Large-Scale Survey of Missing Deciduous Anterior Teeth on Medical Examination at the Age of 3.5 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Protocols
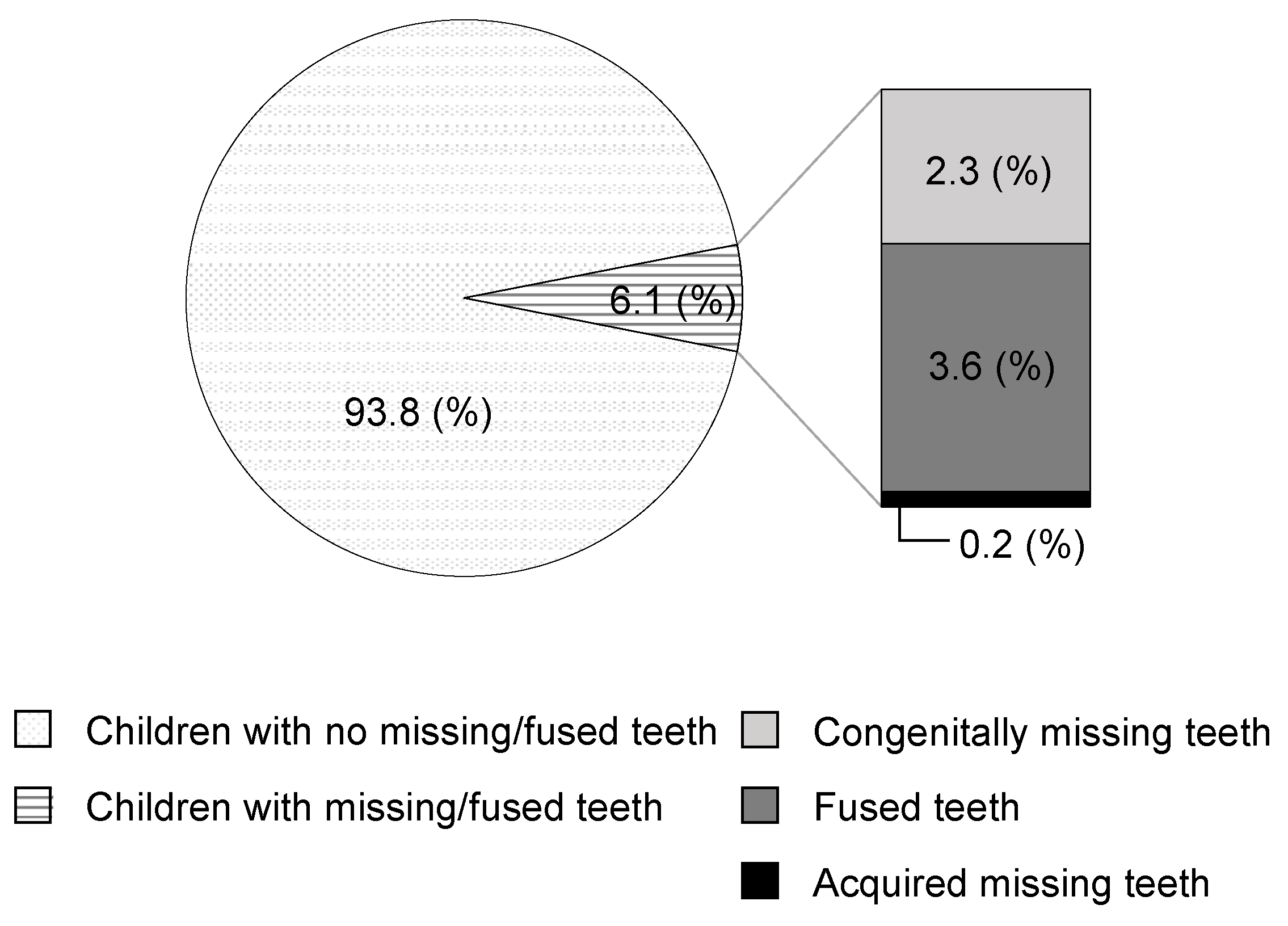
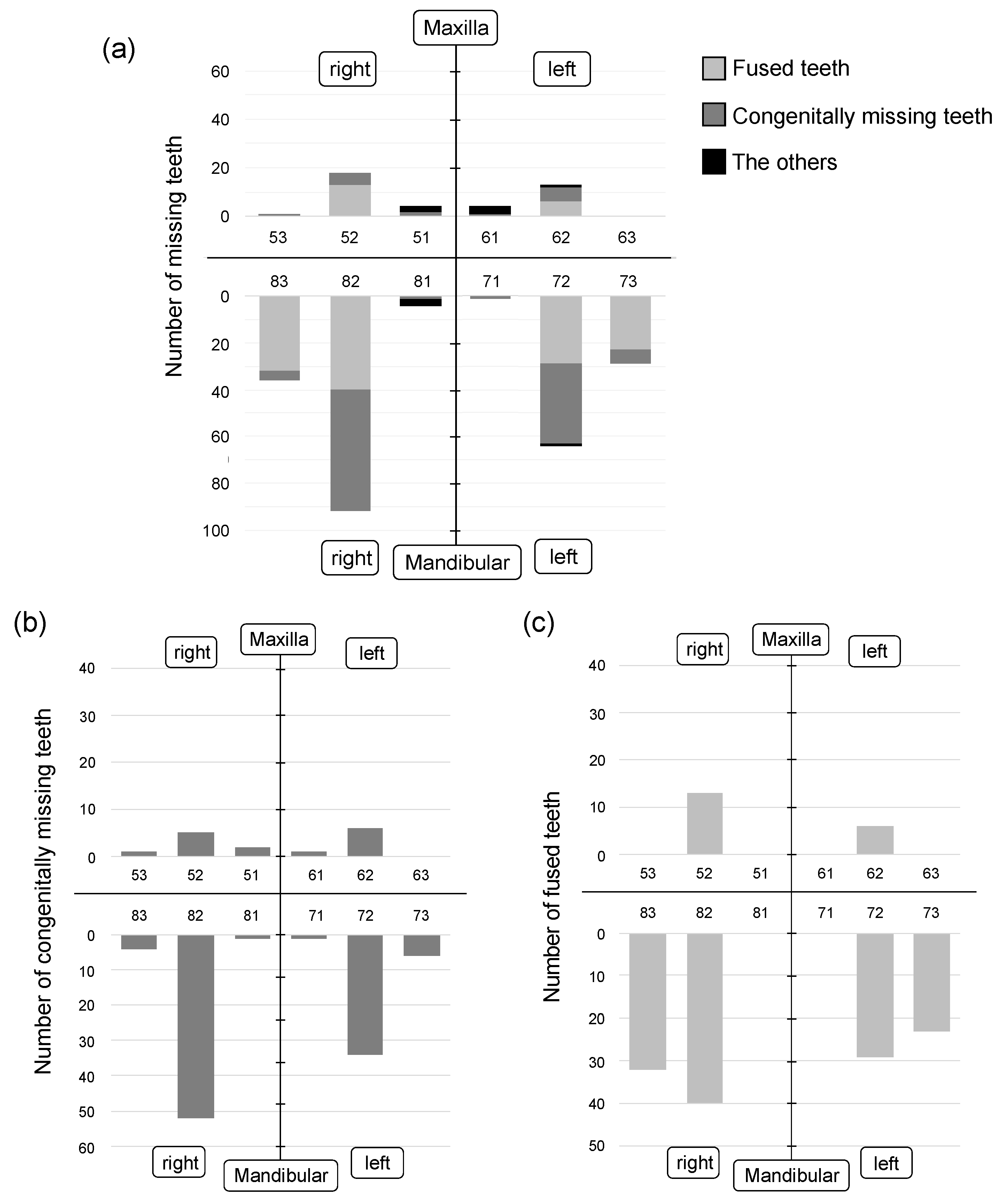
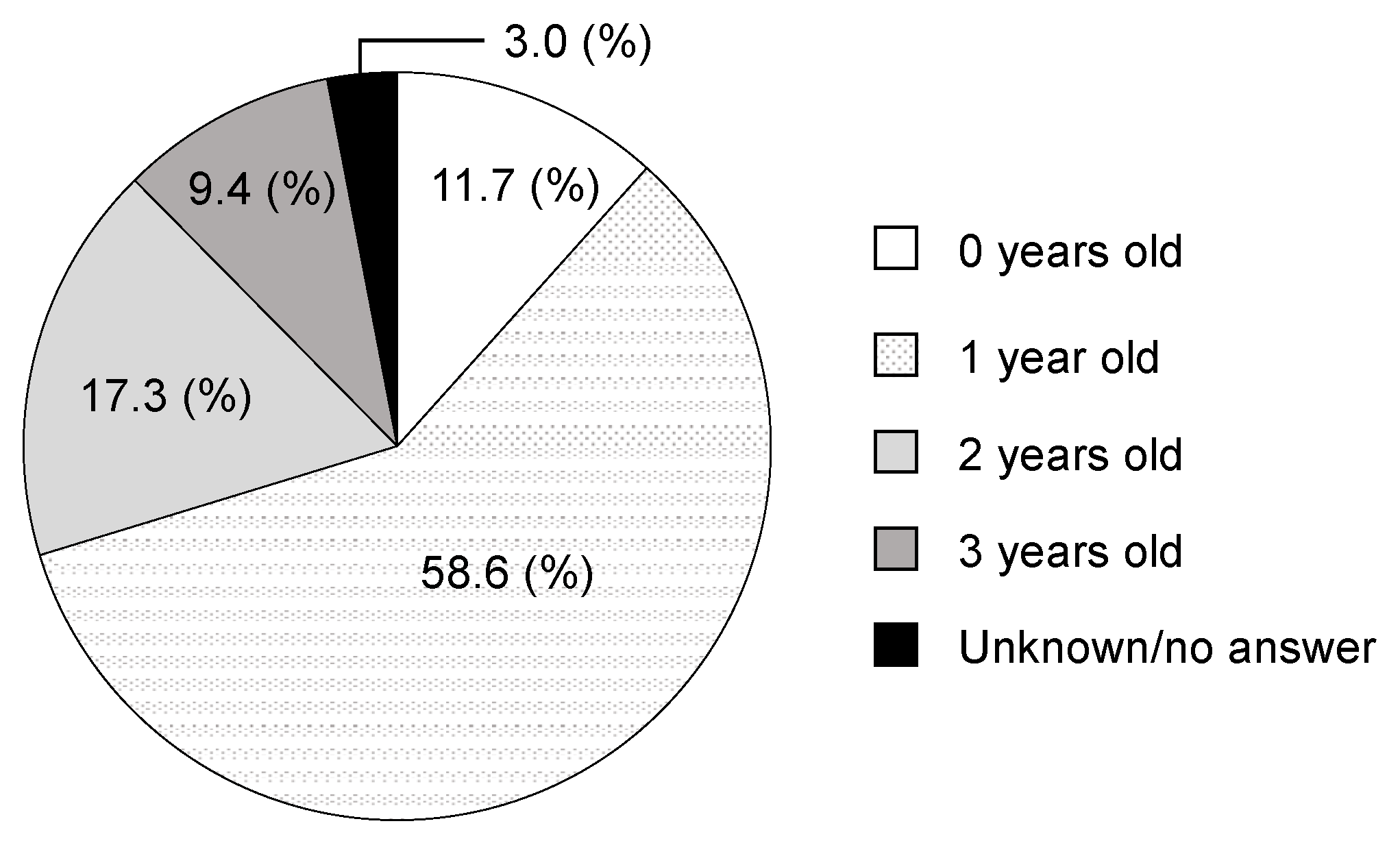
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rakhshan, V. Meta-analysis and systematic review of factors biasing the observed prevalence of congenitally missing teeth in permanent dentition excluding third molars. Prog. Orthod. 2013, 14, 33. [Google Scholar] [CrossRef] [PubMed]
- Altug-Atac, A.T.; Erdem, D. Prevalence and distribution of dental anomalies in orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.K.; Saxena, P.; Jain, S.; Jain, D. Prevalence and distribution of selected developmental dental anomalies in an Indian population. J. Oral Sci. 2011, 53, 231–238. [Google Scholar] [CrossRef]
- Hagiwara, Y.; Uehara, T.; Narita, T.; Tsutsumi, H.; Nakabayashi, S.; Araki, M. Prevalence and distribution of anomalies of permanent dentition in 9584 Japanese high school students. Odontology 2016, 104, 380–389. [Google Scholar] [CrossRef]
- Lochib, S.; Indushekar, K.R.; Saraf, B.G.; Sheoran, N.; Sardana, D. Occlusal characteristics and prevalence of associated dental anomalies in the primary dentition. J. Epidemiol. Glob. Health 2015, 5, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Goya, H.A.; Tanaka, S.; Maeda, T.; Akimoto, Y. An orthopantomographic study of hypodontia in permanent teeth of Japanese pediatric patients. J. Oral Sci. 2008, 50, 143–150. [Google Scholar] [CrossRef]
- Pemberton, T.J.; Das, P.; Patel, P.I. Hypodontia: Genetics and future perspectives. Braz. J. Oral Sci. 2005, 4, 695–709. [Google Scholar]
- Khalaf, K.; Miskelly, J.; Voge, E.; Macfarlane, T.V. Prevalence of hypodontia and associated factors: A systematic review and meta-analysis. J. Orthod. 2014, 41, 299–316. [Google Scholar] [CrossRef]
- Nadelman, P.; Magno, M.B.; Pithon, M.M.; Castro, A.C.R.; Maia, L.C. Does the premature loss of primary anterior teeth cause morphological, functional and psychosocial consequences? Braz. Oral Res. 2021, 35, e092. [Google Scholar] [CrossRef]
- Nadelman, P.; Bedran, N.; Magno, M.B.; Masterson, D.; Castro, A.C.R.; Maia, L.C. Premature loss of primary anterior teeth and its consequences to primary dental arch and speech pattern: A systematic review and meta-analysis. Int. Paediatr. Dent. 2020, 30, 687–712. [Google Scholar] [CrossRef]
- Rakhshan, V. Congenitally missing teeth (hypodontia): A review of the literature concerning the etiology, prevalence, risk factors, patterns and treatment. Dent. Res. J. 2015, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Maeda, T. Prevalence and genetic basis of tooth agenesis. Jpn. Dent. Sci. Rev. 2009, 45, 52–58. [Google Scholar] [CrossRef]
- Polder, B.J.; Van’t Hof, M.A.; Van der Linden, F.P.; Kuijpers-Jagtman, A.M. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent. Oral Epidemiol. 2004, 32, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Reali, J.; Mendoza-Ramos, M.I.; Garrido-Guerrero, E.; Méndez-Catalá, C.F.; Méndez-Cruz, A.R.; Pozo-Molina, G. Hypohidrotic ectodermal dysplasia: Clinical and molecular review. Int. J. Dermatol. 2018, 57, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Gungor, O.E.; Karayilmaz, H.; Yalcin, H.; Hatipoğlu, M. Oro-dental characteristics of three siblings with Papillon-Lefevre syndrome. Niger J. Clin. Pract. 2017, 20, 256–260. [Google Scholar]
- Spodzieja, K.; Olczak-Kowalczyk, D. Premature loss of deciduous teeth as a symptom of systemic disease: A narrative literature review. Int. J. Environ. Res. Public Health 2022, 19, 3386. [Google Scholar] [CrossRef]
- Whyte, M.P. Hypophosphatasia: An overview for 2017. Bone 2017, 102, 15–25. [Google Scholar] [CrossRef]
- Michigami, T.; Ohata, Y.; Fujiwara, M.; Mochizuki, H.; Adachi, M.; Kitaoka, T.; Kubota, T.; Sawai, H.; Namba, N.; Hasegawa, K.; et al. Clinical practice guidelines for hypophosphatasia. Clin. Pediatr. Endocrinol. 2020, 29, 9–24. [Google Scholar] [CrossRef]
- Bloch-Zupan, A. Hypophosphatasia: Diagnosis and clinical signs–a dental surgeon perspective. Int. J. Pediatr. Dent. 2016, 26, 426–438. [Google Scholar] [CrossRef]
- Indira, M.D.; Bhojraj, N.; Narayanappa, D. A cross-sectional study on eruption timing of primary teeth in children of Mysore, Karnataka. Indian J. Dent. Res. 2018, 29, 726–731. [Google Scholar] [CrossRef]
- Arita, K.; Abe, Y.; Nakano, K.; Saitoh, M.; Shimamura, K.; Osuga, M.; Ishitani, N.; Hamada, Y.; Atsumi, N.; Kodaira, H.; et al. Chronology of Deciduous and Permanent Dentition in Japanese Children II Part 1: Deciduous Dentition. Jpn. J. Ped. Dent. 2019, 57, 45–53. [Google Scholar]
- Terasaki, T.; Shiota, K. Congenital absence of teeth. Nihon Koku Kagakkai Zasshi 1954, 3, 88–93. (In Japanese) [Google Scholar]
- Ogita, S.; Ogita, M.; Yamamoto, T.; Yanase, H.; Kondo, Y.; Yokoi, K. The appearance of supernumerary teeth and congenitally missing teeth in Japanese pediatric patients. Aichi-Gakuin Daigaku Shigakkaishi 1995, 33, 19–27. (In Japanese) [Google Scholar]
- Inami, H.; Sodei, F.; Nozaka, K.; Amari, E. The clinical investigation of fused and congenital deficient teeth in primary dentition. Dent. J. Iwate Med. Univ. 1986, 11, 121–133. (In Japanese) [Google Scholar]
- Yamaguchi, N.; Muratsu, K.; Iwase, T.; Nara, Y.; Morioka, T. A study on congenital abnormalities of deciduous teeth in 3-year old children. J. Dent. Health 1991, 41, 79–85. [Google Scholar] [CrossRef]
- Alshahrani, I.; Togoo, R.A.; Alqarni, M.A. A review of hypodontia: Classification, prevalence, etiology, associated anomalies, clinical implications and treatment options. World J. Dent. 2013, 4, 117–125. [Google Scholar]
- Yonezu, T.; Hayashi, Y.; Sasaki, J.; Machida, Y. Prevalence of congenital dental anomalies of the deciduous dentition in Japanese children. Bull. Tokyo Dent. Coll. 1997, 38, 27–32. [Google Scholar]
- Carvalho, J.C.; Vinkler, F.; Declerck, D. Malocclusion, dental injuries and dental anomalies in the primary dentition of Belgian children. Int. J. Paediatr. Dent. 1998, 8, 137–141. [Google Scholar] [CrossRef]
- Kılınç, G.; Çetin, M. Congenital Dental Anomalies in the Primary Dentition. Curr. Res. Dent. Sci. 2020, 30, 247–253. [Google Scholar]
- Kapdan, A.; Kustarci, A.; Buldur, B.; Arslan, D.; Kapdan, A. Dental anomalies in the primary dentition of Turkish children. Eur. J. Dent. 2012, 6, 178–183. [Google Scholar] [CrossRef]
- Shilpa, G.; Gokhale, N.; Mallineni, S.K.; Nuvvula, S. Prevalence of dental anomalies in deciduous dentition and its association with succedaneous dentition: A cross-sectional study of 4180 South Indian children. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Deolia, S.G.; Chhabra, C.; Chhabra, K.G.; Kalghatgi, S.; Khandelwal, N. Dental anomalies of the deciduous dentition among Indian children: A survey from Jodhpur, Rajasthan, India. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Kramer, P.F.; Feldens, C.A.; Ferreira, S.H.; Spiguel, M.H.; Feldens, E.G. Dental anomalies and associated factors in 2- to 5-year-old Brazilian children. Int. J. Paediatr. Dent. 2008, 18, 434–440. [Google Scholar] [CrossRef]
- Whittington, B.R.; Durward, C.S. Survey of anomalies in primary teeth and their correlation with the permanent dentition. N. Z. Dent. J. 1996, 92, 4–8. [Google Scholar] [PubMed]
- Chen, Y.H.; Cheng, C.N.; Wang, Y.B.; Yang, C.Y. Prevalence of congenital dental anomalies in the primary dentition in Taiwan. Pediatr. Dent. 2010, 32, 525–529. [Google Scholar]
- Chang, P.S.; Yen, T.H.; Huang, C.J.; Yen, A.M.; Chen, S.L.; Tsai, A.I. Clinical Orodental Anomalies in Taiwanese Children under Age Six: A Study Based on the 1995–1997 National Dental Survey. Biomed. Res. Int. 2020, 19, 2056340. [Google Scholar] [CrossRef]
- King, N.M.; Tongkoom, S.; Wong, H.M. Morphological and Numerical Characteristics of the Southern Chinese Dentitions. Part III: Anomalies in the Primary Dentition. Open Anthropol. J. 2010, 3, 25–36. [Google Scholar]
- Tanaka, T.; Ohigashi, S.; Miyamoto, A.; Kuwahara, Y. Relationship between fusion or congenitally missing of anterior deciduous teeth and missing of their successors. Jpn. J. Ped. Dent. 2012, 50, 243–248. (In Japanese) [Google Scholar]
- Tasa, G.L.; Lukacs, J.R. The prevalence and expression of primary double teeth in western India. J. Dent. Child. 2001, 68, 196–200. [Google Scholar]
- Mornet, E. Hypophosphatasia. Metabolism 2018, 82, 142–155. [Google Scholar] [CrossRef]
- Shakra, K.A. Management of Unerupted Maxillary Deciduous Central Incisor: A Case Report. Int. J. Clin. Pediatr. Dent. 2014, 7, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Kapur, A.; Goyal, A.; Jaffri, S. Management of inverted impacted primary incisors: An unusual case. J. Indian Soc. Pedod. Prev. Dent. 2008, 26, 26–28. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; DeArmey, S.L.; Weber, T.J.; Kishnani, P.S. Case Series: Odontohypophosphatasia or missed diagnosis of childhood/adult-onset hypophosphatasia? Call for a long-term follow-up of premature loss of primary teeth. Bone Rep. 2016, 5, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Okawa, R.; Nakano, K.; Matsumoto, M.; Kawabata, K.; Ooshima, T. Oral manifestations of patients with hypophosphatasia. Ped. Dent. J. 2012, 22, 155–162. [Google Scholar] [CrossRef]
- Okawa, R.; Kadota, T.; Matayoshi, S.; Nakano, K. Dental manifestation leading to the diagnosis of hypophosphatasia in two children. J. Dent. Child. 2020, 87, 179–183. [Google Scholar]
- Okawa, R.; Kitaoka, T.; Saga, K.; Ozono, K.; Nakano, K. Report of two dental patients diagnosed with hypophosphatasia. J. Clin. Case Rep. 2016, 6, 1–5. [Google Scholar] [CrossRef]
- Mornet, E.; Yvard, A.; Taillandier, A.; Fauvert, D.; Simon-Bouy, B. A molecular- based estimation of the prevalence of hypophosphatasia in European population. Ann. Hum. Genet. 2011, 75, 439–445. [Google Scholar] [CrossRef]
| Reason for Missing Teeth | Number of Teeth (%) |
|---|---|
| Avulsion or exfoliation due to dental trauma | 11 (4.1) |
| Extraction due to dental trauma data | 1 (0.4) |
| Extraction due to dental caries | 1 (0.4) |
| Missing due to cleft lip and palate | 1 (0.4) |
| Unknown | 229 (86.1) |
| No answer | 23 (8.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otsuchi, T.; Ogaya, Y.; Suehiro, Y.; Okawa, R.; Nakano, K. Large-Scale Survey of Missing Deciduous Anterior Teeth on Medical Examination at the Age of 3.5 Years. Children 2022, 9, 1761. https://doi.org/10.3390/children9111761
Otsuchi T, Ogaya Y, Suehiro Y, Okawa R, Nakano K. Large-Scale Survey of Missing Deciduous Anterior Teeth on Medical Examination at the Age of 3.5 Years. Children. 2022; 9(11):1761. https://doi.org/10.3390/children9111761
Chicago/Turabian StyleOtsuchi, Tsutomu, Yuko Ogaya, Yuto Suehiro, Rena Okawa, and Kazuhiko Nakano. 2022. "Large-Scale Survey of Missing Deciduous Anterior Teeth on Medical Examination at the Age of 3.5 Years" Children 9, no. 11: 1761. https://doi.org/10.3390/children9111761
APA StyleOtsuchi, T., Ogaya, Y., Suehiro, Y., Okawa, R., & Nakano, K. (2022). Large-Scale Survey of Missing Deciduous Anterior Teeth on Medical Examination at the Age of 3.5 Years. Children, 9(11), 1761. https://doi.org/10.3390/children9111761





