The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Outcomes of the Study
2.3. Study Design
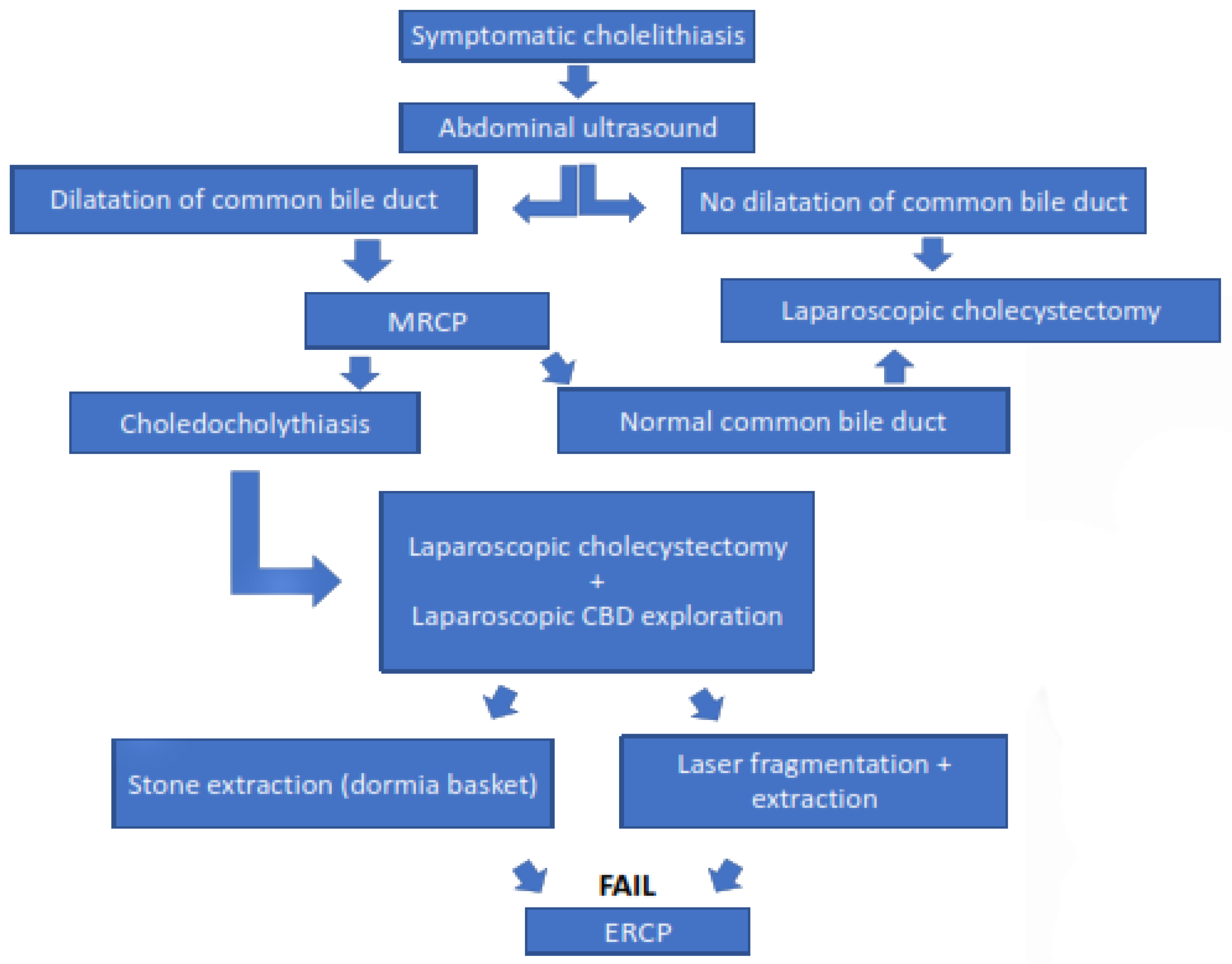
2.4. Diagnostic Procedure and Indications for Surgery
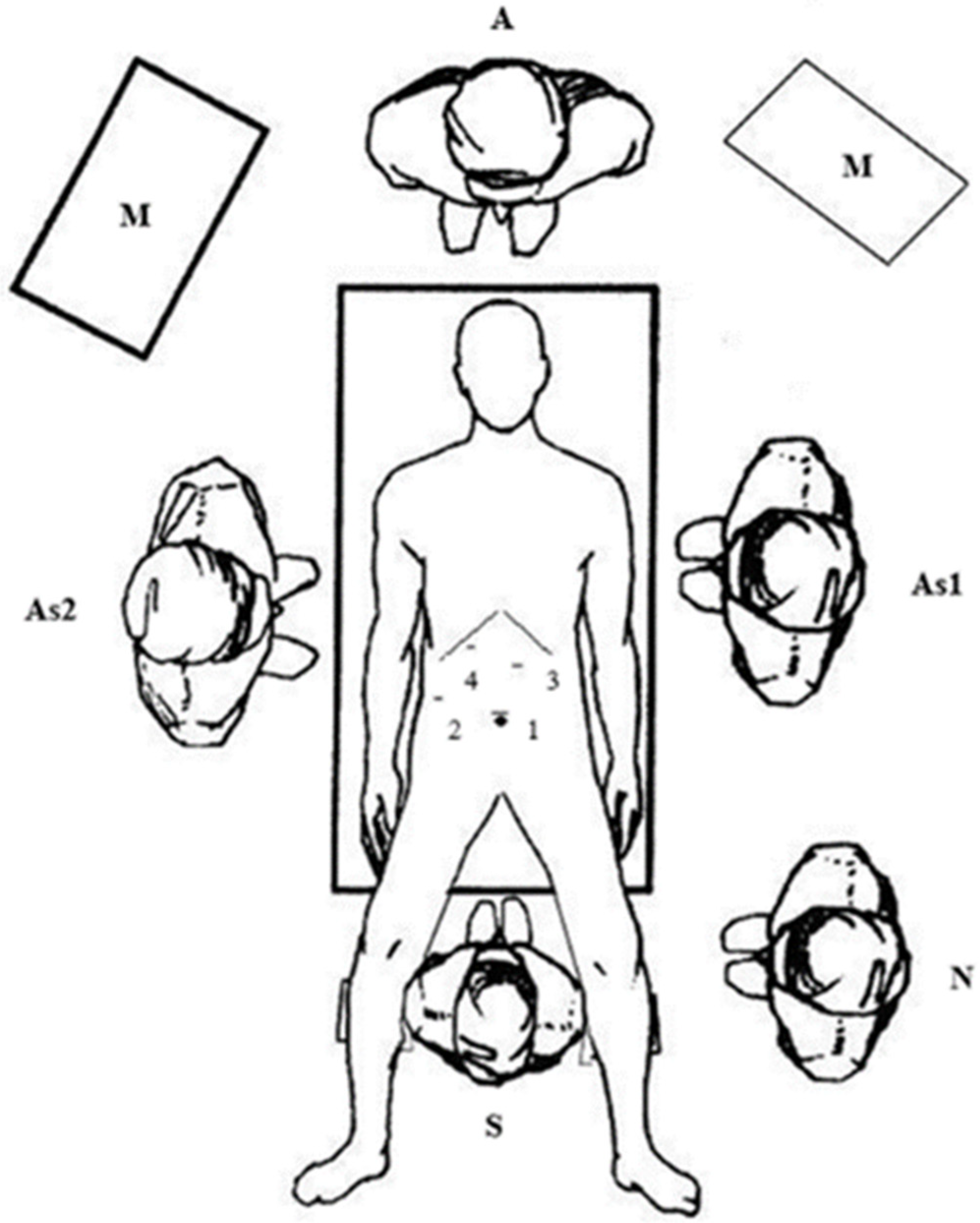
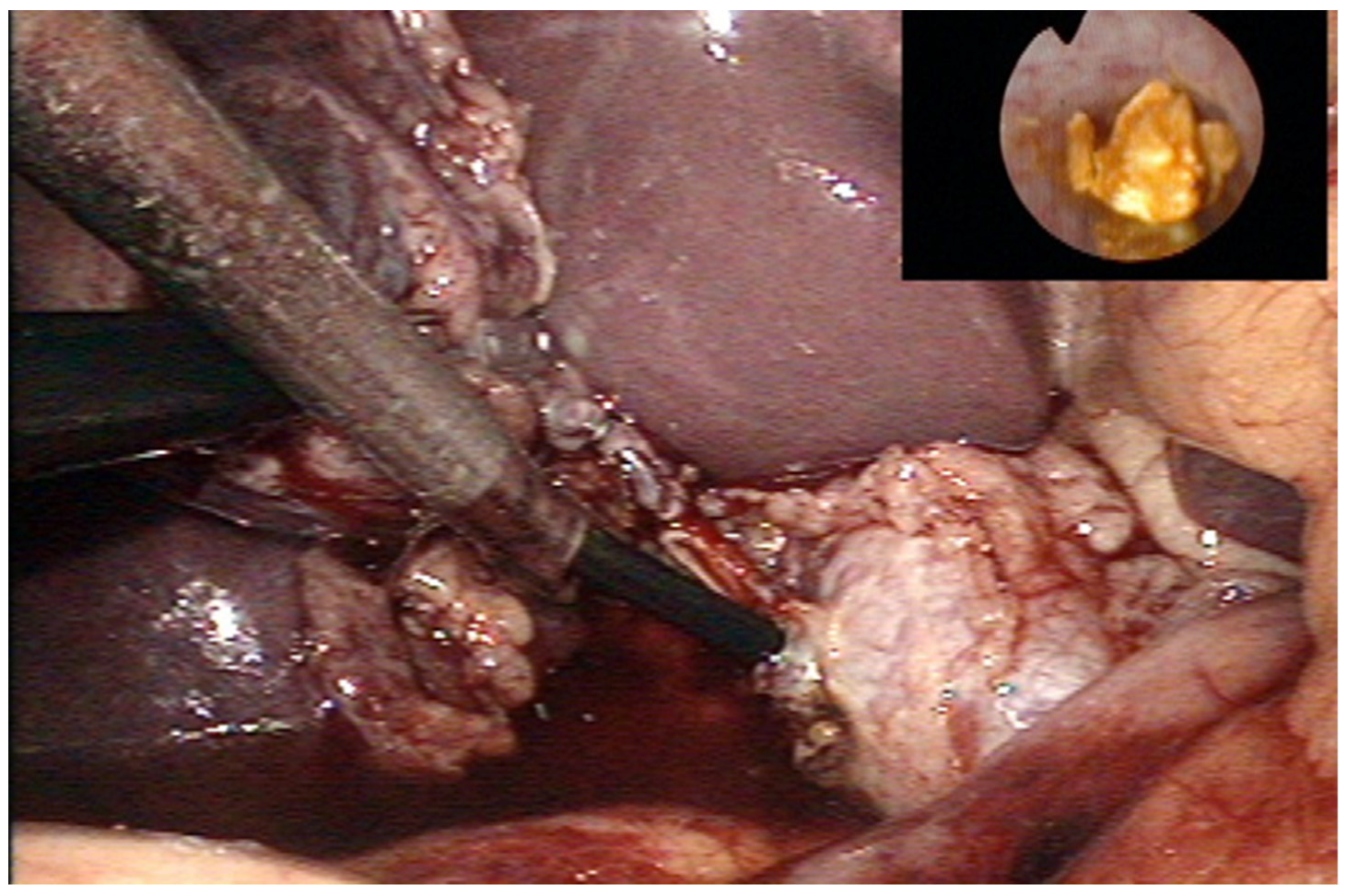
2.5. Surgical Technique (LCBDE)
2.6. Follow-Up
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murphy, P.; Vogt, K.; Winick-Ng, J.; McClure, J.; Welk, B.; Jones, S. The increasing incidence of gallbladder disease in children: A 20 year perspective. J. Pediatr. Surg. 2016, 51, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Poddar, U. Gallstone disease in children. Indian Pediatr. 2010, 47, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.K.; Maki, A.C.; Cannon, R.M.; Foley, D.S.; Wilson, K.M.; Galganski, L.A.; Wiesenauer, C.A.; Bond, S.J. Etiology and incidence of pediatric gallbladder disease. Surgery 2013, 154, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, D.; Harmon, C. Gallbladder disease in children. Semin. Pediatr. Surg. 2016, 25, 225–231. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Aralica, M.; Jukić, M.; Žitko, V.; Despot, R.; Jurić, I. Gallbladder disease in children: A 20-year single-center experience. Indian Pediatr. 2019, 56, 384–386. [Google Scholar] [CrossRef]
- Wong, M.C.Y.; Incerti, F.; Avanzini, S.; Palo, F.; Sertorio, F.; Damasio, M.B.; Arrigo, S.; Gandullia, P.; Mattioli, G. Cholelithiasis management in a third-level pediatric center: Case series and literature review. Updates Surg. 2022, 74, 963–968. [Google Scholar] [CrossRef]
- Agrawal, V.; Tiwari, A.; Sharma, D.; Agrawal, R. Etiology-based decision-making protocol for pediatric cholelithiasis. Indian Pediatr. 2021, 58, 729–732. [Google Scholar] [CrossRef]
- Guo, T.; Wang, L.; Xie, P.; Zhang, Z.; Huang, X.; Yu, Y. Surgical methods of treatment for cholecystolithiasis combined with choledocholithiasis: Six years’ experience of a single institution. Surg. Endosc. 2022, 36, 4903–4911. [Google Scholar] [CrossRef]
- Cianci, P.; Restini, E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J. Gastroenterol. 2021, 27, 4536–4554. [Google Scholar] [CrossRef]
- Mohseni, S.; Bass, G.A.; Forssten, M.P.; Casas, I.M.; Martin, M.; Davis, K.A.; Haut, E.R.; Sugrue, M.; Kurihara, H.; Sarani, B.; et al. Common bile duct stones management: A network meta-analysis. J. Trauma Acute Care Surg. 2022. [Google Scholar] [CrossRef]
- Samara, O.; Azzam, M.I.; Alshrouf, M.A.; Khanfar, A.N.; Mohialdeen, R.R.; Barham, O.F.; Barham, M.F.; AlRyalat, S.A. Diagnostic accuracy of ultrasonography compared with magnetic resonance cholangiopancreatography in the detection of choledocholithiasis. J. Clin. Ultrasound 2022, 50, 247–253. [Google Scholar] [CrossRef]
- Agostini, Â.F.P.; Hochhegger, B.; Forte, G.C.; Susin, L.A.; Difini, J.P.M. Accuracy of abbreviated protocol of magnetic resonance cholangio-pancreatography in the diagnosis of choledocholithiasis. Arq. Gastroenterol. 2022, 59, 188–192. [Google Scholar] [CrossRef]
- Lau, B.J.; Sydorak, R.M.; Shaul, D.B. Laparoscopic techniques for safe and successful removal of common bile duct stones in pediatric patients. J. Laparoendosc. Adv. Surg. Technol. A 2014, 24, 362–365. [Google Scholar] [CrossRef]
- Cohen, R.Z.; Tian, H.; Sauer, C.G.; Willingham, F.F.; Santore, M.T.; Mei, Y.; Freeman, A.J. Creation of a Pediatric Choledocholithiasis Prediction Model. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 636–641. [Google Scholar] [CrossRef]
- Menon, S.; Patel, B.; Saekang, E.; Thomas, G.; Soundappan, S.; Shun, A. Laparoscopic exploration of the common bile duct to relieve choledocholithiasis in children. Pediatr. Surg. Int. 2011, 27, 537–540. [Google Scholar] [CrossRef]
- Kumar, R.; Nguyen, K.; Shun, A. Gallstones and common bile duct calculi in infancy and childhood. Aust. N. Z. J. Surg. 2000, 70, 188–191. [Google Scholar] [CrossRef]
- Frybova, B.; Drabek, J.; Lochmannova, J.; Douda, L.; Hlava, S.; Zemkova, D.; Mixa, V.; Kyncl, M.; Zeman, L.; Rygl, M.; et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS ONE 2018, 13, e0196475. [Google Scholar] [CrossRef]
- Bogue, C.; Murphy, A.; Gerstle, J.; Moineddin, R.; Daneman, A. Risk factors, complications, and outcomes of gallstones in children: A single-center review. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 303–308. [Google Scholar] [CrossRef]
- Kim, H.; Shin, S.; Hwang, J.; Lee, J. Outcomes of laparoscopic common bile duct exploration (LCBDE) after failed endoscopic retrograde cholangiopancreatography versus primary LCBDE for managing cholecystocholedocholithiasis. J. Int. Med. Res. 2020, 48, 300060520957560. [Google Scholar] [CrossRef]
- Wang, C.C.; Tsai, M.C.; Wang, Y.T.; Yang, T.W.; Chen, H.Y.; Sung, W.W.; Huang, S.M.; Tseng, M.H.; Lin, C.C. Role of cholecystectomy in choledocholithiasis patients underwent endoscopic retrograde cholangiopancreatography. Sci. Rep. 2019, 9, 2168. [Google Scholar] [CrossRef]
- Giefer, M.J.; Kozarek, R.A. Technical outcomes and complications of pediatric ERCP. Surg. Endosc. 2015, 29, 3543–3550. [Google Scholar] [CrossRef]
- Enestvedt, B.K.; Tofani, C.; Lee, D.Y.; Abraham, M.; Shah, P.; Chandrasekhara, V.; Ginsberg, G.G.; Long, W.; Ahmad, N.; Jaffe, D.L.; et al. Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 649–654. [Google Scholar] [CrossRef]
- Gad, E.H.; Zakaria, H.; Kamel, Y.; Alsebaey, A.; Zakareya, T.; Abbasy, M.; Mohamed, A.; Nada, A.; Abdelsamee, M.A.; Housseni, M. Surgical (Open and laparoscopic) management of large difficult CBD stones after different sessions of endoscopic failure: A retrospective cohort study. Ann. Med. Surg. 2019, 43, 52–63. [Google Scholar] [CrossRef]
- Perko, Z.; Bilan, K.; Pogorelić, Z.; Srsen, D.; Druzijanić, N.; Kraljević, D.; Juricić, J.; Mimica, Z.; Jurisić, T.; Bekavac-Beslin, M. A novel algorithm for the minimal invasive treatment of choledocholithiasis. Hepatogastroenterology 2007, 54, 1009–1012. [Google Scholar] [PubMed]
- Bansal, V.K.; Misra, M.C.; Rajan, K.; Kilambi, R.; Kumar, S.; Krishna, A.; Kumar, A.; Pandav, C.S.; Subramaniam, R.; Arora, M.K.; et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: A randomized controlled trial. Surg. Endosc. 2014, 28, 875–885. [Google Scholar]
- Short, S.S.; Frykman, P.K.; Nguyen, N.; Liu, Q.; Berel, D.; Wang, K.S. Laparoscopic common bile duct exploration in children is associated with decreased cost and length of stay: Results of a two-center analysis. J. Pediatr. Surg. 2013, 48, 215–220. [Google Scholar] [CrossRef]
- Lee, H.M.; Min, S.K.; Lee, H.K. Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann. Surg. Treat. Res. 2014, 86, 1–6. [Google Scholar] [CrossRef]
- Capparelli, M.A.; DAlessandro, P.D.; Questa, H.A.; Ayarzabal, V.H.; Bailez, M.M.; Barrenechea, M.E. Development of a risk score for choledocholithiasis in pediatric patients. Pediatr. Surg. Int. 2021, 37, 1393–1399. [Google Scholar] [CrossRef]
- St. Peter, S.D.; Keckler, S.J.; Nair, A.; Andrews, W.S.; Sharp, R.J.; Snyder, C.L.; Ostlie, D.J.; Holcomb, G.W. Laparoscopic cholecystectomy in the pediatric population. J. Laparoendosc. Adv. Surg. Technol. A 2008, 18, 127–130. [Google Scholar] [CrossRef]
- Cabrera Chamorro, C.C.; Pabón Arteaga, J.S.; Caicedo Paredes, C.A.; Cabrera Bravo, N.; Villamil Giraldo, C.E.; Chávez Betancourt, G.; Zarama Márquez, R.A.; Rincón Torres, C.A. Cholelithiasis and associated complications in pediatric patients. Cir. Pediatr. 2020, 33, 172–176. [Google Scholar]
| Variable | 2000–2022 |
|---|---|
| Number of cholecystectomies | 84 |
| Demographic data | |
| age; years (median, IQR) | 11.4 (8, 14) |
| female; n (%) | 66 (78.5%) |
| male; n (%) | 18 (21.5%) |
| Anthropometric data | |
| body height; cm (median, IQR) | 147.5 (138.8, 154.9) |
| body mass; kg (median, IQR) | 55.9 (50.3, 63.8) |
| BMI; cm/m2 (median, IQR) | 26.7 (22.4, 29.6) |
| Main indication for surgery | |
| biliary colic; n (%) | 14 (16.7%) |
| hereditary spherocytosis; n (%) | 15 (17.9%) |
| acute pancreatitis; n (%) | 16 (19%) |
| acute cholecystitis; n (%) | 19 (22.6%) |
| obstructive jaundice; n (%) | 20 (23.8%) |
| Complications; n (%) | |
| CBD injury | 1 (1.3%) |
| Variable | LC + ERCP (2000–2007) | LCBDE (2007–2022) | p |
|---|---|---|---|
| Number of procedures—LCBDE; n (%) | 6 (30) | 14 (70) | <0.001 |
| Demographic data Gender—female; n (%) Age; years (median, IQR) BMI; cm/m2 (median, IQR) | 5 (83.5) 14 (11.5, 145) 27.9 (23.5, 29.5) | 12 (85.7) 13.5 (11, 14.5) 27.4 (23, 29.6) | 0.891 0.651 0.722 |
| Clinical presentation; n (%) | |||
| obstructive jaundice colic type pain acute pancreatitis obstruction of papilla Laboratory values (median, IQR) Bilirubin, μmol/L ALP, U/L AST, U/L ALT, U/L GGT, U/L | 6 (100) 6 (100) 2 (60) 2 (40) 129 (91, 204) 1174 (1051, 1387) 133 (112, 159) 196 (173, 211) 186 (169, 201) | 14 (100) 13 (92.9) 7 (50) 5 (41.6) 132 (89, 206) 1105 (1004, 1354) 134 (114, 158) 188 (169, 206) 186 (171, 200) | 1.0 0.874 0.642 0.918 0.874 0.541 0.698 0.884 |
| Stone characteristics Diameter; mm (median, IQR) Number of stones (median, IQR) Diameter of CBD; mm (median, IQR) Surgical approach; n (%) LCBDE—Dormia basket extraction LCBDE—Laser fragmentation | 8 (6.5, 11) 1 (1, 2) 9 (8, 11) - - | 7.5 (6, 11) 1 (1, 3) 9 (7.5, 11) 10 (78.5) 4 (21.5) | 0.478 0.908 0.854 |
| Complications; n (%) | 2 (40) | 0 (0) | 0.078 |
| Operative time; min (median, IQR) LOS; days (median, IQR) | 85 (74, 105) 4 (3, 5) | 79 (68, 98) 2 (2, 4) | 0.125 0.011 |
| Variable | n (%) |
|---|---|
| Type of gallstone | |
| pigment | 6 (42.9) |
| cholesterol | 7 (50) |
| mixed | 1 (7.1) |
| Histopathology report | |
| normal | 1 (7.1) |
| acute cholecystitis | 2 (14.3) |
| chronic cholecystitis | 11 (78.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogorelić, Z.; Lovrić, M.; Jukić, M.; Perko, Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children 2022, 9, 1583. https://doi.org/10.3390/children9101583
Pogorelić Z, Lovrić M, Jukić M, Perko Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children. 2022; 9(10):1583. https://doi.org/10.3390/children9101583
Chicago/Turabian StylePogorelić, Zenon, Marko Lovrić, Miro Jukić, and Zdravko Perko. 2022. "The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis" Children 9, no. 10: 1583. https://doi.org/10.3390/children9101583
APA StylePogorelić, Z., Lovrić, M., Jukić, M., & Perko, Z. (2022). The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children, 9(10), 1583. https://doi.org/10.3390/children9101583








