The Impact of Whole-Body Vibration Training on Bone Minerals and Lean Mass in Children and Adolescents with Motor Disabilities: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Study Selection
2.3. Inclusion and Exclusion Criteria
2.4. Quality Assessment
2.5. Risk of Bias Assessment
2.6. Data Analysis
3. Results
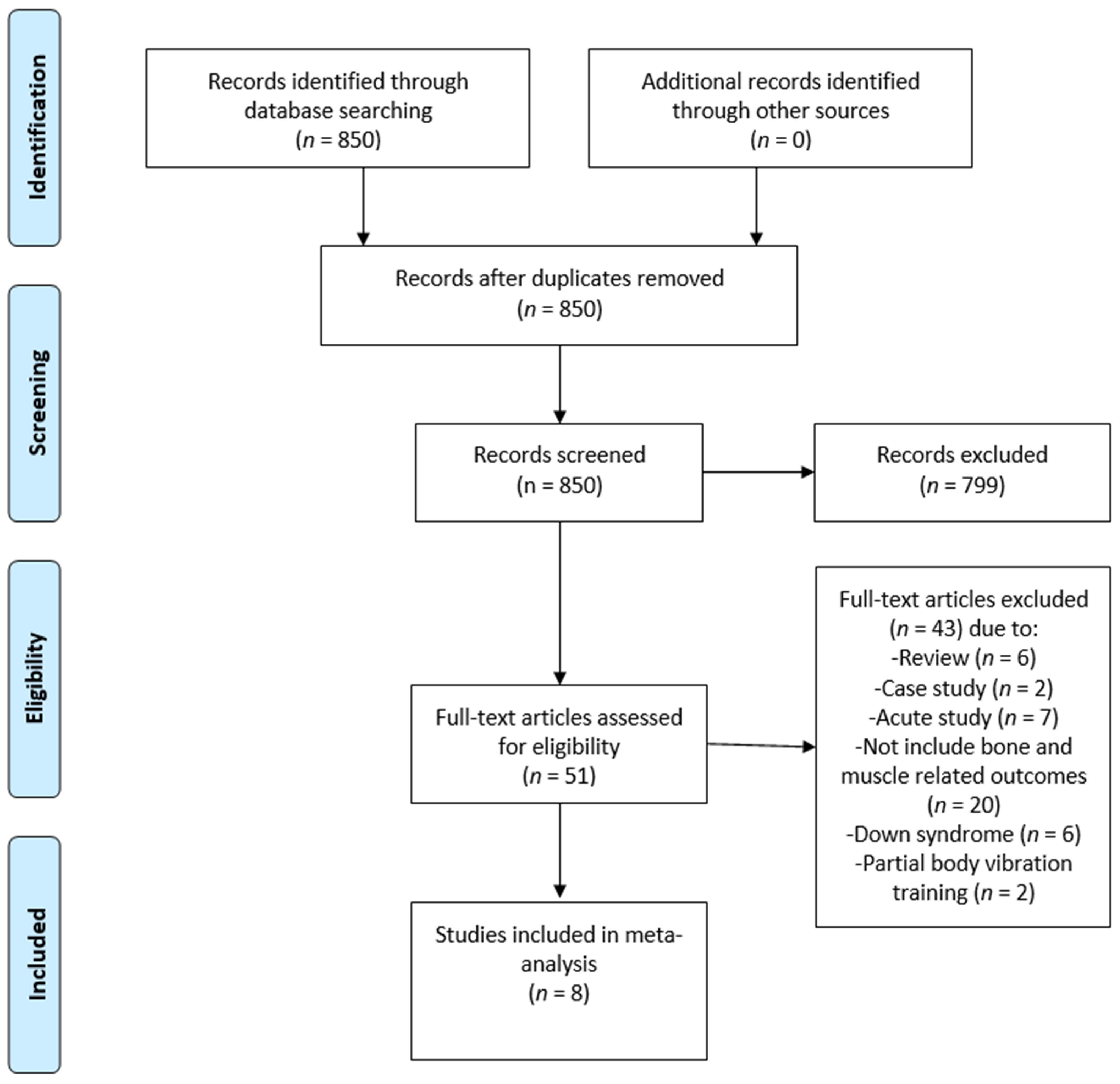
3.1. Eligibility of Studies
3.2. Quality Assessment
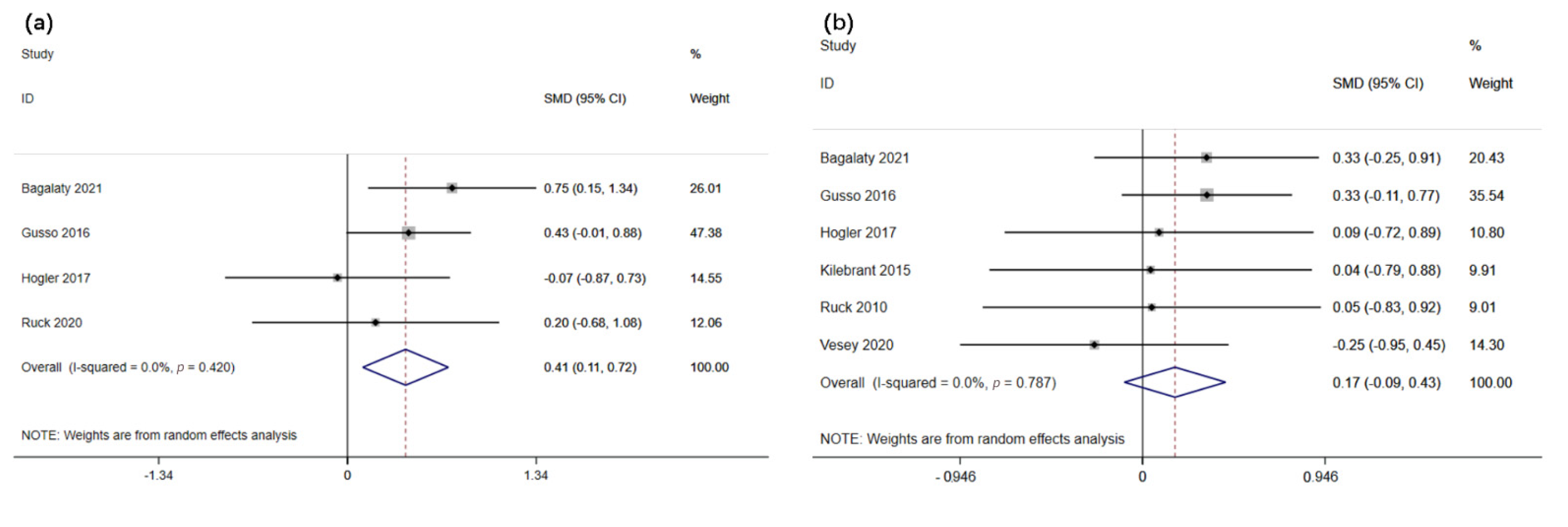
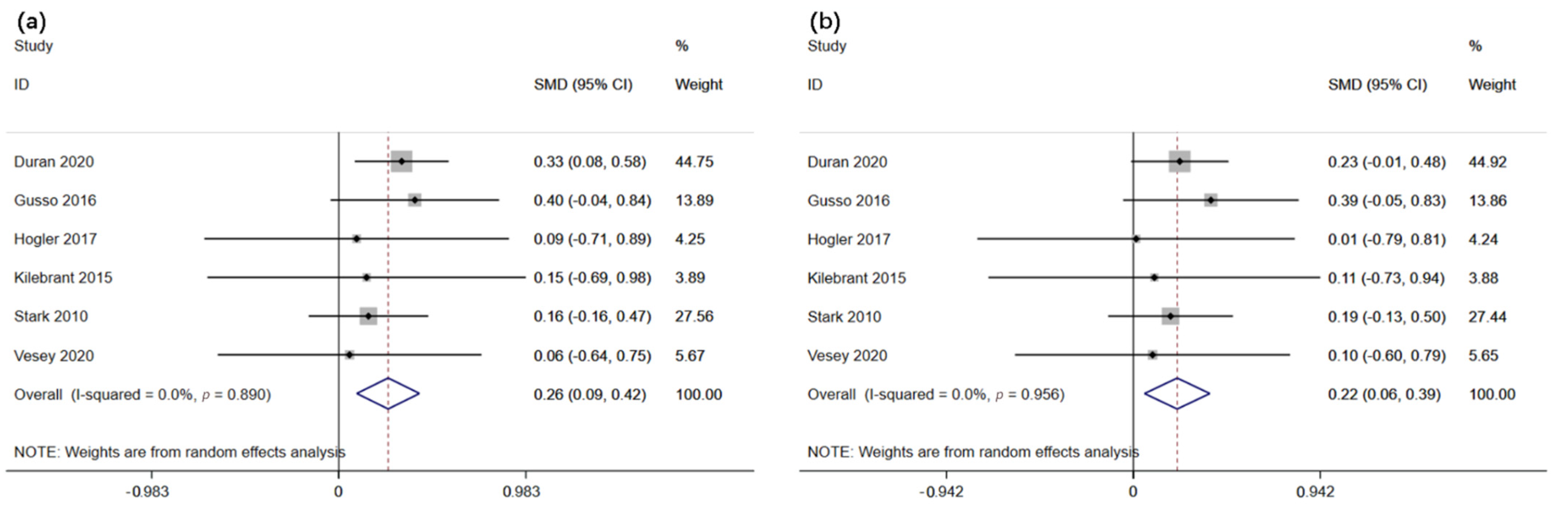
3.3. Quantitative Synthesis
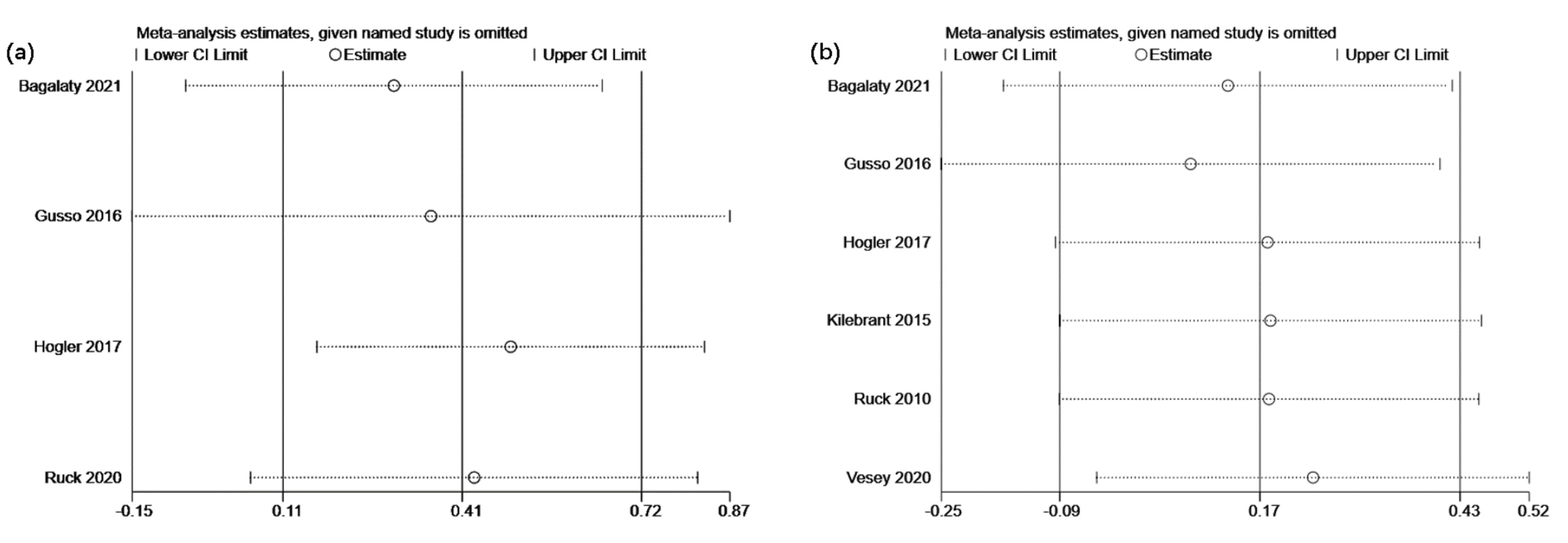
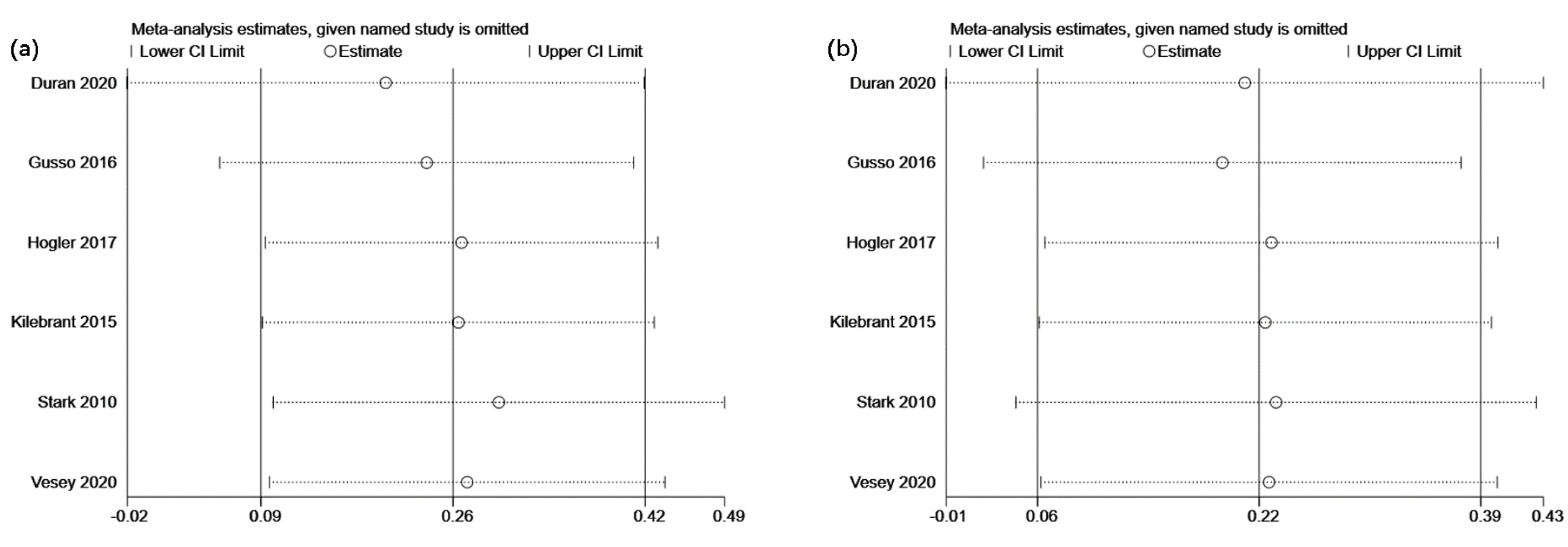
3.4. Sensitivity Analysis
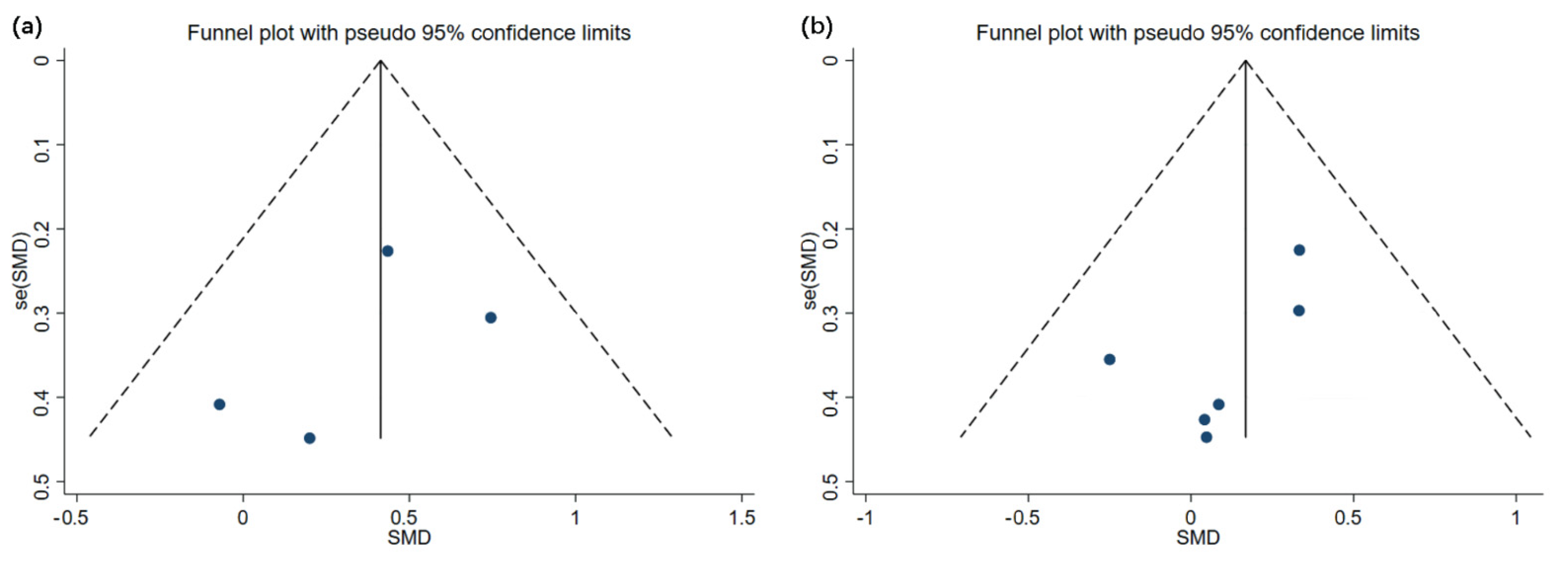
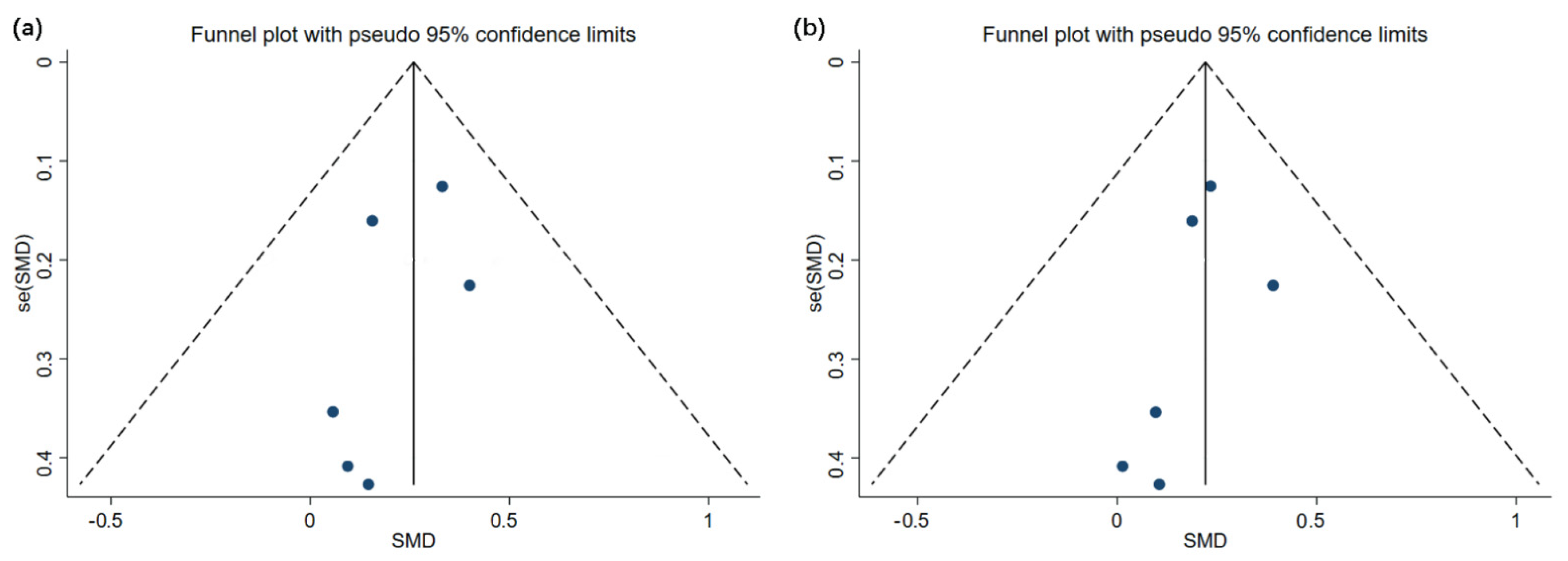
3.5. Analysis of Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search Strategy | Results (Approximately) |
|---|---|---|
| Scopus | #1: Title-Abs-Key (Whole Body Vibration or Whole-Body Vibration) #2: Title-Abs-Key (Children or Adolescents) #3: #1 and #2 Limiters - Published Date: 20060101-20210603 | 4141 2,238,051 272 |
| Pubmed | #1: [Title/Abstract] Whole Body Vibration or Whole-Body Vibration #2: [Title/Abstract] Children or Adolescents #3: #1 and #2 Filters: Publication date from 2006/01/01 to 2021/6/03 | 1727 712,391 222 |
| Web of Science | #1: TOPIC: (Whole Body Vibration or Whole-Body Vibration) #2: TOPIC: (Children or Adolescents) #3: #1 and #2 Refined by: Publication years: (20210603-20060101) Indexes = SCI-EXPANDED, SSCI, CCR-EXPANDED | 3795 1,381,743 185 |
| EBSCO | #1: Abstract: (Whole Body Vibration or Whole-Body Vibration) #2: Abstract: (Children or Adolescents) #3: #1 and #2 Year: 20060101-20210603 | 3654 3,226,740 171 |
References
- Veilleux, L.-N.; Lemay, M.; Pouliot-Laforte, A.; Cheung, M.S.; Glorieux, F.H.; Rauch, F. Muscle Anatomy and Dynamic Muscle Function in Osteogenesis Imperfecta Type I. J. Clin. Endocrinol. Metab. 2014, 99, E356–E362. [Google Scholar] [CrossRef] [PubMed]
- Modlesky, C.M.; Zhang, C. Complicated Muscle-Bone Interactions in Children with Cerebral Palsy. Curr. Osteoporos. Rep. 2020, 18, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Ritzmann, R.; Stark, C.; Krause, A. Vibration therapy in patients with cerebral palsy: A systematic review. Neuropsychiatr. Dis. Treat. 2018, 14, 1607–1625. [Google Scholar] [CrossRef] [PubMed]
- Matute-Llorente, Ángel; González-Agüero, A.; Gómez-Cabello, A.; Vicente-Rodríguez, G.; Mallén, J.A.C. Effect of Whole-Body Vibration Therapy on Health-Related Physical Fitness in Children and Adolescents with Disabilities: A Systematic Review. J. Adolesc. Heal. 2014, 54, 385–396. [Google Scholar] [CrossRef]
- Saquetto, M.; Carvalho, V.; Silva, C.; Conceição, C.; Gomes-Neto, M. The effects of whole body vibration on mobility and balance in children with cerebral palsy: A systematic review with meta-analysis. JMNI 2015, 15, 137–144. [Google Scholar]
- Saquetto, M.B.; Pereira, F.F.; Queiroz, R.S.; Da Silva, C.M.; Conceição, C.S.; Neto, M.G. Effects of whole-body vibration on muscle strength, bone mineral content and density, and balance and body composition of children and adolescents with Down syndrome: A systematic review. Osteoporos. Int. 2018, 29, 527–533. [Google Scholar] [CrossRef]
- Rauch, F.; Sievanen, H.; Boonen, S.; Cardinale, M.; Degens, H.; Felsenberg, D.; Roth, J.; Schoenau, E.; Verschueren, S.; Rittweger, J. Reporting whole-body vibration intervention studies: Recommendations of the International Society of Musculoskeletal and Neuronal Interactions. JMNI 2010, 10, 193–198. [Google Scholar]
- Cardinale, M.; Bosco, C. The Use of Vibration as an Exercise Intervention. Exerc. Sport Sci. Rev. 2003, 31, 3–7. [Google Scholar] [CrossRef]
- Beck, B.R. Vibration Therapy to Prevent Bone Loss and Falls: Mechanisms and Efficacy. Curr. Osteoporos. Rep. 2015, 13, 381–389. [Google Scholar] [CrossRef]
- Chen, H.; Ma, J.; Lu, B.; Ma, X.-L. The effect of whole-body vibration training on lean mass. Medicine 2017, 96, e8390. [Google Scholar] [CrossRef]
- Duran, I.; Martakis, K.; Stark, C.; Schafmeyer, L.; Rehberg, M.; Schoenau, E. Effect of an interval rehabilitation program with home-based, vibration-assisted training on the development of muscle and bone in children with cerebral palsy—An observational study. J. Pediatr. Endocrinol. Metab. 2020, 33, 1083–1092. [Google Scholar] [CrossRef]
- El-Bagalaty, A.E.; Ismaeel, M.M. Suit therapy versus whole-body vibration on bone mineral density in children with spastic diplegia. JMNI 2021, 21, 79–84. [Google Scholar]
- Ruck, J.; Chabot, G.; Rauch, F. Vibration treatment in cerebral palsy: A randomized controlled pilot study. JMNI 2010, 10, 77–83. [Google Scholar]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Suárez-Iglesias, D.; Miller, K.J.; Seijo-Martínez, M.; Ayán, C. Benefits of Pilates in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Medicina 2019, 55, 476. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-L.; Wang, X.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The Levels of Evidence and Their Role in Evidence-Based Medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef]
- Hoegler, W.; Scott, J.; Bishop, N.; Arundel, P.; Nightingale, P.; Mughal, M.Z.; Padidela, R.; Shaw, N.; Crabtree, N. The Effect of Whole Body Vibration Training on Bone and Muscle Function in Children With Osteogenesis Imperfecta. J. Clin. Endocrinol. Metab. 2017, 102, 2734–2743. [Google Scholar] [CrossRef]
- Gusso, S.; Munns, C.F.; Colle, P.; Derraik, J.G.B.; Biggs, J.B.; Cutfield, W.S.; Hofman, P.L. Effects of whole-body vibration training on physical function, bone and muscle mass in adolescents and young adults with cerebral palsy. Sci. Rep. 2016, 6, 22518. [Google Scholar] [CrossRef] [PubMed]
- Vesey, R.M.; Hofman, P.L.; Derraik, J.G.; Colle, P.; Biggs, J.B.; Munns, C.F.; Cutfield, W.S.; Gusso, S. Safety, feasibility and efficacy of side-alternating vibration therapy on bone and muscle health in children and adolescents with musculoskeletal disorders: A pilot trial. J. Paediatr. Child Heal. 2020, 56, 1257–1262. [Google Scholar] [CrossRef]
- Kilebrant, S.; Braathen, G.; Emilsson, R.; Glansén, U.; Söderpalm, A.; Zetterlund, B.; Westerberg, B.; Magnusson, P.; Swolin-Eide, D. Whole-body vibration therapy in children with severe motor disabilities. J. Rehabil. Med. 2015, 47, 223–228. [Google Scholar] [CrossRef]
- Stark, C.; Nikopoulou-Smyrni, P.; Stabrey, A.; Semler, O.; Schoenau, E. Effect of a new physiotherapy concept on bone mineral density, muscle force and gross motor function in children with bilateral cerebral palsy. J. Musculoskelet. Neuronal. Interact. 2010, 10, 151–158. [Google Scholar]
- Lu, Y.; Wang, W.; Ding, X.; Shi, X. Association between the promoter region of serotonin transporter polymorphisms and recurrent aphthous stomatitis: A meta-analysis. Arch. Oral Biol. 2020, 109, 104555. [Google Scholar] [CrossRef]
- Leite, H.R.; Camargos, A.C.R.; Mendonça, V.A.; Lacerda, A.C.R.; Soares, B.A.; Oliveira, V.C. Current evidence does not support whole body vibration in clinical practice in children and adolescents with disabilities: A systematic review of randomized controlled trial. Brazilian J. Phys. Ther. 2019, 23, 196–211. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.A.; Williams, M.T.; Olds, T.; Lane, A.E. Physical and sedentary activity in adolescents with cerebral palsy. Dev. Med. Child Neurol. 2007, 49, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Eid, M.A. Effect of Whole-Body Vibration Training on Standing Balance and Muscle Strength in Children with Down Syndrome. Am. J. Phys. Med. Rehabil. 2015, 94, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.M.; Eid, M.A.; Moawd, S.A. Effect of whole-body vibration on muscle strength, spasticity, and motor performance in spastic diplegic cerebral palsy children. Egypt J. Med. Hum. Genet. 2014, 15, 173–179. [Google Scholar] [CrossRef]
- Lee, B.-K.; Chon, S.-C. Effect of whole body vibration training on mobility in children with cerebral palsy: A randomized controlled experimenter-blinded study. Clin Rehabil. 2013, 27, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Reyes, M.L.; Hernández, M.; Holmgren, L.J.; Sanhueza, E.; Escobar, R.G. High-frequency, low-intensity vibrations increase bone mass and muscle strength in upper limbs, improving autonomy in disabled children. J. Bone Miner. Res. 2011, 26, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Moreau, N.G.; Bodkin, A.W.; Bjornson, K.; Hobbs, A.; Soileau, M.; Lahasky, K. Effectiveness of Rehabilitation Interventions to Improve Gait Speed in Children with Cerebral Palsy: Systematic Review and Meta-analysis. Phys. Ther. 2016, 96, 1938–1954. [Google Scholar] [CrossRef] [PubMed]
- Duquette, S.A.; Guiliano, A.M.; Starmer, D.J. Whole body vibration and cerebral palsy: A systematic review. J. Can. Chiropr Assoc. 2015, 59, 245–252. [Google Scholar]
- Saquetto, M.; Carvalho, V.; Silva, C.; Conceio, C.; Gomes-Neto, M. Systematic review of whole body vibration exercises in the treatment of cerebral palsy: Brief report. Dev. Neurorehabil. 2015, 3, 1–7. [Google Scholar] [CrossRef]
- Baptista, F.; Barrigas, C.; Vieira, F.; Santa-Clara, H.; Homens, P.M.; Fragoso, I. The role of lean body mass and physical activity in bone health in children. J. Bone Miner. Metab. 2012, 30, 100–108. [Google Scholar] [CrossRef]
- Kruse, A.; Schranz, C.; Svehlik, M.; Tilp, M. The Effect of Functional Home-Based Strength Training Programs on the Mechano-Morphological Properties of the Plantar Flexor Muscle-Tendon Unit in Children with Spastic Cerebral Palsy. Pediatr. Exerc. Sci. 2019, 31, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Ritzmann, R.; Kramer, A.; Gruber, M.; Gollhofer, A.; Taube, W. EMG activity during whole body vibration: Motion artifacts or stretch reflexes? Eur J. Appl Physiol. 2010, 110, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Lebedev, M.A.; Polyakov, A.V. Analysis of surface EMG of human soleus muscle subjected to vibration. J. Electromyogr. Kinesiol. 1992, 2, 26–35. [Google Scholar] [CrossRef]
- Martínez de Zabarte Fernández, J.M.; Ros Arnal, I.; Peña Segura, J.L.; García Romero, R.; Rodríguez Martínez, G. Bone health impairment in patients with cerebral palsy. Arch. Osteoporos. 2020, 15, 91. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Whitney, D.G.; Knight, C.A.; Miller, F.; Modlesky, C.M. Site-Specific Transmission of a Floor-Based, High-Frequency, Low-Magnitude Vibration Stimulus in Children with Spastic Cerebral Palsy. Arch. Phys. Med. Rehabil. 2016, 97, 218–223. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Study | Type | Age (y) | Gender | Disease | Duration | WBVT Program | Index | DXA Device |
|---|---|---|---|---|---|---|---|---|
| Bagalaty 2021 | RCT | 5.0 ± 0.84 | 10 M/13 F | CP | 12 weeks;3 x/week | 5–25 Hz; OA = 0–3.9 mm; Erect position, squatting, and side-standing for 20 min; Side-alternating vibrations. | Lumbar-spine BMD; Femur BMD | DP3, Lunar Corporation, USA |
| Duran 2020 | Cohort | 11.9 ± 2.7 | 76 M/52 F | CP | 6 months; 3–10 x/week | 8–20 Hz; OA = 1–2 mm; Standing on a 40 degrees inclined pedal and train for 15 minutes; Side-alternating vibrations. | Total-body BMC; Lean mass | GE, UK |
| Gusso 2016 | Cohort | 16.2 | 23 M/17 F | CP | 20 weeks; 4 x/week | 15–20 Hz; OA = 1 mm; Stand on a vibration pedal with knees bent and train for 9 min; Side-alternating vibrations. | Lumbar-spine BMD; Femur BMD; Total-body BMC; Lean mass | GE Lunar Prodigy, USA |
| Hogler 2017 | RCT | 10.5 ± 2.9 | 6 M/6 F | OI | 5 months; 2 x/day | 20–25 Hz; OA = 2–6 mm; Stand on a 10–45 degrees inclined vibration pedal with knees bent and train for 18 min; Side-alternating vibrations. | Lumbar-spine BMD; Femur BMD; Total-body BMC; Lean mass | GE Lunar Prodigy, USA |
| Kilebrant 2015 | Cohort | 5.1–16.3 | 4 M/7 F | MD | 6 months; 2 x/week | 40–42 Hz; OA = 0.2 mm; Stand on a vibration pedal with knees bent and train for 5–15 min; Vertical vibrations. | Lumbar-spine BMD; Total-body BMC; Lean mass | GE Lunar Prodigy, USA |
| Ruck 2010 | RCT | 8.2 ± 0.9 | 8 M/2 F | CP | 6 months; 5 x/week | 12–18 Hz; OA = 4 mm; Stand on a 35 degrees inclined vibration pedal and train for 15 min; Side-alternating vibrations. | Lumbar-spine BMD; Femur BMD | QDR Discovery, Hologic Inc, USA |
| Stark 2010 | Cohort | 9.76 | 44 M/34 F | CP | 6 months; 1 x/day | 5–25 Hz; OA = 0–3.9 mm; Stand on a vibration pedal and train for 15 min; Side-alternating vibrations. | Total-body BMC; Lean mass | GE, Germany |
| Vesey 2020 | Cohort | 15.7 ± 2.9 | 8 M/8 F | MD | 20 weeks; 4 x/week | 12–20 Hz; OA = 1 mm; Stand on a vibration pedal and train for 15 min; Side-alternating vibrations. | Lumbar-spine BMD; Total-body BMC; Lean mass | GE Lunar Prodigy, USA |
| PEDro Scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | LE | LR | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bagalaty 2021 | Y * | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 | 1B | B | |
| Hogler 2017 | Y * | Y | Y | N | N | N | N | Y | Y | Y | Y | 6/10 | 1B | B | |
| Ruck 2010 | Y * | Y | Y | Y | N | N | N | N | Y | Y | Y | 6/10 | 1B | B | |
| NIH scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Total | ||
| Duran 2020 | Y | Y | Y | N | Y | N | N | N | Y | Y | Y | NA * | 7/11 | 2B | C |
| Gusso 2016 | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Y | NA * | 9/11 | 2B | C |
| Kilebrant 2015 | Y | Y | Y | Y | Y | Y | N | N | N | Y | Y | NA * | 8/11 | 2B | C |
| Stark 2010 | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Y | NA * | 9/11 | 2B | B |
| Vesey 2020 | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Y | NA * | 9/11 | 2B | B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, S.; Yu, W.; Li, W.; Wang, J.; Gao, L.; Li, S. The Impact of Whole-Body Vibration Training on Bone Minerals and Lean Mass in Children and Adolescents with Motor Disabilities: A Systematic Review and Meta-Analysis. Children 2022, 9, 266. https://doi.org/10.3390/children9020266
Li S, Yu W, Li W, Wang J, Gao L, Li S. The Impact of Whole-Body Vibration Training on Bone Minerals and Lean Mass in Children and Adolescents with Motor Disabilities: A Systematic Review and Meta-Analysis. Children. 2022; 9(2):266. https://doi.org/10.3390/children9020266
Chicago/Turabian StyleLi, Shuoqi, Wenbing Yu, Wei Li, Juncheng Wang, Lili Gao, and Shiming Li. 2022. "The Impact of Whole-Body Vibration Training on Bone Minerals and Lean Mass in Children and Adolescents with Motor Disabilities: A Systematic Review and Meta-Analysis" Children 9, no. 2: 266. https://doi.org/10.3390/children9020266
APA StyleLi, S., Yu, W., Li, W., Wang, J., Gao, L., & Li, S. (2022). The Impact of Whole-Body Vibration Training on Bone Minerals and Lean Mass in Children and Adolescents with Motor Disabilities: A Systematic Review and Meta-Analysis. Children, 9(2), 266. https://doi.org/10.3390/children9020266







