Impact of the First COVID Lockdown on Accident- and Injury-Related Pediatric Intensive Care Admissions in Germany—A Multicenter Study
Abstract
:1. Introduction
2. Methods
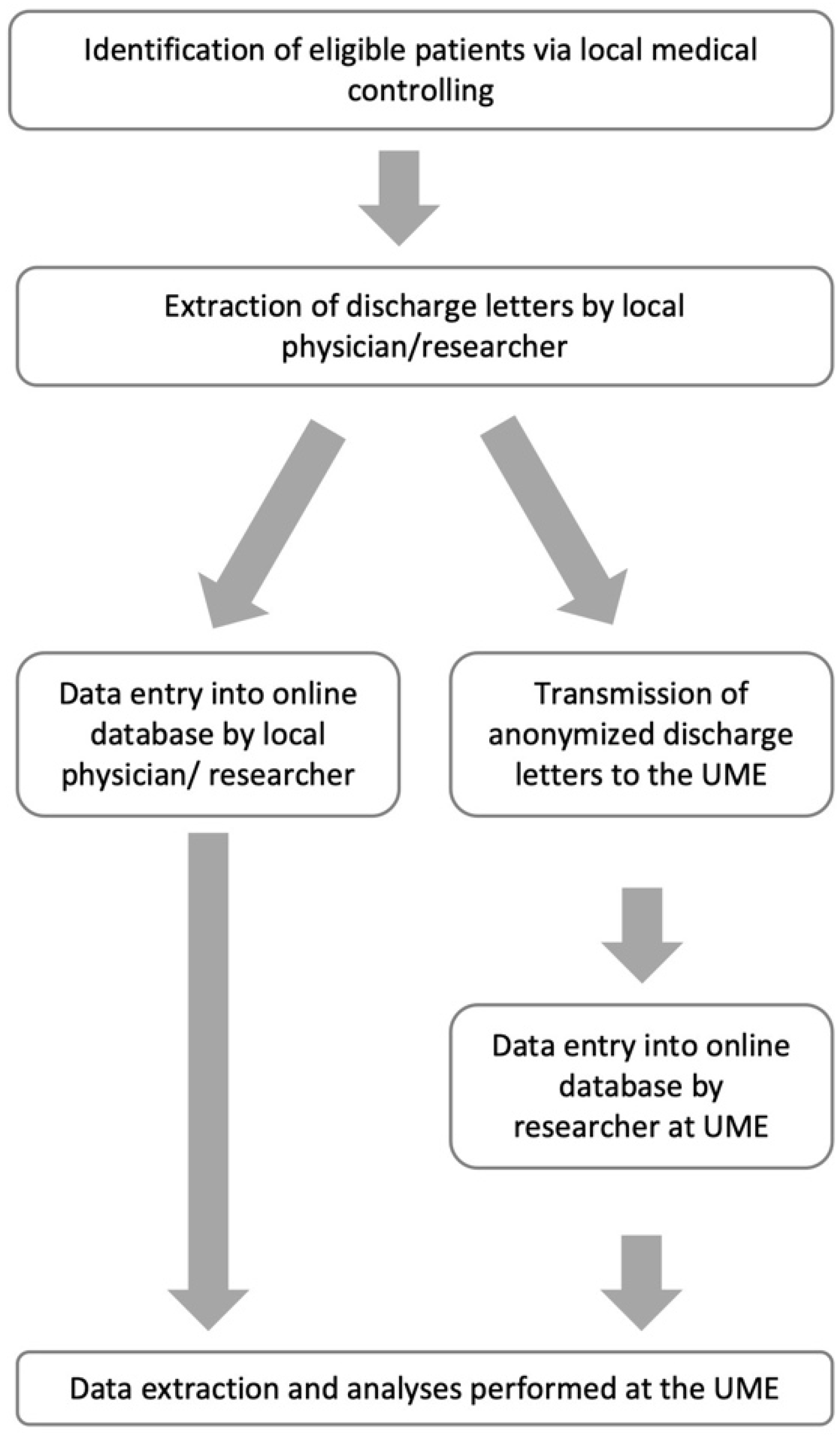
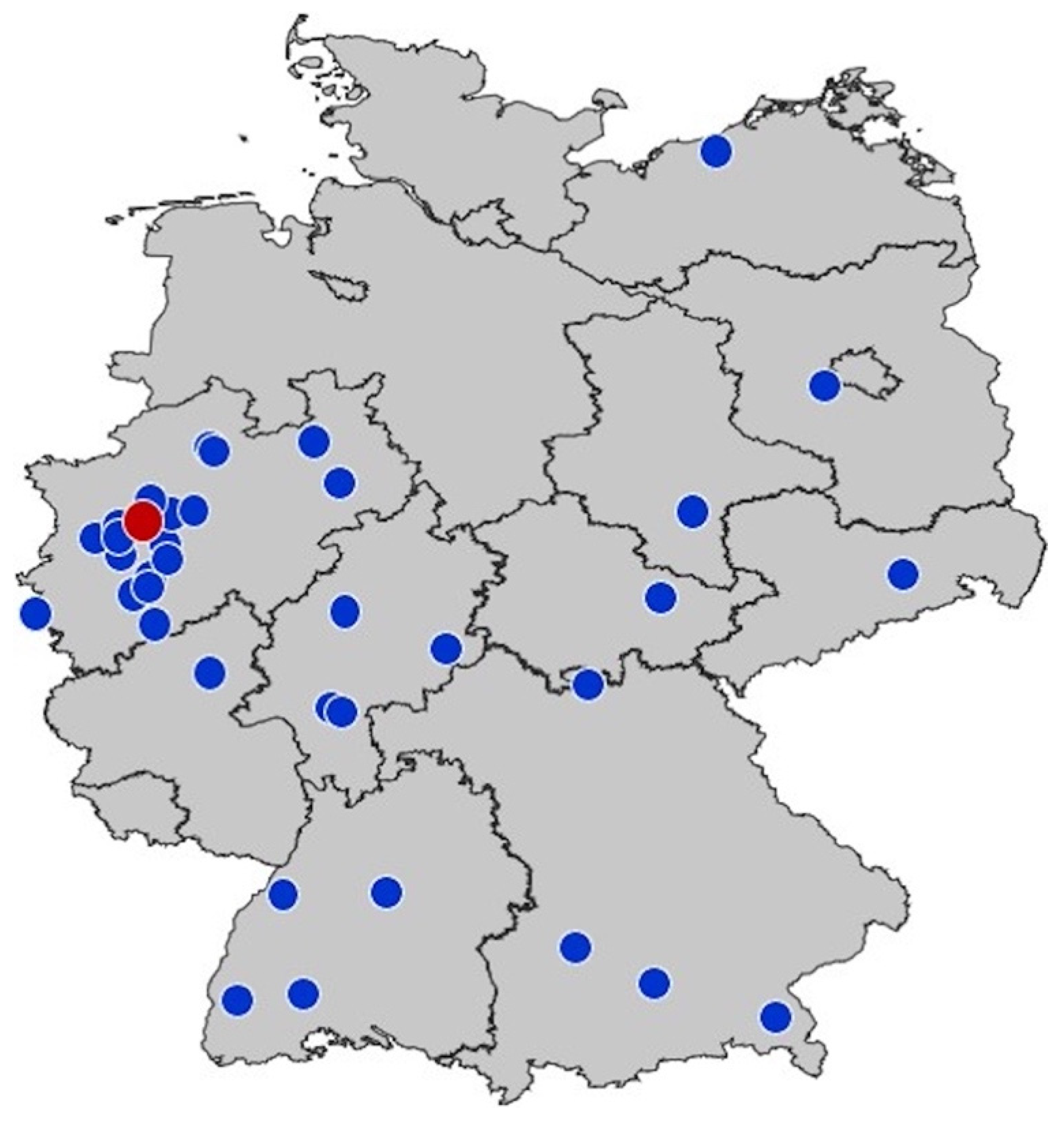
2.1. Study Design and Recruitment
2.2. Eligibility and Identification of Cases
2.3. German Lockdown
2.4. Data Acquisition
2.5. Statistical Analyses
2.6. Ethics Approval
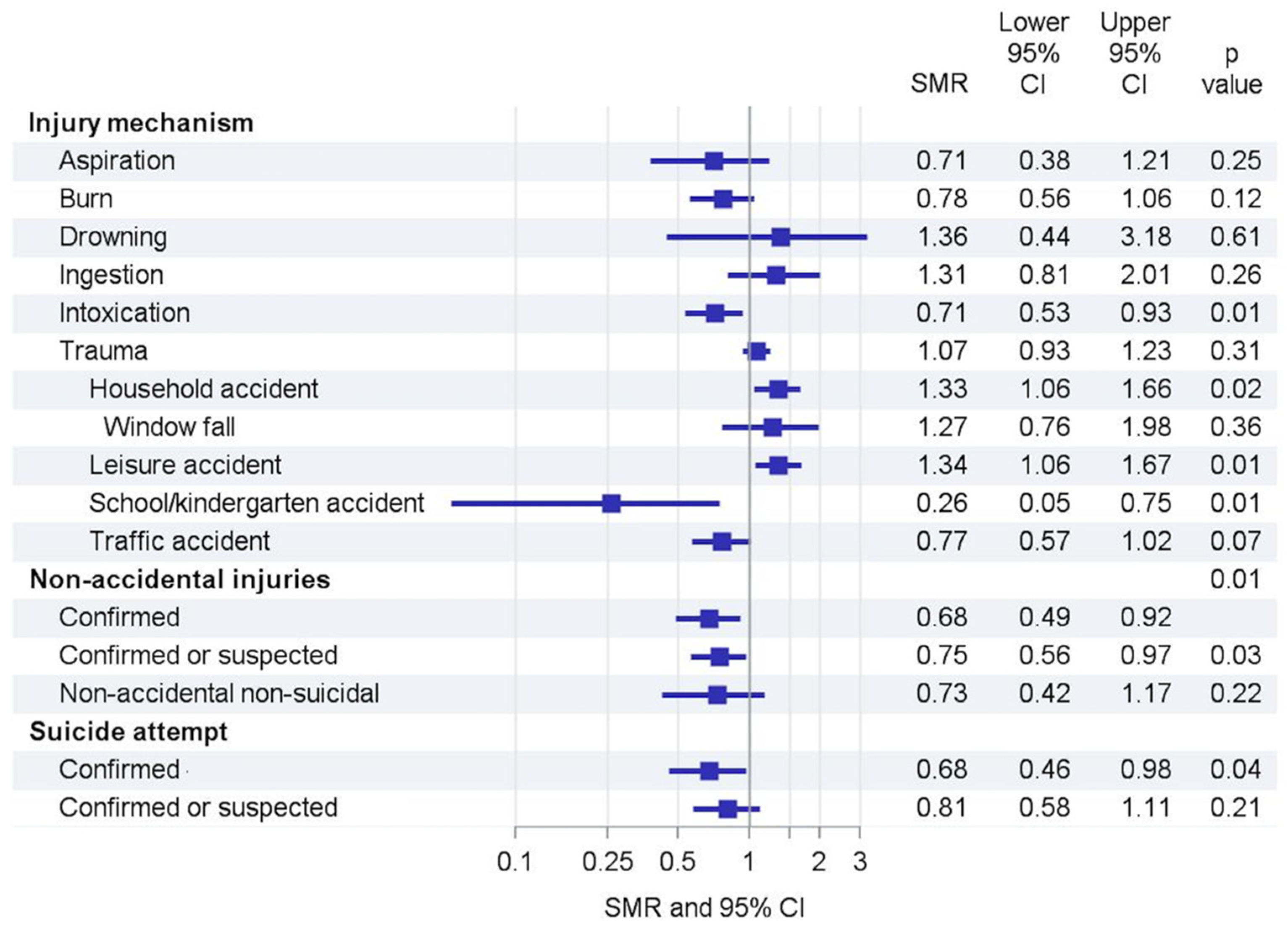
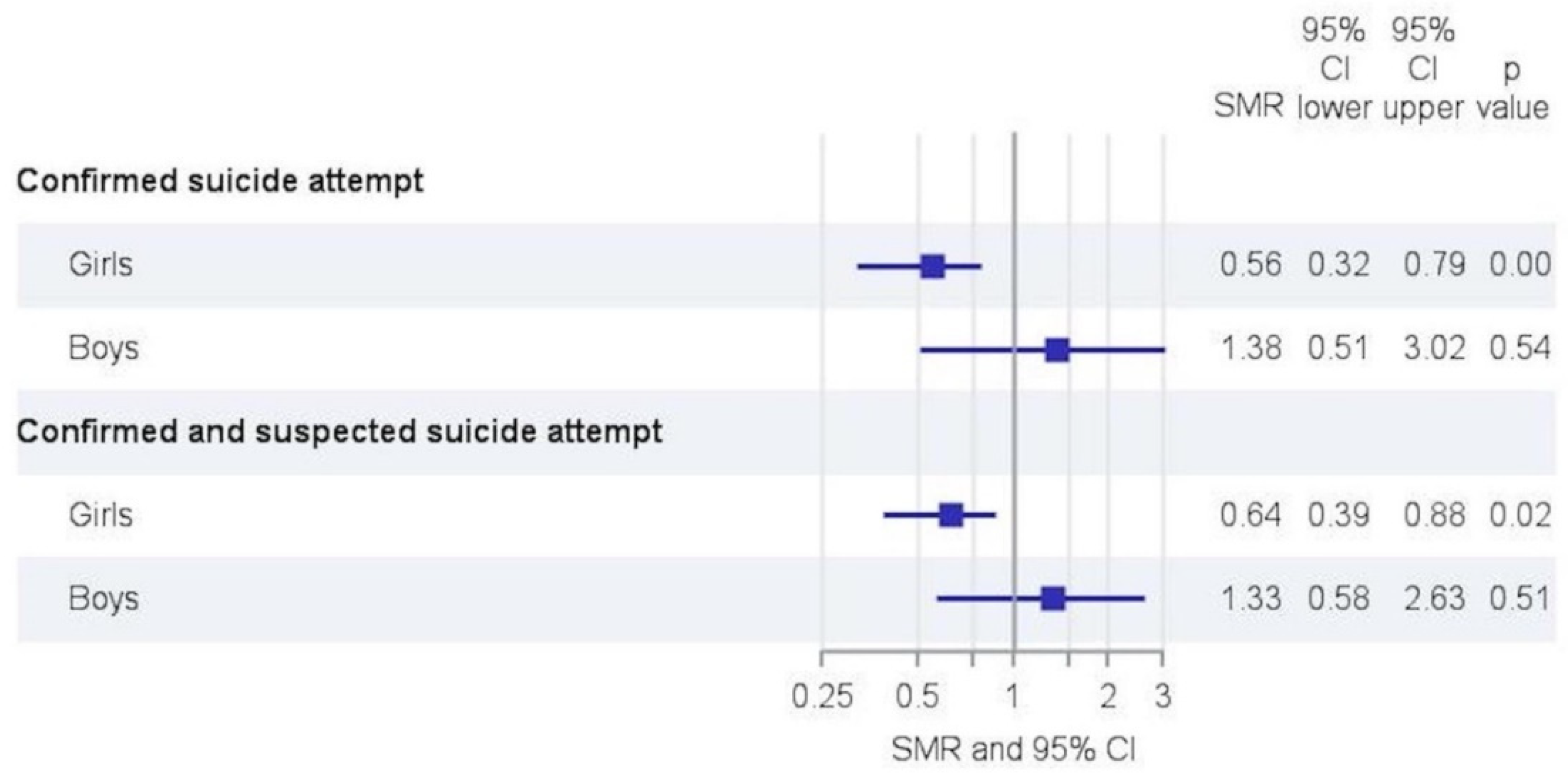
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AL van Tilburg, M.; Edlynn, E.; Maddaloni, M.; van Kempen, K.; Díaz-González de Ferris, M.; Thomas, J. High Levels of Stress Due to the SARS-CoV Pandemic among Parents of Children with and without Chronic Conditions across the USA. Children 2020, 7, 193. [Google Scholar]
- Charlesworth, J.E.G.; Bold, R.; Pal, R. Using ICD-10 diagnostic codes to identify ‘missing’ paediatric patients during nationwide COVID lockdown in Oxfordshire, UK. Eur. J. Pediatr. 2021, 180, 3343–3357. [Google Scholar] [PubMed]
- Kruizinga, M.D.; Peeters, D.; van Veen, M.; van Houten, M.; Wieringa, J.; Noordzij, J.G.; Bekhof, J.; Tramper-Stranders, G.; Vet, N.J.; Driessen, G.J.A. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: A multicenter analysis and review of the literature. Eur. J. Pediatr. 2021, 180, 2271–2279. [Google Scholar] [PubMed]
- Hamill, J.K.; Sawyer, M.C. Reduction of childhood trauma during the COVID-19 Level 4 lockdown in New Zealand. ANZ J. Surg. 2020, 90, 1242–1243. [Google Scholar] [CrossRef] [PubMed]
- Van Aert, G.J.J.; van der Laan, L.; Winter, L.J.M.B.; Berende, C.A.S.; de Groot, H.G.W.; van Hensbroek, P.B.; Schormans, P.M.J.; Winkes, M.B.; Vos, D.I. Effect of the COVID Pandemic During the First Lockdown in the Netherlands on the Number of Trauma-Related Admissions, Trauma Severity and Treatment: The Results of a Retrospective Cohort Study in a Level 2 Trauma Centre. BMJ Open 2021, 11, e045015. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Anderson, K.E.; Han, H.; Barry, C.L. Psychological Distress and COVID–Related Stressors Reported in a Longitudinal Cohort of US Adults in April and July 2020. JAMA 2020, 324, 2555. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021, 1–11. [Google Scholar] [CrossRef]
- Liddell, F.D. Simple exact analysis of the standardised mortality ratio. J. Epidemiol. Community Health 1984, 38, 85–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uitenbroek, D.G. Sisa—Simple Interactive Statistical Analysis. Rate Ratio/SMR Exact. Available online: https://www.quantitativeskills.com/sisa/statistics/smr.htm (accessed on 3 July 2021).
- Hu, N.; Nassar, N.; Shrapnel, J.; Perkes, I.; Hodgins, M.; O’Leary, F.; Trudgett, C.; Eapen, V.; Woolfenden, S.; Knight, K.; et al. The impact of the COVID pandemic on paediatric health service use within one year after the first pandemic outbreak in New South Wales Australia—A time series analysis. Lancet Reg. Health West. Pac. 2021, 19, 100311. [Google Scholar]
- Raffaldi, I.; Castagno, E.; Fumi, I.; Bondone, C.; Ricceri, F.; Besenzon, L.; del Prever, A.B.; Capalbo, P.; Cosi, G.; Felici, E.; et al. Pediatric admissions to emergency departments of North-Western Italy during COVID pandemic: A retrospective observational study. Lancet Reg. Health Eur. 2021, 5, 100081. [Google Scholar] [CrossRef]
- Rusconi, F.; Di Fabrizio, V.; Puglia, M.; Sica, M.; De Santis, R.; Masi, S.; Gagliardi, L. Delayed presentation of children to the emergency department during the first wave of COVID-19 pandemic in Italy: Area-based cohort study. Acta Paediatr. 2021, 110, 2796–2801. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.C.; MacRae, C.; Swann, O.V.; Haseeb, H.; Cunningham, S.; Davies, P.; Gibson, N.; Lamb, C.; Levin, R.; McDougall, C.M.; et al. Indirect effects of the COVID pandemic on paediatric healthcare use and severe disease: A retrospective national cohort study. Arch. Dis. Child. 2021, 106, 911–917. [Google Scholar] [PubMed]
- Baxter, I.; Hancock, G.; Clark, M.; Hampton, M.; Fishlock, A.; Widnall, J.; Flowers, M.; Evans, O. Paediatric Orthopaedics in Lockdown: A Study on the Effect of the SARS-CoV Pandemic on Acute Paediatric Orthopaedics and Trauma. Bone Jt. Open 2020, 1, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Darling, J.; Nowicka, M.; Niazi, N.; Pillai, A. The effect of COVID lockdowns on paediatric lower limb orthopaedic presentations. Arch. Orthop. Trauma. Surg. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gilmartin, S.; Barrett, M.; Bennett, M.; Begley, C.; Ni Chroinin, C.; O’Toole, P.; Blackburn, C. The effect of national public health measures on the characteristics of trauma presentations to a busy paediatric emergency service in Ireland: A longitudinal observational study. Ir. J. Med. Sci. 2021, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Keays, G.; Freeman, D.; Gagnon, I. Injuries in the time of COVID. Health Promot. Chronic Dis. Prev. Can. 2020, 40, 336–341. [Google Scholar] [CrossRef]
- Sugand, K.; Park, C.; Morgan, C.; Dyke, R.; Aframian, A.; Hulme, A.; Evans, S.; Sarraf, K.M.; Baker, C.; Bennett-Brown, K.; et al. Impact of the COVID pandemic on paediatric orthopaedic trauma workload in central London: A multi-centre longitudinal observational study over the “golden weeks. ” Acta Orthop. 2020, 91, 633–638. [Google Scholar] [CrossRef]
- Grassner, L.; Petr, O.; Warner, F.M.; Dedeciusova, M.; Mathis, A.M.; Pinggera, D.; Gsellmann, S.; Meiners, L.C.; Freigang, S.; Mokry, M.; et al. Trends and Outcomes for Non-Elective Neurosurgical Procedures in Central Europe During the COVID Pandemic. Sci. Rep. 2021, 11, 6171. [Google Scholar]
- Garstang, J.; Debelle, G.; Anand, I.; Armstrong, J.; Botcher, E.; Chaplin, H.; Hallett, N.; Morgans, C.; Price, M.; Tan, E.E.H.; et al. Effect of COVID lockdown on child protection medical assessments: A retrospective observational study in Birmingham, UK. BMJ Open 2020, 10, e042867. [Google Scholar] [CrossRef]
- Heimann, T.; Ewert, J.; Metzner, F.; Sigmund, F.; Jud, A.; Pawils, S. Medical Child Protection During the Coronavirus Lockdown. Monatsschr Kinderheilkd 2021, 169, 346–352. [Google Scholar] [CrossRef]
- Loiseau, M.; Cottenet, J.; Bechraoui-Quantin, S.; Gilard-Pioc, S.; Mikaeloff, Y.; Jollant, F.; François-Purssell, I.; Jud, A.; Quantin, C. Physical Abuse of Young Children During the COVID Pandemic: Alarming Increase in the Relative Frequency of Hospitalizations during the Lockdown Period. Child Abuse Negl. 2021, 122, 105299. [Google Scholar] [CrossRef] [PubMed]
- Ebert, C.; Steinert, J.I. Prevalence and risk factors of violence against women and children during COVID, Germany. Bull. World Health Organ. 2021, 99, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Davico, C.; Marcotulli, D.; Lux, C.; Calderoni, D.; Cammisa, L.; Bondone, C.; Rosa-Brusin, M.; Secci, I.; Porro, M.; Campanile, R.; et al. Impact of the COVID Pandemic on Child and Adolescent Psychiatric Emergencies. J. Clin. Psychiatry 2021, 82, 31960. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Kohls, E.; Moessner, M.; Lustig, S.; Bauer, S.; Becker, K.; Thomasius, R.; Eschenbeck, H.; Diestelkamp, S.; Gillé, V.; et al. The Impact of COVID Related Lockdown Measures on Self-Reported Psychopathology and Health-Related Quality of Life in German Adolescents. Eur. Child Adolesc. Psychiatry 2021, 1–10. [Google Scholar] [CrossRef]
- Ougrin, D. Debate: Emergency mental health presentations of young people during the COVID-19 lockdown. Child Adolesc. Ment. Health 2020, 25, 171–172. [Google Scholar] [CrossRef]
- Härtel, C.; Paul, P.; Hanke, K.; Humberg, A.; Kribs, A.; Mehler, K.; Vochem, M.; Wieg, C.; Roll, C.; Herting, E.; et al. Less invasive surfactant administration and complications of preterm birth. Sci. Rep. 2018, 8, 8333. [Google Scholar] [CrossRef]
- Humberg, A.; Dzietko, M.; Schulz, S.; Felderhoff-Müser, U.; Hüning, B.; Stein, A.; Fortmann, M.I.; Marissen, J.; Rausch, T.K.; Herting, E.; et al. Association of ApoE Genotypes and Recovery From Intracerebral Hemorrhage in Very Low Birth Weight Infants. Stroke 2022, 53, 514–522. [Google Scholar] [CrossRef]
- Kanthimathinathan, H.K.; Buckley, H.; Davis, P.J.; Feltbower, R.G.; Lamming, C.; Norman, L.; Palmer, L.; Peters, M.J.; Plunkett, A.; Ramnarayan, P.; et al. In the eye of the storm: Impact of COVID pandemic on admission patterns to paediatric intensive care units in the UK and Eire. Crit. Care 2021, 25, 399. [Google Scholar] [CrossRef]

| Overall n (%) | Reference Period (2017–2019) n (%) | 2020 n (%) | |
|---|---|---|---|
| Admissions (n) | 1444 | 1098 | 346 |
| Admissions < 1 year of age [n (%)] | 121 (8.4%) | 91 (8.3%) | 30 (8.7%) |
| Age [median (IQR) mean (95% CI)] | 6.5 (2–13) 7.5 (7.2–7.8) | 7 (2–14) 7.6 (7.3–8.0) | 6 (2–12) 7.3 (6.7–7.8) |
| Male [n (%)] | 787 (54.5%) | 588 (53.6%) | 199 (57.5%) |
| Female [n (%)] | 654 (45.3%) | 507 (46.2%) | 147 (42.5%) |
| Diverse [n (%)] | 3 (0.2%) | 3 (0.3%) | 0 (0%) |
| Length of stay on intensive care unit (days) [median (IQR) mean (95% CI)] | 2 (1–3) 3.4 (3.0–3.8) | 2 (1–3) 3.5 (3.1–3.9) | 2 (1–3) 3.2 (2.3–4.0) |
| Mechanical ventilation [n (%)] | 259 (17.9%) | 198 (18.0%) | 61 (17.6%) |
| Duration of mechanical ventilation (days) [median (IQR) mean (95% CI)] | 1 (1–3) 3.3 (2.5–4.1) | 1 (1–3) 3.7 (2.6–4.7) | 1 (1–2) 2.2 (1.5–2.8) |
| Vasopressors [n (%)] | 101 (7.0%) | 78 (7.1%) | 23 (6.7%) |
| Resuscitation [n (%)] | 48 (3.3%) | 38 (3.5%) | 10 (2.9%) |
| Anticonvulsives [n (%)] | 54 (3.7%) | 44 (4.0%) | 10 (2.9%) |
| Died [n (%)] | 13 (0.9%) | 9 (0.8%) | 4 (1.2%) |
| Time to death (days) [median (IQR) mean (95% CI)] | 3 (1–3) 4.1 (3.0–3.8) | 3 (1–3) 3.6 (1.1–6.0) | 2.5 (1.5–9) 5.3 (0–15.7) |
| Poor outcome (GOS 1 or 2) [n (%)] | 15 (1.0%) | 11 (1.0%) | 4 (1.2%) |
| Overall n (%) | Reference Period (2017–2019) n (%) | 2020 n (%) | |
|---|---|---|---|
| Type of accident | |||
| Aspiration [n (%)] | 68 (4.7%) | 55 (5.0%) | 13 (3.8%) |
| Burn/scalding [n (%)] | 200 (13.9%) | 159 (14.5%) | 41 (11.9%) |
| Drowning/suffocation [n (%)] | 16 (1.1%) | 11 (1.0%) | 5 (1.5%) |
| Ingestion [n (%)] | 69 (4.8%) | 48 (4.4%) | 21 (6.1%) |
| Intoxication [n (%)] | 272 (18.8%) | 220 (20.0%) | 52 (15%) |
| Inhalation of toxic gas [n (%)] | 4 (0.3%) | 3 (0.3%) | 1 (0.3%) |
| Electrical injury [n (%)] | 10 (0.7%) | 9 (0.8%) | 1 (0.3%) |
| Trauma [n (%)] | 802 (55.5%) | 590 (53.7%) | 212 (61.3%) |
| Traffic [n (%)] | 235 (29.3%) | 187 (31.7%) | 48 (22.6%) |
| Household [n (%)] | 260 (32.4%) | 180 (30.5%) | 80 (37.7%) |
| Window fall [n (% of household accidents)] | 64 (25.6%) | 45 (25.6%) | 19 (25.7%) |
| Leisure/sports [n (%)] | 258 (32.1%) | 178 (30.2%) | 80 (37.7%) |
| School/kindergarten/work [n (%)] | 38 (4.7%) | 35 (5.9%) | 3 (1.4%) |
| Unknown trauma [n (%)] | 11 (1.4%) | 10 (1.7%) | 1 (0.5%) |
| Unknown accident [n (%)] | 4 (0.3%) | 3 (0.3%) | 0 (0.0%) |
| Non-accidental injury [n (%)] | |||
| Confirmed [n (%)] | 223 (15.4%) | 182 (16.6%) | 41 (11.8%) |
| Confirmed and suspected [n (%)] | 282 (19.5%) | 226 (20.6%) | 56 (16.2%) |
| Non-accidental non-suicidal | 87 (6.0%) | 70 (6.4%) | 17 (4.9%) |
| Suicide attempt | |||
| Confirmed [n (%)] | 158 (10.9%) | 129 (11.8%) | 29 (8.4%) |
| Confirmed and suspected [n (%)] | 184 (12.7%) | 145 (13.2%) | 39 (11.3%) |
| Overall n (%) | Reference Period (2017–2019) n (%) | 2020 n (%) | |
|---|---|---|---|
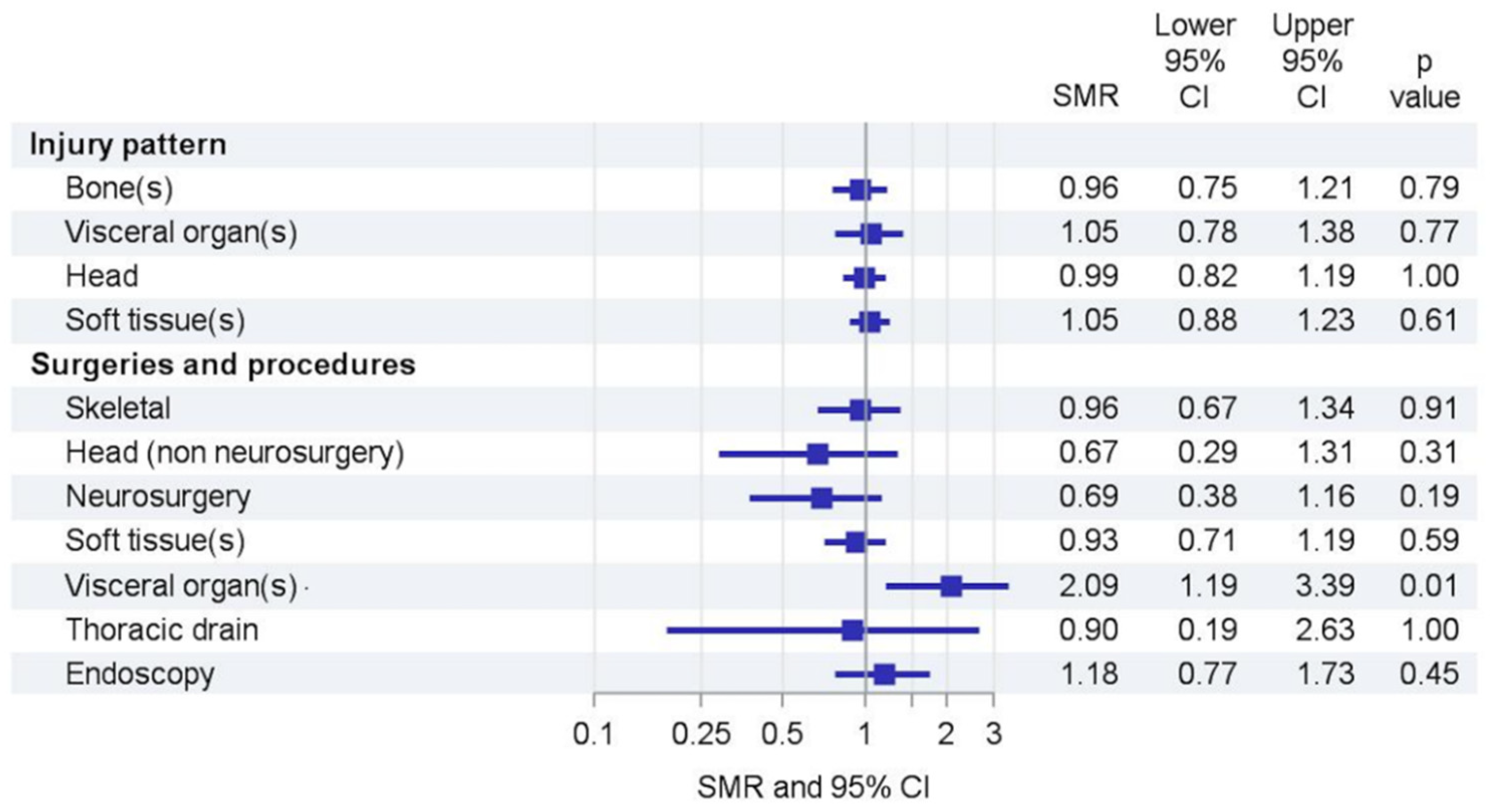
| Injury pattern | |||
| Skeletal injury [n (%)] | 305 (21.1%) | 231 (21.0%) | 74 (24.3%) |
| Head injury [n (%)] | 483 (33.4%) | 363 (33.0%) | 120 (34.7%) |
| Visceral organ injury [n (%)] | 193 (13.4%) | 143 (13.0%) | 50 (14.5%) |
| Soft tissue injury [n (%)] | 559 (38.7%) | 415 (37.8%) | 144 (41.6%) |
| Surgeries and procedures | |||
| Skeletal surgery [n (%)] | 140 (9.7%) | 106 (9.7%) | 34 (9.8%) |
| Head surgery (non-neurosurgery) [n (%)] | 44 (3.1%) | 36 (3.3%) | 8 (2.3%) |
| Neurosurgery [n (%)] | 108 (7.5%) | 88 (8.0%) | 20 (5.8%) |
| Soft tissue procedures/surgery [n (%)] | 265 (18.4) | 203 (18.5%) | 62 (17.9%) |
| Visceral organ surgery [n (%)] | 39 (2.7%) | 23 (2.1%) | 16 (4.6%) |
| Thoracic drain placement [n (%)] | |||
| Endoscopy (after aspiration/ingestion (n = 137)) [n (%)] | 92 (67.2%) | 66 (64.1%) | 26 (76.5%) |
| Any procedure/surgery [n (%)] | 494 (34.2%) | 373 (34.0%) | 121 (35.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruns, N.; Willemsen, L.Y.; Holtkamp, K.; Kamp, O.; Dudda, M.; Kowall, B.; Stang, A.; Hey, F.; Blankenburg, J.; Sabir, H.; et al. Impact of the First COVID Lockdown on Accident- and Injury-Related Pediatric Intensive Care Admissions in Germany—A Multicenter Study. Children 2022, 9, 363. https://doi.org/10.3390/children9030363
Bruns N, Willemsen LY, Holtkamp K, Kamp O, Dudda M, Kowall B, Stang A, Hey F, Blankenburg J, Sabir H, et al. Impact of the First COVID Lockdown on Accident- and Injury-Related Pediatric Intensive Care Admissions in Germany—A Multicenter Study. Children. 2022; 9(3):363. https://doi.org/10.3390/children9030363
Chicago/Turabian StyleBruns, Nora, Lea Y. Willemsen, Katharina Holtkamp, Oliver Kamp, Marcel Dudda, Bernd Kowall, Andreas Stang, Florian Hey, Judith Blankenburg, Hemmen Sabir, and et al. 2022. "Impact of the First COVID Lockdown on Accident- and Injury-Related Pediatric Intensive Care Admissions in Germany—A Multicenter Study" Children 9, no. 3: 363. https://doi.org/10.3390/children9030363
APA StyleBruns, N., Willemsen, L. Y., Holtkamp, K., Kamp, O., Dudda, M., Kowall, B., Stang, A., Hey, F., Blankenburg, J., Sabir, H., Eifinger, F., Fuchs, H., Haase, R., Andrée, C., Heldmann, M., Potratz, J., Kurz, D., Schumann, A., Müller-Knapp, M., ... Dohna-Schwake, C. (2022). Impact of the First COVID Lockdown on Accident- and Injury-Related Pediatric Intensive Care Admissions in Germany—A Multicenter Study. Children, 9(3), 363. https://doi.org/10.3390/children9030363






