The Rates of Breastfeeding in Baby-Friendly Hospitals in Greece: A Nationwide Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sample
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. BF Rates
3.3. Factors Influencing EBF and BF Rates
3.4. Logistic Regression with Reference to the Factors That Influence EBF:
4. Discussion
4.1. EBF Rates during the First 6 Months
4.2. Which Are the Key Points for the Promotion of EBF?
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ΕΒF | Exclusive breastfeeding |
| WHO | World Health Organization |
| BF | Breastfeeding |
| BFH | Baby Friendly Hospital |
| CS | Cesarean section |
| VD | Vaginal Delivery |
References
- World Health Organization. Global Strategy for Infant and Young Child Feeding; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Schwarz, E.B.; Ray, R.M.; Stuebe, A.M.; Allison, M.A.; Ness, R.B.; Freiberg, M.S.; Cauley, J.A. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet. Gynecol. 2009, 113, 974–982. [Google Scholar] [CrossRef]
- Bauer, J.; Gerss, J. Longitudinal analysis of macronutrients and minerals in human milk produced by mothers of preterm infants. Clin. Nutr. 2011, 30, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, D.U.; Proietti, F.A.; Ribas, J.G.; Araújo, M.G.; Pinheiro, S.R.; Guedes, A.C.; Carneiro-Proietti, A.B. Epidemiology, treatment, and prevention of human T-cell leukemia virus type 1-associated diseases. Clin. Microbiol. Rev. 2010, 23, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Horvath, T.; Madi, B.C.; Iuppa, I.M.; Kennedy, G.E.; Rutherford, G.; Read, J.S. Interventions for preventing late postnatal mother-to-child transmission of HIV. Cochrane Database Syst. Rev. 2009, 2009, CD006734. [Google Scholar] [CrossRef]
- Coppa, G.V.; Gabrielli, O.; Zampini, L.; Galeazzi, T.; Ficcadenti, A.; Padella, L.; Santoro, L.; Soldi, S.; Carlucci, A.; Bertino, E.; et al. Oligosaccharides in 4 different milk groups, Bifidobacteria, and Ruminococcus obeum. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 80–87. [Google Scholar] [CrossRef]
- Callen, J.; Pinelli, J. A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Adv. Neonatal. Care. 2005, 5, 72–88, quiz 89–92. [Google Scholar] [CrossRef]
- Iliodromiti, Z.; Zografaki, I.; Papamichail, D.; Stavrou, T.; Gaki, E.; Ekizoglou, C.; Nteka, E.; Mavrika, P.; Zidropoulos, S.; Panagiotopoulos, T.; et al. Increase of breast-feeding in the past decade in Greece, but still low uptake: Cross-sectional studies in 2007 and 2017. Public Health Nutr. 2020, 23, 961–970, Epub 2020 Jan 17. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed]
- Still, R.; Marais, D.; Hollis, J.L. Mothers’ understanding of the term ‘exclusive breastfeeding’: A systematic review. Matern Child Nutr. 2017, 13, e12336. [Google Scholar] [CrossRef]
- Available online: https://www.who.int/publications/i/item/9789241513807 (accessed on 1 January 2022).
- WHO European Region Has Lowest Global Breastfeeding Rates. Available online: https://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newbornhealth/news/news/2015/08/who-european-region-has-lowest-global-breastfeedingrates (accessed on 13 February 2021).
- Binns, C.; Lee, M.; Low, W.Y. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac. J. Public Health 2016, 28, 7–14, PMID: 30562307. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; UNICEF. Global Nutrition Targets 2025: Breastfeeding Policy Brief. [Internet] 2014. Available online: http://apps.who.int/iris/bitstream/10665/149022/1/WHO_NMH_NHD_14.7_eng.pdf?ua=1 (accessed on 3 August 2022).
- Theurich, M.A.; Davanzo, R.; Busck-Rasmussen, M.; Díaz-Gómez, N.M.; Brennan, C.; Kylberg, E.; Bærug, A.; McHugh, L.; Weikert, C.; Abraham, K.; et al. Breastfeeding Rates and Programs in Europe: A Survey of 11 National Breastfeeding Committees and Representatives. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Braegger, C.; Decsi, T.; Kolacek, S.; Koletzko, B.; Michaelsen, K.F.; Mihatsch, W.; Moreno, L.A.; Puntis, J.; ESPGHAN Committee on Nutrition; et al. Breast-feeding: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Breastfeeding. Available online: https://www.cdc.gov/breastfeeding/data/facts.html (accessed on 2 August 2022).
- Bosi, A.T.; Eriksen, K.G.; Sobko, T.; Wijnhoven, T.M.; Breda, J. Breastfeeding practices and policies in WHO European Region Member States. Public Health Nutr. 2016, 19, 753–764, Epub 2015 Jun 22. [Google Scholar] [CrossRef]
- Yotebieng, M.; Labbok, M.; Soeters, H.M.; Chalachala, J.L.; Lapika, B.; Vitta, B.S.; Behets, F. Ten Steps to Successful Breastfeeding programme to promote early initiation and exclusive breastfeeding in DR Congo: A cluster-randomised controlled trial. Lancet Glob. Health. 2015, 3, e546–e555. [Google Scholar] [CrossRef]
- Chen, C.; Yan, Y.; Gao, X.; Xiang, S.; He, Q.; Zeng, G.; Liu, S.; Sha, T.; Li, L. Influences of Cesarean Delivery on Breastfeeding Practices and Duration: A Prospective Cohort Study. J. Hum. Lact. 2018, 34, 526–534. [Google Scholar] [CrossRef]
- Li, L.; Wan, W.; Zhu, C. Breastfeeding after a cesarean section: A literature review. Midwifery 2021, 103, 103117. [Google Scholar] [CrossRef]
- Sharma, A. Efficacy of early skin-to-skin contact on the rate of exclusive breastfeeding in term neonates: A randomized controlled trial. Afr. Health Sci. 2016, 16, 790–797. [Google Scholar] [CrossRef]
- Huang, J.Z.; Chen, C.N.; Lee, C.P.; Kao, C.H.; Hsu, H.C.; Chou, A.K. Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design. Nutrients 2022, 14, 1846. [Google Scholar] [CrossRef] [PubMed]
- Greiner, T. Exclusive breastfeeding: Measurement and indicators. Int. Breastfeed J. 2014, 9, 18. [Google Scholar] [CrossRef]
- Khan, J.; Vesel, L.; Bahl, R.; Martines, J.C. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: Effects on neonatal mortality and morbidity-A systematic review and meta-analysis. Matern. Child Health J. 2015, 19, 468–479. [Google Scholar] [CrossRef]
- Lumbiganon, P.; Martis, R.; Laopaiboon, M.; Festin, M.R.; Ho, J.J.; Hakimi, M. Antenatal breastfeeding education for increasing breastfeeding duration. Cochrane Database Syst. Rev. 2011, 11, CD006425, Update in: Cochrane Database Syst. Rev. 2012, 9, CD006425. [Google Scholar] [CrossRef]
- Cantone, D.; Lombardi, A.; Assunto, D.A.; Piccolo, M.; Rizzo, N.; Pelullo, C.P.; Attena, F. A standardized antenatal class reduces the rate of cesarean section in southern Italy: A retrospective cohort study. Medicine 2018, 97, e0456. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, B.; Levitt, C.; Heaman, M.; O’Brien, B.; Sauve, R.; Kaczorowski, J. Breastfeeding Rates and Hospital Breastfeeding Practices in Canada: A National Survey of Women. Birth 2009, 36, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Neves, P.A.R.; Barros, A.J.D.; Gatica-Domínguez, G.; Vaz, J.S.; Baker, P.; Lutter, C.K. Maternal education and equity in breastfeeding: Trends and patterns in 81 low- and middle-income countries between 2000 and 2019. Int. J. Equity Health 2021, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Laksono, A.D.; Wulandari, R.D.; Ibad, M.; Kusrini, I. The effects of mother’s education on achieving exclusive breastfeeding in Indonesia. BMC Public Health 2021, 21, 14. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Metric, n (%) |
|---|---|
| Maternal Age (in years) | |
| 15–18 | 20 (1.6%) |
| 18–30 | 422 (35.3%) |
| 31–40 | 685 (57.3%) |
| 41–48 | 70 (5.8%) |
| Family status | |
| Single | 119 (9.9%) |
| Married | 1081 (90.1%) |
| Maternal educational attainment | |
| Primary School | 106 (8.8%) |
| High school | 568 (47.4%) |
| University | 524 (43.8%) |
| Maternal employment status during pregnancy | |
| Yes | 645 (53.7%) |
| No | 555 (46.3%) |
| First pregnancy | |
| Yes | 560 (46.6%) |
| No | 640 (53.4%) |
| Mode of delivery | |
| Cesarean section | 732 (61%) |
| Vaginal delivery | 468 (39%) |
| Previous experience of breastfeeding | |
| Yes | 608 (50.6%) |
| No | 592 (49.4) |
| Baby weight (g) median [Q1–Q3 range] | 3140 [2880–3430] |
| Question | n (%) |
|---|---|
| Mothers attended antenatal classes during the current pregnancy | |
| Yes | 224 (18.7%) |
| No | 976 (81.3%) |
| Why didn’t mothers attend antenatal classes of breastfeeding? | |
| COVID-19 | 366 (37.5%) |
| Insufficient knowledge | 256 (26.2%) |
| Not interested | 28 (2.8%) |
| No free time | 210 (21.5%) |
| Language difficulties | 19 (1.9%) |
| Not applicable | 32 (3.3%) |
| Maternal health issue | 56 (5.8) |
| Other reason | 9 (1%) |
| Mothers attended antenatal classes during a previous pregnancy | 234 (36.2%) |
| Mothers knew before their admission that the hospital they delivered is certified as a “Baby Friendly Hospital” | 828 (69.4%) |
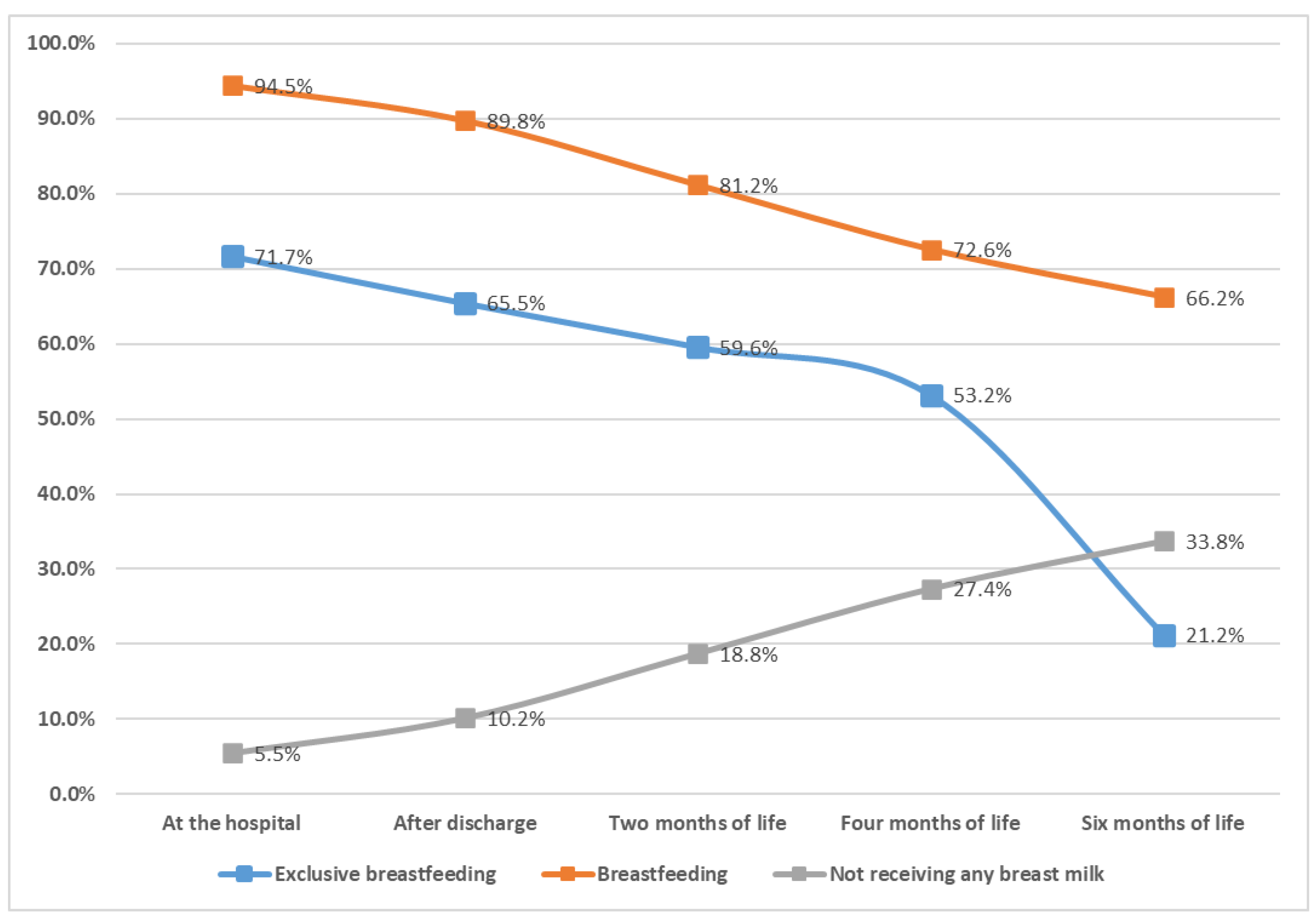
| Delivery Type. | Exclusive Breastfeeding | Breastfeeding | Not Receiving Any Breast Milk | Total | p * | p ** |
|---|---|---|---|---|---|---|
| At the hospital | ||||||
| VD | 383 (81.84%) | 451 (96.3%) | 17 (3.7%) | 468 | <0.0001 | 0.0267 |
| CS | 477 (65.25%) | 682 (93.3%) | 49 (6.7%) | 731 | ||
| Total | 860 (71.73%) | 1133 (94.5%) | 66 (5.5%) | 1199 | ||
| After hospital exit | ||||||
| VD | 357 (76.28%) | 433 (92.5%) | 35 (7.5%) | 468 | <0.0001 | 0.0140 |
| CS | 428 (58.55%) | 644 (88.1%) | 87 (11.9%) | 731 | ||
| Total | 785 (65.47%) | 1077 (89.8%) | 122 (10.2%) | 1199 | ||
| Two months after birth | ||||||
| VD | 326 (69.81%) | 408 (87.4%) | 59 (12.6%) | 467 | <0.0001 | <0.0001 |
| CS | 388 (53.08%) | 565 (77.3%) | 166 (22.7%) | 731 | ||
| Total | 714 (59.6%) | 973 (81.2%) | 225 (18.8%) | 1198 | ||
| Four months after birth | ||||||
| VD | 297 (63.73%) | 369 (79.2%) | 97 (20.8%) | 466 | <0.0001 | <0.0001 |
| CS | 340 (46.51%) | 500 (68.4%) | 231 (31.6%) | 731 | ||
| Total | 637 (53.22%) | 232 (72.6%) | 328 (27.4%) | 1197 | ||
| Six months after birth | ||||||
| VD | 115 (24.68%) | 348 (74.7%) | 118 (25.3%) | 466 | 0.0235 | <0.0001 |
| CS | 139 (19.02%) | 445 (60.7%) | 286 (39.3%) | 731 | ||
| Total | 254 (21.22%) | 793 (66.2%) | 404 (33.8%) | 1197 | ||
| Time of First Breastfeed | Exclusive Breastfeeding | Breastfeeding | Not Receiving Any Breast Milk | Total | p * | p ** | p † | p ‡ |
|---|---|---|---|---|---|---|---|---|
| At the hospital | ||||||||
| 1st hour | 648 (78.64%) | 790 (95.9%) | 34 (4.1%) | 824 (69.8%) | 0.0110 | 0.3417 | <0.0001 | 0.3770 |
| After the 1st hour and within 24 h | 181 (70.7%) | 249 (97.2%) | 7 (2.8%) | 256 (21.7%) | ||||
| After 24 h | 31 (31%) | 94 (94%) | 6 (6%) | 100 (8.5%) | ||||
| Total | 860 (72.9%) | 273 (23.1%) | 47 (4%) | 1180 (100%) | ||||
| After hospital exit | ||||||||
| 1st hour | 589 (71.5%) | 748 (90.7%) | 76 (9.3%) | 824 (69.8%) | 0.0517 | 0.5920 | <0.0001 | 0.2751 |
| After the 1st hour and within 24 h | 166 (64.8%) | 235 (91.8%) | 21 (8.2%) | 256 (21.7%) | ||||
| After 24 h | 30 (30%) | 94 (94%) | 6 (6%) | 100 (8.5%) | ||||
| Total | 785 (66.5%) | 1077 (91.2%) | 103 (8.8%) | 1180 (100%) | ||||
| Two months after birth | ||||||||
| 1st hour | 533 (64.7%) | 683 (83%) | 140 (17%) | 823 (69.8%) | 0.0403 | 0.7115 | <0.0001 | 0.4544 |
| After the 1st hour and within 24 h | 147 (57.4%) | 210 (82%) | 46 (18%) | 256 (21.7%) | ||||
| After 24 h | 34 (34%) | 80 (80%) | 20 (20%) | 100 (8.5%) | ||||
| Total | 714 (60.56%) | 973 (82.5%) | 206 (17.5%) | 1179 (100%) | ||||
| Four months after birth | ||||||||
| 1st hour | 492 (59.85%) | 627 (76.2%) | 195 (23.8%) | 822 (69.8%) | 0.0001 | 0.1549 | <0.0001 | 0.0001 |
| After the 1st hour and within 24 h | 116 (45.31%) | 184 (71.8%) | 72 (28.2%) | 256 (21.7%) | ||||
| After 24 h | 29 (29%) | 58 (58%) | 42 (42%) | 100 (8.5%) | ||||
| Total | 637 (54%) | 869 (73.7%) | 309 (26.3%) | 1178 (100%) | ||||
| Six months after birth | ||||||||
| 1st hour | 200 (24.3%) | 580 (70.5%) | 242 (29.5%) | 822 (69.8%) | 0.0303 | 0.0533 | 0.0009 | <0.0001 |
| After the 1st hour and within 24 h | 45 (17.6%) | 164 (64.1%) | 92 (35.9%) | 256 (21.7%) | ||||
| After 24 h | 9 (9%) | 49 (49%) | 51 (51%) | 100 (8.5%) | ||||
| Total | 254 (21.6%) | 793 (67.3%) | 385 (32.7%) | 1178 (100%) | ||||
| Gestational Age | Exclusive Breastfeeding | Breastfeeding | Not Receiving Any Breast Milk | Total | p * | p ** | p † | p ‡ |
|---|---|---|---|---|---|---|---|---|
| At the hospital | ||||||||
| <34 weeks | 1 (10%) | 8 (80%) | 2 (20%) | 10 | 0.1605 | 0.1661 | <0.0001 | 0.0413 |
| 34–36 + 6 weeks | 37 (37.8%) | 91 (92.8%) | 7 (7.2%) | 98 | ||||
| ≥37 weeks | 822 (75.3%) | 1034 (94.7%) | 57 (5.3%) | 1091 | ||||
| Total | 860 (71.7%) | 1133 (94.5%) | 66 (5.5%) | 1199 | ||||
| After hospital exit | ||||||||
| <34 weeks | 1 (10%) | 10 (100%) | 0 (0%) | 10 | 0.1780 | 0.2913 | 0.0003 | 0.2844 |
| 34–36 + 6 weeks | 36 (36.7%) | 88 (89.8%) | 10 (10.2%) | 98 | ||||
| ≥37 weeks | 748 (68.5%) | 979 (89.7%) | 112 (10.3%) | 1091 | ||||
| Total | 785 (65.4%) | 1077 (89.8%) | 122 (10.2%) | 1199 | ||||
| Two months after birth | ||||||||
| <34 weeks | 2 (20%) | 8 (80%) | 2 (20%) | 10 | 0.5994 | 0.5649 | 0.0158 | 0.8632 |
| 34–36 + 6 weeks | 33 (33.7%) | 70 (71.4%) | 28 (28.6%) | 98 | ||||
| ≥37 weeks | 679 (62.3%) | 895 (82.1%) | 195 (17.9%) | 1090 | ||||
| Total | 714 (59.6%) | 973 (81.2%) | 225 (18.8%) | 1198 | ||||
| Four months after birth | ||||||||
| <34 weeks | 2 (20%) | 5 (50%) | 5 (50%) | 10 | 0.9441 | 0.6278 | 0.0505 | 0.0843 |
| 34–36 + 6 weeks | 26 (26.5%) | 57 (58.2%) | 41 (41.8%) | 98 | ||||
| ≥37 weeks | 609 (55.92%) | 807 (74.1%) | 282 (25.9%) | 1089 | ||||
| Total | 637 (53.22%) | 869 (72.6%) | 328 (27.4%) | 1197 | ||||
| Six months after birth | ||||||||
| <34 weeks | 2 (20%) | 3 (30%) | 7 (70%) | 10 | 0.3356 | 0.2078 | 0.8533 | 0.0109 |
| 34–36 + 6 weeks | 6 (6.1%) | 50 (51%) | 48 (49%) | 98 | ||||
| ≥37 weeks | 246 (22.6%) | 740 (67.9%) | 349 (32.1%) | 1089 | ||||
| Total | 254 (21.2%) | 793 (66.2%) | 404 (33.8%) | 1197 | ||||
| Attended Classes | Exclusive Breastfeeding | Breastfeeding | Not Receiving Any Breast Milk | Total | p * | p ** |
|---|---|---|---|---|---|---|
| At the hospital | ||||||
| Yes | 354 (83.9%) | 411 (97.4%) | 11 (2.6%) | 422 | <0.0001 | 0.0011 |
| No | 506 (65.1%) | 722 (92.9%) | 55 (7.1%) | 777 | ||
| Total | 860 (71.7%) | 1133 (94.5%) | 66 (5.5%) | 1199 | ||
| After hospital exit | ||||||
| Yes | 339 (80.3%) | 405 (96%) | 17 (4%) | 422 | <0.0001 | <0.0001 |
| No | 446 (57.4%) | 670 (86.5%) | 105 (13.5%) | 777 | ||
| Total | 785 (65.5%) | 1077 (89.8%) | 122 (10.2%) | 1199 | ||
| Two months after birth | ||||||
| Yes | 317 (75.1%) | 385 (92.2%) | 37 (8.8%) | 422 | <0.0001 | 0.0008 |
| No | 397 (51.2%) | 588 (75.8%) | 188 (24.2%) | 776 | ||
| Total | 714 (59.6%) | 973 (81.2%) | 225 (18.8%) | 1198 | ||
| Four months after birth | ||||||
| Yes | 291 (69.1%) | 359 (85.3%) | 62 (14.7%) | 421 | <0.0001 | 0.0477 |
| No | 346 (44.6%) | 510 (65.7%) | 266 (34.3%) | 776 | ||
| Total | 637 (53.2%) | 869 (72.6%) | 328 (27.4%) | 1197 | ||
| Six months after birth | ||||||
| Yes | 122 (29%) | 339 (80.5%) | 82 (19.5%) | 421 | <0.0001 | 0.0010 |
| No | 132 (17%) | 454 (58.5%) | 322 (41.5%) | 776 | ||
| Total | 254 (21.2%) | 793 (66.3%) | 404 (33.7%) | 1197 | ||
| At the Hospital | After Hospital Exit | Two Months after Birth | Four Months after Birth | Six Months After Birth | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Effect | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Attended antenatal courses (yes vs no) | 1.93 (1.39–2.69) | <0.0001 | 2.06 (1.53–2.79) | <0.0001 | 1.93 (1.46–2.55) | <0.0001 | 1.95 (1.5–2.54) | <0.0001 | 1.71 (1.34–2.18) | <0.0001 |
| Delivery method (CS vs VD) | 0.54 (0.4–0.74) | 0.0002 | 0.53 (0.39–0.7) | <0.0001 | 0.53 (0.41–0.7) | <0.0001 | 0.63 (0.48–0.81) | 0.0003 | 0.73 (0.58–0.93) | 0.0107 |
| Gestational age (34–36 + 6 w vs <34 w) | 3.5 (0.94–13.11) | 0.7728 | 1.67 (0.46–6.02) | 0.8066 | 0.85 (0.24–3.06) | 0.2083 | 1 (0.27–3.71) | 0.3639 | 1.25 (0.32–4.97) | 0.65 |
| Gestational age (37w vs <34w) | 9.84 (2.72–35.54) | <0.0001 | 3.34 (0.97–11.57) | 0.0058 | 1.85 (0.54–6.37) | 0.0421 | 1.99 (0.56–7.07) | 0.0475 | 2.24 (0.59–8.53) | 0.0567 |
| Education level (high school vs school) | 2.77 (1.73–4.42) | 0.0133 | 4.02 (2.57–6.28) | 0.0001 | 4.08 (2.6–6.39) | 0.0011 | 2.81 (1.78–4.43) | 0.0372 | 2.64 (1.65–4.23) | 0.0646 |
| Education level (university vs school) | 3.53 (2.14–5.84) | <0.0001 | 5.3 (3.29–8.53) | <0.0001 | 6.53 (4.06–10.52) | <0.0001 | 4.36 (2.7–7.02) | <0.0001 | 4.11 (2.52–6.7) | <0.0001 |
| Family status (married vs single) | 1.45 (0.93–2.26) | 0.1035 | 1.68 (1.11–2.54) | 0.0146 | 2.02 (1.34–3.03) | 0.0007 | 2.33 (1.54–3.5) | <0.0001 | 1.82 (1.2–2.77) | 0.0049 |
| 1st breast feeding (after 1 h vs. within 1 h) | 0.65 (0.48–0.89) | 0.0079 | 0.81 (0.6–1.09) | 0.1628 | 0.91 (0.68–1.21) | 0.5015 | 0.69 (0.53–0.91) | 0.0078 | 0.75 (0.58–0.99) | 0.0392 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liakou, E.; Christou, E.; Iacovidou, N.; Pouliakis, A.; Sokou, R.; Petropoulou, C.; Volaki, P.; Triantafyllou, A.; Zantiotou, M.; Vrachnis, D.; et al. The Rates of Breastfeeding in Baby-Friendly Hospitals in Greece: A Nationwide Survey. Children 2022, 9, 1792. https://doi.org/10.3390/children9121792
Liakou E, Christou E, Iacovidou N, Pouliakis A, Sokou R, Petropoulou C, Volaki P, Triantafyllou A, Zantiotou M, Vrachnis D, et al. The Rates of Breastfeeding in Baby-Friendly Hospitals in Greece: A Nationwide Survey. Children. 2022; 9(12):1792. https://doi.org/10.3390/children9121792
Chicago/Turabian StyleLiakou, Eftychia, Evangelos Christou, Nicoletta Iacovidou, Abraham Pouliakis, Rozeta Sokou, Chrysa Petropoulou, Paraskevi Volaki, Anastasia Triantafyllou, Matina Zantiotou, Dionisios Vrachnis, and et al. 2022. "The Rates of Breastfeeding in Baby-Friendly Hospitals in Greece: A Nationwide Survey" Children 9, no. 12: 1792. https://doi.org/10.3390/children9121792
APA StyleLiakou, E., Christou, E., Iacovidou, N., Pouliakis, A., Sokou, R., Petropoulou, C., Volaki, P., Triantafyllou, A., Zantiotou, M., Vrachnis, D., Boutsikou, T., & Iliodromiti, Z. (2022). The Rates of Breastfeeding in Baby-Friendly Hospitals in Greece: A Nationwide Survey. Children, 9(12), 1792. https://doi.org/10.3390/children9121792








