Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Musical Intervention
2.3. Data Collection
2.4. Statistical Analysis
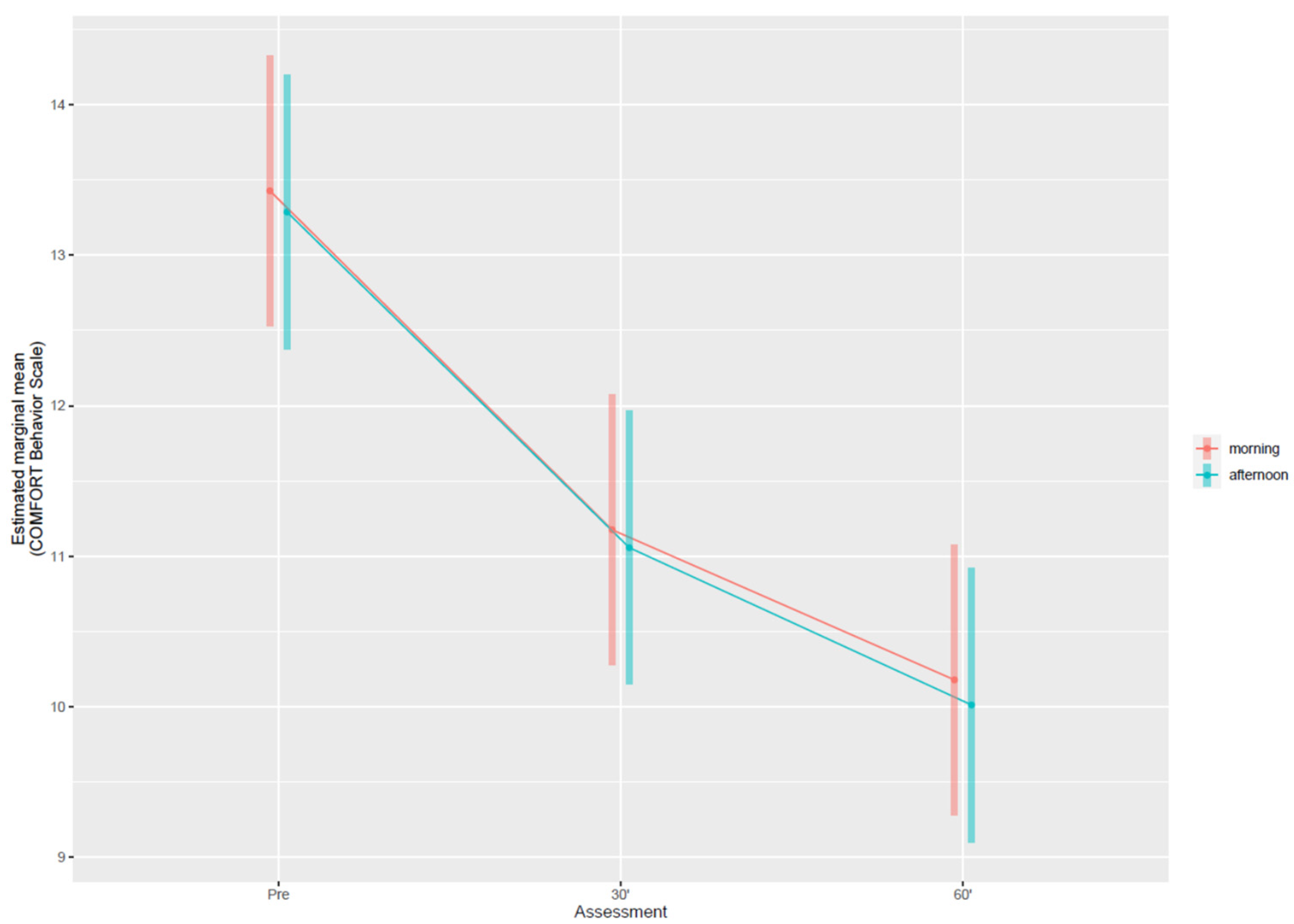
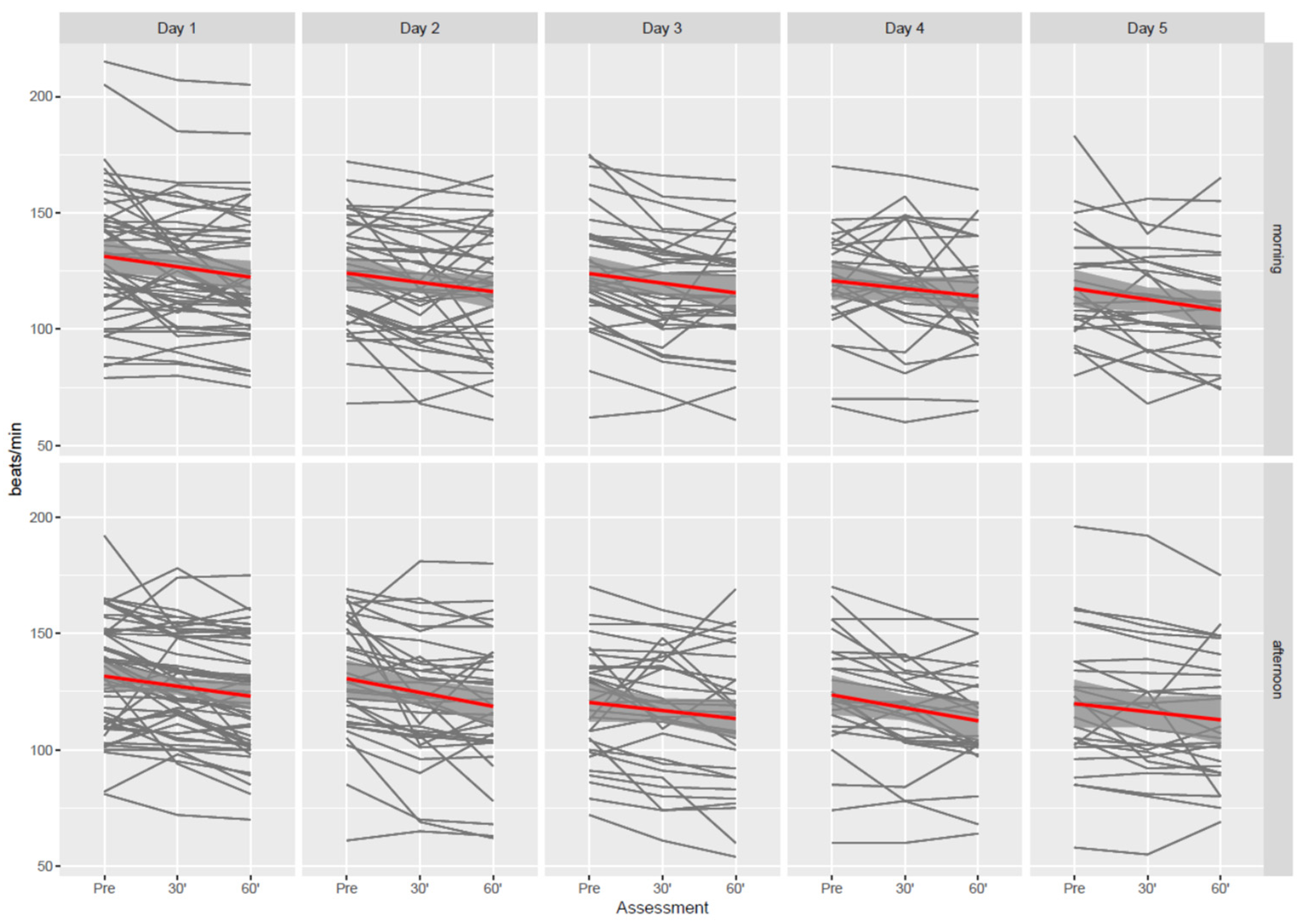
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ciğerci, Y.; Kısacık, Ö.G.; Özyürek, P.; Çevik, C. Nursing music intervention: A systematic mapping study. Complement. Ther. Clin. Pract. 2019, 35, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Drahota, A.; Ward, D.; Mackenzie, H.; Stores, R.; Higgins, B.; Gal, D.; Dean, T.P. Sensory environment on health-related outcomes of hospital patients. Cochrane Database Syst. Rev. 2012, 2012, 005315. [Google Scholar] [CrossRef]
- Mrázová, M.; Celec, P. A Systematic Review of Randomized Controlled Trials Using Music Therapy for Children. J. Altern. Complement. Med. 2010, 16, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.F.; Jiang, X.Y.; Chen, J.; Zeng, Z.; Chen, X.Y.; Li, Y.; Huining, X.; Evans, D.J.W. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst. Rev. 2015, 2015, 008808. [Google Scholar] [CrossRef] [PubMed]
- Messika, J.; Martin, Y.; Maquigneau, N.; Puechberty, C.; Henry-Lagarrigue, M.; Stoclin, A.; Panneckouke, N.; Villard, S.; Dechanet, A.; Lafourcade, A.; et al. A musical intervention for respiratory comfort during noninvasive ventilation in the ICU. Eur. Respir. J. 2019, 53, 1801873. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Rohlik, G.; Nemergut, M.; Tripathi, S. Comparison of staff and family perceptions of causes of noise pollution in the Pediatric Intensive Care Unit and suggested intervention strategies. Noise Health 2016, 18, 78. [Google Scholar] [CrossRef] [PubMed]
- Weatherhead, J.R.; Niedner, M.; Dahmer, M.K.; Malas, N.; Owens, T.; Kawai, Y. Patterns of Delirium in a Pediatric Intensive Care Unit and Associations with Noise Pollution. J. Intensive Care Med. 2021, 088506662110556. [Google Scholar] [CrossRef]
- Smith, J.R.; Pineda, R.G. Determining Appropriate Sensory Exposures in the NICU: Too Much, Too Little, or Just Right? Neonatal Netw. 2016, 35, 63–65. [Google Scholar] [CrossRef]
- Ko, M.S.M.; Poh, P.-F.; Heng, K.Y.C.; Sultana, R.; Murphy, B.; Ng, R.W.L.; Lee, J.H. Assessment of Long-term Psychological Outcomes After Pediatric Intensive Care Unit Admission: A Systematic Review and Meta-analysis. JAMA Pediatr. 2022, 176, 215767. [Google Scholar] [CrossRef]
- Foroushani, S.M.; Herman, C.A.; Wiseman, C.A.; Anthony, C.M.; Drury, S.S.; Howell, M.P. Evaluating physiologic outcomes of music interventions in the neonatal intensive care unit: A systematic review. J. Perinatol. 2020, 40, 1770–1779. [Google Scholar] [CrossRef]
- Tripathi, S.; Kaur, H.; Kashyap, R.; Dong, Y.; Gajic, O.; Murthy, S. A survey on the resources and practices in pediatric critical care of resource-rich and resource-limited countries. J. Intensive Care 2015, 3, 40. [Google Scholar] [CrossRef] [Green Version]
- Robb, S.L.; Carpenter, J.S.; Burns, D.S. Reporting guidelines for music-based interventions. J. Health Psychol. 2011, 16, 342–352. [Google Scholar] [CrossRef] [Green Version]
- United Nations High Commissioner for Refugees. Syria Emergency. 2021. Available online: https://www.unhcr.org (accessed on 8 December 2021).
- Bernardi, L.; Porta, C.; Sleight, P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: The importance of silence. Heart 2006, 92, 445–452. [Google Scholar] [CrossRef] [Green Version]
- Bernardi, L.; Porta, C.; Casucci, G.; Balsamo, R.; Bernardi, N.F.; Fogari, R.; Sleight, P. Dynamic interactions between musical, cardiovascular, and cerebral rhythms in humans. Circulation 2009, 119, 3171–3180. [Google Scholar] [CrossRef] [Green Version]
- Khalfa, S.; Roy, M.; Rainville, P.; Dalla Bella, S.; Peretz, I. Role of tempo entrainment in psychophysiological differentiation of happy and sad music? Int. J. Psychophysiol. 2008, 68, 17–26. [Google Scholar] [CrossRef]
- Modesti, P.A.; Ferrari, A.; Bazzini, C.; Costanzo, G.; Simonetti, I.; Taddei, S.; Biggeri, A.; Parati, G.; Gensini, G.F.; Sirigatti, S. Psychological predictors of the antihypertensive effects of music-guided slow breathing. J. Hypertens. 2010, 28, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Modesti, P.A.; Ferrari, A.; Bazzini, C.; Boddi, M. Time sequence of autonomic changes induced by daily slow-breathing sessions. Clin. Auton. Res. 2015, 25, 95–104. [Google Scholar] [CrossRef]
- Di Nasso, L.; Nizzardo, A.; Pace, R.; Pierleoni, F.; Pagavino, G.; Giuliani, V. Influences of 432 Hz Music on the Perception of Anxiety during Endodontic Treatment: A Randomized Controlled Clinical Trial. J. Endod. 2016, 42, 1338–1343. [Google Scholar] [CrossRef]
- Bernardi, N.F.; Codrons, E.; di Leo, R.; Vandoni, M.; Cavallaro, F.; Vita, G.; Bernardi, L. Increase in Synchronization of Autonomic Rhythms between Individuals When Listening to Music. Front. Physiol. 2017, 8, 785. [Google Scholar] [CrossRef]
- Clayton, M.; Sager, R.; Will, U. In time with the music: The concept of entrainment and its significance for ethnomusicology. Eur. Meet. Ethnomusicol. 2005, 11, 1–82. [Google Scholar]
- Filippa, M.; Lordier, L.; De Almeida, J.S.; Monaci, M.G.; Adam-Darque, A.; Grandjean, D.; Kuhn, P.; Hüppi, P.S. Early vocal contact and music in the NICU: New insights into preventive interventions. Pediatr. Res. 2020, 87, 249–264. [Google Scholar] [CrossRef]
- An, K.; Hasegawa, C.; Hirosawa, T.; Tanaka, S.; Saito, D.N.; Kumazaki, H.; Yaoi, K.; Kikuchi, M.; Yoshimura, Y. Brain responses to human-voice processing predict child development and intelligence. Hum. Brain Mapp. 2020, 41, 2292–2301. [Google Scholar] [CrossRef] [Green Version]
- Ista, E.; Van Dijk, M.; Tibboel, D.; De Hoog, M. Assessment of sedation levels in pediatric intensive care patients can be improved by using the COMFORT “behavior” scale. Pediatr. Crit. Care Med. 2005, 6, 58–63. [Google Scholar] [CrossRef] [Green Version]
- Vet, N.J.; Kleiber, N.; Ista, E.; de Hoog, M.; de Wildt, S.N. Sedation in Critically Ill Children with Respiratory Failure. Front. Pediatr. 2016, 4, 89. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. 2019. Available online: https://www.r-project.org (accessed on 8 December 2021).
- Alipour, Z.; Eskandari, N.; Ahmari Tehran, H.; Eshagh Hossaini, S.K.; Sangi, S. Effects of music on physiological and behavioral responses of premature infants: A randomized controlled trial. Complement. Ther. Clin. Pract. 2013, 19, 128–132. [Google Scholar] [CrossRef]
- Taheri, L.; Jahromi, M.K.; Abbasi, M.; Hojat, M. Effect of recorded male lullaby on physiologic response of neonates in NICU. Appl. Nurs. Res. 2017, 33, 127–130. [Google Scholar] [CrossRef]
- Schwilling, D.; Vogeser, M.; Kirchhoff, F.; Schwaiblmair, F.; Boulesteix, A.-L.; Schulze, A.; Flemmer, A.W. Live music reduces stress levels in very low-birthweight infants. Acta Paediatr. 2015, 104, 360–367. [Google Scholar] [CrossRef]
- Liu, M.H.; Zhu, L.H.; Peng, J.X.; Zhang, X.P.; Xiao, Z.H.; Liu, Q.J.; Qiu, J.; Latour, J.M. Effect of Personalized Music Intervention in Mechanically Ventilated Children in the PICU: A Pilot Study. Pediatr. Crit. Care Med. 2020, 21, 8–14. [Google Scholar] [CrossRef]
- Turner, H.C.; Hao, N.V.; Yacoub, S.; Hoang, V.M.T.; Clifton, D.A.; Thwaites, G.E.; Dondorp, A.M.; Thwaites, C.L.; Chau, N.V.V. Achieving affordable critical care in low-income and middle-income countries. BMJ Glob. Health 2019, 4, 001675. [Google Scholar] [CrossRef] [Green Version]
- Robb, S.L.; Hanson-Abromeit, D.; May, L.; Hernandez-Ruiz, E.; Allison, M.; Beloat, A.; Daugherty, S.; Kurtz, R.; Ott, A.; Oyedele, O.O.; et al. Reporting quality of music intervention research in healthcare: A systematic review. Complement. Ther. Med. 2018, 38, 24–41. [Google Scholar] [CrossRef]
- Kennelly, J.; Queensland, H.; Edwards, J. Providing music therapy to the unconscious child in the paediatric intensive care unit. Aust. J. Music Ther. 1997, 8, 18–29. [Google Scholar]
- Hatem, T.P.; Lira, P.I.C.; Mattos, S.S. The therapeutic effects of music in children following cardiac surgery. J. Pediatr. 2006, 82, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Garcia Guerra, G.; Joffe, A.R.; Sheppard, C.; Hewson, K.; Dinu, I.A.; Hajihosseini, M.; deCaen, A.; Jou, H.; Hartling, L.; Vohra, S. Music Use for Sedation in Critically ill Children (MUSiCC trial): A pilot randomized controlled trial. J. Intensive Care 2021, 9, 7. [Google Scholar] [CrossRef]
- Liu, Y.; Petrini, M.A. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complement. Ther. Med. 2015, 23, 714–718. [Google Scholar] [CrossRef]
- Wu, P.-Y.; Huang, M.-L.; Lee, W.-P.; Wang, C.; Shih, W.-M. Effects of music listening on anxiety and physiological responses in patients undergoing awake craniotomy. Complement. Ther. Med. 2017, 32, 56–60. [Google Scholar] [CrossRef]
- Thaut, M.H.; Hoemberg, V. (Eds.) Handbook of Neurologic Music Therapy; Oxford University Press: New York, NY, USA, 2014; ISBN 978-0-19-969546-1. (Hardcover). [Google Scholar]
- Fitzsimons, B. Approaching music therapy in a different country: A literature review on cultural considerations when practising in a developing country. Br. J. Music Ther. 2016, 30, 83–88. [Google Scholar] [CrossRef]
- What Is Islamic Music?|The Muslim 500. Available online: https://themuslim500.com/guest-contributions-2016/what-is-islamic-music/ (accessed on 23 December 2021).
- Van Der Heijden, M.J.E.; Araghi, S.O.; Van Dijk, M.; Jeekel, J.; Hunink, M.G.M. The Effects of Perioperative Music Interventions in Pediatric Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2015, 10, 0133608. [Google Scholar] [CrossRef] [Green Version]
- Hartling, L.; Newton, A.S.; Liang, Y.; Jou, H.; Hewson, K.; Klassen, T.P.; Curtis, S. Music to Reduce Pain and Distress in the Pediatric Emergency Department: A Randomized Clinical Trial. JAMA Pediatr. 2013, 167, 826–835. [Google Scholar] [CrossRef]
- Lee, J.H. The Effects of Music on Pain: A Meta-Analysis. J. Music Ther. 2016, 53, 430–477. [Google Scholar] [CrossRef]
- Green, P.; Macleod, C.J. SIMR: An R package for power analysis of generalized linear mixed models by simulation. Methods Ecol. Evol. 2015, 7, 493–498. [Google Scholar] [CrossRef]
| Characteristics | N = 59 |
|---|---|
| Age (years) | 2.0 (0.7–8.0) |
| Sex | |
| Male | 35 (59.0%) |
| Female | 24 (41.0%) |
| Religion | |
| Muslim | 49 (83.0%) |
| Yazidism | 10 (17.0%) |
| Admission Diagnosis | |
| Gastrointestinal | 18 (30.5%) |
| Neurologic | 15 (25.4%) |
| Cardiovascular | 7 (11.9%) |
| Trauma | 7 (11.9%) |
| Nephrological | 4 (6.8%) |
| Oncologic | 1 (1.7%) |
| Respiratory | 1 (1.7%) |
| Other diagnosis | 6 (10.2%) |
| Respiratory Support | N = 59 |
|---|---|
| Spontaneous breathing | 26 (44.1%) |
| High flow nasal cannula | 18 (30.5%) |
| Oxygen mask | 8 (13.6%) |
| Mechanical ventilation | 33 (55.9%) |
| Endotracheal tube | 30 (50.8%) |
| Tracheostomy tube | 3 (5.1%) |
| Vital Signs | |
| Heart rate (beats per minute) | 132.0 (114.0–148.0) |
| Systolic blood pressure (mmHg) | 114.0 (103.0–124.0) |
| Diastolic blood pressure (mmHg) | 64.0 (57.0–76.0) |
| Respiratory rate (breaths per minute) | 32.0 (29.0–41.0) |
| Oxygen saturation (%) | 100.0 (98.0–100.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buzzi, F.; Yahya, N.B.; Gambazza, S.; Binda, F.; Galazzi, A.; Ferrari, A.; Crespan, S.; Al-Atroushy, H.A.; Cantoni, B.M.; Laquintana, D.; et al. Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study. Children 2022, 9, 455. https://doi.org/10.3390/children9040455
Buzzi F, Yahya NB, Gambazza S, Binda F, Galazzi A, Ferrari A, Crespan S, Al-Atroushy HA, Cantoni BM, Laquintana D, et al. Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study. Children. 2022; 9(4):455. https://doi.org/10.3390/children9040455
Chicago/Turabian StyleBuzzi, Federica, Nizar Bakir Yahya, Simone Gambazza, Filippo Binda, Alessandro Galazzi, Antonella Ferrari, Stefano Crespan, Hevan Adel Al-Atroushy, Barbara Maria Cantoni, Dario Laquintana, and et al. 2022. "Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study" Children 9, no. 4: 455. https://doi.org/10.3390/children9040455
APA StyleBuzzi, F., Yahya, N. B., Gambazza, S., Binda, F., Galazzi, A., Ferrari, A., Crespan, S., Al-Atroushy, H. A., Cantoni, B. M., Laquintana, D., & Collaborative Group. (2022). Use of Musical Intervention in the Pediatric Intensive Care Unit of a Developing Country: A Pilot Pre–Post Study. Children, 9(4), 455. https://doi.org/10.3390/children9040455






