Taking a Closer Look at Social Performance in Childhood Social Anxiety Disorder: Biopsychosocial Context Considerations and Effects of Cognitive Behavior Therapy
Abstract
1. Introduction
1.1. A Stress Model of Social Performance
1.2. The Current Study
2. Materials and Methods
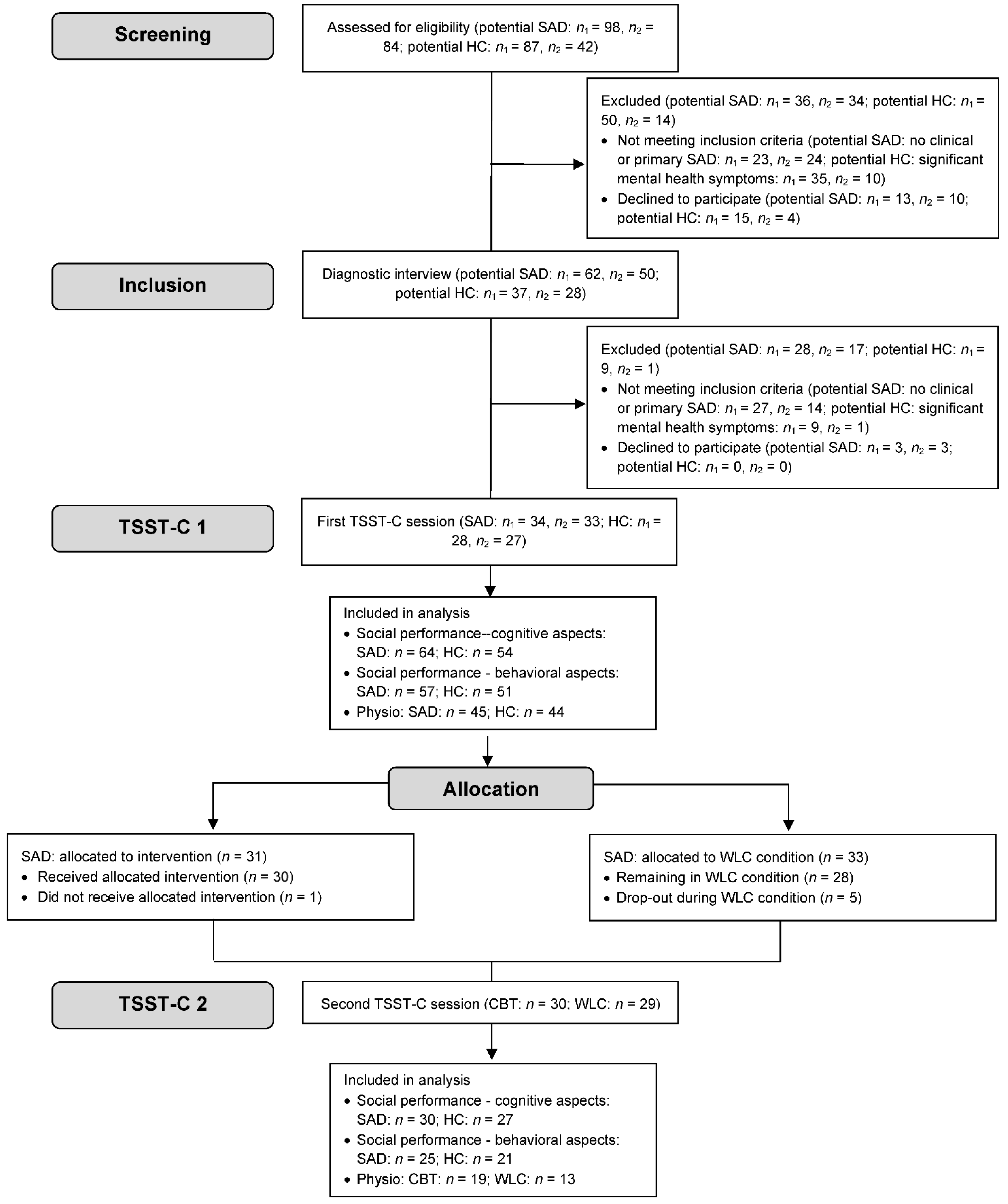
2.1. Study Design
2.2. Participants
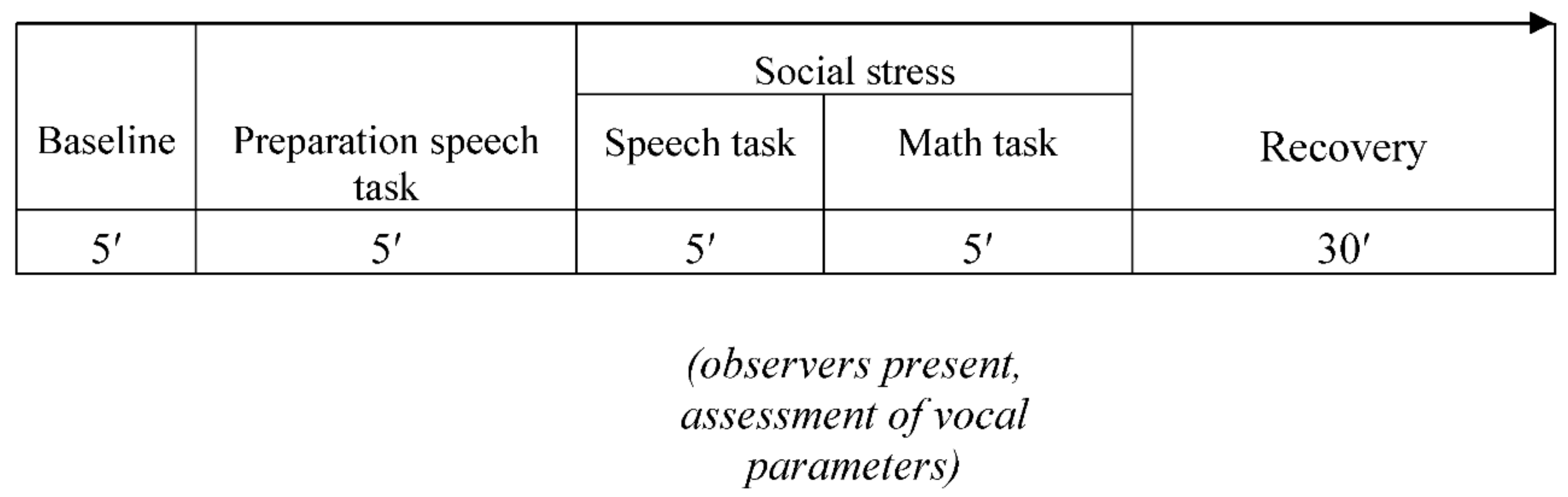
2.3. Procedure
2.4. Psychometric Measures
2.5. Cognitive Measure: Social Performance Self-Report
2.6. Behavioral Measures: Social Performance Other-Report
2.7. Physiological Measures: Vocal Arousal
2.8. Treatment
2.9. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Psychometric Considerations of Self- and Other-Report of Social Performance
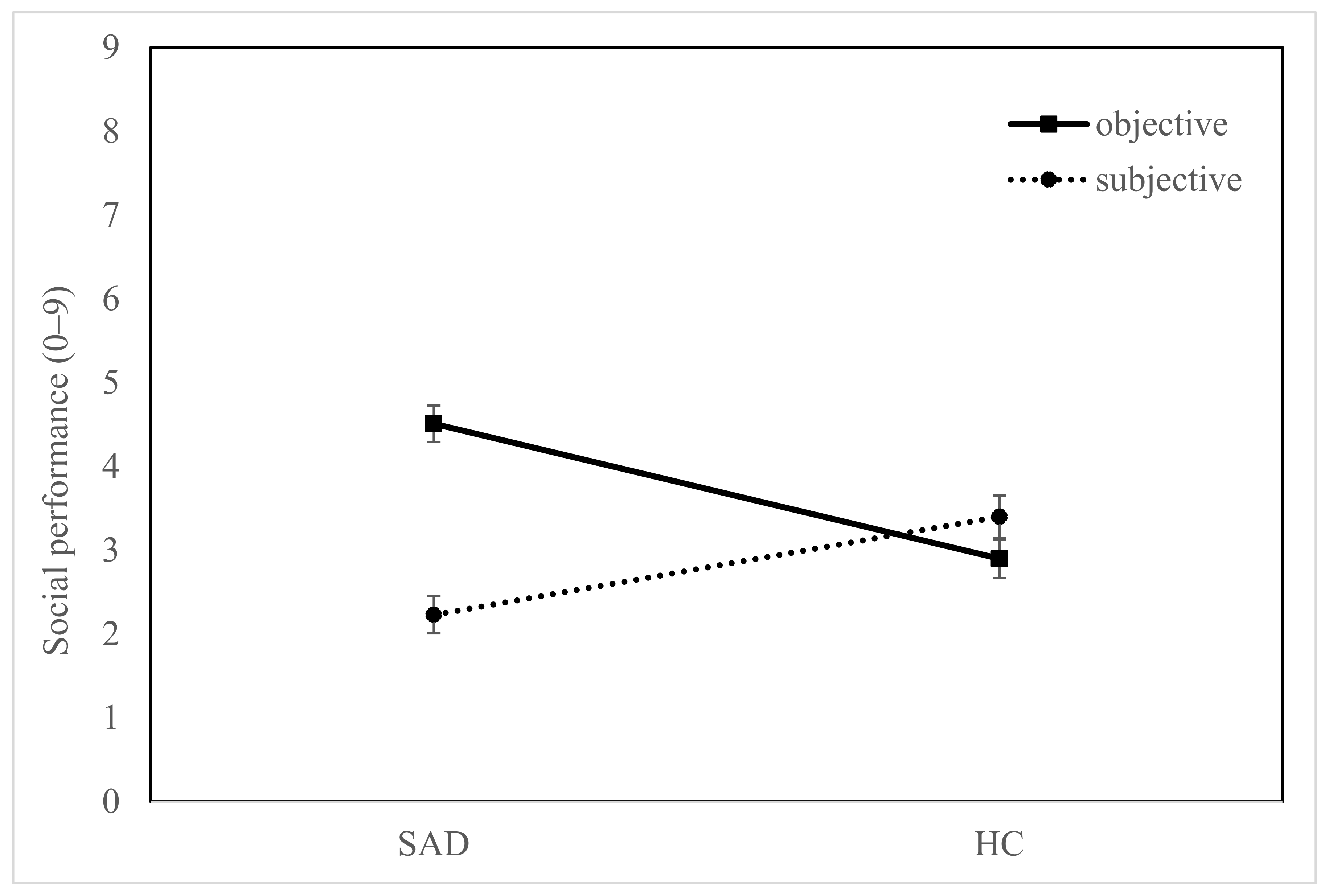
3.3. Social Performance
3.4. Social Performance in Relation to CBT
3.5. Biopsychosocial Considerations of Social Performance
4. Discussion
4.1. The Relevance of Subjective and Objective Social Performance in Childhood SAD
4.2. Implications for a Biopsychosocial Stress Model of Social Performance
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Burstein, M.; He, J.P.; Kattan, G.; Albano, A.M.; Avenevoli, S.; Merikangas, K.R. Social phobia and subtypes in the National Comorbidity Survey-Adolescent Supplement: Prevalence, correlates, and comorbidity. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 870–880. [Google Scholar] [CrossRef] [PubMed]
- Beesdo, K.; Knappe, S.; Pine, D.S. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatr. Clin. N. Am. 2009, 32, 483–524. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.M.; Wells, A. A cognitive model of social phobia. In Social Phobia: Diagnosis, Assessment, and Treatment; Heimberg, R.G., Liebowitz, M., Hope, D., Scheier, F., Eds.; Guilford Press: New York, NY, USA, 1995; pp. 69–93. [Google Scholar]
- Spence, S.H.; Rapee, R.M. The etiology of social anxiety disorder: An evidence-based model. Behav. Res. Ther. 2016, 86, 50–67. [Google Scholar] [CrossRef] [PubMed]
- Cartwright-Hatton, S.; Hodges, L.; Porter, J. Social anxiety in childhood: The relationship with self and observer rated social skills. J. Child Psychol. Psychiatry 2003, 44, 737–742. [Google Scholar] [CrossRef]
- Cartwright-Hatton, S.; Tschernitz, N.; Gomersall, H. Social anxiety in children: Social skills deficit, or cognitive distortion? Behav. Res. Ther. 2005, 43, 131–141. [Google Scholar] [CrossRef]
- Krämer, M.; Schmitz, J.; Heinrichs, N.; Tuschen-Caffier, B. Self-evaluation, social and cognitive performance in children with social phobia. J. Exp. Psychopathol. 2011, 2, 586–600. [Google Scholar] [CrossRef]
- Blöte, A.W.; Miers, A.C.; Van Den Bos, E.; Westenberg, P.M. The role of performance quality in adolescents’ self-evaluation and rumination after a speech: Is it contingent on social anxiety level? Behav. Cogn. Psychother. 2019, 47, 148–163. [Google Scholar] [CrossRef]
- Alfano, C.A.; Beidel, D.C.; Turner, S.M. Cognitive correlates of social phobia among children and adolescents. J. Abnorm. Child Psychol. 2006, 34, 189–201. [Google Scholar] [CrossRef]
- Miers, A.C.; Blöte, A.W.; Bokhorst, C.L.; Westenberg, P.M. Negative self-evaluations and the relation to performance level in socially anxious children and adolescents. Behav. Res. Ther. 2009, 47, 1043–1049. [Google Scholar] [CrossRef]
- Tuschen-Caffier, B.; Kühl, S.; Bender, C. Cognitive-evaluative features of childhood social anxiety in a performance task. J. Behav. Ther. Exp. Psychiatry 2011, 42, 233–239. [Google Scholar] [CrossRef]
- Miers, A.C.; Blöte, A.W.; Westenberg, P.M. Negative social cognitions in socially anxious youth: Distorted reality or a kernel of truth? J. Child Fam. Stud. 2011, 20, 214–223. [Google Scholar] [CrossRef]
- Halldorsson, B.; Castelijn, S.; Creswell, C. Are children with social anxiety disorder more likely than children with other anxiety disorders to anticipate poor social performance and reflect negatively on their performance? J. Affect. Disord. 2019, 245, 561–568. [Google Scholar] [CrossRef]
- Inderbitzen-Nolan, H.M.; Anderson, E.R.; Johnson, H.S. Subjective versus objective behavioral ratings following two analogue tasks: A comparison of socially phobic and non-anxious adolescents. J. Anxiety Disord. 2007, 21, 76–90. [Google Scholar] [CrossRef]
- Voncken, M.J.; Bögels, S.M. Social performance deficits in social anxiety disorder: Reality during conversation and biased perception during speech. J. Anxiety Disord. 2008, 22, 1384–1392. [Google Scholar] [CrossRef]
- Owens, M.; Stevenson, J.; Norgate, R.; Hadwin, J.A. Processing efficiency theory in children: Working memory as a mediator between trait anxiety and academic performance. Anxiety Stress Coping 2008, 21, 417–430. [Google Scholar] [CrossRef]
- Ashcraft, M.H.; Kirk, E.P. The relationships among working memory, math anxiety, and performance. J. Exp. Psychol. Gen. 2001, 130, 224–237. [Google Scholar] [CrossRef]
- Laukka, P.; Linnman, C.; Åhs, F.; Pissiota, A.; Frans, Ö.; Faria, V.; Michelgård, Å.; Appel, L.; Fredrikson, M.; Furmark, T. In a nervous voice: Acoustic analysis and perception of anxiety in social phobics’ speech. J. Nonverbal Behav. 2008, 32, 195–214. [Google Scholar] [CrossRef]
- Scharfstein, L.A.; Beidel, D.C.; Sims, V.K.; Rendon Finnell, L. Social skills deficits and vocal characteristics of children with social phobia or asperger’s disorder: A comparative study. J. Abnorm. Child Psychol. 2011, 39, 865–875. [Google Scholar] [CrossRef]
- Weeks, J.W.; Lee, C.Y.; Reilly, A.R.; Howell, A.N.; France, C.; Kowalsky, J.M.; Bush, A. “The Sound of Fear”: Assessing vocal fundamental frequency as a physiological indicator of social anxiety disorder. J. Anxiety Disord. 2012, 26, 811–822. [Google Scholar] [CrossRef]
- Juslin, P.N.; Scherer, K.R. Vocal Expression of Affect. In The New Handbook of Methods in Nonverbal Behavior Research; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Baucom, B.R.; Saxbe, D.E.; Ramos, M.C.; Spies, L.A.; Iturralde, E.; Duman, S.; Margolin, G. Correlates and characteristics of adolescents’ encoded emotional arousal during family conflict. Emotion 2012, 12, 1281–1291. [Google Scholar] [CrossRef]
- Bänziger, T.; Hosoya, G.; Scherer, K.R. Path models of vocal emotion communication. PLoS ONE 2015, 10, e0136675. [Google Scholar] [CrossRef]
- Weusthoff, S.; Baucom, B.R.; Hahlweg, K. Fundamental frequency during couple conflict: An analysis of physiological, behavioral, and sex-linked information encoded in vocal expression. J. Fam. Psychol. 2013, 27, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Laukka, P.; Elenius, K.; Fredrikson, M.; Furmark, T.; Neiberg, D. Vocal Expression in Spontaneous and Experimentally Induced Affective Speech: Acoustic Correlates of Anxiety, Irritation and Resignation. Available online: https://sail.usc.edu/publications/files/W2_Proceedings.pdf#page=52 (accessed on 2 August 2022).
- Spence, S.H.; Donovan, C.; Brechman-Toussaint, M.L. The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. J. Child Psychol. Psychiatry Allied Discip. 2000, 41, 713–726. [Google Scholar] [CrossRef]
- Van Dam-Baggen, R.; Kraaimaat, F. Group social skills training or cognitive group therapy as the clinical treatment of choice for generalized social phobia? J. Anxiety Disord. 2000, 14, 437–451. [Google Scholar] [CrossRef]
- Scaini, S.; Belotti, R.; Ogliari, A.; Battaglia, M. A comprehensive meta-analysis of cognitive-behavioral interventions for social anxiety disorder in children and adolescents. J. Anxiety Disord. 2016, 42, 105–112. [Google Scholar] [CrossRef]
- Buske-Kirschbaum, A.; Jobst, S.; Wustmans, A.; Kirschbaum, C.; Rauh, W.; Hellhammer, D.H. Attenuated free cortisol response to psychosocial stress in children with atopic dermatitis. Psychosom. Med. 1997, 59, 419–426. [Google Scholar] [CrossRef]
- Asbrand, J.; Heinrichs, N.; Schmidtendorf, S.; Nitschke, K.; Tuschen-Caffier, B. Experience versus report: Where are changes seen after exposure-based cognitive-behavioral therapy ? A randomized controlled group treatment of childhood social anxiety disorder. Child Psychiatry Hum. Dev. 2020, 51, 427–441. [Google Scholar] [CrossRef]
- Asbrand, J.; Schmitz, J.; Krämer, M.; Nitschke, K.; Heinrichs, N.; Tuschen-Caffier, B. Effects of group-based CBT on post-event processing in children with social anxiety disorder following an experimental social stressor. J. Abnorm. Child Psychol. 2019, 47, 1945–1956. [Google Scholar] [CrossRef]
- Asbrand, J.; Heinrichs, N.; Nitschke, K.; Wolf, O.T.; Tuschen-Caffier, B. Repeated stress leads to enhanced cortisol stress response in child social anxiety disorder but this effect can be prevented with CBT. Psychoneuroendocrinology 2019, 109, 1043–1052. [Google Scholar] [CrossRef]
- Asbrand, J.; Vögele, C.; Heinrichs, N.; Nitschke, K.; Tuschen-Caffier, B. Autonomic Dysregulation in Child Social Anxiety Disorder: An Experimental Design Using CBT Treatment. Appl. Psychophysiol. Biofeedback 2022, 47, 199–212. [Google Scholar] [CrossRef]
- Asbrand, J.; Schulz, A.; Heinrichs, N.; Tuschen-Caffier, B. Biased perception of physiological arousal in child social anxiety disorder before and after cognitive behavioral treatment. Clin Psychol Eur. 2020, 2, 1–25. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- La Greca, A.M.; Stone, W.L. Social Anxiety Scale for Children—Revised: Factor Structure and concurrent validity. J. Clin. Child Psychol. 1993, 22, 17–27. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Schneider, S.; Unnewehr, S.; Margraf, J. Kinder-DIPS: Diagnostisches Interview bei Psychischen Störungen im Kindes- und Jugendalter, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Owren, M.J.; Bacharowski, J. Measuring emotion-related vocal acoustins. In Handbook of Emotion Elicitation and Assessment; Coan, J.A., Allen, J.J.B., Eds.; Oxford University Press: Oxford, UK, 2007; pp. 239–266. [Google Scholar]
- Boersma, P.; Weenink, D. Praat: Doing Phonetics by Computer (Computer Program). 2019. Available online: http://www.praat.org/ (accessed on 16 November 2021).
- Tuschen-Caffier, B.; Kühl, S.; Bender, C. Soziale Ängste und Soziale Angststörung im Kindesalter: Ein Manual zur Indizierten Prävention und Psychologischen Therapie; Hogrefe: Göttingen, Germany, 2009. [Google Scholar]
- Beidel, D.C.; Turner, S.M.; Hamlin, K.; Morris, T.L. The Social Phobia and Anxiety Inventory for Children (SPAI-C): External and discriminative validity. Behav. Ther. 2001, 31, 75–87. [Google Scholar] [CrossRef]
- Parr, C.J.; Cartwright-Hatton, S. Social anxiety in adolescents: The effect of video feedback on anxiety and the self-evaluation of performance. Clin. Psychol. Psychother. 2009, 16, 46–54. [Google Scholar] [CrossRef]
- Flora, D.B. Your coefficient alpha Is probably wrong, but which coefficient omega is right? A tutorial on using R to obtain cetter reliability estimates. Adv. Methods Pract. Psychol. Sci. 2020, 3, 484–501. [Google Scholar] [CrossRef]
- Nájera Catalán, H.E. Reliability, Population Classification and Weighting in Multidimensional Poverty Measurement: A Monte Carlo Study. Soc. Indic. Res. 2019, 142, 887–910. [Google Scholar] [CrossRef]
- Hase, A.; O’Brien, J.; Moore, L.J.; Freeman, P. The relationship between challenge and threat states and performance: A systematic review. Sport Exerc. Perform. Psychol. 2019, 8, 123–144. [Google Scholar] [CrossRef]
- Miers, A.C.; Blöte, A.W.; Westenberg, P.M. Peer perceptions of social skills in socially anxious and nonanxious adolescents. J. Abnorm. Child Psychol. 2010, 38, 33–41. [Google Scholar] [CrossRef][Green Version]
- Mezulis, A.H.; Hyde, J.S.; Abramson, L.Y. The developmental origins of cognitive vulnerability to depression: Temperament, parenting, and negative life events in childhood as contributors to negative cognitive style. Dev. Psychol. 2006, 42, 1012–1025. [Google Scholar] [CrossRef]
- Asbrand, J.; Blechert, J.; Nitschke, K.; Tuschen-Caffier, B.; Schmitz, J. Aroused at Home: Basic Autonomic Regulation during Orthostatic and Physical Activation is Altered in Children with Social Anxiety Disorder. J. Abnorm. Child Psychol. 2017, 45, 143–155. [Google Scholar] [CrossRef]
- Blöte, A.W.; Miers, A.C.; Heyne, D.A.; Clark, D.M.; Westenberg, P.M. The relation between social anxiety and audience perception: Examining Clark and Wells’ (1995) model among adolescents. Behav. Cogn. Psychother. 2014, 42, 555–567. [Google Scholar] [CrossRef]
| Variable | Group | Statistics | |
|---|---|---|---|
| Social Anxiety Disorder (SAD) | Healthy Control (HC) | ||
| N | 67 | 55 | |
| Age (in years) a | 11.3 (1.4) | 11.3 (1.4) | t (117) = 0.06, n.s. |
| % female | 63.6 | 60.0 | χ2 (1) = 0.17, n.s. |
| Mean SPAI-C (SD) | 23.3 (9.03) | 4.2 (5.4) | t (117) = −13.71 ***, d = −2.71, CI [−3.28, −2.14] |
| Mean SASC-R a,b (child report) (SD) | 49.4 (13.0) | 28.2 (8.7) | t (117) = 10.59 ***, d = −2.03, CI [−2.54, −1.52] |
| Mean SASC-R a,c (mother report) (SD) | 60.9 (11.0) | 28.4 (6.9) | T (114) = 19.34 ***, d = −3.44, CI [−4.10, −2.78] |
| Monthly income (%) | χ2 (8) = 11.42, n.s. | ||
| NA | 0 | 1.3 | |
| <€1000 | 0 | 5.9 | |
| <€1500 | 1.9 | 7.4 | |
| <€2000 | 11.1 | 8.8 | |
| <€3000 | 35.2 | 32.4 | |
| <€4000 | 14.8 | 16.2 | |
| <€5000 | 14.8 | 20.6 | |
| >€5000 | 22.2 | 7.4 | |
| State anxiety during TSST-C (before treatment) a | 6.6 (2.8) | 4.5 (2.9) | t (117) = 4.05 ***, d = −0,75, CI [−1.12, −0,37] |
| Variable | Group | |
|---|---|---|
| Treatment (CBT) | Wait-List Control (WLC) | |
| N | 31 | 33 |
| Age (in years) a | 11.5 (1.4) | 11.2 (1.3) |
| % female | 51.6 | 67.6 |
| Mean SPAI-C (SD) | 21.9 (10.2) | 23.7 (7.74) |
| Mean SASC-R a,b (child report) (SD) | 49.3 (14.0) | 49.6 (12.3) |
| Mean SASC-R a,c (mother report) (SD) | 60.5 (12.5) | 61.3 (9.5) |
| Monthly income (%) | ||
| NA | 3.2 | 0 |
| <€1000 | 6.5 | 5.6 |
| <€1500 | 9.7 | 5.6 |
| <€2000 | 6.5 | 8.3 |
| <€3000 | 41.9 | 23.7 |
| <€4000 | 16.1 | 16.7 |
| <€5000 | 9.7 | 30.6 |
| >€5000 | 6.5 | 8.3 |
| State anxiety during TSST-C (before treatment) a | 6.7 (2.9) | 6.6 (2.8) |
| Variable | M | SD | 1.1 | 2.1 | 3.1 | 3.2 | |
|---|---|---|---|---|---|---|---|
| Social performance (cognitive) | 1.1 Self-report | 2.77 | 1.90 | ||||
| Social performance (behavioral) | 2.1 Other-report | 3.75 | 1.82 | −0.23 * | |||
| Physiological arousal | 3.1 f0 mean | 218.6 | 25.58 | −0.11 | −0.19 | ||
| 3.2 f0 range | 42.9 | 10.19 | −0.13 | −0.06 | −0.06 | ||
| Trait social anxiety | 4.1 SPAIC | 13.81 | 12.14 | −0.42 *** | 0.40 *** | −0.09 | 0.05 |
| Variable | M | SD | 1.1 | 2.1 | 3.1 | 3.2 | |
|---|---|---|---|---|---|---|---|
| Social performance 2 (cognitive) | 1.1 Subjective | 2.39 | 1.91 | ||||
| Social performance 2 (behavioral) | 2.1 Objective | 5.52 | 1.82 | −0.14 | |||
| Physiological arousal 2 | 3.1 f0 mean | 206.92 | 25.47 | −0.09 | 0.08 | ||
| 3.2 f0 range | 39.53 | 11.27 | −0.28 | −0.11 | −0.18 | ||
| Trait social anxiety | 4.1 SPAIK | 18.79 | 8.85 | −0.20 | −0.19 | −0.31 | 0.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asbrand, J.; Tuschen-Caffier, B. Taking a Closer Look at Social Performance in Childhood Social Anxiety Disorder: Biopsychosocial Context Considerations and Effects of Cognitive Behavior Therapy. Children 2022, 9, 1515. https://doi.org/10.3390/children9101515
Asbrand J, Tuschen-Caffier B. Taking a Closer Look at Social Performance in Childhood Social Anxiety Disorder: Biopsychosocial Context Considerations and Effects of Cognitive Behavior Therapy. Children. 2022; 9(10):1515. https://doi.org/10.3390/children9101515
Chicago/Turabian StyleAsbrand, Julia, and Brunna Tuschen-Caffier. 2022. "Taking a Closer Look at Social Performance in Childhood Social Anxiety Disorder: Biopsychosocial Context Considerations and Effects of Cognitive Behavior Therapy" Children 9, no. 10: 1515. https://doi.org/10.3390/children9101515
APA StyleAsbrand, J., & Tuschen-Caffier, B. (2022). Taking a Closer Look at Social Performance in Childhood Social Anxiety Disorder: Biopsychosocial Context Considerations and Effects of Cognitive Behavior Therapy. Children, 9(10), 1515. https://doi.org/10.3390/children9101515





