The Use and Complications of Halo Gravity Traction in Children with Scoliosis
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Kamtsiuris, P.; Atzpodien, K.; Ellert, U.; Schlack, R.; Schlaud, M. Prevalence of somatic diseases in German children and adolescents. Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Bundesgesundheitsblatt Gesundh. Gesundh. 2007, 50, 686–700. [Google Scholar] [CrossRef] [PubMed]
- Cilli, K.; Tas, T.; Ozturk, H.; Oztemur, Z.; Unsaldi, T.; Tezeren, G.; Bulut, O. School screening for scoliosis in Sivas, Turkey. Acta Orthop. Traumatol. Turc. 2009, 43, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Scaturro, D.; Costantino, C.; Terrana, P.; Vitagliani, F.; Falco, V.; Cuntrera, D.; Sannasardo, C.E.; Vitale, F.; Mauro, G.L. Risk Factors, Lifestyle and Prevention among Adolescents with Idiopathic Juvenile Scoliosis: A Cross Sectional Study in Eleven First-Grade Secondary Schools of Palermo Province, Italy. Int. J. Environ. Res. Public Health 2021, 18, 12335. [Google Scholar] [CrossRef]
- Soucacos, P.N.; Zacharis, K.; Soultanis, K.; Gelalis, J.; Xenakis, T.; Beris, A.E. Risk Factors for Idiopathic Scoliosis: Review of a 6-Year Prospective Study. Orthopedics 2000, 23, 833–838. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J.; Weiss, H.-R.; Chockalingam, N.; Taranu, R.; Srinivas, S.; Hogg, J.; Whittaker, V.; Kalyan, R.V.; Arnell, T. Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst. Rev. 2015, 4, CD010663. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Aulisa, L.; Circo, A.B.; de Mauroy, J.C.; Durmala, J.; Grivas, T.B.; Knott, P.; Kotwicki, T.; Maruyama, T.; et al. 2011 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012, 7, 3. [Google Scholar] [CrossRef]
- Maruyama, T.; Takeshita, K. Surgical treatment of scoliosis: A review of techniques currently applied. Scoliosis 2008, 3, 41–46. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; Aldakhil, S.S.; Al-Rabiah, M.A.; Al-Rabiah, A.M. Surgical treatment of adolescent idiopathic scoliosis: Complications. Ann. Med. Surg. 2020, 52, 19–23. [Google Scholar] [CrossRef]
- De Mendonça, R.G.M.; Sawyer, J.R.; Kelly, D.M. Complications After Surgical Treatment of Adolescent Idiopathic Scoliosis. Orthop. Clin. N. Am. 2016, 47, 395–403. [Google Scholar] [CrossRef]
- Hamilton, D.K.; Smith, J.; Shaffrey, C.; Sansur, C.; Berven, S.; Broadstone, P.; Choma, T.; Goytan, M.; Noordeen, H.; Knapp, R.; et al. Rates of Neurological Injury Associated with Spine Surgery Based on 108,419 Procedures: A Report of the Scoliosis Research Society Morbidity And Mortality Committee. Spine J. 2011, 36, 1218–1228. [Google Scholar] [CrossRef] [PubMed]
- Pahys, J.M.; Guille, J.T.; D’Andrea, L.P.; Samdani, A.F.; Beck, J.; Betz, R.R. Neurologic injury in the surgical treatment of idiopathic scoliosis: Guidelines for as-sessment and management. JAAOS-J. Am. Acad. Orthop. Surg. 2009, 17, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Carp, M.; Tevanov, I.; Florea, C.; Ladaru, A.; Sterian, G.; Dusca, A.; Ulici, A.; Alex, A. Severe Kyphosis Secondary to Glucocorticoid-Induced Osteoporosis in Adolescent Twins with Congenital Adrenal Hyperplasia—A Case Report and Literature Review. J. Clin. Case Rep. 2017, 7, 6. [Google Scholar] [CrossRef]
- Seller, K.; Haas, S.; Raab, P.; Krauspe, R.; Wild, A. A Preoperative halo-traction in severe paralytic scoliosis. Z. Fur Orthop. Und Ihre Grenzgeb. 2005, 143, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Herdea, A.; Stancu, T.A.; Ulici, A.; Lungu, C.N.; Dragomirescu, M.-C.; Charkaoui, A. Quality of Life Evaluation Using SRS-30 Score for Operated Children and Adolescent Idiopathic Scoliosis. Medicina 2022, 58, 674. [Google Scholar] [CrossRef]
- McIntosh, A.L.; Ramo, B.S.; Johnston, C.E. Halo Gravity Traction for Severe Pediatric Spinal Deformity: A Clinical Concepts Review. Spine Deform. 2019, 7, 395–403. [Google Scholar] [CrossRef]
- Barrueto, K.S.; Prigent, N.Q.; Py, A.; LeMenager, F.; Chamberon, M.; Coll, C.; Finidori, G.; Vialle, R.; Ilharreborde, B. Benefits and complications of halo-gravity traction in adolescents with severe idiopathic or secondary scoliosis prior to vertebral fusion. Series of 16 cases. Ann. Phys. Rehabil. Med. 2018, 61, e330–e331. [Google Scholar] [CrossRef]
- Murray, R.J. Respiratory Manifestations of Extrapulmonary Disorders; Elsevier Saunders: Philadelphia, PA, USA, 2007. [Google Scholar]
- Nickel, V.L.; Perry, J.; Garrett, A.; Heppenstall, M. The halo: A spinal skeletal traction fixation device. J. Bone Jt. Surg. 1968, 50, 1400–1409. [Google Scholar] [CrossRef]
- Stagnara, P. Cranial traction using the “Halo” of Rancho Los Amigos. Rev. Chir. Orthop. Reparatrice L’appareil Mot. 1971, 57, 287–300. [Google Scholar]
- Caubet, J.-F.; Emans, J.B. Halo-Gravity Traction Versus Surgical Release Before Implantation of Expandable Spinal Devices. J. Spinal Disord. Tech. 2011, 24, 99–104. [Google Scholar] [CrossRef]
- Rinella, A.; Lenke, L.; Whitaker, C.; Kim, Y.; Park, S.-S.; Peelle, M.; Edwards, C.; Bridwell, K. Perioperative Halo-Gravity Traction in the Treatment of Severe Scoliosis and Kyphosis. Spine 2005, 30, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Sponseller, P.D.; Takenaga, R.K.; Newton, P.; Boachie, O.; Flynn, J.; Letko, L.; Betz, R.; Bridwell, K.; Gupta, M.; Marks, M.; et al. The use of traction in the treatment of severe spinal deformity. Spine 2008, 33, 2305–2309. [Google Scholar] [CrossRef] [PubMed]
- Letts, R.M.; Palakar, G.; Bobecko, W.P. Preoperative skeletal traction in scoliosis. J. Bone Jt. Surg. 1975, 57, 616–619. [Google Scholar] [CrossRef]
- Gonzalez, C.; Ferris, G.; Diaz, J.; Fontana, I.; Nunez, J.; Marín, J. Kyphoscoliotic ventilatory insufficiency: Effects of longterm intermittent positive-pressure ventilation. Chest 2003, 124, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Zenner, J.; Gajic, V.; Meier, O.; Ferraris, L.; Hitzl, W. The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: A clinical study and narrative review of the literature. Eur. Spine J. 2011, 21, 514–529. [Google Scholar] [CrossRef]
- Park, D.K.; Braaksma, B.; Hammerberg, K.W.; Sturm, P. The efficacy of preoperative halo-gravity traction in pediatric spinal deformity: The effect of traction duration. Clin. Spine Surg. 2013, 26, 146–154. [Google Scholar] [CrossRef]
- Bogunovic, L.; Lenke, L.G.; Bridwell, K.H.; Luhmann, S.J. Preoperative Halo-Gravity Traction for Severe Pediatric Spinal Deformity: Complications, Radiographic Correction and Changes in Pulmonary Function. Spine Deform. 2013, 1, 33–39. [Google Scholar] [CrossRef]
- Rocos, B.; Reda, L.; Lebel, D.E.; Dodds, M.K.; Zeller, R. The Use of Halo Gravity Traction in Severe, Stiff Scoliosis. J. Pediatr. Orthop. 2021, 41, 338–343. [Google Scholar] [CrossRef]
- Hwang, C.J.; Kim, D.G.; Lee, C.S.; Lee, D.-H.; Cho, J.H.; Park, J.-W.; Baik, J.M.; Lee, K.B. Preoperative Halo Traction for Severe Scoliosis. Spine 2020, 45, E1158–E1165. [Google Scholar] [CrossRef]
- Garabekyan, T.; Hosseinzadeh, P.; Iwinski, H.J.; Muchow, R.D.; Talwalkar, V.R.; Walker, J.; Milbrandt, T.A. The results of preoperative halo-gravity traction in children with severe spinal deformity. J. Pediatr. Orthop. B 2014, 23, 1–5. [Google Scholar] [CrossRef]
- Iyer, S.; Duah, H.O.; Wulff, I.; Tutu, H.O.; Mahmud, R.; Yankey, K.P.; Akoto, H.; Boachie-Adjei, O. The Use of Halo Gravity Traction in the Treatment of Severe Early Onset Spinal Deformity. Spine 2019, 44, E841–E845. [Google Scholar] [CrossRef] [PubMed]








| Variable | Study Group (n = 19) |
|---|---|
| Age (years) | 14.16 * ± 2.46 ** (range 9–17) |
| Gender n, (%) | |
| Males | 6 (31.6) |
| Females | 13 (68.4) |
| Body Weight | 48.89 * ±9.83 ** (range 25–63) |
| Traction duration (days) | 28.46 * ±7.86 ** (range 17–43) |
| Traction weight (Kg) | 20.11 * ±2.54 ** (range 12–22) |
| Variable | Study Group |
|---|---|
| Main curve localisation n, (%) | |
| Thoracic | 10 (52.63) |
| Lumbar | 1 (5.26) |
| Thoraco-lumbar | 8 (42.11) |
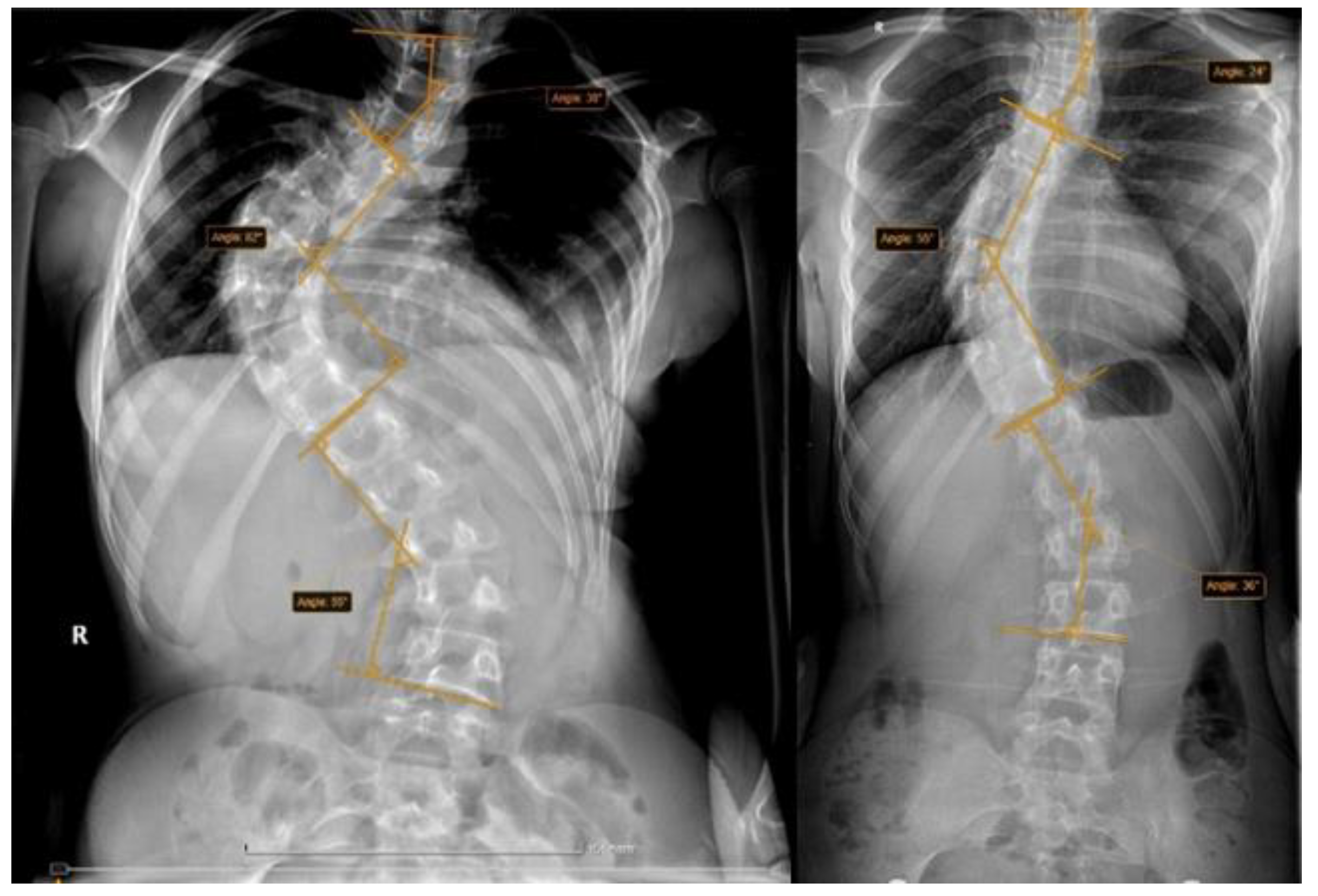
| Cobb angle before traction (degrees) Mean ± Standard deviation | 86.21 ±13.88 (range 66–115) |
| Cobb angle pre-operative (degrees) Mean ± Standard deviation | 63.16 ± 10.27 (range 47–85) |
| Vertebral rotation n, (%) | |
| ++ | 8 (42.1) |
| +++ | 9 (47.4) |
| ++++ | 2 (10.5) |
| Risser sign n, (%) | |
| 0 | 3 (15.8) |
| 1 | 2 (10.5) |
| 2 | 1 (5.3) |
| 3 | 4 (21.2) |
| 4 | 8 (42.1) |
| 5 | 1 (5.3) |
| Variable n, (%) | Study Group |
|---|---|
| Curve type | |
| 1 | 7 (36.8) |
| 2 | 1 (5.3) |
| 3 | 8 (42.1) |
| 5 | 2 (10.5) |
| 6 | 1 (5.3) |
| Lumbar spine modifier | |
| A | 9 (47.4) |
| B | 7 (36.8) |
| C | 3 (15.8) |
| Thoracic sagittal Profile | |
| Normal | 14 (73.7) |
| + | 2 (10.5) |
| - | 3 (15.8) |
| Variable n, (%) | Study Group (n = 19) |
|---|---|
| Complication occurrence | 18 (94.7) |
| Cervical pain | 17 (89.5) |
| Back pain | 7 (36.8) |
| Neurological symptoms | 5 (26.3) |
| Headache | 2 (10.5) |
| Vertigo | 1 (5.3) |
| Pin pain | 5 (26.3) |
| Pin infection | 5 (26.3) |
| Pin displacement | 1 (5.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, M.B.; Ulici, A.; Carp, M.; Haram, O.; Ionescu, N.S. The Use and Complications of Halo Gravity Traction in Children with Scoliosis. Children 2022, 9, 1701. https://doi.org/10.3390/children9111701
Popescu MB, Ulici A, Carp M, Haram O, Ionescu NS. The Use and Complications of Halo Gravity Traction in Children with Scoliosis. Children. 2022; 9(11):1701. https://doi.org/10.3390/children9111701
Chicago/Turabian StylePopescu, Mihai B., Alexandru Ulici, Madalina Carp, Oana Haram, and Nicolae S. Ionescu. 2022. "The Use and Complications of Halo Gravity Traction in Children with Scoliosis" Children 9, no. 11: 1701. https://doi.org/10.3390/children9111701
APA StylePopescu, M. B., Ulici, A., Carp, M., Haram, O., & Ionescu, N. S. (2022). The Use and Complications of Halo Gravity Traction in Children with Scoliosis. Children, 9(11), 1701. https://doi.org/10.3390/children9111701







