Coughing Can Be Modulated by the Hydration Status in Adolescents with Asthma
Abstract
1. Introduction
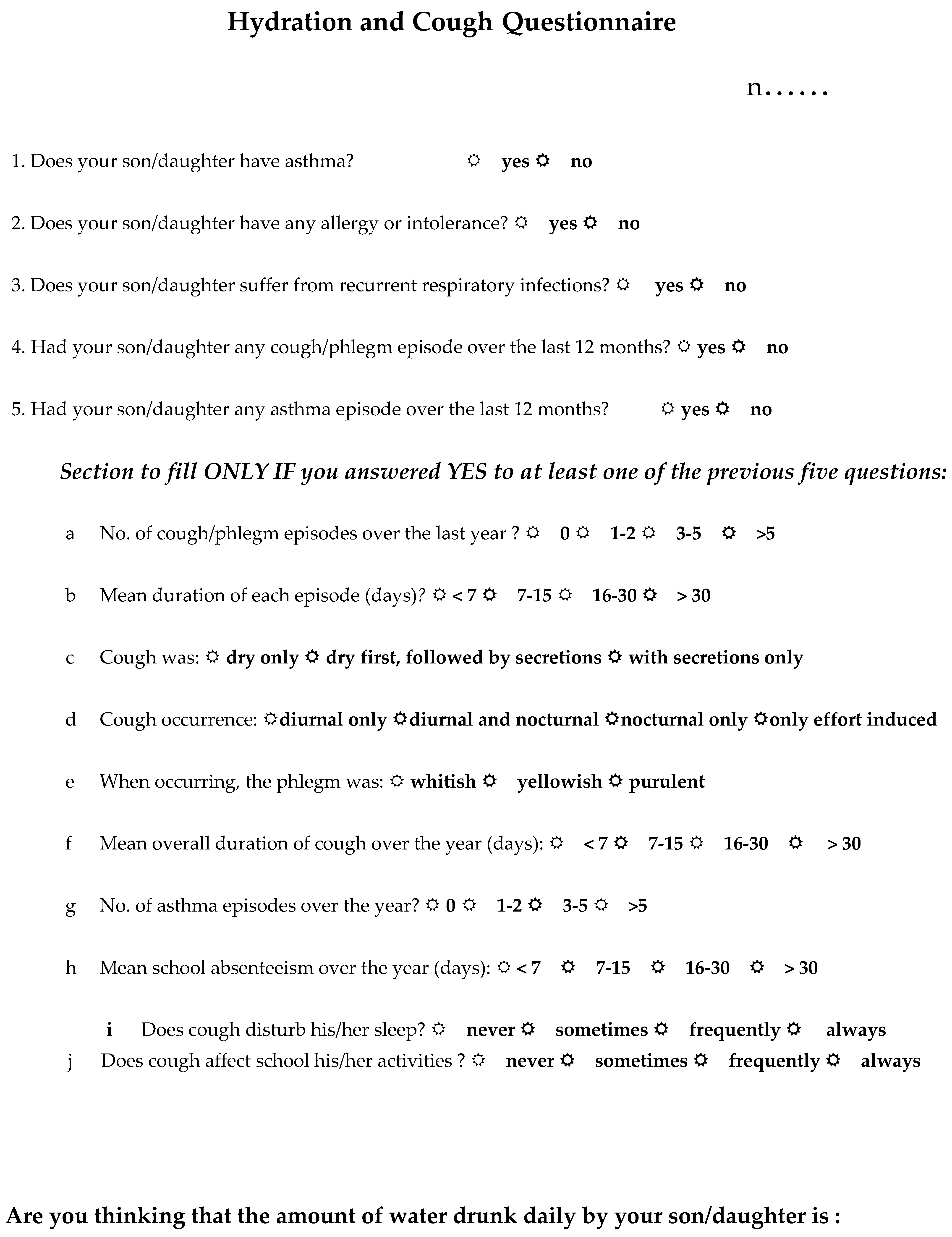
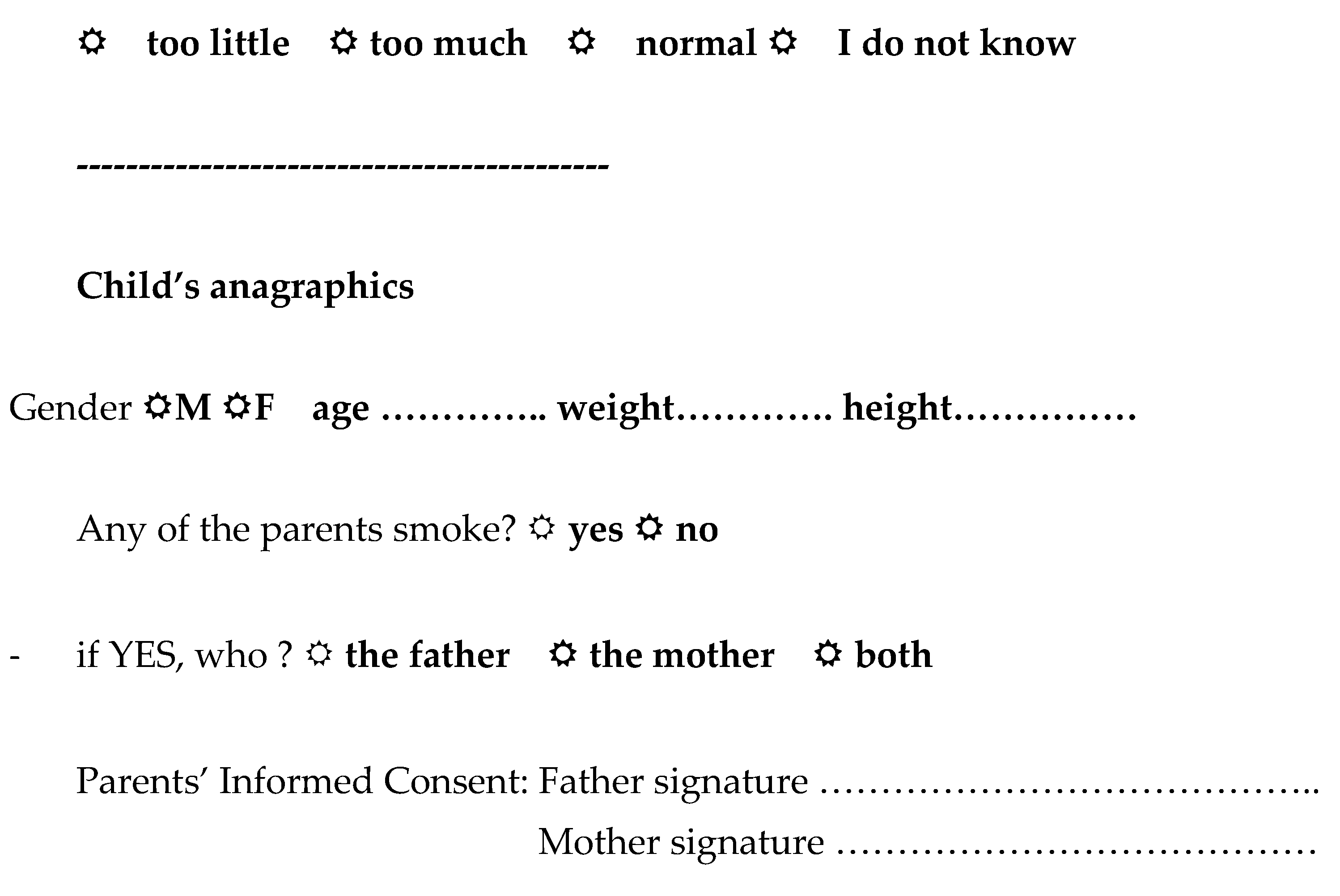
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Marchant, J.M.; Newcombe, P.A.; Juniper, E.F.; Sheffield, J.K.; Stathis, S.L.; Chang, A.B. What is the burden of chronic cough for families? Chest 2008, 134, 303–309. [Google Scholar] [CrossRef]
- Institute of Medicine of The National Academies. Dietary Reference Intakes: Electrolytes and Water. 2017. Available online: http://www.nationalacademies.org/hmd/Activities/Nutrition/SummaryDRIs/DRI-Tables.aspx (accessed on 4 April 2022).
- Jéquier, E.; Constant, F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 2010, 64, 115–123. [Google Scholar] [CrossRef]
- Diggins, K.C. Treatment of mild to moderate dehydration in children with oral rehydration therapy. J. Am. Acad. Nurse Pract. 2008, 20, 402–406. [Google Scholar] [CrossRef]
- Bar-David, Y.; Urkin, J.; Kozminsky, E. The effect of voluntary dehydration on cognitive functions of elementary school children. Acta Paediatr. 2005, 94, 1667–1673. [Google Scholar] [CrossRef]
- D’Anci, K.E.; Constant FRosenberg, I.H. Hydration and cognitive function in children. Nutr. Rev. 2006, 64, 457–464. [Google Scholar] [CrossRef]
- Kalhoff, H. Mild dehydration: A risk factor of broncho-pulmonary disorders? Eur. J. Clin. Nutr. 2003, 57, S81–S87. [Google Scholar] [CrossRef][Green Version]
- Bonnet, F.; Lepicard, E.M.; Cathrin, L.; Letellier, C.; Constant, F.; Hawili, N.; Friedlander, G. French children start their school day with a hydration deficit. Ann. Nutr. Metab. 2012, 60, 257–263. [Google Scholar] [CrossRef]
- Maloney, E.D.; Griffin, S.; Burke, C.M.; Poulter, L.W.; O’Sullivan, S. Release of inflammatory mediators from eosinophils following a hyperosmolar stimulus. Respir. Med. 2003, 97, 928–932. [Google Scholar] [CrossRef]
- Zanasi, A.; Mazzolini, M.; Fontana, G.A.; Bernacchi, G.; Fabbrizzi, A.; Dal Negro, R.W. Alterations in the Hydration Status Affect Coughing in Otherwise Normal School Children. World Wide J. Multidiscip. Res. Dev. 2021, 7, 50–54. [Google Scholar]
- Gouda, Z.; Zarea, M.; El-Hennawy, U.; Viltard, M.; Lepicard, E.M.; Ms, N.H.; Constant, F. Hydration Deficit in 9- to 11-Year-Old Egyptian Children. Glob. Pediatr. Health 2015, 2, 2333794X15611786. [Google Scholar] [CrossRef]
- El-Sharkawy, A.M.; Sahota, O.; Lobo, D.N. Acute and chronic effects of hydration status on health. Nutr. Rev. 2015, 73 (Suppl. 2), 97–109. [Google Scholar] [CrossRef]
- Manz, F.; Wentz, A. 24-h hydration status: Parameters, epidemiology and recommendations. Eur. J. Clin. Nutr. 2003, 57 (Suppl. 2), S10–S18. [Google Scholar] [CrossRef]
- Sands, J.M.; Layton, H.E. The Physiology of Urinary Concentration: An Update. Semin. Nephrol. 2009, 29, 178–195. [Google Scholar] [CrossRef]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of hydration status in a large population. Br. J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef]
- Assael, B.M.; Cipolli, M.; Meneghelli, I.; Passiu, M.; Cordioli, S.; Tridello, G.; Lepicard, E.M.; Constant, F.; Hawili, N.; Friedlander, G. Italian Children Go to School with a Hydration Deficit. J. Nutr. Disord. Ther. 2012, 2, 114. [Google Scholar] [CrossRef]
- Stookey JBrass, B.; Holliday, A.; Arieff, A. What is the cell hydration status of healthy children in the USA? Preliminary data on urine osmolality and water intake. Public Health Nutr. 2012, 15, 2148–2156. [Google Scholar] [CrossRef]
- Edmonds, C.J.; Burford, D. Should children drink more water?: The effects of drinking water on cognition in children. Appetite 2009, 52, 776–779. [Google Scholar] [CrossRef]
- Cian, C.; Barraud, P.A.; Melin, B.; Raphel, C. Effects of fluid ingestion on cognitive function after heat stress or exercise-induced dehydration. Int. J. Psychophysiol. 2001, 42, 243–251. [Google Scholar] [CrossRef]
- Carlton, A.; Orr, R. The effects of fluid loss on physical performance: A critical review. J. Sport Health Sci. 2015, 4, 357–363. [Google Scholar] [CrossRef][Green Version]
- Committee on Sport Medicine and Fitness. Climatic heat stress and the exercising child and adolescent. Pediatrics 2000, 106, 158–159. [Google Scholar] [CrossRef]
- Ghosh, A.; Boucher, R.C.; Tarran, R. Airway hydration in COPD. Cell Mol. Life Sci. 2015, 72, 3637–3652. [Google Scholar] [CrossRef]
- Kjaer, A.; Larsen, P.J.; Knigge, U.; Warberg, J. Dehydration stimulates hypothalamic gene expression of histamine synthesis enzyme: Importance for neuroendocrine regulation of vasopressin and oxytocin secretion. Endocrinology 1995, 136, 2189–2197. [Google Scholar] [CrossRef]
- Kjaer, A.; Knigge, U.; Rouleau, A.; Garbarg, M.; Warberg, J. Dehydration-induced release of vasopressin involves activation of hypothalamic histaminergic neurons. Endocrinology 1994, 135, 675–681. [Google Scholar] [CrossRef]
- Goldstein, D.J.; Halperin, J.A. Mast cell histamine and cell dehydration thirst. Nature 1977, 267, 250–252. [Google Scholar] [CrossRef]
- Moloney, E.; O’Sullivan, S.; Hogan, T.; Poulter, L.W.; Burke, C.M. Airway dehydration: A therapeutic target in asthma? Chest 2002, 121, 1806–1811. [Google Scholar] [CrossRef]
- Åstrand, A.B.M.; Hemmerling, M.; Root, J.; Wingren, C.; Pesic, J.; Johansson, E.; Garland, A.L.; Ghosh, A.; Tarran, R. Linking increased airway hydration, ciliary beating, and mucociliary clearance through ENaC inhibition. Am. J. Physiol. Cell. Mol. Physiol. 2015, 308, L22–L32. [Google Scholar] [CrossRef]
- Manz, F. Hydration and disease. J. Am. Coll. Nutr. 2007, 26 (Suppl. 5), 535S–541S. [Google Scholar] [CrossRef]
- Boucher, R.C. Evidence for airway surface dehydration as the initiating event in CF airway disease. J. Intern. Med. 2007, 261, 5–16. [Google Scholar] [CrossRef]
- Thornton, S.N.; Trabalon, M. Chronic dehydration is associated with obstructive sleep apnoea syndrome. Clin. Sci. 2014, 128, 225. [Google Scholar] [CrossRef]
- Högman, M.; Mörk, A.-C.; Roomans, G. Hypertonic saline increases tight junction permeability in airway epithelium. Eur. Respir. J. 2002, 20, 1444–1448. [Google Scholar] [CrossRef]
- Hess, A.S.; Abd-Elsayed, A. Observational Studies: Uses and Limitations; Abd-Elsayed, A., Ed.; Pain Springer: New York, NY, USA, 2019. [Google Scholar]
| Healthy Males (n = 155) | Asthmatic Males (n = 29) | Healthy Females (n = 150) | Asthmatic Females (n = 27) | |
|---|---|---|---|---|
| Age (years) | 11.6 ± 3.8 | 11.4 ± 4.1 | 11.9 ± 3.7 | 11.5 ± 3.9 |
| Weight (kg) | 39.7 ± 13.4 | 39.2 ± 12.9 | 38.1 ± 11.6 | 38.6 ± 12.0 |
| Height (cm) | 146.2 ± 16.0 | 145.8 ± 16.6 | 134.1 ± 11.0 | 135.2 ± 11.4 |
| BMI | 18.1 ± 3.2 | 17.9 ± 3.8 | 16.8 ± 2.6 | 17.1 ± 3.6 |
| Healthy Students (n = 305) | Asthmatic Students (n = 56) | p | |
|---|---|---|---|
| mOsm/kg | 837.1 ± 220.2 | 1012.4 ± 197.7 | 0.01 |
| % Prevalence | |||
| Normal osmolarity | 120 (39.3%) | 8 (14.3%) | 0.001 |
| Mild dehydration | 86 (28.2%) | 16 (28.6%) | 0.08 |
| Severe dehydration | 99 (32.4%) | 32 (57.1%) | 0.001 |
| Asymptomatic Asthmatic Students (n = 24) | Symptomatic Asthmatic Students (n = 32) | p | |
|---|---|---|---|
| mOsm/kg | 909.4 ± 190.7 | 1025 ± 191.6 | 0.01 |
| % Prevalence | |||
| ≤800 mOsm/kg | 6 (25.0%) | 2 (6.2%) | 0.001 |
| >800 mOsm/kg | 18 (75.0%) | 30 (93.8%) | 0.01 |
| Healthy Students (n = 305) | Asthmatic Students (n = 56) | |||
|---|---|---|---|---|
| ≤800 mOsm/kg (n = 120) | >800 mOsm/kg (n = 185) | ≤800 mOsm/kg (n = 8) | >800 mOsm/kg (n = 48) | |
| Cough episodes/year (n) | ||||
| 1–2 | 117 (97.5%) | 91 (49.2%) | 5 (62.5%) | 17 (35.4%) |
| 3–5 | 3 (2.5%) | 67 (36.2%) | 2 (25.0%) | 21 (43.8%) |
| >5 | 0 | 27 (14.6%) | 1 (12.5%) | 10 (20.8%) |
| p | 0.001 | 0.001 | ||
| Duration of episodes (days) | ||||
| <7 | 103 (85.8%) | 136 (73.5%) | 5 (62.5%) | 25 (52.1%) |
| 7–15 | 17 (14.2%) | 41 (22.2%) | 2 (25.0%) | 19 (39.6%) |
| 16–30 | 0 | 8 (4.3%) | 0 (12.5%) | 4 (8.3%) |
| p | 0.001 | 0.001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanasi, A.; Dal Negro, R.W. Coughing Can Be Modulated by the Hydration Status in Adolescents with Asthma. Children 2022, 9, 577. https://doi.org/10.3390/children9040577
Zanasi A, Dal Negro RW. Coughing Can Be Modulated by the Hydration Status in Adolescents with Asthma. Children. 2022; 9(4):577. https://doi.org/10.3390/children9040577
Chicago/Turabian StyleZanasi, Alessandro, and Roberto Walter Dal Negro. 2022. "Coughing Can Be Modulated by the Hydration Status in Adolescents with Asthma" Children 9, no. 4: 577. https://doi.org/10.3390/children9040577
APA StyleZanasi, A., & Dal Negro, R. W. (2022). Coughing Can Be Modulated by the Hydration Status in Adolescents with Asthma. Children, 9(4), 577. https://doi.org/10.3390/children9040577






