatic hernia: A long-term follow-up study. J. Pediatr. Surg. 2001, 36, 152–154. [Google Scholar] [CrossRef] [PubMed]
- Terui, K.; Nagata, K.; Ito, M.; Yamoto, M.; Shiraishi, M.; Taguchi, T.; Hayakawa, M.; Okuyama, H.; Yoshida, H.; Masumoto, K.; et al. Surgical approaches for neonatal congenital diaphragmatic hernia: A systematic review and meta-analysis. Pediatr. Surg. Int. 2015, 31, 891–897. [Google Scholar] [CrossRef]
- Okawada, M.; Ohfuji, S.; Yamoto, M.; Urushihara, N.; Terui, K.; Nagata, K.; Taguchi, T.; Hayakawa, M.; Amari, S.; Masumoto, K.; et al. Thoracoscopic repair of congenital diaphragmatic hernia in neonates: Findings of a multicenter study in Japan. Surg. Today 2021, 51, 1694–1702. [Google Scholar] [CrossRef] [PubMed]
- Shieh, H.F.; Wilson, J.M.; Sheils, C.A.; Smithers, C.J.; Kharasch, V.S.; Becker, R.E.; Studley, M.; Morash, D.; Buchmiller, T.L. Does the ex utero intrapartum treatment to extracorporeal membrane oxygenation procedure change morbidity outcomes for high-risk congenital diaphragmatic hernia survivors? J. Pediatr. Surg. 2017, 52, 22–25. [Google Scholar] [CrossRef]
- Vu, L.T.; McFarland, C.; Bratton, B.; Lee, H. Closer Look at the Nutritional Outcomes of Patients After Primary Repair of Congenital Diaphragmatic Hernia. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 237–241. [Google Scholar] [CrossRef]
- Morandi, A.; Macchini, F.; Ophorst, M.; Borzani, I.; Ciralli, F.; Farolfi, A.; Porro, G.A.; Franzini, S.; Fabietti, I.; Persico, N.; et al. Tracheal Diameter and Respiratory Outcome in Infants with Congenital Diaphragmatic Hernia Treated by Fetal Endoscopic Tracheal Occlusion. Fetal Diagn. Ther. 2019, 46, 296–305. [Google Scholar] [CrossRef]
- Burgos, C.M.; Modée, A.; Öst, E.; Frenckner, B. Addressing the causes of late mortality in infants with congenital diaphragmatic hernia. J. Pediatr. Surg. 2017, 52, 526–529. [Google Scholar] [CrossRef]
- Morini, F.; Valfrè, L.; Bagolan, P. Long-term morbidity of congenital diaphragmatic hernia: A plea for standardization. Semin. Pediatr. Surg. 2017, 26, 301–310. [Google Scholar] [CrossRef]
- American Academy of Pediatrics Section on Section on Surgery and the Committee on Fetus and Newborn Postdischarge Follow-up of Infants with Congenital Diaphragmatic Hernia. Pediatrics 2008, 121, 627–632. [CrossRef] [PubMed] [Green Version]
- Abman, S.H.; Hansmann, G.; Archer, S.L.; Ivy, D.D.; Adatia, I.; Chung, W.K.; Hanna, B.D.; Rosenzweig, E.B.; Raj, J.U.; Cornfield, D.; et al. Pediatric Pulmonary Hypertension: Guidelines from the American Heart Association and American Thoracic Society. Circulation 2015, 132, 2037–2099. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Dassios, T.; Khaliq, S.A.; Williams, E.E.; Tamura, K.; Davenport, M.; Greenough, A. Outcomes of infants with congenital diaphragmatic hernia by side of defect in the FETO era. Pediatr. Surg. Int. 2019, 35, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Long, A.-M.; Bunch, K.J.; Knight, M.; Kurinczuk, J.J.; Losty, P.D. One-year outcomes of infants born with congenital diaphragmatic hernia: A national population cohort study. Arch. Dis. Child.-Fetal Neonatal Ed. 2019, 104, F643–F647. [Google Scholar] [CrossRef] [PubMed]
- Leeuwen, L.; Mous, D.S.; van Rosmalen, J.; Olieman, J.F.; Andriessen, L.; Gischler, S.J.; Joosten, K.F.; Wijnen, R.M.; Tibboel, D.; Ijsselstijn, H.; et al. Congenital Diaphragmatic Hernia and Growth to 12 Years. Pediatrics 2017, 140, e20163659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taczalska, A.; Piaseczna-Piotrowska, A.; Koziarkiewicz, M. Long-Term Follow-Up of Children with Congenital Diaphragmatic Hernia—Observations from a Single Institution. Eur. J. Pediatr. Surg. 2014, 24, 500–507. [Google Scholar] [CrossRef]
- Bagolan, P.; Morini, F. Long-term follow up of infants with congenital diaphragmatic hernia. Semin. Pediatr. Surg. 2007, 16, 134–144. [Google Scholar] [CrossRef]
- Leeuwen, L.; Fitzgerald, A.D. Congenital diaphragmatic hernia. J. Paediatr. Child Health 2014, 50, 667–673. [Google Scholar] [CrossRef]
- Fasching, G.; Huber, A.; Uray, E.; Sorantin, E.; Lindbichler, F.; Mayr, J. Gastroesophageal Reflux and Diaphragmatic Motility after Repair of Congenital Diaphragmatic Hernia. Eur. J. Pediatr. Surg. 2000, 10, 360–364. [Google Scholar] [CrossRef]
- Kieffer, J.; Sapin, E.; Berg, A.; Beaudoin, S.; Bargy, F.; Helardot, P. Gastroesophageal reflux after repair of congenital diaphragmatic hernia. J. Pediatr. Surg. 1995, 30, 1330–1333. [Google Scholar] [CrossRef]
- Nagaya, M.; Akatsuka, H.; Kato, J. Gastroesophageal reflux occurring after repair of congenital diaphragmatic hernia. J. Pediatr. Surg. 1994, 29, 1447–1451. [Google Scholar] [CrossRef]
- Sigalet, D.; Nguyen, L.; Adolph, V.; Laberge, J.-M.; Hong, A.; Guttman, F. Gastroesophageal reflux associated with large diaphragmatic hernias. J. Pediatr. Surg. 1994, 29, 1262–1265. [Google Scholar] [CrossRef]
- Arcos-Machancoses, J.V.; Hernández, C.R.; De Carpi, J.M.; Pisón, S.P. A systematic review with meta-analysis of the prevalence of gastroesophageal reflux in congenital diaphragmatic hernia pediatric survivors. Dis. Esophagus 2018, 31. [Google Scholar] [CrossRef]
- Campanozzi, A.; Boccia, G.; Pensabene, L.; Panetta, F.; Marseglia, A.; Strisciuglio, P.; Barbera, C.; Magazzù, G.; Pettoello-Mantovani, M.; Staiano, A. Prevalence and Natural History of Gastroesophageal Reflux: Pediatric Prospective Survey. Pediatrics 2009, 123, 779–783. [Google Scholar] [CrossRef] [PubMed]
- Koivusalo, A.I.; Pakarinen, M.P.; Lindahl, H.G.; Rintala, R. The cumulative incidence of significant gastroesophageal reflux in patients with congenital diaphragmatic hernia—A systematic clinical, pH-metric, and endoscopic follow-up study. J. Pediatr. Surg. 2008, 43, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Chamond, C.; Morineau, M.; Gouizi, G.; Bargy, F.; Beaudoin, S. Preventive Antireflux Surgery in Patients with Congenital Diaphragmatic Hernia. World J. Surg. 2008, 32, 2454–2458. [Google Scholar] [CrossRef] [PubMed]
- Maier, S.; Zahn, K.; Wessel, L.M.; Schaible, T.; Brade, J.; Reinshagen, K. Preventive antireflux surgery in neonates with congenital diaphragmatic hernia: A single-blinded prospective study. J. Pediatr. Surg. 2011, 46, 1510–1515. [Google Scholar] [CrossRef]
- Peter, S.D.S.; Valusek, P.A.; Tsao, K.; Holcomb, G.W.; Ostlie, D.J.; Snyder, C.L. Abdominal Complications Related to Type of Repair for Congenital Diaphragmatic Hernia. J. Surg. Res. 2007, 140, 234–236. [Google Scholar] [CrossRef]
- Baoquan, Q.; Diez-Pardo, J.A.; Tovar, J.A. Intestinal rotation in experimental congenital diaphragmatic hernia. J. Pediatr. Surg. 1995, 30, 1457–1462. [Google Scholar] [CrossRef]
- Hosgor, M.; Karaca, I.; Karkıner, A.; Ucan, B.; Temir, G.; Erdag, G.; Fescekoglu, O. Associated malformations in delayed presentation of congenital diaphragmatic hernia. J. Pediatr. Surg. 2004, 39, 1073–1076. [Google Scholar] [CrossRef]
- Ward, E.P.; Wang, A.; Thangarajah, H.; Lazar, D.; Bickler, S.; Fairbanks, T.; Kling, K.M. Preemptive Ladd Procedure in congenital diaphragmatic hernia and Abdominal Wall defects does not reduce the risk of future volvulus. J. Pediatr. Surg. 2017, 52, 1956–1961. [Google Scholar] [CrossRef] [PubMed]
- Kuklova, P.; Zemková, D.; Kyncl, M.; Pýcha, K.; Stranak, Z.; Melichar, J.; Šnajdauf, J.; Rygl, M. Large diaphragmatic defect: Are skeletal deformities preventable? Pediatr. Surg. Int. 2011, 27, 1343–1349. [Google Scholar] [CrossRef] [PubMed]
- Tsiligiannis, T.; Grivas, T. Pulmonary function in children with idiopathic scoliosis. Scoliosis 2012, 7, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Agostino, J.A.; Bernbaum, J.C.; Gerdes, M.; Schwartz, I.P.; Coburn, E.C.; Hirschl, R.B.; Baumgart, S.; Polin, R.A. Outcome for infants with congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: The first year. J. Pediatr. Surg. 1995, 30, 10–15. [Google Scholar] [CrossRef]
- Aydın, E.; Özler, O.; Burns, P.; Lim, F.-Y.; Peiró, J.L. Left congenital diaphragmatic hernia-associated musculoskeletal deformities. Pediatr. Surg. Int. 2019, 35, 1265–1270. [Google Scholar] [CrossRef]
- Jancelewicz, T.; Chiang, M.; Oliveira, C.; Chiu, P.P. Late surgical outcomes among congenital diaphragmatic hernia (CDH) patients: Why long-term follow-up with surgeons is recommended. J. Pediatr. Surg. 2013, 48, 935–941. [Google Scholar] [CrossRef]
- Masumoto, K.; Nagata, K.; Uesugi, T.; Yamada, T.; Taguchi, T. Risk factors for sensorineural hearing loss in survivors with severe congenital diaphragmatic hernia. Eur. J. Pediatr. 2006, 166, 607–612. [Google Scholar] [CrossRef]
- Amoils, M.; Janik, M.C.; Lustig, L.R. Patterns and Predictors of Sensorineural Hearing Loss in Children with Congenital Diaphragmatic Hernia. JAMA Otolaryngol. Neck Surg. 2015, 141, 923–926. [Google Scholar] [CrossRef] [Green Version]
- Fligor, B.J.; Neault, M.W.; Mullen, C.H.; Feldman, H.A.; Jones, D.T. Factors Associated with Sensorineural Hearing Loss among Survivors of Extracorporeal Membrane Oxygenation Therapy. Pediatrics 2005, 115, 1519–1528. [Google Scholar] [CrossRef]
- Hutson, J.M.; Balic, A.; Nation, T.; Southwell, B. Cryptorchidism. Semin. Pediatr. Surg. 2010, 19, 215–224. [Google Scholar] [CrossRef]
- Cortes, D.; Kjellberg, E.M.; Breddam, M.; Thorup, J. The True Incidence of Cryptorchidism in Denmark. J. Urol. 2008, 179, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Fauza, D.O.; Wilson, J.M. Congenital diaphragmatic hernia and associated anomalies: Their incidence, identification, and impact on prognosis. J. Pediatr. Surg. 1994, 29, 1113–1117. [Google Scholar] [CrossRef]
- Lund, D.P.; Mitchell, J.; Kharasch, V.; Quigley, S.; Kuehn, M.; Wilson, J.M. Congenital diaphragmatic hernia: The hidden morbidity. J. Pediatr. Surg. 1994, 29, 258–264. [Google Scholar] [CrossRef]
- Benjamin, D.R.; Juul, S.; Siebert, J.R. Congenital posterolateral diaphragmatic hernia: Associated malformations. J. Pediatr. Surg. 1988, 23, 899–903. [Google Scholar] [CrossRef]


| Variables 1 | N or Median | (% or IQR) |
|---|---|---|
| Gender | ||
| Male | 340 | (54.3) |
| Female | 286 | (45.7) |
| Gestational age (week) | 37 | (37–38) |
| Birth weight (g) | 2724 | (2426–2990) |
| Genetic variant 2 | ||
| Mild | 9 | (1.4) |
| Severe | 8 | (1.3) |
| Cardiac malformation 2 | ||
| Mild | 35 | (5.6) |
| Severe | 24 | (3.8) |
| Neurological disorder 2 | ||
| Mild | 5 | (0.8) |
| Severe | 3 | (0.5) |
| CDH laterality | ||
| Left | 579 | (92.5) |
| Right | 46 | (7.3) |
| Bilateral | 1 | (0.2) |
| Diaphragmatic defect size 3 | ||
| Defect size A and B | 401 | (64.1) |
| Defect size C and D | 101 | (30.8) |
| Unknown | 32 | (5.1) |
| Position of the liver | ||
| Intra-abdominal | 419 | (66.9) |
| Intrathoracic | 207 | (33.1) |
| Fetal Endoscopic Tracheal Occlusion | 6 | (1) |
| Delivery | ||
| Vaginal birth | 224 | (35.8) |
| Caesarean section | 402 | (64.2) |
| Age at repair (days) | 2 | (2–3) |
| Surgical approach | ||
| Abdominal | 554 | (88.4) |
| Thoracic | 6 | (1) |
| Laparoscopy | 3 | (0.5) |
| Thoracoscopy | 63 | (10.1) |
| Repair method | ||
| Primary closure | 401 | (64.2) |
| Patch closure | 217 | (34.7) |
| Muscular tissue | 2 | (0.3) |
| Unknown | 5 | (0.8) |
| History of ECMO 4 | 29 | (4.6) |
| History of NO 5 | 420 | (67.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamoto, M.; Nagata, K.; Terui, K.; Hayakawa, M.; Okuyama, H.; Amari, S.; Yokoi, A.; Masumoto, K.; Okazaki, T.; Inamura, N.; et al. Long-Term Outcomes of Congenital Diaphragmatic Hernia: Report of a Multicenter Study in Japan. Children 2022, 9, 856. https://doi.org/10.3390/children9060856
Yamoto M, Nagata K, Terui K, Hayakawa M, Okuyama H, Amari S, Yokoi A, Masumoto K, Okazaki T, Inamura N, et al. Long-Term Outcomes of Congenital Diaphragmatic Hernia: Report of a Multicenter Study in Japan. Children. 2022; 9(6):856. https://doi.org/10.3390/children9060856
Chicago/Turabian StyleYamoto, Masaya, Kouji Nagata, Keita Terui, Masahiro Hayakawa, Hiroomi Okuyama, Shoichiro Amari, Akiko Yokoi, Kouji Masumoto, Tadaharu Okazaki, Noboru Inamura, and et al. 2022. "Long-Term Outcomes of Congenital Diaphragmatic Hernia: Report of a Multicenter Study in Japan" Children 9, no. 6: 856. https://doi.org/10.3390/children9060856
APA StyleYamoto, M., Nagata, K., Terui, K., Hayakawa, M., Okuyama, H., Amari, S., Yokoi, A., Masumoto, K., Okazaki, T., Inamura, N., Toyoshima, K., Koike, Y., Yazaki, Y., Furukawa, T., & Usui, N. (2022). Long-Term Outcomes of Congenital Diaphragmatic Hernia: Report of a Multicenter Study in Japan. Children, 9(6), 856. https://doi.org/10.3390/children9060856







