Early Skin-to-Skin Contact Does Not Affect Cerebral Tissue Oxygenation in Preterm Infants <32 Weeks of Gestation
Abstract
:1. Introduction
2. Materials and Methods
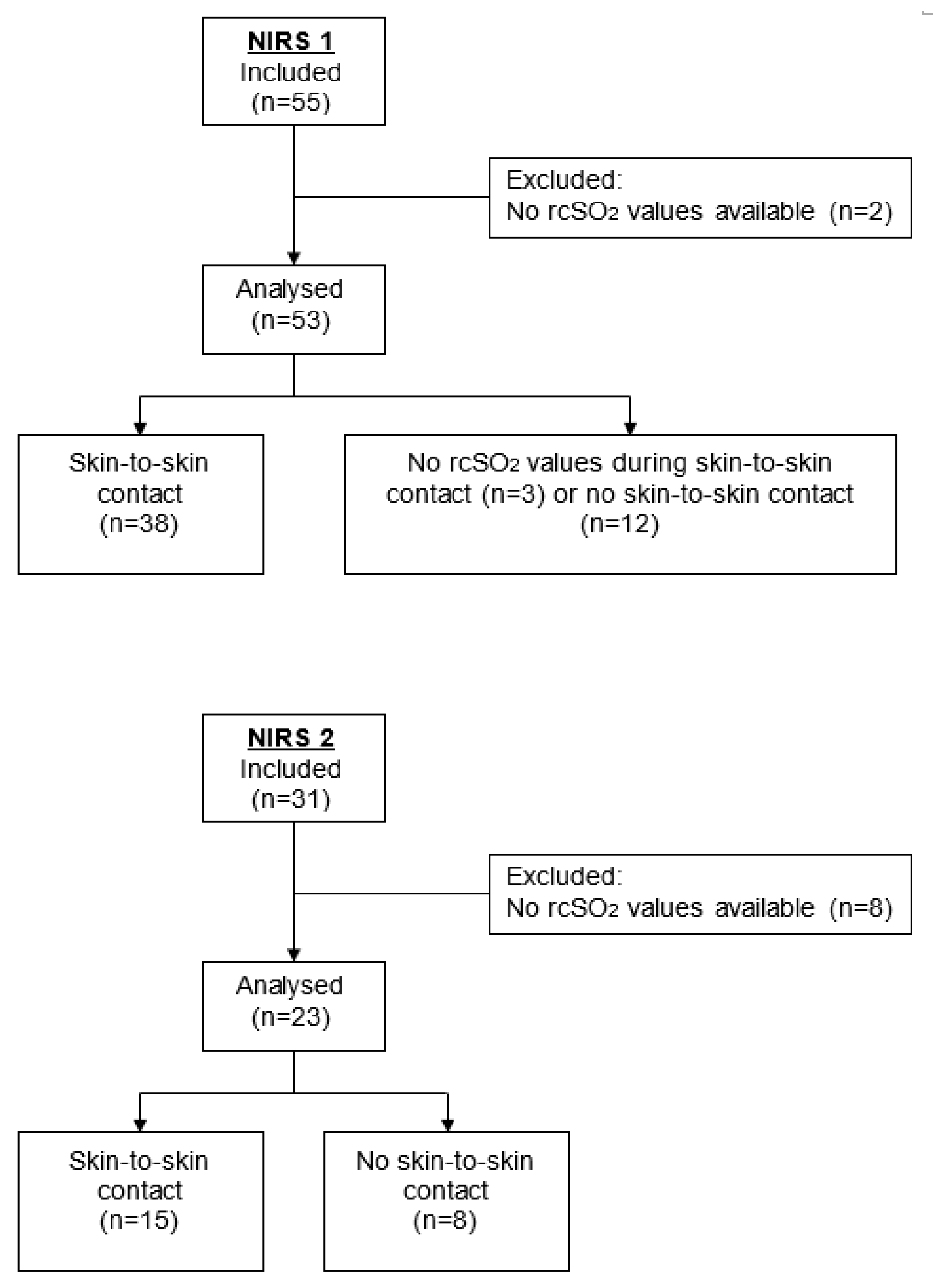
2.1. Study Cohort
2.2. Monitoring Cerebral Oxygenation
2.3. Definitions
2.4. Period Analysis
2.5. Statistical Analysis
2.6. Software
3. Results
3.1. Clinical Characteristics of the Study Group
3.2. Implementation of Skin-to-Skin Contact
3.3. Regional Cerebral Oxygenation Saturation Values Are Not Different between Resting Times and Nursing Care Periods
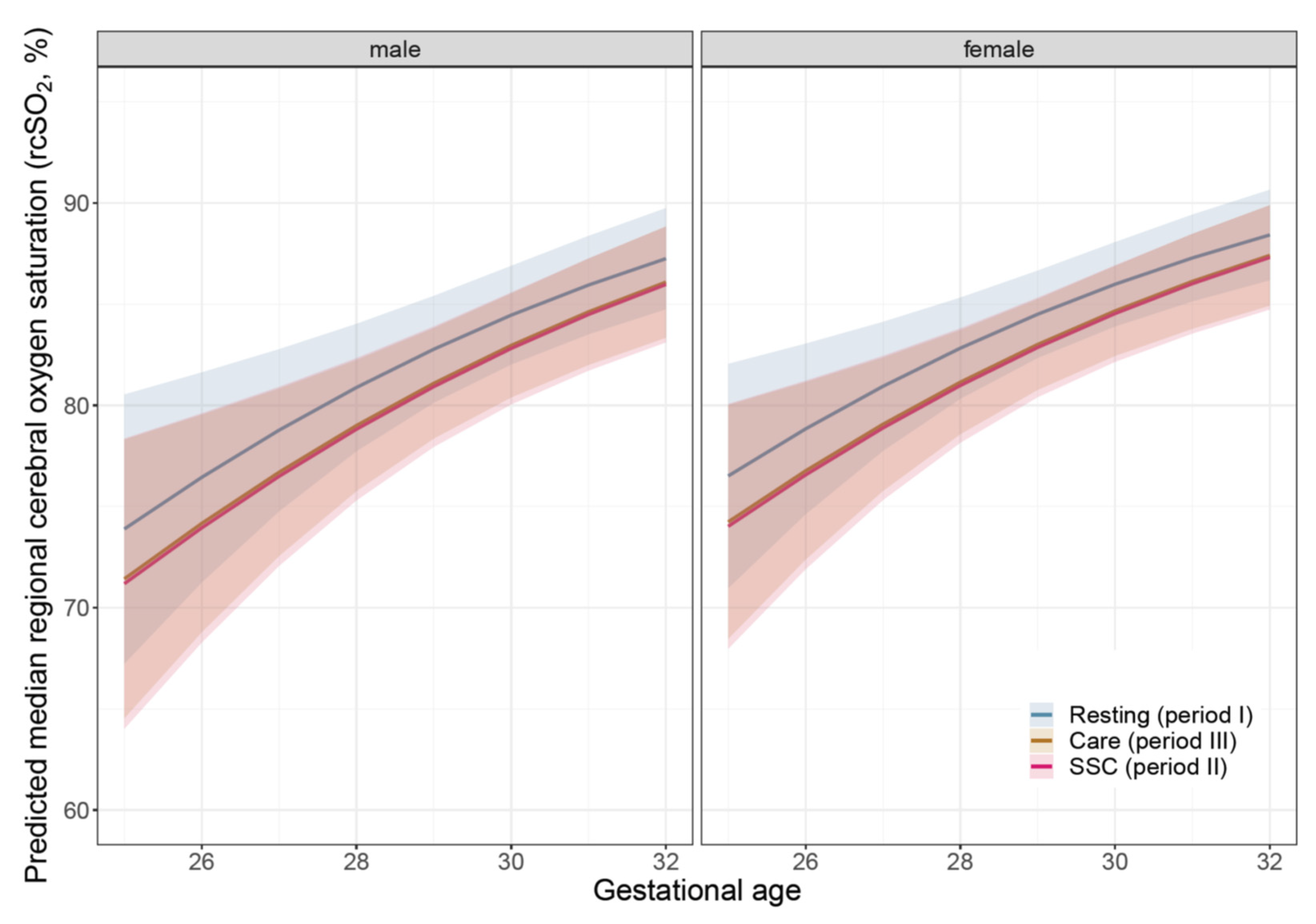
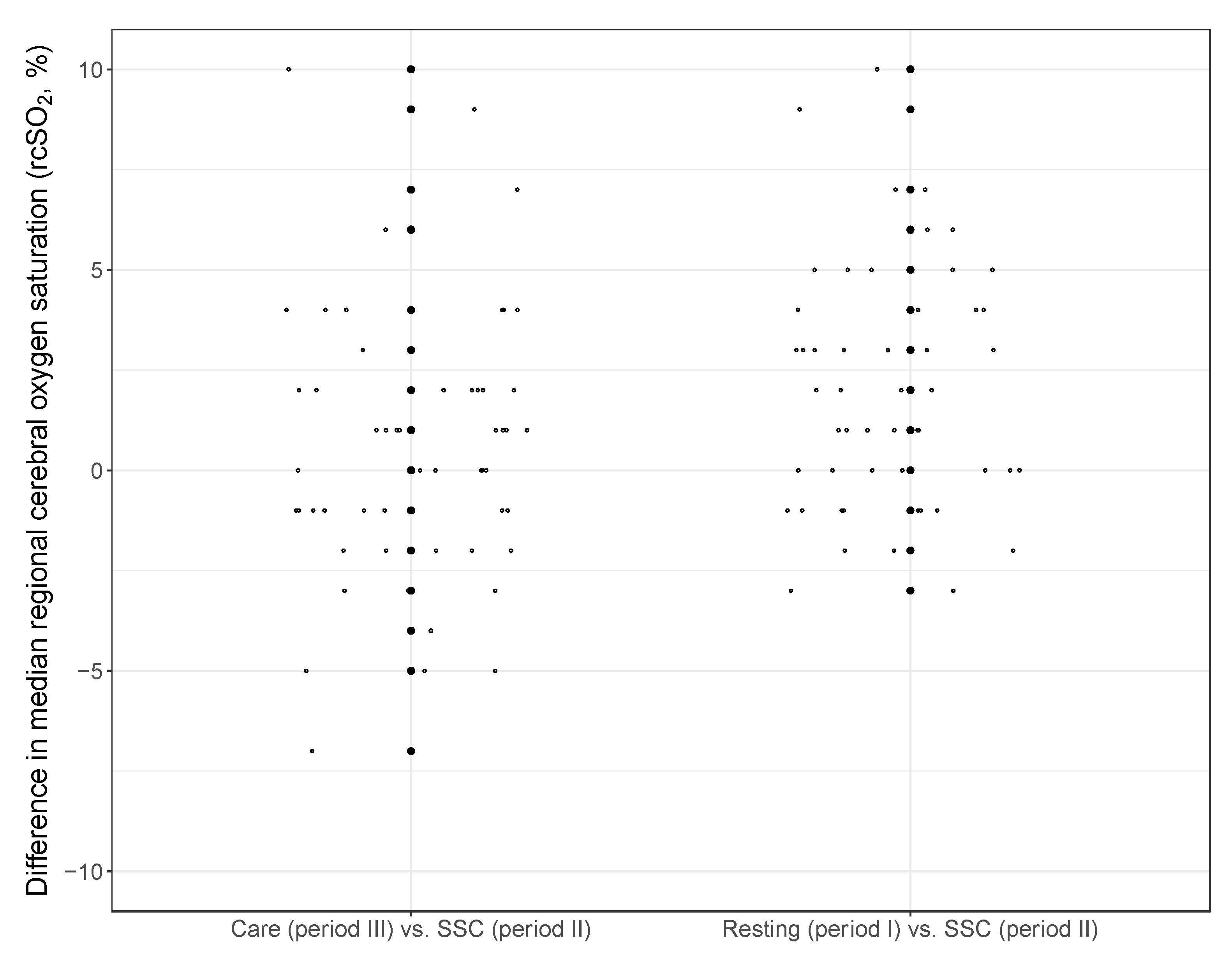
3.4. Regional Cerebral Oxygenation Saturation during Skin-to-Skin Contact
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NIRS | Near-infrared-spectroscopy |
| rcSO2 | regional cerebral tissue oxygenation saturation |
| SSC | Skin-to-skin contact |
References
- Flacking, R.; Lehtonen, L.; Thomson, G.; Axelin, A.; Ahlqvist, S.; Moran, V.H.; Ewald, U.; Dykes, F. Closeness and separation in neonatal intensive care. Acta Paediatr. 2012, 101, 1032–1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, K.J.; Bradshaw, W.T. Sixty golden minutes. Neonatal Netw. 2012, 31, 289–294. [Google Scholar] [CrossRef]
- Moore, E.R.; Bergmann, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2016, 11, CD003519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conde-Agudelo, A.; Díaz-Rossello, J.L. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst. Rev. 2014, 4, CD002771. [Google Scholar] [CrossRef]
- Boundy, E.O.; Dastjerdi, R.; Spiegelmann, D.; Fawzi, W.W.; Missmer, S.A.; Lieberman, E.; Kajeepeta, S.; Wall, S.; Chan, G.J. Kangaroo mother care and neonatal outcomes: A meta-analysis. Pediatrics 2016, 137, e20152238. [Google Scholar] [CrossRef] [Green Version]
- Karlsson, V.; Heinemann, A.B.; Sjörs, G.; Nykvist, K.H.; Agren, J. Early skin-to-skin care in extremely preterm infants: Thermal balance and care environment. J. Pediatr. 2012, 161, 422–426. [Google Scholar] [CrossRef] [Green Version]
- Mörelius, E.; Angelhoff, C.; Erikson, J.; Olhager, E. Time of initiation of skin- to- skin contact in extremely preterm infants in Sweden. Acta Paediatr. 2012, 101, 14–18. [Google Scholar] [CrossRef]
- Maastrup, R.; Greisen, G. Extremely preterm infants tolerate skin-to-skin contact during the first weeks of life. Acta Paediatr. 2010, 99, 1145–1149. [Google Scholar] [CrossRef] [PubMed]
- Linnér, A.; Klemming, S.; Sundberg, B.; Lilliesköld, S.; Westruo, B.; Jonas, W.; Skiöld, B. Immediate skin-to-skin contact is feasible for very preterm infants but thermal control remains a challenge. Acta Paediatr. 2020, 109, 697–704. [Google Scholar] [CrossRef]
- Bohnhorst, B.; Heyne, T.; Peter, C.S.; Poets, C.F. Skin-to-skin (kangaroo) care, respiratory control and thermoregulation. J. Pediatr. 2001, 138, 193–197. [Google Scholar] [CrossRef]
- Bohnhorst, B.; Gill, D.; Dördelmann, M.; Peter, C.S.; Poets, C.F. Bradycardia and desaturationduring skin-to-skin care: No relationship to hyperthermia. J. Pediatr. 2004, 145, 499–502. [Google Scholar] [CrossRef]
- Hyttel-Sorensen, S.; Pellicer, A.; Alderliesten, T.; Austin, T.; van Bel, F.; Benders, M.; Claris, O.; Dempsey, E.; Franz, A.R.; Fumagalli, M.; et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: Phase II randomised clinical trial. BMJ 2015, 350, g7635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tataranno, M.L.; Alderliesten, T.; de Vries, L.S.; Groenendaal, F.; Toer, M.C.; Lemmers, P.M.A.; Vosse van de, R.E.; van Bel, F.; Benders, M.J.N.L. Early oxygen-utilization and brain activity in preterm infants. PLoS ONE 2015, 10, e0124623. [Google Scholar] [CrossRef]
- Pichler, G.; Urlesberger, B.; Baik, N.; Schwaberger, B.; Binder-Heschl, C.; Avian, A.; Pasny, J.; Cheung, P.-Y.; Schmölzer, G.M. Cerebral Oxygen Saturation to Guide Oxygen Delivery in Preterm Neonates for the Immediate Transition after Birth: A 2-Center Randomized Controlled Pilot Feasibility Trial. J. Pediatr. 2016, 170, 73-8.e1-4. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, L.; Marulli, A.; Dawson, J.A.; Owen, L.S.; Manley, B.J.; Donath, S.M.; Davis, P.G.; Kamlin, C.O.F. Cerebral oxygenation during skin-to-skin care in preterm infants not receiving respiratory support. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F137–F142. [Google Scholar] [CrossRef] [PubMed]
- Begum, E.A.; Bonno, M.; Ohtani, N.; Yamashita, S.; Tanaka, S.; Yamamoto, H.; Kawai, M.; Komada, Y. Cerebral oxygenation responses during kangaroo care in low birth weight infants. BMC Pediatr. 2008, 8, 51. [Google Scholar] [CrossRef] [Green Version]
- Seidman, G.; Unnikrishnan, S.; Kenny, E.; Myslinski, S.; Cairns-Smith, S.; Mulligan, B.; Engmann, C. Barriers and enablers of kangaroo mother care practice: A systematic review. PLoS ONE 2015, 10, e0125643. [Google Scholar] [CrossRef] [Green Version]
- Lorenz, L.; Dawson, J.A.; Jones, H.; Jacobs, S.E.; Cheong, J.L.; Donath, S.M.; Davis, P.G.; Kamlin, C.O.F. Skin-to-skin care in preterm infants receiving respirator support does not lead to physiological instability. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F339–F344. [Google Scholar] [CrossRef]
- Alderliesten, T.; Dix, L.; Baerts, W.; Caicedo, A.; van Huffel, S.; Naulaers, G.; Groenendaal, F.; van Bel, F.; Lemmers, P. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr. Res. 2016, 79, 55–64. [Google Scholar] [CrossRef]
- Pichler, G.; Binder, C.; Alexander, A.; Beckenbach, E.; Schmölzer, M.G.; Urlesberger, B. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J. Pediatr. 2013, 163, 1558–1563. [Google Scholar] [CrossRef]
- Hanke, K.; Rausch, T.K.; Paul, P.; Hellwig, I.; Krämer, C.; Stichtenoth, G.; Herz, A.; Wieg, C.; König, I.R.; Göpel, W.; et al. The effect of less invasive surfactant administration on cerebral oxygenation in preterm infants. Acta Paediatr. 2020, 109, 291–299. [Google Scholar] [CrossRef] [PubMed]
| NIRS 1 | NIRS 2 | Total | |
|---|---|---|---|
| Number of infants | 53 | 23 | 76 |
| Gestational age (weeks) | 29.7 [28.0; 31.2] | 26.9 [25.3; 28.0] | 28.8 [27; 30.7] |
| Birth weight (g) | 1270 [1045; 1570] | 920 [650; 980] | 1149 [953; 1454] |
| Female gender | 25 (47) | 8 (35) | 33 (43) |
| Multiple birth | 17 (32) | 2 (9) | 19 (25) |
| Surfactant application | 31 (58) | 18 (78) | 49 (65) |
| Oxygen application | 31 (58) | 18 (78) | 49 (65) |
| Primary intubation | 8 (15) | 6 (26) | 14 (18) |
| Duration of invasive ventilation (h) | 25 [17.25; 58.75] | 54.5 [10.25; 120] | 25 [15.25; 77.5] |
| Pneumonia | 2 (4) | 2 (9) | 4 (5) |
| Sepsis | 15 (28) | 3 (13) | 18 (24) |
| NIRS 1 (n = 53) | NIRS 2 (n = 23) | |||
|---|---|---|---|---|
| Time Period | Period I Resting | Period III Care | Period I Resting | Period III Care |
| v | 2,299,792 | 358,452 | 977,026 | 148,820 |
| Mean ± SD | 80.63 ± 9.79 | 79.45 ± 10.21 | 76.84 ± 10.06 | 75.45 ± 9.76 |
| Median [Q1; Q3] | 82 [76; 88] | 81 [74; 87] | 78 [71; 83] | 76 [71; 82] |
| Minimum | 15 | 15 | 15 | 15 |
| Maximum | 95 | 95 | 95 | 95 |
| a | NIRS 1 (n = 38) | NIRS 2 (n = 15) | ||||
| Time Period | Period I Resting | Period II SSC | Period III Care | Period I Resting | Period II SSC | Period III Care |
| v | 1,772,009 | 115,555 | 260,101 | 613,555 | 49,057 | 105,898 |
| Mean ± SD | 81.62 ± 9.56 | 81.62 ± 8.67 | 81.19 ± 8.85 | 79.48 ± 7.66 | 77.45 ± 7.45 | 77.44 ± 7.90 |
| Median [Q1; Q3] | 83 [77; 88] | 83 [78; 87] | 82 [76; 88] | 80 [74; 85] | 78 [73; 82] | 78 [72; 83] |
| Minimum | 15 | 25 | 19 | 15 | 15 | 15 |
| Maximum | 95 | 95 | 95 | 95 | 95 | 95 |
| b | Combined Data of NIRS 1 and NIRS 2 | |||||
| Time Period | Period I Resting | Period II SSC | Period III Care | |||
| Median [Q1; Q3] | 82 [77; 87] | 81 [76; 86] | 81 [76; 86] | |||
| Minimum | 68 | 62 | 67 | |||
| Maximum | 95 | 92 | 95 | |||
| Number of values per infant in the periods | ||||||
| Median [Q1; Q3] | 41,910 [40,094; 45,362] | 2812 [1260; 4506] | 6770 [6511; 7386] | |||
| Minimum | 33,505 | 472 | 4698 | |||
| Maximum | 60,814 | 9245 | 8447 | |||
| c | Results of the GLMM | |||||
| Estimate | SE | OR [95%-CI] | p-Value | |||
| Intercept | −3.0008 | 1.4369 | 0.050 [−2.767; 2.866] | |||
| Female gender | 0.1993 | 0.1626 | 1.220 [0.902; 1.539] | |||
| Gestational age | 0.1570 | 0.0485 | 1.770 [1.075; 1.265] | |||
| NIRS 2 | −0.1188 | 0.2051 | 0.888 [0.486; 1.290] | |||
| SSC (period II) | Reference | |||||
| Resting (period I) | 0.1639 | 0.0381 | 1.178 [1.103; 1.253] | <0.0001 | ||
| Nursing care (period III) | 0.0112 | 0.0413 | 1.011 [0.930; 1.092] | 0.7869 | ||
| NIRS 1 (n = 38) | NIRS 2 (n = 15) | |||||
|---|---|---|---|---|---|---|
| rcSO2 (%) | Period I Resting | Period II SSC | Period III Handling | Period I Resting | Period II SSC | Period III Handling |
| v | 1,772,009 | 115,555 | 260,101 | 613,555 | 49,057 | 105,898 |
| 15–< 55% | 2.1 | 1.2 | 0.4 | 0.3 | 0.4 | 0.5 |
| 55–85% | 60.3 | 63.4 | 65 | 78.8 | 87.5 | 84.7 |
| 15–< 65% | 5.5 | 5.3 | 4.7 | 2.6 | 3.4 | 5.1 |
| 15–< 70% | 9.7 | 9.5 | 10.7 | 9.6 | 13.7 | 14.7 |
| 15–< 80% | 34.6 | 32.3 | 38.3 | 48.2 | 59.5 | 59.6 |
| >85–95% | 37.6 | 35.4 | 34.5 | 21 | 12.1 | 14.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanke, K.; Rausch, T.K.; Sosnowski, R.; Paul, P.; Spiegler, J.; Müller, M.; König, I.R.; Göpel, W.; Herting, E.; Härtel, C. Early Skin-to-Skin Contact Does Not Affect Cerebral Tissue Oxygenation in Preterm Infants <32 Weeks of Gestation. Children 2022, 9, 211. https://doi.org/10.3390/children9020211
Hanke K, Rausch TK, Sosnowski R, Paul P, Spiegler J, Müller M, König IR, Göpel W, Herting E, Härtel C. Early Skin-to-Skin Contact Does Not Affect Cerebral Tissue Oxygenation in Preterm Infants <32 Weeks of Gestation. Children. 2022; 9(2):211. https://doi.org/10.3390/children9020211
Chicago/Turabian StyleHanke, Kathrin, Tanja K. Rausch, Runa Sosnowski, Pia Paul, Juliane Spiegler, Mirja Müller, Inke R. König, Wolfgang Göpel, Egbert Herting, and Christoph Härtel. 2022. "Early Skin-to-Skin Contact Does Not Affect Cerebral Tissue Oxygenation in Preterm Infants <32 Weeks of Gestation" Children 9, no. 2: 211. https://doi.org/10.3390/children9020211
APA StyleHanke, K., Rausch, T. K., Sosnowski, R., Paul, P., Spiegler, J., Müller, M., König, I. R., Göpel, W., Herting, E., & Härtel, C. (2022). Early Skin-to-Skin Contact Does Not Affect Cerebral Tissue Oxygenation in Preterm Infants <32 Weeks of Gestation. Children, 9(2), 211. https://doi.org/10.3390/children9020211






