Parental Knowledge about Allergies and Problems with an Elimination Diet in Children Aged 3 to 6 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Analysis
3. Results
3.1. General Characteristics of the Study Group
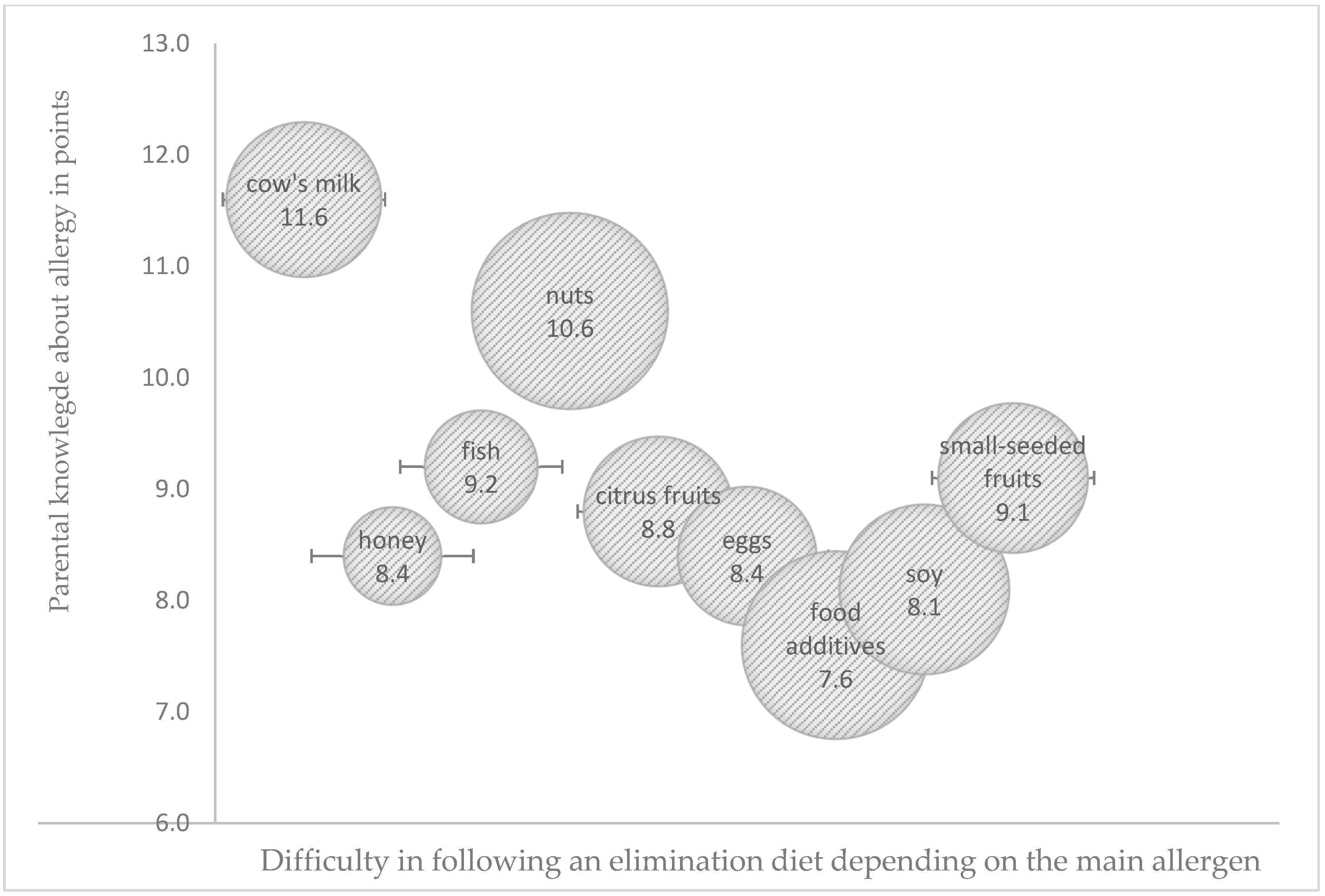
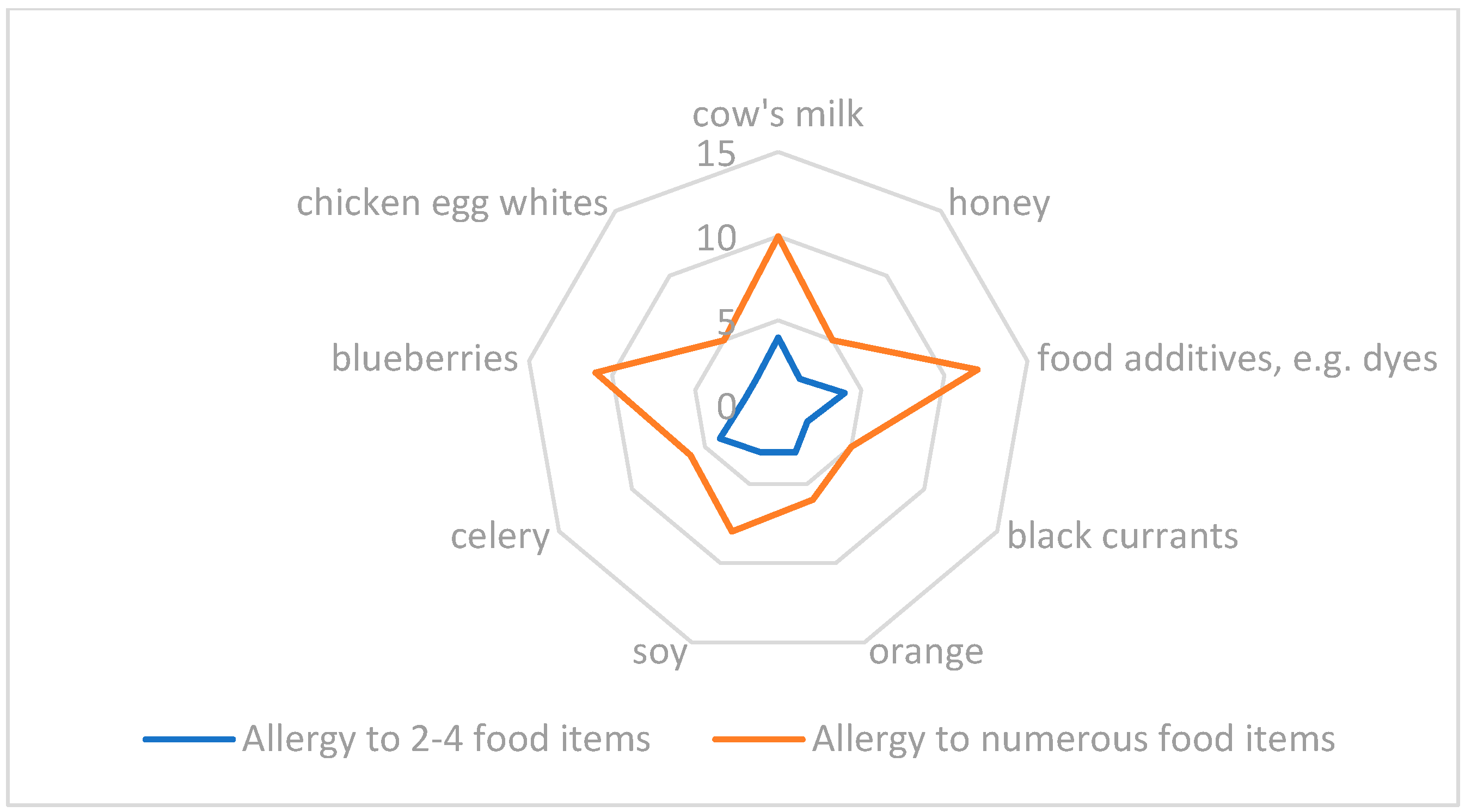
3.2. Parental Knowledge about Allergy Management
3.3. Problems with Adherence to an Elimination Diet in Food Allergies
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aleraj, B.; Tomić, B. Epidemiologija alergijskih bolesti [Epidemiology of allergic diseases]. Acta Med. Croat. 2011, 65, 147–153. [Google Scholar]
- Doll, R.J.; Joseph, N.I.; McGarry, D.; Jhaveri, D.; Sher, T.; Hostoffer, R. Epidemiology of Allergic Diseases; Mahmoudi, M., Ed.; Allergy and Asthma; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Johansson, S.G.; Hourihane, J.O.; Bousquet, J.; Bruijnzeel-Koomen, C.; Dreborg, S.; Haahtela, T.; Kowalski, M.L.; Mygind, N.; Ring, J.; van Cauwenberge, P.; et al. EAACI (the European Academy of Allergology and Cinical Immunology) nomenclature task force. A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy 2001, 56, 813–824, Erratum in Allergy 2001, 56, 1229. [Google Scholar] [CrossRef] [PubMed]
- Antó, J.M.; Pinart, M.; Akdis, M.; Auffray, C.; Bachert, C.; Basagaña, X.; Carlsen, K.H.; Guerra, S.; von Hertzen, L.; Illi, S.; et al. Understanding the complexity of IgE-related phenotypes from childhood to young adulthood: A Mechanisms of the Development of Allergy (MeDALL) seminar. J. Allergy Clin. Immunol. 2012, 129, 943–954. [Google Scholar] [CrossRef] [PubMed]
- Alduraywish, S.A.; Lodge, C.J.; Campbell, B.; Allen, K.J.; Erbas, B.; Lowe, A.J.; Dharmage, S.C. The march from early life food sensitization to allergic disease: A systematic review and meta-analyses of birth cohort studies. Allergy 2016, 71, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, S.F. Epidemiology and natural history of atopic diseases. Eur. Clin. Respir. J. 2015, 24, 24642. [Google Scholar] [CrossRef]
- Liebhard, J.; Małolepszy, J.; Wojtyniak, B.; Pisiewicz, K.; Plusa, T.; Gladysz, U. Polish multicentre study of epidemiology of allergic diseases. Prevalence and risk factors for asthma in Poland: Results from the PMSEAD study. J. Investig. Allergol. Clin. Immunol. 2007, 17, 367–374. [Google Scholar]
- Samoliński, B.; Raciborski, F.; Lipiec, A.; Tomaszewska, A.; Krzych-Fałta, E.; Samel-Kowalik, P.; Walkiewicz, A.; Lusawa, A.; Borowicz, J.; Komorowski, J.; et al. Epidemiologia chorób alergicznych w Polsce (ECAP). Pol. J. Allergol. 2014, 1, 10–18. [Google Scholar] [CrossRef]
- Horvath, A.; Krawiec, M.; Jarocka-Cytra, E.; Zawadzka-Krajewska, A.; Rachtan-Janicka, J.; Zakościelny, K.; Dziechciarz, P. Allergy-focused Diet History-Polish version of the European Academy of allergy and clinical Immunology tool. Stand. Med. Pediatr. 2018, 15, 25–45. (In Polish) [Google Scholar]
- Asher, M.I.; Keil, U.; Anderson, H.R.; Beasley, R.; Crane, J.; Martinez, F.; Mitchell, E.A.; Pearce, N.; Sibbald, B.; Stewart, A.W.; et al. International Study of Asthma and Allergies in Childhood (ISAAC): Rationale and methods. Eur. Respir. J. 1995, 8, 483–491. [Google Scholar] [CrossRef]
- Jezewska-Zychowicz, M.; Gawecki, J.; Wadolowska, L.; Czarnocinska, J.; Galinski, G.; Kollajtis-Dolowy, A.; Roszkowski, W.; Wawrzyniak, A.; Przybylowicz, K.; Stasiewicz, B. KomPAN® Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data, 2nd ed.; Committee of Human Nutrition; Polish Academy of Sciences: Warsaw, Poland, 2020. [Google Scholar]
- Kowalkowska, J.; Wadolowska, L.; Hamulka, J.; Wojtas, N.; Czlapka-Matyasik, M.; Kozirok, W.; Bronkowska, M.; Sadowska, J.; Naliwajko, S.; Dziaduch, I.; et al. Reproducibility of a Short-Form, Multicomponent Dietary Questionnaire to Assess Food Frequency Consumption, Nutrition Knowledge, and Lifestyle (SF-FFQ4PolishChildren) in Polish Children and Adolescents. Nutrients 2019, 11, 2929. [Google Scholar] [CrossRef]
- Koletzko, S.; Niggemann, B.; Arato, A.; Dias, J.A.; Heuschkel, R.; Husby, S.; Mearin, M.L.; Papadopoulou, A.; Ruemmele, F.M.; Staiano, A.; et al. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.S.; Springston, E.E.; Warrier, M.R.; Smith, B.; Kumar, R.; Pongracic, J.; Holl, J.L. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 2011, 128, e9–e17. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Ahn, S.S.; Sicherer, S.H. Prevalence of allergy to multiple versus single foods in a pediatric food allergy referral practice. J. Allergy Clin. Immunol. 2010, 125, AB216. [Google Scholar] [CrossRef]
- Howe, L.; Franxman, T.; Teich, E.; Greenhawt, M. What affects quality of life among caregivers of food-allergic children? Ann. Allery Asthma Immunol. 2014, 113, 69–74. [Google Scholar] [CrossRef]
- Ward, C.E.; Greenhawt, M. Treatment of allergic reactions and quality of life among caregivers of food-allergic children. Ann. Allergy Asthma Immunol. 2015, 114, 312–318. [Google Scholar] [CrossRef]
- Birdi, G.; Cooke, R.; Knibb, R. Quality of Life, Stress, and Mental Health in Parents of Children with Parentally Diagnosed Food Allergy Compared to Medically Diagnosed and Healthy Controls. J. Allergy 2016, 1497375. [Google Scholar] [CrossRef]
- Morou, Z.; Tatsioni, A.; Dimoliatis, I.D.K.; Papadopoulos, N.G. Health-related quality of life in children with food allergy and their parents: A systematic review of the literature. J. Investig. Allergol. Clin. Immunol. 2014, 24, 382–397. [Google Scholar]
- Abrams, E.M.; Kim, H.; Gerdts, J.; Protudjer, J.L.P. Milk allergy most burdensome in multi-food allergic children. Pediatr. Allergy Immunol. 2020, 31, 827–834. [Google Scholar] [CrossRef]
- Boaventura, R.M.; Mendonca, R.B.; Fonseca, F.A.; Mallozi, M.; Souza, F.S.; Sarni, R.O.S. Nutritional status and food intake of children with cow’s milk allergy. Allergol. Immunopathol. 2019, 47, 30048–30055. [Google Scholar] [CrossRef]
- Foong, R.X.; Santos, A.F. Biomarkers of diagnosis and resolution of food allergy. Pediatr. Allergy Immunol. 2021, 32, 223–233. [Google Scholar] [CrossRef]
- Calvani, M.; Bianchi, A.; Reginelli, C.; Peresso, M.; Testa, A. Oral Food Challenge. Medicina 2019, 55, 651. [Google Scholar] [CrossRef] [PubMed]
- Grabenhenrich, L.B.; Reich, A.; Bellach, J.; Trendelenburg, V.; Sprikkelman, A.B.; Roberts, G.; Grimshaw, K.E.; Sigurdardottir, S.; Kowalski, M.L.; Papadopoulos, N.G.; et al. A new framework for the documentation and interpretation of oral food challenges in population-base and clinical research. Allergy 2017, 72, 453–461. [Google Scholar] [CrossRef]
- Eigenmann, P.; Atanaskovic-Markovic, M.; Hourihane, J.O.; Lack, G.; Lau, S.; Matricardi, P.M.; Muraro, A.; Baranova, L.N.; Nieto, A.; Papadopoulos, N.G.; et al. Testing children for allergies: Why, how, who and when. Pediatr. Allergy Immunol. 2013, 24, 195–209. [Google Scholar] [CrossRef]
- Sampson, H.A.; Van Wijk, R.G.; Bindslev-Jensen, C.; Sicherer, S.H.; Teuber, S.S.; Burks, A.W.; Dubois, A.E.; Beyer, K.; Eigenmann, P.A.; Spergel, J.M.; et al. Standardizing double-blind, placebo-controlled oral food challenges: American Academy of Allergy, Asthma & Immunology—European Academy of Allergy and Clinical Immunology PRACTALL consensus report. J. Allergy Clin. Immunol. 2012, 130, 1260–1274. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.N.C.; Adel-Patient, K.; Bernard, H.; De Loose, M.; Gillard, N.; Huet, A.C.; Larré, C.; Nitride, C.; Pilolli, R.; Tranquet, O.; et al. Detection and Quantification of Allergens in Foods and Minimum Eliciting Doses in Food-Allergic Individuals (ThRAll). J. AOAC Int. 2019, 102, 1346–1353. [Google Scholar] [CrossRef] [PubMed]
- Kok, M.; Compagner, A.; Panneman, I.; Sprikkelman, A.; Vlieg-Boerstra, B. A Food, a Bite, a Sip: How Much Allergen Is in That? Nutrients 2021, 3, 587. [Google Scholar] [CrossRef]
- Muraro, A.; Werfel, T.; Hoffmann-Sommergruber, K.; Roberts, G.A.; Beyer, K.; Bindslev-Jensen, C.; Cardona, V.; Dubois, A.; Dutoit, G.; Eigenmann, P.; et al. EAACI food allergy and anaphylaxis guidelines: Diagnosis and management of food allergy. Allergy 2014, 69, 1008–1025. [Google Scholar] [CrossRef]
- Alanne, S.; Laitinen, K.; Paavilainen, E. Living ordinary family life with an allergic child-the mother’s perspective. J. Pediatr. Nurs. 2014, 29, 679–687. [Google Scholar] [CrossRef]
- Bollinger, M.E.; Dahlquist, L.M.; Mudd, K.; Sonntag, C.; Dillinger, L.; McKenna, K. The impact of food allergy on the daily activities of children and their families. Ann. Allergy Asthma Immunol. 2006, 96, 415–421. [Google Scholar] [CrossRef]
- Annunziato, R.A.; Rubes, M.; Ambrose, M.A.; Mullarkey, C.; Shemesh, E.; Sicherer, S.H. Longitudinal evaluation of food allergy-related bullying. J. Allergy Clin. Immunol. Pract. 2014, 2, 639–641. [Google Scholar] [CrossRef]
- Knibb, R.C.; Semper, H. Impact of suspected food allergy on emotional distress and family life of parents prior to allergy diagnosis. Pediatr. Allergy Immunol. 2013, 24, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.; Godwin, H.; Dziubak, R.; Panepinto, J.A.; Foong, R.M.; Bryon, M.; Lozinsky, A.C.; Reeve, K.; Shah, N. The impact on quality of life on families of children on an elimination diet for Non-immunoglobulin E mediated gastrointestinal food allergies. World Allergy Organ. J. 2017, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Blackman, A.C.; Wang, H.T.; Anvari, S.; Joseph, M.; Davis, C.M.; Staggers, K.A.; Anagnostou, A. Quality of life in food allergic children: Results from 174 quality-of-life patient questionnaires. Ann. Allergy Asthma Immunol. 2020, 124, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Rouf, K.; White, L.; Evans, K. A qualitative investigation into the maternal experience of having a young child with severe food allergy. Clin. Child Psychol. Psychiatry 2012, 17, 49–64. [Google Scholar] [CrossRef]
- Weber, T.K.; Speridiao, P.G.; Sdepanian, V.L.; Neto, U.F.; De Morais, M.B. The performance of parents of children receiving cow’s milk free diets at identification of commercial food products with and without cow’s milk. J. Pediatr. 2007, 83, 459–464. [Google Scholar] [CrossRef]
- Gupta, R.S.; Kim, J.S.; Springston, E.E.; Pongracic, J.; Wang, J.; Holl, J.A. Development of the Chicago Food Allergy Research Surveys: Assessing food allergy knowledge, attitudes, and beliefs of parents, physicians, and the general public. BMC Health Serv. Res. 2009, 9, 142. [Google Scholar] [CrossRef]
- Arkwright, P.D.; Farragher, A.J. Factors determining the ability of parents to effectively administer intramuscular adrenaline to food allergic children. Pediatr. Allergy Immunol. 2006, 17, 227–229. [Google Scholar] [CrossRef]
- Gupta, R.S.; Springston, E.E.; Smith, B.; Kim, J.S.; Pongracic, J.A.; Wang, X.; Holl, J. Food allergy knowledge, attitudes, and beliefs of parents with food-allergic children in the United States. Pediatr. Allergy Immunol. 2010, 21, 927–934. [Google Scholar] [CrossRef]
- Primeau, M.N.; Kagan, R.; Joseph, L.; Lim, H.; Dufresne, C.; Duffy, C.; Prhcal, D.; Clarke, A. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin. Exp. Allergy 2000, 30, 1135–1143. [Google Scholar] [CrossRef]
- Akeson, N.; Worth, A.; Sheikh, A. The psychosocial impact of anaphylaxis on young people and their parents. Clin. Exp. Allergy 2007, 37, 1213–1220. [Google Scholar] [CrossRef]
- Cummings, A.J.; Knibb, R.C.; King, R.M.; Lucas, J.S. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: A review. Allergy 2010, 65, 933–945. [Google Scholar] [CrossRef] [PubMed]
- Calsbeek, H.; Rijken, M.; Bekkers, M.J.; Kerssens, J.J.; Dekker, J.; Van Berge Henegouwen, G.P. Social position of adolescents with chronic digestive disorders. Eur. J. Gastroenterol. Hepatol. 2002, 14, 543–549. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Calsbeek, H.; Rijken, M.; Bekkers, M.J.; Dekker, J.; Van Berge Henegouwen, G.P. School and leisure activities in adolescents and young adults with chronic digestive disorders: Impact of burden of disease. Int. J. Behav. Med. 2006, 13, 121–130. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Total | Gender | p | |
|---|---|---|---|---|
| Male n [%] | Female n [%] | |||
| Age | ||||
| 3–4 years | 93 | 44 [47.31%] | 49 [52.69%] | <0.05 |
| 5–6 years | 104 | 36 [34.61%] | 68 [65.39%] | <0.05 |
| Age at diagnosis (in months) | 9.4 ± 5.7 | 9.2 ± 5.5 | 9.7 ± 5.9 | >0.05 |
| Type of allergy * | ||||
| Food allergy, including: | 105 | 43 [40.9%] | 62 [59.1%] | <0.05 |
| Cow’s-milk protein | 46 | 21 [45.6%] | 25 [54.4%] | <0.05 |
| Chicken-egg whites | 29 | 10 [34.5%] | 19 [65.5%] | <0.05 |
| Soy | 23 | 11 [47.8%] | 12 [52.2%] | >0.05 |
| Small-seeded fruits | 22 | 13 [59.1%] | 9 [40.9%] | <0.05 |
| Citrus fruits | 20 | 14 [70%] | 6 [30%] | <0.05 |
| Nuts | 17 | 5 [29.4%] | 12 [70.6%] | <0.05 |
| Cacao | 15 | 7 [46.7%] | 8 [53.3%] | >0.05 |
| Honey | 11 | 3 [27.3%] | 8 [72.7%] | <0.05 |
| Food dyes | 10 | 7 [70%] | 3 [30%] | <0.05 |
| Celery | 6 | 4 [66.7%] | 2 [33.3%] | <0.05 |
| Fish | 6 | 3 [50%] | 3 [50%] | >0.05 |
| Inhaled (airborne) allergy, including: | 145 | 56 [38.8%] | 89 [61.2%] | <0.005 |
| House-dust mites | 91 | 44 [48.4%] | 47 [51.6%] | >0.05 |
| Birch pollen | 84 | 37 [44%] | 47 [56%] | <0.05 |
| Hazel pollen | 72 | 51 [70.8%] | 21 [29.2%] | <0.005 |
| Grass pollen | 70 | 37 [52.9%] | 33 [47.1%] | >0.05 |
| Mugwort pollen | 34 | 17 [50%] | 17 [50%] | >0.05 |
| Other | 56 | 24 [42.9%] | 32 [57.1%] | <0.05 |
| Contact dermatitis, including: | 58 | 21 [36.2%] | 37 [63.8%] | <0.005 |
| Dog or cat hair | 43 | 24 [55.8%] | 19 [44.2%] | <0.05 |
| Hair of other animals | 27 | 11 [40.7%] | 16 [59.3%] | <0.05 |
| Ears of cereals | 11 | 3 [27.3%] | 8 [72.7%] | <0.005 |
| Allergies in the family | ||||
| None | 57 | 19 [33.3%] | 38 [66.7%] | <0.005 |
| One parent | 54 | 27 [50%] | 27 [50%] | >0.05 |
| Both parents | 47 | 25 [53.2%] | 22 [46.8%] | >0.05 |
| Other family members | 39 | 9 [23.1%] | 30 [76.9%] | <0.005 |
| Child’s Age (Ref. 5–6 Years) 3–4 Years | Child’s Gender (Ref. Girls) Boys | Allergies in the Family (Ref. No Allergies in the Family) | Allergy Diagnosed by a Pediatrician or Other Specialist (Ref. Allergist) | Allergy Skin Test (Ref. Serology Test) | Applied Treatment—Steroids (Ref. Antihistamines) | |
|---|---|---|---|---|---|---|
| Contact dermatitis: skin redness, erythema, pruritus, urticaria, eczema | 1.45 * (1.24–1.77) | 1.12 (1.03–1.29) | 1.04 (0.96–1.12) | 0.84 * (0.72–1.05) | 1.36 * (1.22–1.59) | 0.71 * (0.62–0.89) |
| Contact dermatitis: atopic dermatitis | 1.74 ** (1.33–1.89) | 1.07 (0.88–1.23) | 0.78 * (0.64–0.93) | 1.37 * (1.19–1.51) | 0.71 * (0.62–0.89) | 1.87 ** (1.42–2.06) |
| Oral allergy: itchiness or swelling of lips/tongue/throat, laryngeal edema, globus sensation | 1.07 (0.96–1.27) | 0.94 (0.88–1.07) | 1.11 (1.02–1.26) | 1.10 (1.01–1.24) | 0.75 * (0.67–0.91) | 0.63 ** (0.51–0.83) |
| Gastrointestinal allergy: abdominal pain, nausea, vomiting, diarrhea, gas, gastroesophageal reflux | 0.74 * (0.62–1.02) | 1.29 * (1.17–1.40) | 1.05 (0.99–1.17) | 1.14 (0.97–1.20) | 1.08 (0.94–1.20) | 0.47 ** (0.32–0.70) |
| Upper-respiratory-tract reactions: nasal pruritus, sneezing, nasal/postnasal drip, cough, hoarseness, tightness in the chest, wheezing, dyspnea | 1.11 (1.02–1.24) | 1.06 (0.94–1.18) | 1.39 * (1.26–1.57) | 1.84 ** (1.29–2.09) | 1.76 ** (1.54–1.89) | 1.57 ** (1.24–1.86) |
| Cardiovascular reactions: dizziness, hypotension, loss of consciousness | 1.03 (0.93–1.11) | 0.76 * (0.64–0.89) | 1.03 (0.92–1.14) | 1.77 ** (1.23–1.89) | 1.12 (0.96–1.34) | 1.05 (1.01–1.08) |
| Anaphylaxis | 0.72 * (0.65–0.91) | 1.18 (1.06–1.32) | 0.54 ** (0.41–0.76) | 1.34 * (1.11–1.45) | 0.71 * (058–0.88) | 1.02 (0.95–1.08) |
| Other: skin pallor, diaphoresis, fatigue, retarded growth, etc. | 1.04 (0.89–1.10) | 0.95 (0.82–1.11) | 1.03 (0.94–1.09) | 1.07 (0.91–1.15) | 1.09 (1.01–1.24) | 1.04 (0.91–1.12) |
| Total Sample | CHILD’S AGE | |||
|---|---|---|---|---|
| Parents of 3–4-Year-Olds | Parents of 5–6-Year-Olds | p | ||
| Mean score | 9.8 | 10.6 | 9.1 | * |
| Upper tertile | 49 | 27 | 22 | * |
| Middle tertile | 81 | 48 | 33 | * |
| Bottom tertile | 67 | 18 | 49 | ** |
| Allergy type | ||||
| Food | 10.5 | 11.2 | 9.6 | ** |
| Cow’s-milk protein | 10.9 | 11.7 | 9.3 | ** |
| Chicken-egg whites | 9.4 | 9.2 | 9.7 | |
| Inhaled | 9.7 | 9.2 | 9.9 | |
| House-dust mites | 9.5 | 9.3 | 9.7 | |
| Pollen of trees | 10.8 | 9.2 | 11.0 | ** |
| Contact dermatitis | 8.4 | 8.6 | 8.0 | * |
| Dog or cat hair | 8.5 | 8.3 | 8.6 | |
| Allergies in the family | ||||
| None | 7.8 | 7.6 | 8.1 | |
| One parent | 9.6 | 9.4 | 9.7 | |
| Both parents | 11.8 | 12.4 | 11.1 | ** |
| Other family members | 9.7 | 9.1 | 10.6 | ** |
| Children’s age at diagnosis (in months) | ||||
| Under 6 months | 11.3 | 11.9 | 10.7 | * |
| Over 6 months | 9.7 | 10.4 | 9.5 | * |
| Parental age | ||||
| <35 years | 9.7 | 10.2 | 9.1 | * |
| >35 years | 9.9 | 10.5 | 9.4 | * |
| Parental education | ||||
| Primary/vocational | 7.6 | 7.4 | 7.6 | |
| Secondary | 8.5 | 8.7 | 8.3 | |
| University | 11.6 | 12.7 | 11.1 | ** |
| Employment | ||||
| Unemployed/on prolonged leave | 9.1 | 9.3 | 9.0 | |
| Employed | 10.5 | 11.2 | 10.3 | * |
| Allergy to 1 Food Item | Allergy to 2–4 Food Items | Allergy to Numerous Food Items | |
|---|---|---|---|
| Allergenic foods were eliminated from the diet for more than 6 months (ref. for 3 months or less). | 1.08 (0.84–1.19) | 1.39 * (1.20–1.54) | 1.89 ** (1.33–2.19) |
| The elimination diet was recommended by a pediatrician and consulted with a dietician (ref. the elimination diet was recommended by a pediatrician, but not consulted with a dietician). | 1.02 (0.89–1.16) | 1.13 (1.02–1.24) | 1.36 * (1.11–1.57) |
| Allergenic foods were replaced with safe substitutes to minimize the loss of nutrients (ref. safe substitutes were not used). | 1.09 (1.01–1.23) | 0.81 * (0.67–0.96) | 1.54 * (1.39–1.78) |
| When shopping for food, I always read food allergen labels (ref. I sporadically read food allergen labels). | 1.13 (0.97–1.24) | 1.36 * (1.09–1.57) | 1.79 ** (1.41–2.27) |
| I always buy a different product if a given food product contains allergenic ingredients (ref. I sporadically buy other food products). | 074 * (0.63–0.91) | 1.05 (0.93–1.27) | 1.38 * (1.22–1.59) |
| I often buy food products that may contain trace amounts of allergenic ingredients (ref. I never buy such products). | 1.04 (0.93–1.15) | 1.30 * (1.19–1.43) | 0.51 ** (0.41–0.72) |
| Frequent consumption of small amounts of allergenic foods does not pose a health threat (ref. both sporadic and frequent consumption of allergenic foods is dangerous for the child). | 1.37 * (1.15–1.49) | 1.08 (1.01–1.14) | 1.14 (1.03–1.26) |
| Parental Education—Primary Education (Ref. University Education) | Parental Age—>35 Years (Ref. <35 Years) | Allergies in the Family (Ref. No Allergies in the Immediate Family) | Parental Knowledge—Parents in the Bottom Tertile (Ref. Parents in the Upper Tertile) | |
|---|---|---|---|---|
| The elimination diet was recommended by a pediatrician and consulted with a dietician. | 0.59 ** (0.51–0.68) | 1.07 (0.96–1.11) | 1.03 (0.94–1.14) | 0.74 * (0.69–0.93) |
| Allergenic foods are replaced with safe substitutes to minimize the loss of nutrients. | 1.34 * (1.27–1.56) | 1.09 (1.01–1.17) | 0.91 (0.82–1.04) | 1.49 * (1.23–1.65) |
| When shopping for food, I always read food allergen labels. | 0.77 * (0.54–0.91) | 1.39 * (1.21–1.56) | 0.96 (0.84–1.07) | 1.31 * (1.25–1.48) |
| I sporadically buy other food products than those with listed ingredients. | 1.21 * (1.03–1.37) | 1.11 (0.94–1.27) | 0.82 * (0.73–0.97) | 1.13 (0.94–1.21) |
| I often buy food products that may contain trace amounts of allergenic ingredients. | 1.11 (0.95–1.28) | 1.27 * (1.12–1.42) | 1.04 (0.92–1.23) | 0.74 * (0.61–0.93) |
| Foods consumed outside the home setting are not safe because they often contain allergens. | 1.54 * (1.27–1.87) | 1.14 (0.96–1.27) | 0.92 (0.76–1.09) | 1.76 ** (1.54–1.89) |
| Both sporadic and frequent consumption of allergens is dangerous for the child. | 0.88 (0.69–1.04) | 0.76 * (0.61–0.95) | 1.09 (0.91–1.25) | 0.59 ** (0.41–0.78) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kostecka, M.; Kostecka-Jarecka, J.; Kostecka, J.; Iłowiecka, K.; Kolasa, K.; Gutowska, G.; Sawic, M. Parental Knowledge about Allergies and Problems with an Elimination Diet in Children Aged 3 to 6 Years. Children 2022, 9, 1693. https://doi.org/10.3390/children9111693
Kostecka M, Kostecka-Jarecka J, Kostecka J, Iłowiecka K, Kolasa K, Gutowska G, Sawic M. Parental Knowledge about Allergies and Problems with an Elimination Diet in Children Aged 3 to 6 Years. Children. 2022; 9(11):1693. https://doi.org/10.3390/children9111693
Chicago/Turabian StyleKostecka, Malgorzata, Joanna Kostecka-Jarecka, Julianna Kostecka, Katarzyna Iłowiecka, Katarzyna Kolasa, Gabriela Gutowska, and Magdalena Sawic. 2022. "Parental Knowledge about Allergies and Problems with an Elimination Diet in Children Aged 3 to 6 Years" Children 9, no. 11: 1693. https://doi.org/10.3390/children9111693
APA StyleKostecka, M., Kostecka-Jarecka, J., Kostecka, J., Iłowiecka, K., Kolasa, K., Gutowska, G., & Sawic, M. (2022). Parental Knowledge about Allergies and Problems with an Elimination Diet in Children Aged 3 to 6 Years. Children, 9(11), 1693. https://doi.org/10.3390/children9111693









