ADHD-Gaming Disorder Comorbidity in Children and Adolescents: A Narrative Review
Abstract
1. Introduction
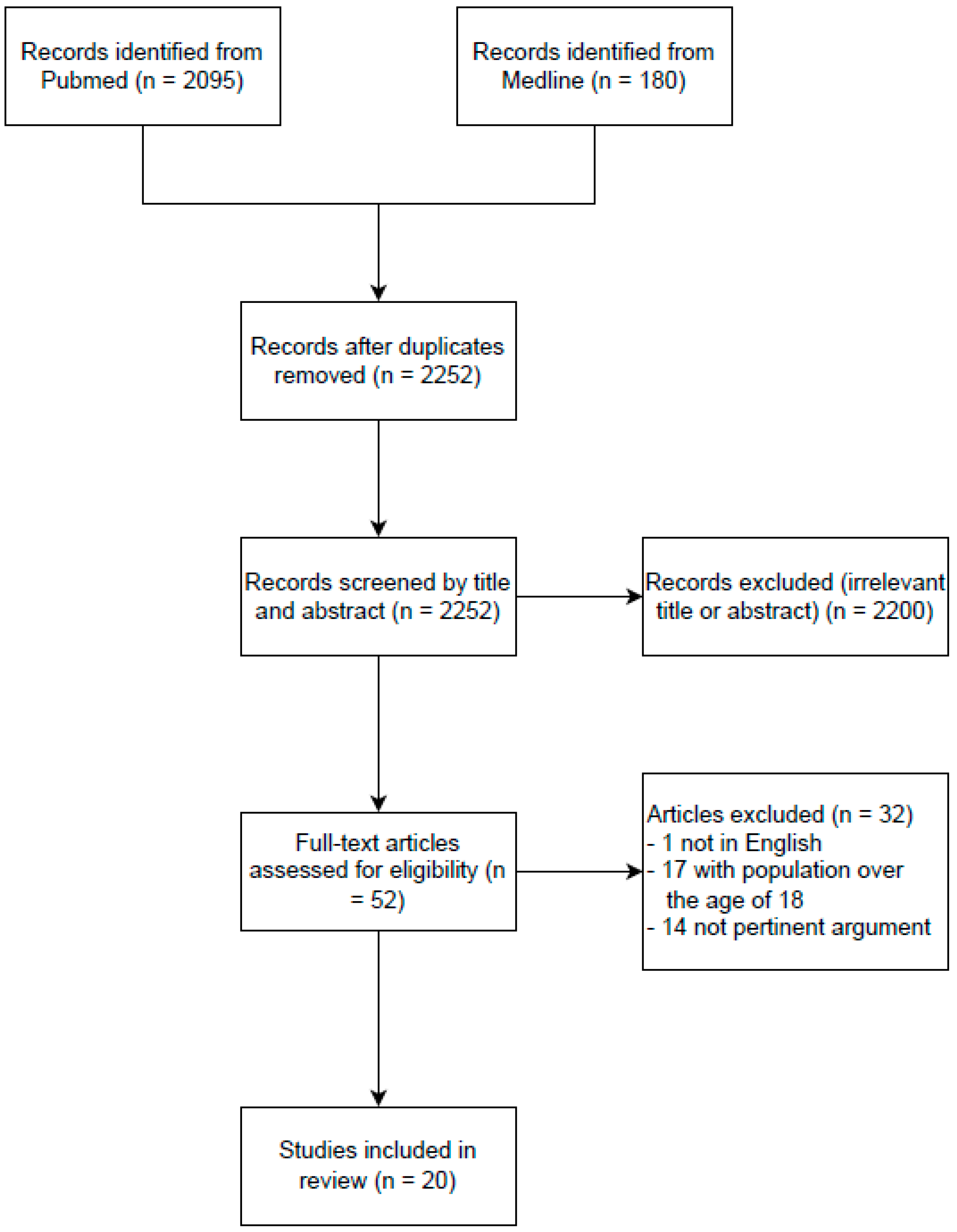
2. Materials and Methods
3. Results
3.1. Assessment of GD in ADHD
3.2. What We Currently Know about The ADHD–GD Comorbidity
3.3. The Impact of ADHD on Gaming Disorder across the Lifespan
3.4. Brain Structural and Functional Connectivity in ADHD and GD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Fayyad, J.; Sampson, N.A.; Hwang, I.; Adamowski, T.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Andrade, L.H.; Borges, G.; de Girolamo, G.; Florescu, S.; et al. The descriptive epidemiology of DSM-IV adult ADHD in the World Health Organization World Mental Health Surveys. Atten. Defic. Hyperact. Disord. 2017, 9, 47–65. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 2019, 24, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Brikell, I.; Lichtenstein, P.; Serlachius, E.; Kuja-Halkola, R.; Sandin, S.; Larsson, H. Familial aggregation of attention-deficit/hyperactivity disorder. J. Child Psychol. Psychiatry 2017, 58, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Nikolas, M.A.; Burt, S.A. Genetic and environmental influences on ADHD symptom dimensions of inattention and hyperactivity: A meta-analysis. J. Abnorm. Psychol. 2010, 119, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Pallanti, S.; Salerno, L. The Burden of Adult ADHD in Comorbid Psychiatric and Neurological Disorders; Springer Nature: Cham, Switzerland, 2020; pp. 61–86. [Google Scholar]
- Feldman, H.M.; Reiff, M.I. Clinical practice. Attention deficit-hyperactivity disorder in children and adolescents. N. Engl. J. Med. 2014, 370, 838–846. [Google Scholar] [CrossRef]
- Franke, B.; Michelini, G.; Asherson, P.; Banaschewski, T.; Bilbow, A.; Buitelaar, J.K.; Cormand, B.; Faraone, S.V.; Ginsberg, Y.; Haavik, J.; et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur. Neuropsychopharmacol. 2018, 28, 1059–1088. [Google Scholar] [CrossRef]
- Barkley, R.A.; Fischer, M.; Smallish, L.; Fletcher, K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. J. Am. Acad. Child. Adolesc. Psychiatry 2006, 45, 192–202. [Google Scholar] [CrossRef]
- Flory, K.; Molina, B.S.; Pelham, W.E., Jr.; Gnagy, E.; Smith, B. Childhood ADHD predicts risky sexual behavior in young adulthood. J. Clin. Child. Adolesc. Psychol. 2006, 35, 571–577. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. ICD-11: International Classification of Diseases (11th Revision). 2019. Available online: https://icd.who.int/ (accessed on 23 July 2022).
- Castro-Calvo, J.; King, D.L.; Stein, D.J.; Brand, M.; Carmi, L.; Chamberlain, S.R.; Demetrovics, Z.; Fineberg, N.A.; Rumpf, H.J.; Yücel, M.; et al. Expert appraisal of criteria for assessing gaming disorder: An international Delphi study. Addiction 2021, 116, 2463–2475. [Google Scholar] [CrossRef]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.S. Clinical characteristics of diagnosis for internet gaming disorder: Comparison of DSM-5 IGD and ICD-11 GD diagnosis. J. Clin. Med. 2019, 8, 945. [Google Scholar] [CrossRef] [PubMed]
- Martin-Fernandez, M.; Matali, J.L.; Garcia-Sanchez, S.; Pardo, M.; Lleras, M.; Castellano-Tejedor, C. Adolescents with Internet Gaming Disorder (IGD): Profiles and treatment response. Addiciones 2016, 29, 125–133. [Google Scholar] [CrossRef]
- Bozkurt, H.; Coskun, M.; Ayaydin, H.; Adak, I.; Zoroglu, S.S. Prevalence and patterns of psychiatric disorders in referred adolescents with Internet addiction. Psychiatry Clin. Neurosci. 2013, 67, 352–359. [Google Scholar] [CrossRef]
- Rodrigo-Yanguas, M.; González-Tardón, C.; Bella-Fernández, M.; Blasco-Fontecilla, H. Serious video games: Angels or demons in patients with Attention-Deficit Hyperactivity Disorder? A quasi-systematic review. Front. Psychiatry 2022, 13, 798480. [Google Scholar] [CrossRef] [PubMed]
- Strahler Rivero, T.; Herrera Núñez, L.M.; Uehara Pires, E.; Amodeo Bueno, O.F. ADHD rehabilitation through video gaming: A systematic review using Primsa guidelines of the current findings and the associated risk of bias. Front. Psychiatry 2015, 6, 151. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Hong, J.S.; Han, D.H.; Min, K.J.; Lee, Y.S.; Kee, B.S.; Kim, S.M. Comparison of QEEG findings between adolescents with Attention Deficit Hyperactivity Disorder (ADHD) without comorbidity and ADHD comorbid with Internet gaming disorder. J. Korean Med. Sci. 2017, 32, 514–521. [Google Scholar] [CrossRef]
- Lee, J.; Bae, S.; Kim, B.N.; Han, D.H. Impact of attention-deficit/hyperactivity disorder comorbidity on longitudinal course in Internet gaming disorder: A 3-year clinical cohort study. J. Child Psychol. Psychiatry Allied Discip. 2021, 62, 1110–1119. [Google Scholar] [CrossRef]
- Kim, M.; Kim, D.; Bae, S.; Han, D.H.; Jeong, B. Aberrant structural network of comorbid attention deficit/hyperactivity disorder is associated with addiction severity in internet gaming disorder. Neuroimage Clin. 2020, 27, 102263. [Google Scholar] [CrossRef]
- Han, D.H.; Kim, S.M.; Bae, S.; Renshaw, P.F.; Anderson, J.S. Brain connectivity and psychiatric comorbidity in adolescents with Internet gaming disorder. Addict. Biol. 2017, 22, 802–812. [Google Scholar] [CrossRef]
- Chang, C.H.; Chang, Y.C.; Cheng, H.; Tzang, R.F. Treatment efficacy of internet gaming disorder with Attention Deficit Hyperactivity Disorder and Emotional Dysregulaton. Int. J. Neuropsychopharmacol. 2020, 23, 349–355. [Google Scholar] [CrossRef]
- Chang, Y.-C.; Tzang, R.-F. Proposing and validating the diagnosis scale for Internet Gaming Disorder in Taiwanese ADHD adolescents: Likert scale method based on the DSM-5. Int. J. Environ. Res. Public Health 2021, 18, 1492. [Google Scholar] [CrossRef] [PubMed]
- Tzang, R.-F.; Chang, C.-H.; Chang, Y.-C. Structural Equation Modeling (SEM): Gaming Disorder leading untreated Attention-Deficit/Hyperactivity Disorder to Disruptive Mood Dysregulation. Int. J. Environ. Res. Public Health 2022, 19, 6648. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, A.; Yaacov, Y.; Manning, M.; Danon, P.; Weizman, A. Internet addiction and Attention Deficit Hyperactivity Disorder among schoolchildren. Isr. Med. Assoc. J. 2015, 17, 731–734. [Google Scholar] [PubMed]
- Berloffa, S.; Salvati, A.; D’Acunto, G.; Fantozzi, P.; Inguaggiato, E.; Lenzi, F.; Milone, A.; Muratori, P.; Pfanner, C.; Ricci, F.; et al. Internet Gaming Disorder in children and adolescents with Attention Deficit Hyperactivity Disorder. Children 2022, 9, 428. [Google Scholar] [CrossRef]
- Hygen, B.W.; Skalická, V.; Stenseng, F.; Belsky, J.; Steinsbekk, S.; Wichstrøm, L. The co-occurrence between symptoms of internet gaming disorder and psychiatric disorders in childhood and adolescence: Prospective relations or common causes? J. Child Psychol. Psychiatry 2020, 61, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Vadlin, S.; Åslund, C.; Hellström, C.; Nilsson, K.W. Associations between problematic gaming and psychiatric symptoms among adolescents in two samples. Addict. Behav. 2016, 61, 8–15. [Google Scholar] [CrossRef]
- Han, D.H.; Bae, S.; Hong, J.; Kim, S.M.; Son, Y.D.; Renshaw, P. Resting-state fMRI study of ADHD and Internet Gaming Disorder. J. Atten. Disor. 2021, 25, 1080–1095. [Google Scholar] [CrossRef]
- Menendez-Garcia, A.; Jimenez-Arroyo, A.; Rodrigo-Yanguas, M.; Marín-Vila, M.; Sánchez-Sánchez, F.; Román-Riechmann, E.; Blasco-Fontecilla, H. Internet, video game and mobile phone addiction in children and adolescents diagnosed with ADHD: A case-control study. Adicciones 2020, 34, 1469. [Google Scholar] [CrossRef]
- André, F.; Munck, I.; Håkansson, A.; Claesdotter-Knutsson, E. Game addiction scale for adolescents-psychometric analyses of gaming behavior, gender differences and ADHD. Front. Psychiatry 2022, 13, 791254. [Google Scholar] [CrossRef]
- Mazurek, M.O.; Engelhardt, C.R. Video game use in boys with autism spectrum disorder, ADHD, or typical development. Pediatrics 2013, 132, 260–266. [Google Scholar] [CrossRef]
- Haghbin, M.; Shaterian, F.; Hosseinzadeh, D.; Griffiths, M.D.A. brief report on the relationship between self-control, video game addiction and academic achievement in normal and ADHD students. J. Behav. Addict. 2013, 2, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Stenseng, F.; Hygen, B.W.; Wichstrøm, L. Time spent gaming and psychiatric symptoms in childhood: Cross-sectional associations and longitudinal effects. Eur. Child Adolesc. Psychiatry 2020, 29, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Gentile, D.A.; Swing, E.; Lim, C.G.; Khoo, A. Video game playing, attention problems, and impulsiveness: Evidence of bidirectional causality. Psychol. Pop. Media Cult. 2012, 1, 62–70. [Google Scholar] [CrossRef]
- Gao, X.; Zhang, M.; Yang, Z.; Wen, M.; Huang, H.; Zheng, R.; Wang, W.; Wei, Y.; Cheng, J.; Han, S.; et al. Structural and functional brain abnormalities in Internet Gaming Disorder and Attention-Deficit/Hyperactivity Disorder: A comparative Meta-analysis. Front. Psychiatry 2021, 12, 679437. [Google Scholar] [CrossRef] [PubMed]
- Nikkelen, S.W.; Valkenburg, P.M.; Huizinga, M.; Bushman, B.J. Media use and ADHD-related behaviors in children and adolescents: A meta-analysis. Dev. Psychol. 2014, 50, 2228–2241. [Google Scholar] [CrossRef]
- Stevens, M.W.; Dorstyn, D.; Delfabbro, P.H.; King, D.L. Global prevalence of gaming disorder: A systematic review and meta-analysis. Aust. N. Z. J. Psychiatry 2020, 2020, 4867420962851. [Google Scholar] [CrossRef]
- Paulus, F.W.; Ohmann, S.; von Gontard, A.; Popow, C. Internet gaming disorder in children and adolescents: A systematic review. Dev. Med. Child Neurol. 2018, 60, 645–659. [Google Scholar] [CrossRef]
- Desai, R.A.; Krishnan-Sarin, S.; Cavallo, D.; Potenza, M.N. Video-gaming among high school students: Health correlates, gender differences, and problematic gaming. Pediatrics 2010, 126, e1414–e1424. [Google Scholar] [CrossRef]
- Slobodin, O.; Davidovitch, M. Gender differences in objective and subjective measures of ADHD among clinic-referred children. Front. Hum. Neurosci. 2019, 13, 441. [Google Scholar] [CrossRef]
- Marmet, S.; Studer, J.; Grazioli, V.S.; Gmel, G. Bidirectional associations between self-reported gaming disorder and adult attention deficit hyperactivity disorder: Evidence from a sample of young Swiss men. Front. Psychiatry 2018, 9, 649. [Google Scholar] [CrossRef]
- Chou, W.J.; Liu, T.L.; Yang, P.; Yen, C.F.; Hu, H.F. Multi-dimensional correlates of Internet addiction symptoms in adolescents with attention-deficit/hyperactivity disorder. Psychiatry Res. 2015, 225, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Dalbudak, E.; Evren, C. The relationship of Internet addiction severity with attention deficit hyperactivity disorder symptoms in Turkish University students; impact of personality traits, depression and anxiety. Compr. Psychiatry 2014, 55, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Granic, I.; Lobel, A.; Engels, R.C. The benefits of playing video games. Am. Psychol. 2014, 69, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Tahiroglu, A.; Celik, G.; Avci, A.; Seydaoglu, G.; Uzel, M.; Altunbas, H. Short- term effects of playing computer games on attention. J. Atten. Disord. 2010, 13, 668–676. [Google Scholar] [CrossRef]
- Lawrence, V.; Houghton, S.; Tannock, R.; Douglas, G.; Durkin, K.; Whiting, K. ADHD outside the laboratory: Boys’ executive function performance on tasks in videogame play and on a visit to the zoo. J. Abnorm. Child. Psychol. 2002, 30, 447–462. [Google Scholar] [CrossRef]
- Wilkinson, N.; Ang, R.P.; Goh, D.H. Online video game therapy for mental health concerns: A review. Int. J. Soc. Psychiatry 2008, 54, 370–382. [Google Scholar] [CrossRef]
- Lau, H.M.; Smit, J.H.; Fleming, T.M.; Riper, H. Serious games for mental health: Are they accessible, feasible, and effective? A systematic review and meta-analysis. Front. Psychiatry 2017, 7, 209. [Google Scholar] [CrossRef]
- Lim, C.G.; Lim-Ashworth, N.S.; Fung, D.S. Updates in technology-based interventions for attention deficit hyperactivity disorder. Curr. Opin. Psychiatry 2020, 33, 577. [Google Scholar] [CrossRef]
- Pandian, G.S.B.; Jain, A.; Raza, Q.; Sahu, K.K. Digital health interventions (DHI) for the treatment of attention deficit hyperactivity disorder (ADHD) in children-a comparative review of literature among various treatment and DHI. Psychiatry Res. 2021, 297, 113742. [Google Scholar] [CrossRef]
- Vajawat, B.; Varshney, P.; Banerjee, D. digital gaming interventions in psychiatry: Evidence, applications and challenges. Psychiatry Res. 2020, 295, 113585. [Google Scholar] [CrossRef]
- van der Oord, S.; Ponsionen, A.J.G.B.; Geurts, H.M.; Ten Brink, E.L.; Prins, P.J.M.A. Pilot study of the efficacy of a computerized executive functioning remediation training with game elements for children with ADHD in an outpatient setting:outcome on parent- and teacher-rated executive functioning and ADHD behavior. J. Atten. Disord. 2014, 18, 699–712. [Google Scholar] [CrossRef] [PubMed]
- Weerdmeester, J.; Cima, M.; Granic, I.; Hashemian, Y.; Gotsis, M. A feasibility study on the effectiveness of a full-body videogame intervention for decreasing attention deficit hyperactivity disorder symptoms. Games Health J. 2016, 5, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Bikic, A.; Christensen, T.Ø.; Leckman, J.F.; Bilenberg, N.; Dalsgaard, S. A doubleblind randomized pilot trial comparing computerized cognitive exercises to Tetris in adolescents with attention-deficit/hyperactivity disorder. Nord J. Psychiatry 2017, 71, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Loo, B.R.Y.; Castellanos, F.X.; Liu, S.; Koh, H.L.; Poh, X.W.W.; Krishnan, R.; Fung, D.; Chee, M.W.L.; Guan, C.; et al. Brain-computer-interface-based intervention re-normalizes brain functional network topology in children with attention deficit/hyperactivity disorder. Transl. Psychiatry 2018, 8, 149. [Google Scholar] [CrossRef]
- Hahn-Markowitz, J.; Berger, I.; Manor, I.; Maeir, A. Efficacy of cognitivefunctional (Cog-Fun) occupational therapy intervention among children with ADHD: An RCT. J. Atten. Disord. 2020, 24, 655–666. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.D.; Vitulano, L.A.; Katsovich, L.; Li, S.; Moore, C.; Li, F.; Grantz, H.; Zheng, X.; Eicher, V.; Guloksuz, S.A.; et al. A randomized controlled trial of an integrated brain, body, and social intervention for children with ADHD. J. Atten. Disord. 2020, 24, 780–794. [Google Scholar] [CrossRef] [PubMed]
- Bikic, A.; Leckman, J.F.; Christensen, T.Ø.; Bilenberg, N.; Dalsgaard, S. Attention and executive functions computer training for attention-deficit/hyperactivity disorder (ADHD): Results from a randomized, controlled trial. Eur. Child. Adolesc. Psychiatry 2018, 27, 1563–1574. [Google Scholar] [CrossRef]
- Benzing, V.; Schmidt, M. The effect of exergaming on executive functions in children with ADHD: A randomized clinical trial. Scand. J. Med. Sci. Sports 2019, 29, 1243–1253. [Google Scholar] [CrossRef]
- Bush, G. Cingulate, frontal, and parietal cortical dysfunction in attention-deficit/hyperactivity disorder. Biol. Psychiatry 2011, 69, 1160–1167. [Google Scholar] [CrossRef]
- Haber, S.N.; Knutson, B. The reward circuit: Linking primate anatomy and human imaging. Neuropsychopharmacol. 2010, 35, 4–26. [Google Scholar] [CrossRef]
- Yao, Y.W.; Liu, L.; Ma, S.S.; Shi, X.H.; Zhou, N.; Zhang, J.T.; Potenza, M.N. Functional and structural neural alterations in Internet gaming disorder: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2017, 83, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, M.T.; McHugh, M.J.; Pariyadath, V.; Stein, E.A. Resting state functional connectivity in addiction: Lessons learned and a road ahead. Neuroimage 2012, 62, 2281–2295. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Deng, W.; Wang, H.; Guo, W.; Li, T. The prefrontal dysfunction in individuals with Internet gaming disorder: A meta-analysis of functional magnetic resonance imaging studies. Addict. Biol. 2015, 20, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Etkin, A.; Egner, T.; Kalisch, R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn. Sci. 2011, 15, 85–93. [Google Scholar] [CrossRef]
- Kennerley, S.W.; Walton, M.E.; Behrens, T.E.; Buckley, M.J.; Rushworth, M.F. Optimal decision making and the anterior cingulate cortex. Nat. Neurosci. 2006, 9, 940–947. [Google Scholar] [CrossRef]
- Bonath, B.; Tegelbeckers, J.; Wilke, M.; Flechtner, H.-H.; Krauel, K. Regional gray matter volume differences between adolescents with ADHD and typically developing controls: Further evidence for anterior cingulate involvement. J. Atten. Disord. 2018, 22, 627–638. [Google Scholar] [CrossRef]
- Lin, X.; Dong, G.; Wang, Q.; Du, X. Abnormal gray matter and white matter volume in ’Internet gaming addicts’. Addict. Behav. 2015, 40, 137–143. [Google Scholar] [CrossRef]
- Cavanna, A.E.; Trimble, M.R. The precuneus: A review of its functional anatomy and behavioural correlates. Brain. 2006, 129, 564–583. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, J.; Fan, L.; Zhang, Y.; Fox, P.T.; Eickhoff, S.B.; Yu, C.; Jiang, T. Functional organization of the fusiform gyrus revealed with connectivity profiles. Hum. Brain Mapp. 2016, 37, 3003–3016. [Google Scholar] [CrossRef]
- Zhu, Y.; Yang, D.; Ji, W.; Huang, T.; Xue, L.; Jiang, X.; Chen, L.; Wang, F. The relationship between neurocircuitry dysfunctions and Attention Deficit Hyperactivity Disorder: A review. BioMed. Res. Int. 2016, 2016, 3821579. [Google Scholar] [CrossRef]
- Massat, I.; Slama, H.; Kavec, M.; Linotte, S.; Mary, A.; Baleriaux, D.; Metens, T.; Mendlewicz, J.; Peigneux, P. Working memory-related functional brain patterns in never medicated children with ADHD. PLoS ONE 2012, 7, e49392. [Google Scholar] [CrossRef] [PubMed]
- Baroni, A.; Castellanos, F.X. Neuroanatomic and cognitive abnormalities in attention-deficit/ hyperactivity disorder in the era of ‘high definition’ neuroimaging. Curr. Opin. Neurobiol. 2015, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tripp, G.; Wickens, J.R. Research review: Dopamine transfer deficit: A neurobiological theory of altered reinforcement mechanisms in {ADHD}. J. Child. Psychol. Psychiatry 2008, 49, 691–704. [Google Scholar] [CrossRef] [PubMed]
- Luman, M.; Tripp, G.; Scheres, A. Identifying the neurobiology of altered reinforcement sensitivity in ADHD: A review and research agenda. Neurosci. Biobehav. Rev. 2010, 34, 744–754. [Google Scholar] [CrossRef] [PubMed]
- Plichta, M.M.; Scheres, A. Ventral-striatal responsiveness during reward anticipation in ADHD and its relation to trait impulsivity in the healthy population: A meta-analytic review of the fMRI literature. Neurosci. Biobehav. Rev. 2014, 38, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, E.; Bado, P.; Tripp, G.; Mattos, P.; Wickens, J.R.; Bramati, I.E.; Alsop, B.; Ferreira, F.M.; Lima, D.; Tovar-Moll, F.; et al. Abnormal striatal {BOLD} responses to reward anticipation and reward delivery in {ADHD}. PLoS ONE 2014, 9, e89129. [Google Scholar] [CrossRef]
- Costa Dias, T.G.; Wilson, V.B.; Bathula, D.R.; Iyer, S.; Mills, K.L.; Thurlow, B.L.; Stevens, C.A.; Musser, E.D.; Carpenter, S.D.; Grayson, D.S.; et al. Reward circuit connectivity relates to delay discounting in children with attention-deficit/ hyperactivity disorder. Eur. Neuropsychopharmacol. 2012, 23, 33–45. [Google Scholar] [CrossRef]
- Marsh, P.J.; Williams, L.M. ADHD and schizophrenia phenomenology: Visual scanpaths to emotional faces as a potential psychophysiological marker? Neurosci. Biobehav. Rev. 2006, 30, 651–665. [Google Scholar] [CrossRef]
- Ibáñez, A.; Petroni, A.; Urquina, H.; Torrente, F.; Torralva, T.; Hurtado, E.; Guex, R.; Blenkmann, A.; Beltrachini, L.; Muravchik, C.; et al. Cortical deficits of emotional face processing in adults with ADHD: Its relation to social cognition and executive function. Soc. Neurosci. 2011, 6, 464–481. [Google Scholar] [CrossRef]
- Uekermann, J.; Kraemer, M.; Abdel-Hamid, M.; Schimmelmann, B.G.; Hebebrand, J.; Daum, I. Social cognition in attention-deficit hyperactivity disorder (ADHD). Neurosci. Biobehav. Rev. 2010, 34, 734–743. [Google Scholar] [CrossRef]
- Salerno, L.; Makris, N.; Pallanti, S. Sleep disorders in adult ADHD: A key feature. J. Psychopathol. 2016, 22, 135–140. [Google Scholar]
- Makris, N.; Biederman, J.; Monuteaux, M.C.; Seidman, L.J. Towards conceptualizing a neural systems-based anatomy of attention-deficit/hyperactivity disorder. Dev. Neurosci. 2009, 31, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Zambrano-Vazquez, L.; Levy, H.C.; Belleau, E.L.; Dworkin, E.R.; Howard Sharp, K.M.; Pittenger, S.L.; Schumacher, J.A.; Coffey, S.F. Using the research domain criteria framework to track domains of change in comorbid PTSD and SUD. Psychol. Trauma 2017, 9, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Kwako, L.E.; Momenan, R.; Litten, R.Z.; Koob, G.F.; Goldman, D. Addictions neuroclinical assessment: A neurosciencebased framework for addictive disorders. Biol. Psychiatry 2016, 80, 179–189. [Google Scholar] [CrossRef]
- Lee, S.Y.; Lee, H.K.; Jeong, H.; Yim, H.W.; Bhang, S.Y.; Jo, S.J.; Baek, K.Y.; Kim, E.; Kim, M.S.; Choi, J.S.; et al. The hierarchical implications of internet gaming disorder criteria: Which indicate more severe pathology? Psychiatry Investig. 2017, 14, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Li, R.; Li, S.; Zhang, Y.; Yang, S.; Ning, H. A review on serious games for ADHD. arXiv 2021, arXiv:abs/2105.02970. Available online: https://arxiv.org/abs/2105.02970 (accessed on 7 July 2022).
- Loo, S.K.; Bilder, R.M.; Cho, A.L.; Sturm, A.; Cowen, J.; Walshaw, P.; Levitt, J.; Del’Homme, M.; Piacentini, J.; McGough, J.J. Effects of D-methylphenidate, guanfacine, and their combination on electroencephalogram resting state spectral power in attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 674–682. [Google Scholar] [CrossRef]
- Han, D.H.; Lee, Y.S.; Na, C.; Ahn, J.Y.; Chung, U.S.; Daniels, M.A.; Haws, C.A.; Ren-Shaw, P.F. The effect of methylphenidate on Internet video game play in children with attention-deficit/hyperactivity disorder. Compr. Psychiatry 2009, 50, 251–256. [Google Scholar] [CrossRef]
- Metin, B.; Krebs, R.M.; Wiersema, J.R.; Verguts, T.; Gasthuys, R.; van der Meere, J.J.; Achten, E.; Roeyers, H.; Sonuga-Barke, E. Dysfunctional modulation of default mode network activity in attention-deficit/hyperactivity disorder. J. Abnorm. Psychol. 2015, 124, 208–214. [Google Scholar] [CrossRef]
- Howard-Jones, P.A.; Jay, T.; Mason, A.; Jones, H. Gamification of learning deactivates the default mode network. Front. Psychol. 2016, 6, 1891. [Google Scholar] [CrossRef]
- Weinstein, A.; Weizman, A. Emerging association between addictive gaming and attention-deficit/hyperactivity disorder. Curr. Psychiatry Rep. 2012, 14, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Yen, J.Y.; Yen, C.F.; Chen, C.S.; Tang, T.C.; Ko, C.H. The association between adult ADHD symptoms and internet addiction among college students: The gender difference. Cyberpsychol. Behav. 2009, 12, 18–91. [Google Scholar] [CrossRef]
- Stavropoulos, V.; Adams, B.L.M.; Beard, C.L.; Dumble, E.; Trawley, S.; Gomez, R.; Pontes, H.M. Associations between attention deficit hyperactivity and internet gaming disorder symptoms: Is there consistency across types of symptoms, gender and countries? Addict. Behav. Rep. 2019, 9, 100158. [Google Scholar] [CrossRef]
- Grusser, S.M.; Thalemann, R.; Albrecht, U.; Thalemann, C.N. Excessive computer usage in adolescents—Results of a psychometric evaluation. Wien Klin Wochenschr. 2005, 117, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Thalemann, R.; Wolfling, K.; Grusser, S.M. Specific cue reactivity on computer game-related cues in excessive gamers. Behav. Neurosci. 2007, 121, 614–618. [Google Scholar] [CrossRef]
- Jeong, E.J.; Ferguson, C.J.; Lee, S.J. Pathological gaming in young adolescents: A longitudinal study focused on academic stress and self-control in South Korea. J. Youth Adolesc. 2019, 48, 2333–2342. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.; King, D.; Delfabbro, P. Family factors in adolescent problematic Internet gaming: A systematic review. J. Behav. Addict. 2017, 6, 321–333. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Bueso, V.; Santamaria, J.J.; Fernandez, D.; Merino, L.; Montero, E.; Jimenez-Murcia, S.; del Pino-Gutiérrez, A.; Ribas, J. Internet gaming disorder in adolescents: Personality, psychopathology and evaluation of a psychological intervention combined with parent psychoeducation. Front. Psychol. 2018, 9, 787. [Google Scholar] [CrossRef]
- Han, J.; Seo, Y.; Hwang, H.; Kim, S.M.; Han, D.H. Efficacy of cognitive behavioural therapy for internet gaming disorder. Clin. Psychol. Psychother. 2020, 27, 203–213. [Google Scholar] [CrossRef]
- Torres-Rodriguez, A.; Griffiths, M.D.; Carbonell, X.; Oberst, U. Treatment efficacy of a specialized psychotherapy program for Internet Gaming Disorder. J. Behav. Addict. 2018, 7, 939–952. [Google Scholar] [CrossRef]
- Hornstra, R.; van der Oord, S.; Staff, A.I.; Hoekstra, P.J.; Oosterlaan, J.; van der Veen-Mulders, L.; Luman, M.; van den Hoofdakker, B.J. Which techniques work in behavioral parent training for children with ADHD? A randomized controlled microtrial. J. Clin. Child Adolesc. Psychol. 2021, 50, 888–903. [Google Scholar] [CrossRef] [PubMed]
- Döpfner, M.; Wähnke, L.; Klemp, M.T.; Mühlenmeister, J.; Schürmann, S.; Hellmich, M.; Plück, J. Efficacy of web-assisted self-help for parents of children with ADHD (WASH)—A three-arm randomized trial under field/routine care conditions in Germany. BMC Psychiatry 2020, 20, 76. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, P.A.; Goldman, D. Neuromodulation interventions for addictive disorders: Challenges, promise, and roadmap for future research. Brain 2017, 140, 1183–1203. [Google Scholar] [CrossRef]
- Gomis-Vicent, E.; Thoma, V.; Turner, J.J.D.; Hill, K.P.; Pascual-Leone, A. Review: Non-invasive brain stimulation in behavioral addictions: Insights from direct comparisons with substance use disorders. Am. J. Addict. 2019, 28, 431–454. [Google Scholar] [CrossRef] [PubMed]
- Aarseth, E.; Bean, A.M.; Boonen, H.; Colder Carras, M.; Coulson, M.; Das, D.; Deleuze, J.; Dunkels, E.; Edman, J.; Ferguson, C.J.; et al. Scholars’ open debate paper on the world health organization ICD-11 gaming disorder proposal. J. Behav. Addict. 2017, 6, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Bean, A.M.; Nielsen, R.K.L.; van Rooij, A.J.; Ferguson, C.J. Video game addiction: The push to pathologize video games. Prof. Psychol. Res. Pract. 2017, 48, 378–389. [Google Scholar] [CrossRef]
- Billieux, J.; Flayelle, M.; Rumpf, H.-J.; Stein, D.J. High involvement versus pathological involvement in video games: A crucial distinction for ensuring the validity and utility of gaming disorder. Curr. Addict. Rep. 2019, 6, 323–330. [Google Scholar] [CrossRef]
| Authors (Year) | Study Design | Sample | Age (Years) | Assessment Tool for IGD | Outcomes |
|---|---|---|---|---|---|
| Hygen, B. W. et al. (2020) [28] | Cross-sectional | N = 702 children and adolescents | 10–14 | Internet-Gaming Disorder Interview (IGDI); Child and Adolescent Psychiatric Assessment (CAPA) | At all ages there was a positive and significant correlation between IGD symptoms and those of ADHD, anxiety, depression, and ODD/CD. More IGD symptoms were associated with more ADHD, anxiety, and ODD/CD symptoms but not depression at the between-group level. |
| Vadlin, S. et al. (2016) [29] | Cross-sectional | Community sample: N = 1868; Clinical sample: N = 242 adolescents (male = 834; 44.6%; female = 1034; 55.4%) | Community sample: aged 12–16 (mean age = 13.9); Clinical sample: aged 12–18 (mean age = 15.39) | Gaming Addiction Identification Test (GAIT); for psychiatric symptoms: Adult ADHD Self-Report Scale Adolescent version (ASRS-A); Depression Self-Rating Scale Adolescent version (DSRS-A); Spence Children’s Anxiety Scale (SCAS); psychotic-like experiences (PLEs) | Girls constituted 55.4% of the community sample and 69.8% of the total sample (p < 0.001). A total of 21.3% of the problematic gamers belonging to the community sample had symptoms of ADHD vs 42.3% belonging to the clinical sample (p = 0.019). ADHD symptoms were associated with ORs of 2.43 (95% CI, 1.44–4.11) with respect to coexisting problematic gaming. |
| Han, D. H. et al. (2021) [30] | Case-control | N = 113 adolescents (29 ADHD + IGD; 20 pure IGD; 26 pure ADHD; 38 HC) | 14–15 | Korean–Wechsler Adult Intelligence Scale (K-WAIS); Korean version of Dupaul’s ADHD-Rating Scale (K-ADHD); Korean Young’s Internet Addiction Rating Scale (YIAS-K); Children’s Depression Inventory (CDI); Beck Anxiety Inventory (BAI); Behavioral Inhibitory System/Behavioral Activation System (BIS/BAS) Scale; Clinical Global Impression-Improvement Scale (CGI-I) | At the baseline, in the all-ADHD and all-IGD groups, the Functional Connectivity (FC) from the right-middle frontal gyrus to the caudate as well as the FC from the left cingulate to caudate were reduced in comparison to HC. After one year of treatment for ADHD and IGD symptoms there was an increase in the FC between the cortex and subcortex in both all-ADHD and all-IGD participants with a good prognosis in comparison with participants with poor prognoses. |
| Park, J. H. et al. (2017) [19] | Case-control | ADHD+IGD group: N = 16 male adolescents; ADHD-only group: N = 15 male adolescents; HC group: N = 14 male adolescents. | ADHD+IGD group: mean age = 14.6 ± 1.9; ADHD-only group: mean age = 13.7 ± 0.8; HC group: mean age = 14.4 ± 1.7 | Korean ADHD-Rating Scale (K-ARS); Young’s Internet Addiction Scale (YIAS) | Adolescents with ADHD who also had a problematic Internet use showed differences in qEEG in comparison with those with only ADHD; specifically, ADHD+IGD comorbidity presented lower relative delta power and greater relative beta power compared to adolescents with only ADHD. |
| Chang, C. H., et al. (2020) [23] | Cross-sectional | N = 101 ADHD children and adolescents (49 without Internet Addiction; 52 with Internet Addiction. Male = 69, 68.32%; Female = 32, 31.68%) | 7–18 | Chen Internet Addiction Scale (CIA); Swanson, Nolan and Pelham, Version IV Questionnaire (SNAP-IV) | Internet-addicted ADHD youths showed increased comorbidity with DMDD, such as emotional dysregulation, than ADHD youths without IGD and had poorer interpersonal relationships. The efficacy of IGD treatment was good when the underlying ADHD symptomatology was controlled. IGD can lead to severe emotional dysregulation. |
| Menéndez-García, A. et al. (2022) [31] | Case-control | N = 112 children and adolescents (51 with ADHD; 61 without ADHD) | 7–17 | TEA questionnaire for the assessment of executive function and ADHD (ATENTO); ADITEC questionnaire (ADITEC) | ADHD is a risk factor for developing IAD and IGD, with good social adaptation buffering such an association. ADHD combined type and predominantly hyper active/impulsive type were each associated with IGD. Gender vulnerability to IGD and MPA was reported since there was an association between female gender and MPA and an association between male gender and IGD. |
| Lee, J. et al. (2021) [20] | Prospective cohort | N = 255 patients (128 = Pure-IGD, 127 = ADHD-IGD. Male = 246, 96.47%; Female = 9, 3.53%) | 11–42 | Young’s Internet Addiction Scale (YIAS); Korean ADHD-rating scale (ADHD-RS); Beck’s Depression Inventory (BDI); Beck’s Anxiety Inventory (BAI); Social Avoidance and Distress Scale (SADS); Family Environment Scale (FES) | Individuals with both ADHD and IGD showed a lower recovery probability compared to individuals with only (pure) IGD (p < 0.001) and a higher probability of recurrence over the follow-up period (p = 0.006). Changes in symptoms of ADHD were greatly associated with changes in symptoms of IGD. |
| Haghbin, M. et al. (2013) [34] | Cross-sectional | N = 326 high school students. 146 (49.1%) females, 166 (50.9%) males | 14–18 | Computer and Video Game Addiction Scale; Self-control Scale; Diagnostic Checklist and Self-report Scale; Grade Point Average (GPA) | There was a significantly different relationship between self-control, video game addiction, and academic achievement between normal and ADHD students. The shared factor between ADHD, self-control, and video game addiction was impulsivity. Males showed higher probability of being addicted to video games than females. |
| Chang, Y. C. et al. (2021) [24] | Cross-sectional | N = 102 children and adolescents (Male = 70, 68.63%; Female = 32, 31.37%) | 7–18 (mean age = 11.16 ± 3.35) | Chen Internet Addiction Scale (CIA); Swanson, Nolan, and Pelham, Version IV Questionnaire (SNAP-IV) | Youth with ADHD showed more pathological videogaming activity, greater loss of control, and more conflictual and withdrawal tendencies compared to youth with ADHD but without IGD. In those with IGD, there was a more severe inattentive symptomatology, more emotional difficulties, and more mood dysregulation disorders. Moreover, they spent more time in gaming or chatting online daily and during weekends, and their interpersonal relationships were poorer than those without IGD. |
| Kim, M. et al. (2020) [21] | Case-control | N = 46 male IGD+ADHD patients; N = 48 male IGD-ADHD patients; N = 34 HC | 15–26 | Young’s Internet Addiction Scale (YIAS), Korean Kiddie Schedule for Affective Disorders and Schizophrenia; Dupaul’s ADHD scale—Korean version (K-ARS-P) | Symptomatic associations between IGD and ADHD were found and abnormal increases in some structural connections within circuitry pertaining to inhibitory function or sensory integration can point out how the ADHD comorbidity is associated with addiction severity in IGD. |
| Weinstein, A. et al. (2015) [26] | Case-control | N = 100 schoolchildren and adolescents (N = 50 with ADHD; N = 50 without ADHD) | 13–15 | Young’s Internet Addiction Test (IAT) | Children and adolescents with ADHD were more addicted to the internet, spent more time online, and went to sleep later at night compared to those without ADHD. |
| Stenseng, F. et al. (2020) [35] | Prospective cohort | N = 905 children at T1 (Male = 458, 50.6%; Female = 447, 49.4%); N = 752 children at T2 (Male = 380, 50.5%; Female = 372, 49.5%); N = 661 children at T3 (Male = 322; 48.7%; Female = 339, 51.3%) | 6–10 | Preschool Age Psychiatric Assessment/Child and Adolescents Psychiatric Assessment (PAPA/CAPA); parents’ reports on gaming behavior | At age 6, more ADHD symptoms and emotional problems did not predict increased gaming activity at age 8, whereas more ADHD symptoms at age 8 predicted increased gaming activity at age 10. Thus, the time spent gaming did not predict more psychiatric problems at these ages, but children with greater ADHD symptomatology were more likely to increase their amount of gaming during middle childhood. |
| Han, D. H. et al. (2017) [22] | Case-control | N = 151 male children and adolescents (N = 78 with IGD, N = 73 without IGD) | 10–19 | Young’s Internet Addiction Scale (YIAS); Beck Depression Inventory (BDI); Beck Anxiety Inventory (BAI); Korean ADHD-rating scales (K-ARS) | Chronic exposure to Internet game play was associated with heightened connectivity between the salience network (anterior insula and dorsal anterior cingulate) and frontal eye fields, between ipsilateral DLPFC and left TPJ, and between motor cortex, auditory cortex, and SMA, which was not explained by comorbidities such as ADHD. Increased connectivity hypothesized as a training effect of prolonged game play, reflecting adaptive functional gain in individuals with a pattern of protracted internet game use. |
| Berloffa, S. et al. (2022) [27] | Case-control | N = 108 children and adolescents (Male = 96, 89%; Female = 12, 11%) | 8–18 (mean age = 11.7 ± 2.6) | Internet Addiction Scale (IAT); Internet Gaming Disorder Scale-Short Form (IGDS9-SF); Clinical Global Impression-Severity score (GCI-S); Children Global Assessment Scale (C-GAS); Conners’ Parent Rating Scale - Revised: Short Form (CPRS-R:S); Use, Abuse, and Dependence on Internet (UADI); Wechsler Intelligence Scale for Children—Fourth Edition (WISC-IV) | ADHD+IGD patients showed more severe ADHD symptoms, more withdrawal/depression and socialization problems, and greater salience of addiction and evasion dimensions. The binary logistic regression revealed that the degree of inattention had a greater weight in determining IGD. |
| Tzang, R. F. et al. (2022) [25] | Case-control | N = 102 ADHD children and adolescents (Male = 70, 68.63%; Female = 32, 31.37% | 8–15 | Chen Internet Addiction Scale (CIAS); Swanson, Nolan, and Pelham Version IC Questionnaire (SNAP-IV) | Youth with ADHD+IGD were significantly more likely to be characterized by poor interpersonal relationships and DMDD-like symptomatology compared to those with only ADHD. IGD played a mediating role in the increase in the risk of disruptive mood dysregulation in youths with ADHD. |
| André, F. et al. (2022) [32] | Cross-sectional | N = 144 children and adolescents (Male = 69, 50.4%; Female = 68, 49.6%) | 8–18 | Game Addiction Scale for Adolescents (GASA) | ADHD increases the risk of over utilization of computer games, and while for boys the negative consequences had a social direction, they were more emotional for girls. |
| Mazurek, M. O. et al. (2013) [33] | Cross-sectional | N = 141 male children and adolescents (N = 56 with ASD, N = 44 with ADHD, N = 41 TD) | 8–18 | Problem Video Game-Playing Test (PVGT); Vanderbilt Attention Deficit/Hyperactivity Disorder Parent Rating Scale (VADPRS); Social Communication Questionnaire-Current (SCQ) | Boys with ASD and ADHD showed higher risk for problematic gaming than boys with TD. Inattentive symptomatology was strongly associated with problematic gaming for both groups. |
| Gao, X.et al. (2021) [37] | Meta-analysis | N = 5454 patients with ADHD and/or IGD compared to HC (Male = 4189, 76.81%; Female = 1265, 23.19%) | 9–37 | IGD diagnosed by using DSM-5 or YIAS or CIAS | IGD and ADHD have common and distinctive structural and functional alterations. IGD showed disorder-differentiating structural alterations in the putamen while ADHD showed aberrations in the orbitofrontal cortex. Disorder-differentiating fMRI activations were predominantly evident in the precuneus among IGD patients and common impairing function connection was present in the reward circuitry. |
| Nikkelen, S. W. et al. (2014) [38] | Meta-analysis | Children and adolescents with ADHD versus control group (Female 42.27%; Male 57.73%) | 0–18 years | Child Behavior Checklist (CBCL); Strenghts and Difficulties Questionnaire (SDQ); Continuous Performance Task (CPT); Attentional Networks Test (ANT); Matching Familiar Figures Test (MFFT); a measure of overall media use | Small significant association between ADHD-related behaviors and use of media. Even though media use was more strongly related to problems with attention than to impulsivity, such a difference was only marginally significant. The ADHD–media use relationship was stronger for boys than for girls. |
| Gentile, D.A. et al. (2012) [36] | Prospective cohort | N = 3034 children/adolescents | 8–17 years (mean age = 11.2, SD = 2.1) | Current ADHD Symptoms Scale Self-Report; Barratt Impulsiveness Scale-11; Self-reports of gaming behavior | Results suggested a bidirectional relationship between video game-playing and ADHD. Children and adolescents with higher impulsiveness and attention difficulties spent more time playing video games, which in turn intensifies consequent problems in attention and impulsiveness. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salerno, L.; Becheri, L.; Pallanti, S. ADHD-Gaming Disorder Comorbidity in Children and Adolescents: A Narrative Review. Children 2022, 9, 1528. https://doi.org/10.3390/children9101528
Salerno L, Becheri L, Pallanti S. ADHD-Gaming Disorder Comorbidity in Children and Adolescents: A Narrative Review. Children. 2022; 9(10):1528. https://doi.org/10.3390/children9101528
Chicago/Turabian StyleSalerno, Luana, Leonardo Becheri, and Stefano Pallanti. 2022. "ADHD-Gaming Disorder Comorbidity in Children and Adolescents: A Narrative Review" Children 9, no. 10: 1528. https://doi.org/10.3390/children9101528
APA StyleSalerno, L., Becheri, L., & Pallanti, S. (2022). ADHD-Gaming Disorder Comorbidity in Children and Adolescents: A Narrative Review. Children, 9(10), 1528. https://doi.org/10.3390/children9101528








