Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Selection Criteria
2.2.1. Type of Study
2.2.2. Population
2.2.3. Interventions
2.2.4. Comparator(s)
2.2.5. Outcomes
- The average worst Cobb angle before and after treatment;
- The percentage of patients with improvements (reduction in the Cobb angle >5°), progression (increase >5°), or stability (±5°);
- The percentage of patients with curves larger than 45°;
- The percentage of patients with curves larger than 50°;
- The percentage of surgically treated patients.
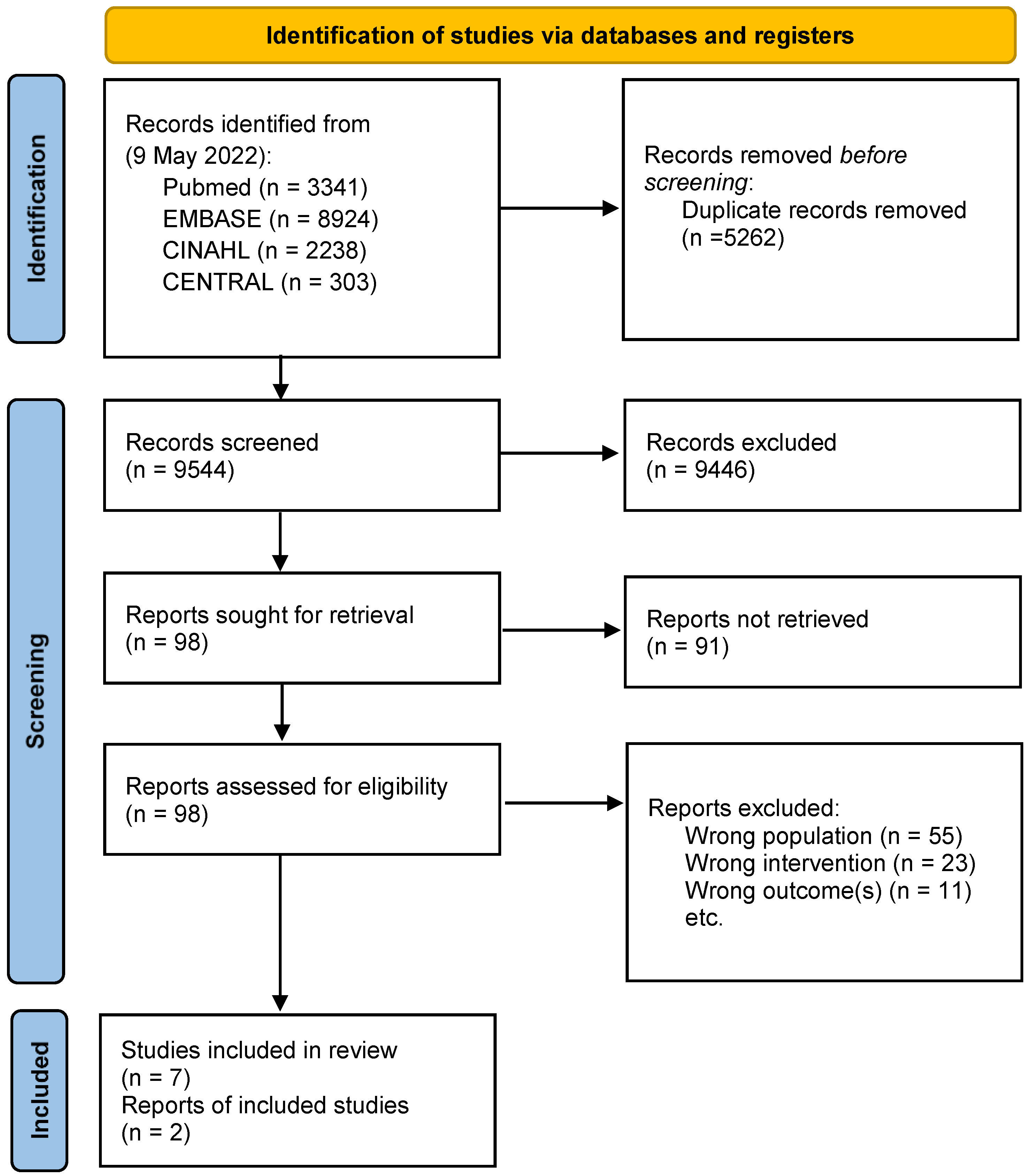
2.3. The Search Strategy and Screening
2.4. Assessment of Risk of Bias and Critical Appraisal in Included Studies
- -
- NRCTs: if it is clear in the study what is the ‘cause’ and what is the ‘effect’; if the participants included in any comparisons were similar; if the participants included in any comparisons received a similar treatment/care, other than the exposure or intervention of interest; if there was a control group; if there were multiple measurements of the outcome both pre- and post-intervention/exposure; if the follow-up was complete and, if not, if differences between the groups in terms of their follow-up were adequately described and analyzed; if the outcomes of the participants included in any comparisons were measured in the same way; if the outcomes were measured in a reliable way; and finally if an appropriate statistical analysis was used.
- -
- Observational studies: if the two groups were similar and recruited from the same population; if the exposures were measured similarly to assign people to both the exposed and unexposed groups; if the exposure was measured in a valid and reliable way; if confounding factors were identified; if strategies to deal with the confounding factors were stated; if the groups/participants were free of the outcome at the start of the study (or at the moment of exposure); if the outcomes were measured in a valid and reliable way; if the follow-up time was reported and sufficient to be long enough for the outcomes to occur; if the follow-up was complete, and if not, were the reasons for the lack of a follow-up described and explored; if strategies to address the incomplete follow-up were utilized; and if the appropriate statistical analysis was used?
- -
- Case series: if there were clear criteria for the participants’ inclusion; if the condition was measured in a standard, reliable way for all the participants included; if valid methods were used for the identification of the condition for all the participants included; if the case series had a consecutive inclusion of the participants; if the case series had completed the inclusion of participants; if there was a clear reporting of the demographics of the participants; if there was a clear reporting of the clinical information of the participants; if the outcomes or a follow-up to the results were clearly reported; if there was a clear reporting of the presenting site(s)/clinic(s) demographic information; and if the statistical analysis was appropriate.
2.5. Summary of Findings and Assessment of the Certainty of the Evidence
- Report characteristics (year, author, title, DOI, country, and aim).
- Study design (groups and the number of participants).
- Characteristics of the intervention (description of the intervention, frequency, and duration).
- Comparator characteristics (description of intervention, frequency, and duration).
- Outcomes assessed and measures (type of outcomes and how outcomes are measured).
- Numerical data for the outcomes of interest (effect size between groups, statistically significance).
3. Results
Assessment of Risk of Bias and Critical Appraisal in Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategies
| PubMed (via pubmed-ncbi.nlm.nih.gov/ (accessed on 9 May 2022)) |
|
| Embase (via Embase.com (accessed on 9 May 2022)) |
|
| CINAHL (via EBSCOhost (accessed on 9 May 2022)) |
|
| CENTRAL (Via Cochrane Library) |
|
References
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Di Felice, F.; Zaina, F.; Donzelli, S.; Negrini, S. The Natural History of Idiopathic Scoliosis during Growth: A Meta-Analysis. Am. J. Phys. Med. Rehabil. 2018, 97, 346–356. [Google Scholar] [CrossRef]
- Hresko, M.T. Clinical practice. Idiopathic Scoliosis in Adolescents. N. Engl. J. Med. 2013, 368, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L. The Natural History of Adolescent Idiopathic Scoliosis. J. Pediatr. Orthop. 2019, 39, S44–S46. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Cerny, P.; de Mauroy, J.C.; McAviney, J.; Mills, A.; Donzelli, S.; Grivas, T.B.; Hresko, M.T.; Kotwicki, T.; et al. The classification of scoliosis braces developed by SOSORT with SRS, ISPO, and POSNA and approved by ESPRM. Eur. Spine J. 2022, 31, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Adolescent Idiopathic Scoliosis | Scoliosis Research Society. Available online: https://www.srs.org/professionals/online-education-and-resources/conditions-and-treatments/adolescent-idiopathic-scoliosis (accessed on 29 August 2022).
- De Kleuver, M.; Lewis, S.J.; Germscheid, N.M.; Kamper, S.J.; Alanay, A.; Berven, S.H.; Cheung, K.M.; Ito, M.; Lenke, L.G.; Polly, D.W.; et al. Optimal surgical care for adolescent idiopathic scoliosis: An international consensus. Eur. Spine J. 2014, 23, 2603–2618. [Google Scholar] [CrossRef]
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Zaina, F. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst. Rev. 2015, 18, CD006850. [Google Scholar] [CrossRef]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of Criteria for Adolescent Idiopathic Scoliosis Brace Studies: SRS Committee on Bracing and Nonoperative Management. Spine 2005, 30, 2068–2075, discussion 2076–2077. [Google Scholar] [CrossRef]
- Negrini, S.; Boards, S.; Hresko, T.M.; O’Brien, J.P.; Price, N.; SOSORT Boards; SRS Non-Operative Committee Recommendations for Research Studies on Treatment of Idiopathic Scoliosis. Consensus 2014 between SOSORT and SRS non–operative management committee. Scoliosis 2015, 10, 8. [Google Scholar] [CrossRef]
- Carr, W.A.; Moe, J.H.; Winter, R.B.; Lonstein, J.E. Treatment of idiopathic scoliosis in the Milwaukee brace. J. Bone Jt. Surg. 1980, 62, 599–612. [Google Scholar] [CrossRef]
- Roye, B.D.; Simhon, M.E.; Matsumoto, H.; Bakarania, P.; Berdishevsky, H.; Dolan, L.A.; Grimes, K.; Grivas, T.B.; Hresko, M.T.; Karol, L.A.; et al. Establishing consensus on the best practice guidelines for the use of bracing in adolescent idiopathic scoliosis. Spine Deform. 2020, 8, 597–604. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Akl, E.; Altman, D.; Aluko, P.; Askie, L.; Beaton, D.; Berlin, J.; Bhaumik, B.; Bingham, C.; Boers, M.; Booth, A.; et al. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons Ltd.: Oxford, UK, 2019; ISBN 978-1-119-53660-4. [Google Scholar]
- Critical Appraisal Tools | JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 29 August 2022).
- Verhofste, B.P.; Whitaker, A.T.; Glotzbecker, M.P.; Miller, P.E.; Karlin, L.I.; Hedequist, D.J.; Emans, J.B.; Hresko, M.T. Efficacy of bracing in skeletally immature patients with moderate–severe idiopathic scoliosis curves between 40° and 60°. Spine Deform. 2020, 8, 911–920. [Google Scholar] [CrossRef]
- Xu, L.; Yang, X.; Wang, Y.; Wu, Z.; Xia, C.; Qiu, Y.; Zhu, Z. Brace Treatment in Adolescent Idiopathic Scoliosis Patients with Curve between 40° and 45°: Effectiveness and Related Factors. World Neurosurg. 2019, 126, e901–e906. [Google Scholar] [CrossRef]
- Zhu, Z.; Xu, L.; Jiang, L.; Sun, X.; Qiao, J.; Qian, B.-P.; Mao, S.; Qiu, Y. Is Brace Treatment Appropriate for Adolescent Idiopathic Scoliosis Patients Refusing Surgery with Cobb Angle between 40 and 50 Degrees. Clin. Spine Surg. 2017, 30, 85–89. [Google Scholar] [CrossRef]
- Negrini, S.; Negrini, F.; Fusco, C.; Zaina, F. Idiopathic scoliosis patients with curves more than 45 Cobb degrees refusing surgery can be effectively treated through bracing with curve improvements. Spine J. 2011, 11, 369–380. [Google Scholar] [CrossRef]
- Razeghinezhad, R.; Kamyab, M.; Babaee, T.; Ganjavian, M.S.; Bidari, S. The Effect of Brace Treatment on Large Curves of 40° to 55° in Adolescents with Idiopathic Scoliosis Who Have Avoided Surgery: A Retrospective Cohort Study. Neurospine 2021, 18, 437–444. [Google Scholar] [CrossRef]
- Karavidas, N. Complete Non-Operative Treatment with Brace and Scoliosis Specific Exercises Can Be Effective for Severe Scoliotic Curves Exceeding 40° at Peak of Growth. In Proceedings of the SOSORT International Congress, San Sebastian, Spain, 4–7 May 2022. [Google Scholar]
- Maruyama, T.; Kobayashi, Y.; Miura, M.; Nakao, Y. Outcomes of brace treatment for adolescent idiopathic scoliosis with curve magnitude of 41 to 50 degrees. Scoliosis 2014, 9, O22. [Google Scholar] [CrossRef][Green Version]
- Aulisa, A.G.; Guzzanti, V.; Falciglia, F.; Giordano, M.; Galli, M.; Aulisa, L. Brace treatment of Idiopathic Scoliosis is effective for a curve over 40 degrees, but is the evaluation of Cobb angle the only parameter for the indication of treatment? Eur. J. Phys. Rehabil. Med. 2019, 55, 231–240. [Google Scholar] [CrossRef]
- Lusini, M.; Donzelli, S.; Minnella, S.; Zaina, F.; Negrini, S. Brace treatment is effective in idiopathic scoliosis over 45°: An observational prospective cohort controlled study. Spine J. 2013, 14, 1951–1956. [Google Scholar] [CrossRef]
- Bunge, E.M.; Habbema, J.D.F.; de Koning, H.J. A Randomised Controlled Trial on the Effectiveness of Bracing Patients with Idiopathic Scoliosis: Failure to Include Patients and Lessons to Be Learnt. Eur. Spine J. 2010, 19, 747–753. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of Bracing in Adolescents with Idiopathic Scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef] [PubMed]
- Shaughnessy, W.J. Advances in Scoliosis Brace Treatment for Adolescent Idiopathic Scoliosis. Orthop. Clin. North Am. 2007, 38, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Di Felice, F.; Negrini, F.; Rebagliati, G.; Zaina, F.; Donzelli, S. Predicting final results of brace treatment of adolescents with idiopathic scoliosis: First out-of-brace radiograph is better than in-brace radiograph—SOSORT 2020 award winner. Eur. Spine J. 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Emans, J.B.; Kaelin, A.; Bancel, P.; Hall, J.E.; Miller, M.E. The Boston Bracing System for Idiopathic Scoliosis. Follow-up Results in 295 Patients. Spine 1986, 11, 792–801. [Google Scholar] [CrossRef]
- Edmonsson, A.S.; Morris, J.T. Follow-up study of Milwaukee brace treatment in patients with idiopathic scoliosis. Clin. Orthop. Relat. Res. 1977, 58–61. [Google Scholar] [CrossRef]
- Lange, J.E.; Steen, H.; Gunderson, R.; Brox, J.I. Long-term results after Boston brace treatment in late-onset juvenile and adolescent idiopathic scoliosis. Scoliosis 2011, 6, 18. [Google Scholar] [CrossRef]
- Danielsson, A.J.; Hallerman, K.L. Quality of Life in Middle-Aged Patients with Idiopathic Scoliosis with Onset before the Age of 10 Years. Spine Deform. 2015, 3, 440–450. [Google Scholar] [CrossRef]
- Schwieger, T.; Campo, S.; Weinsteiny, S.L.; Dolan, L.A.; Ashida, S.; Steuber, K.R. Body Image and Quality-of-Life in Untreated versus Brace-Treated Females with Adolescent Idiopathic Scoliosis. Spine 2016, 41, 311–319. [Google Scholar] [CrossRef]
- Tavernaro, M.; Pellegrini, A.; Tessadri, F.; Zaina, F.; Zonta, A.; Negrini, S. Team care to cure adolescents with braces (avoiding low quality of life, pain and bad compliance): A case-control retrospective study. 2011 SOSORT Award winner. Scoliosis 2012, 7, 17. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; Aldakhil, S.S.; Al-Rabiah, M.A.; Al-Rabiah, A.M. Surgical treatment of adolescent idiopathic scoliosis: Complications. Ann. Med. Surg. 2020, 52, 19–23. [Google Scholar] [CrossRef]
| Brace | N | Age | Sex (%F) | Risser | Baseline Cobb | Study | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Design | Ref | ||||||||||||
| Av | ± | Av | ± | Av | ± | Min | Max | ||||||
| Boston | 100 | 11.8 | 2.36 | 85 | 0.8 | 1.2 | 45 | 3.9 | 40 | 60 | RCS | Verhofste et al., 2020 [16] | |
| Boston | 90 | 12.6 | 1.3 | 84 | 1 | 1.2 | 42.5 | 2.1 | 40 | 45 | RCS | Xu et al., 2019 [17] | |
| Boston | 54 | 13.7 | 83 | 43.4 | 2.4 | RCS | Zhu et al., 2017 [18] | ||||||
| Milwaukee | |||||||||||||
| Lion | 28 | 14.2 | 86 | 49.4 | 3.8 | 45 | 48 | RC | Negrini et al., 2011 [19] | ||||
| Risser cast | |||||||||||||
| Sforzesco | |||||||||||||
| Milwaukee | 60 | 12.6 | 88 | 44.9 | 4.8 | RC | Razeghinezhad et al., 2021 [20] | ||||||
| Cheneau | 48 | 12.3 | 98 | 47 | 5.3 | PC | Karavitas et al., 2022 * [21] | ||||||
| Rigo Cheneau | 12 | 100 | 45 | 41 | 50 | PCS | Maruyama et al., 2014 * [22] | ||||||
| Lion | ITT | 132 | 47 | 5.3 | PC | Aulisa et al., 2018 [23] | |||||||
| PASB | EA | 104 | 12.9 | 93 | 47 | 5.3 | PC | Aulisa et al., 2018 [23] | |||||
| Sforzesco | ITT | 39 | 15.3 | 52.5 | 45 | 93 | PCC | Lusini et al., 2013 [24] | |||||
| EA | 34 | 81 | 52.5 | 45 | 93 | PCC | Lusini et al., 2013 [24] | ||||||
| Weighted means | |||||||||||||
| Total | 563 | 12.6 | 1.8 | 94 | 1.0 | 1.2 | 44.9 | 4.2 | |||||
| Retrospective studies | 332 | 12.7 | 1.8 | 85 | 1.1 | 1.2 | 44.4 | 3.4 | |||||
| Prospective studies EA | 198 | 10.5 | 1.8 | 93 | 0.7 | 0.8 | 47.8 | 5.3 | |||||
| Prospective studies ITT | 171 | 15 | 1.1 | 2 | 48.3 | 5.3 | |||||||
| Study (Case Series) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Verhofste 2020 [16] | + | + | + | + | + | − | + | + | + | + |
| Xu 2019 [17] | + | + | + | + | + | − | + | + | + | + |
| Study (observational studies) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Negrini 2011 [19] | + | + | + | − | − | + | + | + | − | − |
| Study (Non-randomized Controlled Trials) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| Lusini 2013 [24] | + | + | + | + | + | + | + | + | + | |
| Aulisa 2018 [23] | + | + | + | − | + | + | + | + | + |
| Brace | Cobb Angle Change (%) | Curves ≥ 45° (%) | Curves ≥ 50° (%) | Surgery (%) | Treatment Duration (Years) | Study | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||||||
| + | = | − | Av | ± | |||||||||
| Boston | 11 | 32 | 57 | 8 | 14.8 | 46 | 74 | 13 | 58 | 1.8 (1.2–1.9) * | Verhofste et al., 2020 | ||
| Boston | 13.3 | 37.8 | 48.9 | −0.4 | 8.9 | 2.4 (1.3) | Xu et al., 2019 | ||||||
| Boston | 14 | 22 | 64 | 1.8 | 9.8 | 0 | 2.3 (1.8-2.6) ** | Zhu et al., 2017 | |||||
| Milwaukee | |||||||||||||
| Lion | 71 | 25 | 4 | −9.25 | 8.04 | 100 | 32 | 43 | 7 | 0 | 4 (1.5-7.4) ** | Negrini et al., 2011 | |
| Risser cast | |||||||||||||
| Sforzesco | |||||||||||||
| Milwaukee | 18 | 25 | 57 | 2.36 | 11.6 | 13 | 40 | 52 | 3.1 (1.7) | Razeghinezhad et al., 2021 | |||
| Cheneau | 27.1 | 50 | 22.9 | Th: −2.5 | 77 | 60 | 54 | 44 | 3 | Karavitas et al., 2022 | |||
| L: −5.2 | |||||||||||||
| Rigo Cheneau | 0 | 50 | 5.3 | 42 | 0 | 50 | 25 | 3 | Maruyama et al., 2014 | ||||
| Lion | ITT | 61 | 11 | 28 | 5.3 (1.5) | Aulisa et al., 2018 | |||||||
| PASB | EA | 78 | 13 | 9 | −12.83 | 9.9 | 55 | 21 | 15 § | Aulisa et al., 2018 | |||
| Sforzesco | ITT | 54 | 13 | 33 | 100 | 38.5 | 15 ^ | 5.3 (1.1) | Lusini et al., 2013 | ||||
| EA | 62 | 15 | 23 | −10.4 | 10.7 | Lusini et al., 2013 | |||||||
| Weighted means | |||||||||||||
| Total | 31 | 27 | 42 | −1.83 | 64 | 47 | 24 | 36 | 29 | ||||
| Retrospective studies | 18 | 30 | 51.5 | 1.81 | 58 | 65 | 17 | 30 | |||||
| Prospective studies EA | 58 | 25 | 17 | −11.25 | 50 | 33 | 43 | 45 | |||||
| Prospective studies ITT | 59 | 11 | 29 | 55 | 39 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaina, F.; Cordani, C.; Donzelli, S.; Lazzarini, S.G.; Arienti, C.; Del Furia, M.J.; Negrini, S. Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review. Children 2022, 9, 1672. https://doi.org/10.3390/children9111672
Zaina F, Cordani C, Donzelli S, Lazzarini SG, Arienti C, Del Furia MJ, Negrini S. Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review. Children. 2022; 9(11):1672. https://doi.org/10.3390/children9111672
Chicago/Turabian StyleZaina, Fabio, Claudio Cordani, Sabrina Donzelli, Stefano Giuseppe Lazzarini, Chiara Arienti, Matteo Johann Del Furia, and Stefano Negrini. 2022. "Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review" Children 9, no. 11: 1672. https://doi.org/10.3390/children9111672
APA StyleZaina, F., Cordani, C., Donzelli, S., Lazzarini, S. G., Arienti, C., Del Furia, M. J., & Negrini, S. (2022). Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review. Children, 9(11), 1672. https://doi.org/10.3390/children9111672








