The Incidence of Bracing Treatment on Static and Dynamic Baropodometric Parameters in Adolescent Idiopathic Scoliosis
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joseph, A.; Janicki, J.A.; Benjamin Alman, B. Scoliosis: Review of diagnosis and treatment. Paediatr. Child Health 2007, 12, 771–776. [Google Scholar]
- Kotwicki, T.; Walczak, A.; Szulc, A. Trunk rotation and hip joint range of rotation in adolescent girls with idiopathic scoliosis: Does the ”dinner plate” turn asymmetrically? Scoliosis 2008, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Stokes, I.A. Three-Dimensional Terminology of Spinal Deformity: A Report Presented to the Scoliosis Research Society by The Scoliosis Research Society Working Group on 3-D Terminology of Spinal Deformity. Spine 1994, 19, 236–248. [Google Scholar] [CrossRef]
- Havey, R.M.; Gavin, T.M.; Patwardhan, A.G. Stability of the Scoliotic Spine: Effect of Scoliosis Braces. Spine 2016, 41 (Suppl. 7), S18–S19. [Google Scholar] [CrossRef]
- Upadhyay, S.; Nelson, I.; Ho, E.K.; Hsu, L.C.; Leong, J. New prognostic factors to predict the final outcome of brace treatment in adolescent idiopathic scoliosis. Spine 1995, 20, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Dickson, R.A. Conservative treatment for idiopathic scoliosis. J. Bone Jt. Surg. 1985, 67, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Mahaudens, P.; Raison, M.; Banse, X.; Mousny, M.; Detrembleur, C. Effect of long-term orthotic treatment on gait biomechanics in adolescent idiopathic scoliosis. Spine J. 2014, 14, 1510–1519. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, O. Interrelationship between postural balance and body posture in children and adolescents. J. Phys. Ther. Sci. 2017, 29, 1154–1158. [Google Scholar] [CrossRef]
- Gefen, A.; Megido-Ravid, M.; Itzchak, Y.; Arcan, M. Biomechanical analysis of the three-dimensional foot structure during gait: A basic tool for clinical applications. J. Biomech. Eng. 2000, 122, 630–639. [Google Scholar] [CrossRef]
- Sun, P.-C.; Shih, S.-L.; Chen, Y.-L.; Hsu, Y.-C.; Yang, R.-C.; Chen, C.-S. Biomechanical analysis of foot with different foot arch heights: A finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 563–569. [Google Scholar] [CrossRef]
- Hebert-Losier, K.; Murray, L. Reliability of centre of pressure, plantar pressure, and plantar-flexion isometric strength measures: A systematic review. Gait Posture 2020, 75, 46–62. [Google Scholar] [CrossRef]
- Baker, R.; Esquenazi, A.; Benedetti, M.G.; Desloovere, K. Gait analysis: Clinical facts. Eur. J. Phys. Rehabil. Med. 2016, 62, 560–574. [Google Scholar]
- Palmieri, R.M.; Ingersoll, C.D.; Cordova, M.L.; Kinzey, S.J.; Stone, M.B.; Krause, B.A. The effect of a simulated knee joint effusion on postural control in healthy subjects. Arch. Phys. Med. Rehabil. 2003, 84, 1076–1079. [Google Scholar] [CrossRef]
- Reimann, B.L.; Caggiano, N.A.; Lephart, S.M. Examination of a clinical method of assessing postural control during a functional performance task. J. Sport Rehabil. 1999, 8, 171–183. [Google Scholar] [CrossRef]
- Yiou, E.; Hamaoui, A.; Gilles Allali, G. The Contribution of Postural Adjustments to Body Balance and Motor Performance. Front. Hum. Neurosci. 2018, 12, 487. [Google Scholar] [CrossRef] [PubMed]
- Yiou, E.; Artico, R.; Teyssedre, C.A.; Labaune, O.; Fourcade, P. Anticipatory Postural Control of Stability during Gait Initiation Over Obstacles of Different Height and Distance Made Under Reaction-Time and Self-Initiated Instructions. Front. Hum. Neurosci. 2016, 10, 449. [Google Scholar] [CrossRef]
- Conforti, M.P. La Postura. Master’s Thesis, Facoltà di Scienze Matematiche, Fisiche e Naturali, Università degli studi di Pisa, Pisa, Italy, 2006. [Google Scholar]
- Kramers-de Quervain, I.A.; Müller, R.; Stacoff, A.; Grob, D.; Stüssi, E. Gait analysis in patients with idiopathic scoliosis. Eur. Spine J. 2004, 13, 449–456. [Google Scholar] [CrossRef]
- Wong, M.S.; Cheng, C.Y.; Ng, B.K.W.; Lam, T.P.; Sin, S.W.; Lee-Shum, L.F.; Chow, H.K.; Tam, Y.P. The effect of rigid versus flexible spinal orthosis on the gait pattern of patients with adolescent idiopathic scoliosis. Gait Posture 2008, 27, 189–195. [Google Scholar] [CrossRef]
- Yağcı, G.; Yakut, Y. Effects of A Spinal Brace on the Functional Profile of the Feet in Adolescent Idiopathic Scoliosis. ACU Saglik Bil. Derg. 2018, 9, 282–288. [Google Scholar]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef]
- Horne, J.; Flannery, R.; Usman, S. Adolescent idiopathic scoliosis: Diagnosis and management. Am. Fam. Phys. 2014, 89, 193–198. [Google Scholar]
- Coelho, D.; Bonagamba, G.; Oliveira, A. Scoliometer measurements of patients with idiopathic scoliosis. Braz. J. Phys. Ther. 2013, 17, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, S.; Parent, E.C.; Hill, D.L.; Hedden, D.M.; Moreau, M.J.; Southon, S.C. Patients with adolescent idiopathic scoliosis perceive positive improvements regardless of change in the Cobbangle—Results from a randomized controlled trial comparing a 6-month Schroth intervention added to standard care and standard care alone. BMC Musculoskelet. Disord. 2019, 20, 319. [Google Scholar] [CrossRef] [PubMed]
- Troy, M.J.; Miller, P.E.; Price, N.; Talwalkar, V.; Zaina, F.; Donzelli, S.; Negrini, S.; Hresko, M.T. The “Risser+” grade: A new grading system to classify skeletal maturity in idiopathic scoliosis. Eur. Spine J. 2019, 28, 559–566. [Google Scholar] [CrossRef]
- Negrini, S.; Marchini, G. Efficacy of the symmetric, patient-oriented, rigid, three-dimensional, active concept of bracing for scoliosis: A prospective study of the Sfornisco versus Lyon brace. Eura Meddicophys. 2007, 43, 171–181. [Google Scholar]
- Bettany-Saltikov, J.; Weiss, H.R.; Chockalingam, N.; Taranu, R.; Srinivas, S.; Hogg, J.; Whittaker, V.; Kalyan, R.V.; Arnell, T. Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst. Rev. 2015, 4, CD1010663. [Google Scholar] [CrossRef]
- Romano, M.; Minozzi, S.; Bettany-Saltikov, J.; Zaina, F.; Chockalingam, N.; Kotwicki, T.; Maier-Hennes, A.; Stefano Negrini, S. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2012, 8, CD007837. [Google Scholar] [CrossRef]
- El Hawary, R.; Zaaroor-Regev, D.; Floman, Y.; Lonner, B.S.; Alkhalife, Y.I.; Betz, R.R. Brace treatment in adolescent idiopathic scoliosis risk factor for failure—A literature review. Spine J. 2019, 19, 1917–1925. [Google Scholar] [CrossRef]
- Neto, H.P.; Grecco, L.A.C.; Ferreira, L.A.B.; Christovão, T.C.L.C.; Carvalho Duarte, N.A.; Santos Oliveira, C. Clinical analysis and baropodometric evaluation in diagnosis of abnormal foot posture: A clinical trial. J. Bodyw. Mov. Ther. 2015, 19, 429–433. [Google Scholar] [CrossRef]
- Diaz, M.A.; Gibbons, M.W.; Song, J.; Hillstrom, H.J.; Choe, K.H.; Pasquale, M.R. Concurrent validity of an automated algorithm for computing the center of pressure excursion index (CPEI). Gait Posture 2018, 59, 7–10. [Google Scholar] [CrossRef]
- Levine, D.; Richards, J.; Whittle, M.W. Whittle’s Gait Analysis, 5th ed.; Churchill Livingstone, Elsevier: Chatswood, Australia, 2012. [Google Scholar]
- Baumfeld, D.; Baumfeld, T.; da Rocha, R.L.; Macedo, B.; Raduan, F.; Zambelli, R.; Alves Silva, T.A.; Ne, C. Reliability of baropodrometry on the evaluation of plantar load distribution: A transversal study. Biomed. Res. Int. 2017, 2017, 5925137. [Google Scholar] [CrossRef]
- McGee, M. Case for omitting tied observations in the two-sample t-test and the Wilcoxon-Mann-Whitney Test. PLoS ONE 2017, 13, e0200837. [Google Scholar] [CrossRef]
- Haumont, T.; Gauchard, G.C.; Lascombes Perrin, P.P. Postural instability in early-stage idiopathic scoliosis in adolescent girls. Spine 2011, 36, E847–E854. [Google Scholar] [CrossRef]
- Lee, J.-U.; Kim, M.-Y.; Kim, J. Comparison of static plantar foot pressure between healthy subjects and patients with adolescent idiopathic scoliosis. Toxicol. Environ. Health Sci. 2014, 6, 127–132. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Rodgers, M.M.; Liboshi, A. Pressure distribution under symptom-free feet during barefoot standing. Foot Ankle 1987, 7, 262–276. [Google Scholar] [CrossRef]
- Putti, A.B.; Arnold, G.P.; Cochrane, L.A.; Abboud, R.J. Normal pressure values and repeatability of the Emed® ST4 system. Gait Posture 2008, 27, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Hong, Q.; Guo, X.; Wang, D.; Chen, J.; Zhu, Q.; Zhang, C.; Chen, W.; Zhang, M. A comparison of foot posture and walking performance in patients with mild, moderate, and severe adolescent idiopathic scoliosis. PLoS ONE 2021, 16, e0251592. [Google Scholar] [CrossRef]
- Sim, T.; Yoo, H.; Lee, D.; Suh, S.-W.; Yang, J.H.; Kim, H.; Mun, J.H. Analysis of sensory system aspects of postural stability during quiet standing in adolescent idiopathic scoliosis patients. J. Neuroeng. Rehabil. 2018, 15, 54. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-J.; Sim, T.; Suh, S.-W.; Yang, J.H.; Koo, H.; Mun, J.H. Analysis of coordination between thoracic and pelvic kinematic movements during gait in adolescents with idiopathic scoliosis. Eur. Spine J. 2016, 25, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Ravalli, S.; Maugeri, G.; Bianco, A.; Palma, A.; Di Rosa, M.; Musumeci, G. Technological advancements in the analysis of human motion and posture management through digital devices. World J. Orthop. 2021, 12, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Kwok, G.; Yip, J.; Yick, K.-L.; Cheung, M.-C.; Tse, C.-Y.; Ng, S.-P. Ameersing Luximon Postural Screening for Adolescent Idiopathic Scoliosis with Infrared Thermography. Sci. Rep. 2017, 7, 14431. [Google Scholar] [CrossRef] [PubMed]
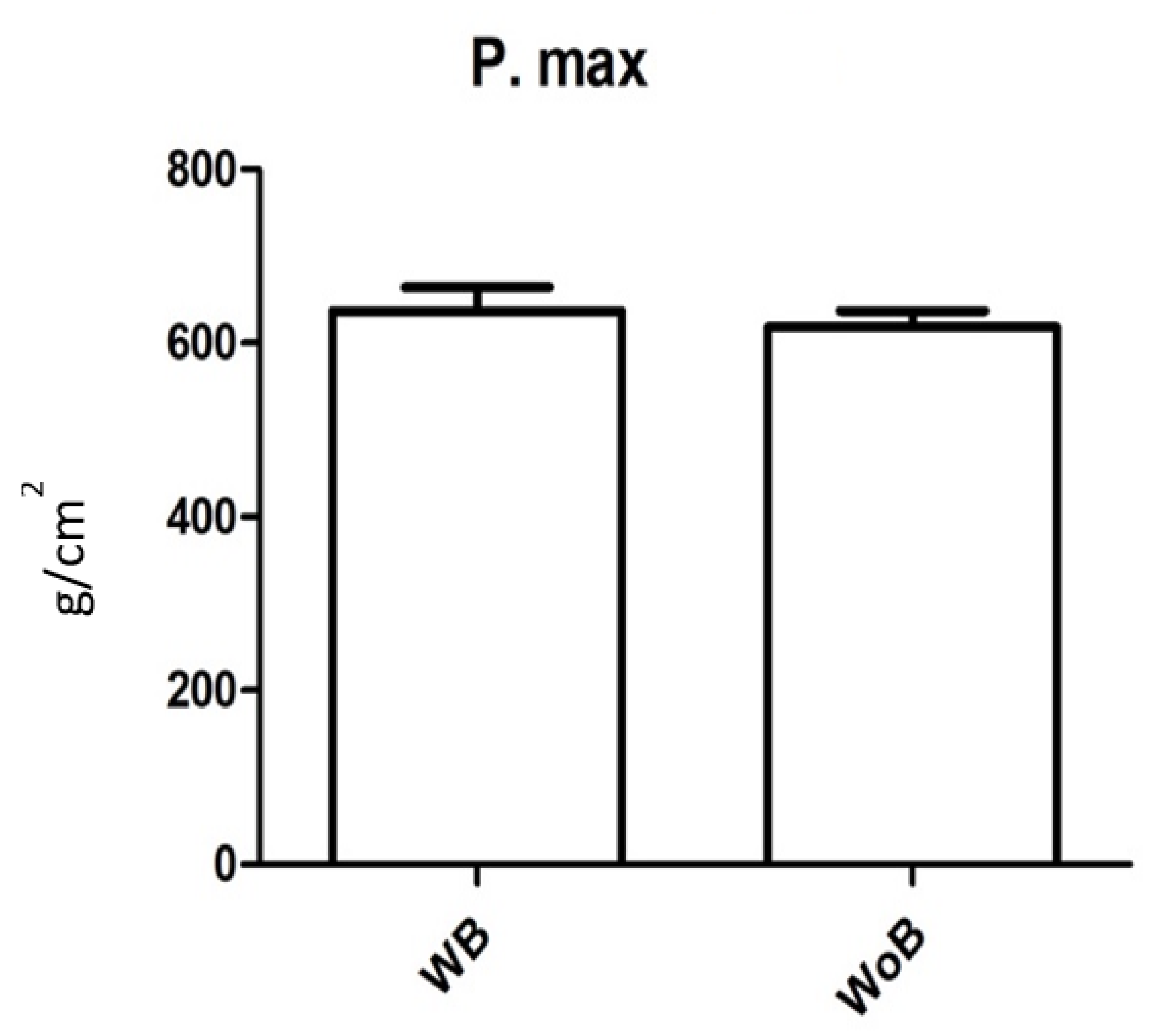
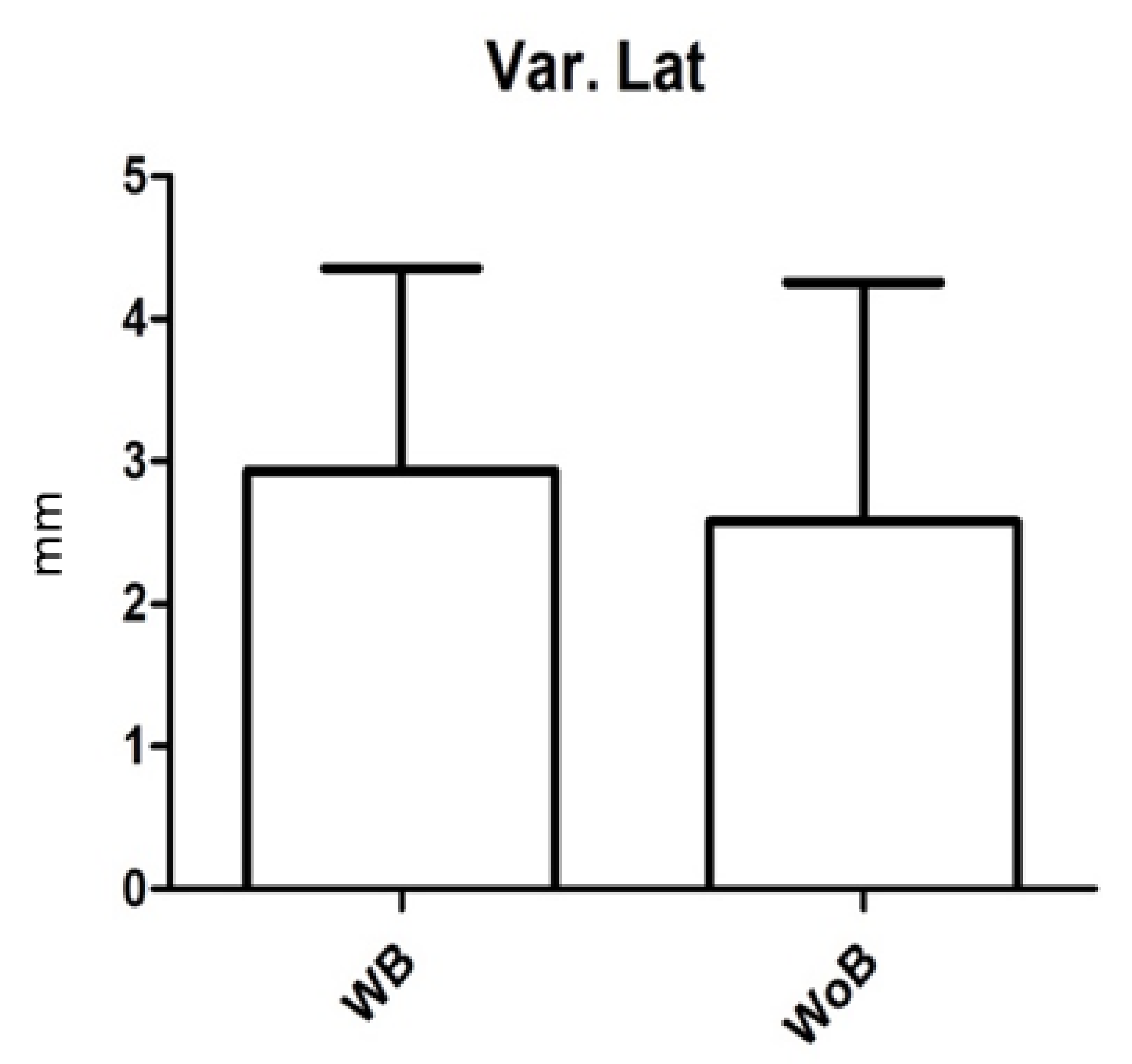
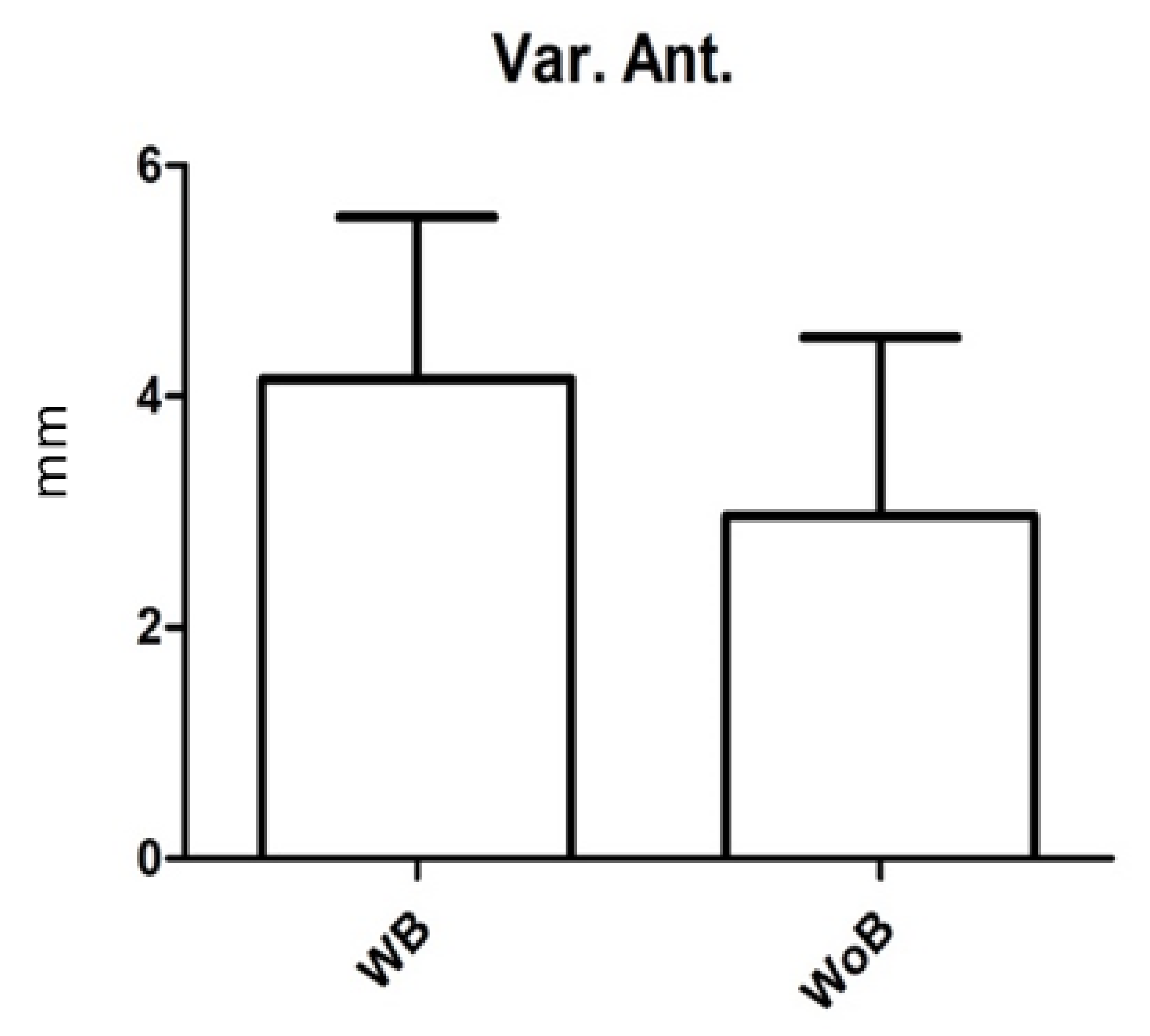
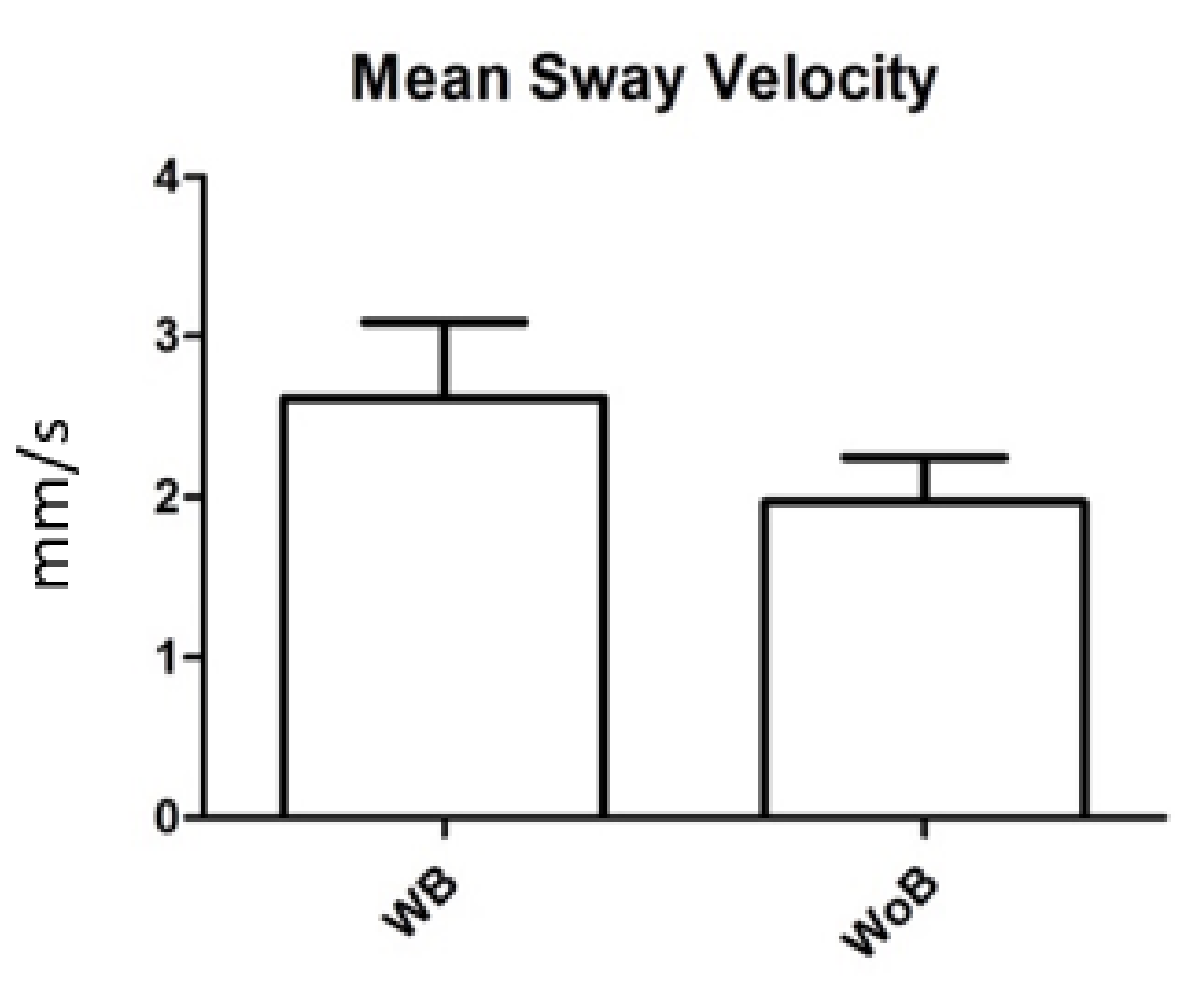
| STATIC | POSTURAL | GAIT ANALYSIS | ||||
|---|---|---|---|---|---|---|
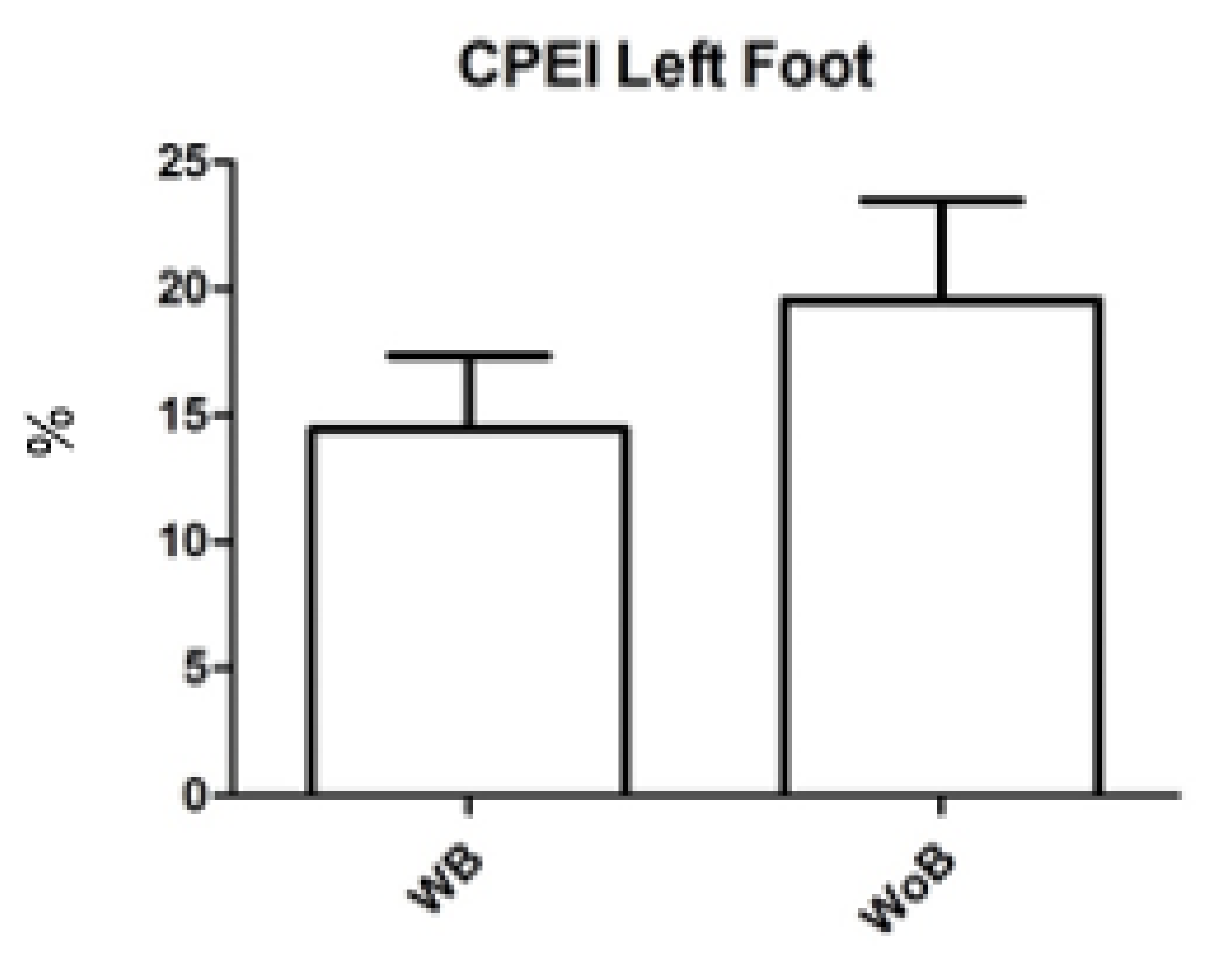
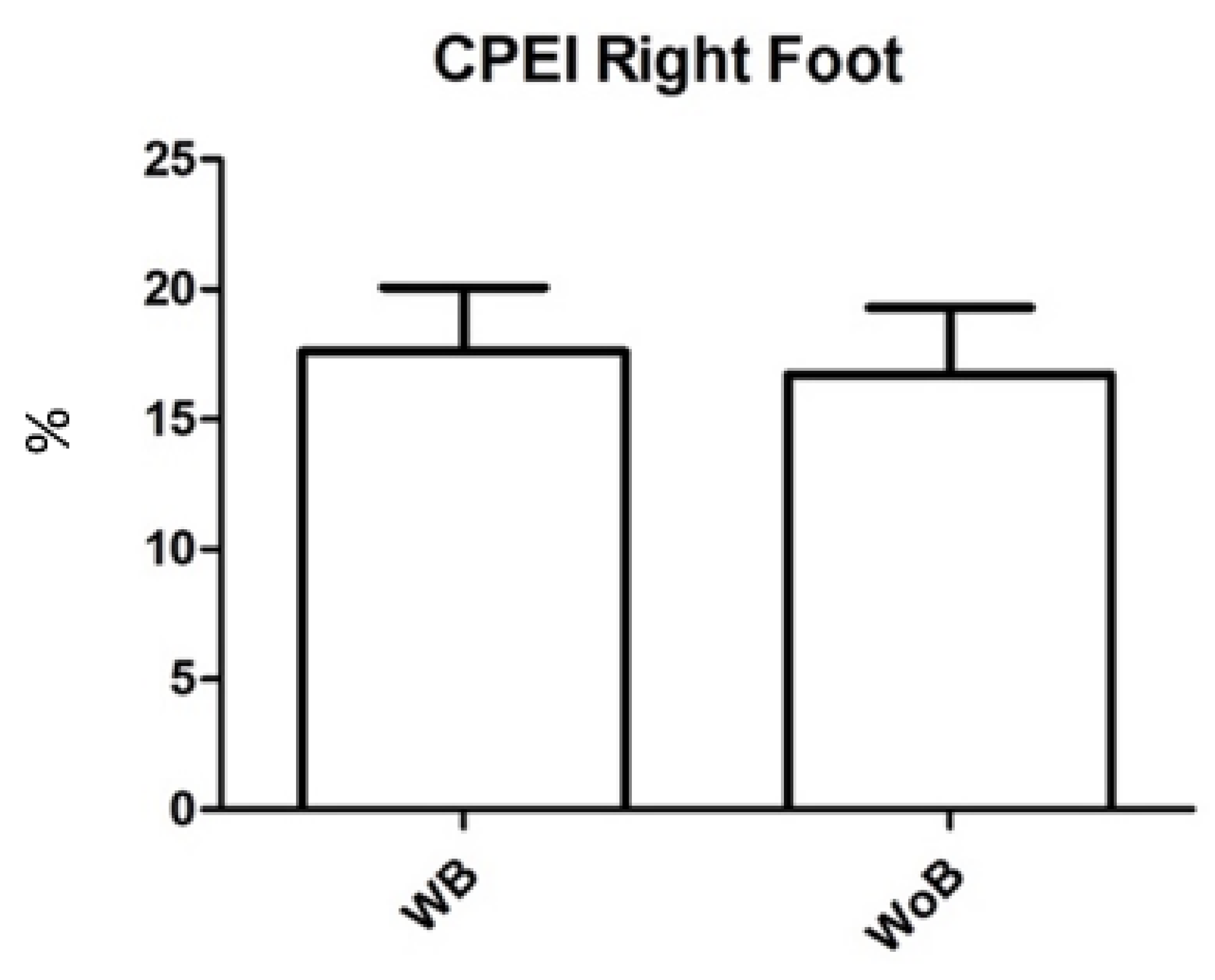
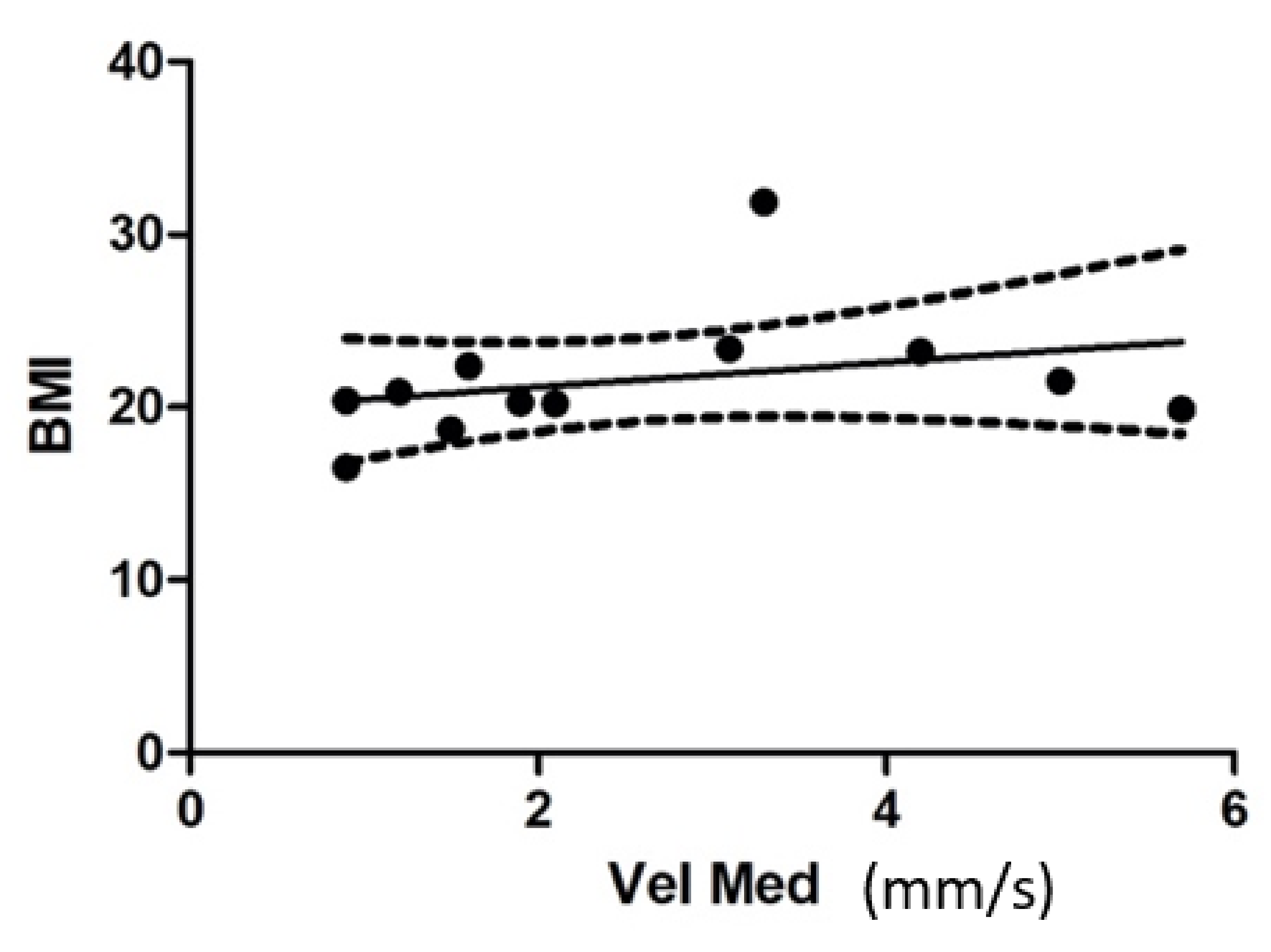
| P. max | Var. Lat | Var. Ant. | Vel. Mean | CPEI SX | CPEI DX | |
| NO BRACE | 620 (±65) | 2.6 (±5.8) | 3 (±5.4) | 2 (±0.97) | 20 (±14) | 17 (±8.9) |
| BRACE | 640 (±95) | 2.9 (±4.9) | 4.2 (±4.9) | 2.6 (±1.6) | 14 (±10) | 18 (±8.5) |
| WILCOXON TEST (p value) | 0.2277 | 0.2852 | 0.0881 | 0.0458 | 0.2065 | 0.1902 |
| PATIENTS | AGE (YEAR) | GENDER | HEIGHT (CM) | WEIGHT (KG) | BMI | TIME OF TREATMENT (MONTHS) | COBB ANGLE (DEGREE) | RISSER SCORE | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | S. V. | 13 | F | 165 | 55 | 20.2 | 12 | 28 | 3 |
| 2 | S. G. | 15 | F | 159 | 53 | 20.9 | 14 | 32 | 4 |
| 3 | S. G. | 16 | F | 170 | 54 | 18.7 | 24 | 24 | 4 |
| 4 | G. P. | 13 | F | 155 | 49 | 20.4 | 8 | 21 | 3 |
| 5 | C. S. | 13 | F | 152 | 55 | 23.4 | 9 | 22 | 3 |
| 6 | B. S. | 11 | F | 135 | 58 | 31.9 | 4 | 23 | 1 |
| 7 | C. C. | 13 | F | 152 | 46 | 19.9 | 7 | 26 | 2 |
| 8 | C. M. | 15 | F | 163 | 54 | 20.3 | 22 | 30 | 4 |
| 9 | C. M. | 11 | F | 125 | 35 | 22.4 | 2 | 21 | 1 |
| 10 | P. C. | 15 | F | 165 | 45 | 16.5 | 13 | 32 | 4 |
| 11 | S. A. | 12 | F | 128 | 38 | 23.2 | 2 | 28 | 2 |
| 12 | U. A. T. | 14 | F | 160 | 55 | 21.5 | 10 | 26 | 3 |
| MEAN | 13.4 | 152.4 | 49.75 | 21.6 | 10.6 | 26.08 | 2.83 | ||
| SD | 1.55 | 14.42 | 7.01 | 3.59 | 6.72 | 3.81 | 1.06 | ||
| MIN. | 11 | 125 | 35 | 16.5 | 2 | 21 | 1 | ||
| MAX. | 16 | 170 | 58 | 31.9 | 24 | 32 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pavone, V.; Caldaci, A.; Mangano, G.R.A.; Maria, F.D.; Panvini, F.M.C.; Sapienza, M.; Vescio, A.; Roggio, F.; Musumeci, G.; Testa, G. The Incidence of Bracing Treatment on Static and Dynamic Baropodometric Parameters in Adolescent Idiopathic Scoliosis. Children 2022, 9, 1608. https://doi.org/10.3390/children9111608
Pavone V, Caldaci A, Mangano GRA, Maria FD, Panvini FMC, Sapienza M, Vescio A, Roggio F, Musumeci G, Testa G. The Incidence of Bracing Treatment on Static and Dynamic Baropodometric Parameters in Adolescent Idiopathic Scoliosis. Children. 2022; 9(11):1608. https://doi.org/10.3390/children9111608
Chicago/Turabian StylePavone, Vito, Alessia Caldaci, Giulia Rita Agata Mangano, Fabrizio Di Maria, Flora Maria Chiara Panvini, Marco Sapienza, Andrea Vescio, Federico Roggio, Giuseppe Musumeci, and Gianluca Testa. 2022. "The Incidence of Bracing Treatment on Static and Dynamic Baropodometric Parameters in Adolescent Idiopathic Scoliosis" Children 9, no. 11: 1608. https://doi.org/10.3390/children9111608
APA StylePavone, V., Caldaci, A., Mangano, G. R. A., Maria, F. D., Panvini, F. M. C., Sapienza, M., Vescio, A., Roggio, F., Musumeci, G., & Testa, G. (2022). The Incidence of Bracing Treatment on Static and Dynamic Baropodometric Parameters in Adolescent Idiopathic Scoliosis. Children, 9(11), 1608. https://doi.org/10.3390/children9111608










