Comparison of Hospital Consultation and Summer Camp Lifestyle Intervention Programs for Sustained Body Weight Loss in Overweight/Obese Greek Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
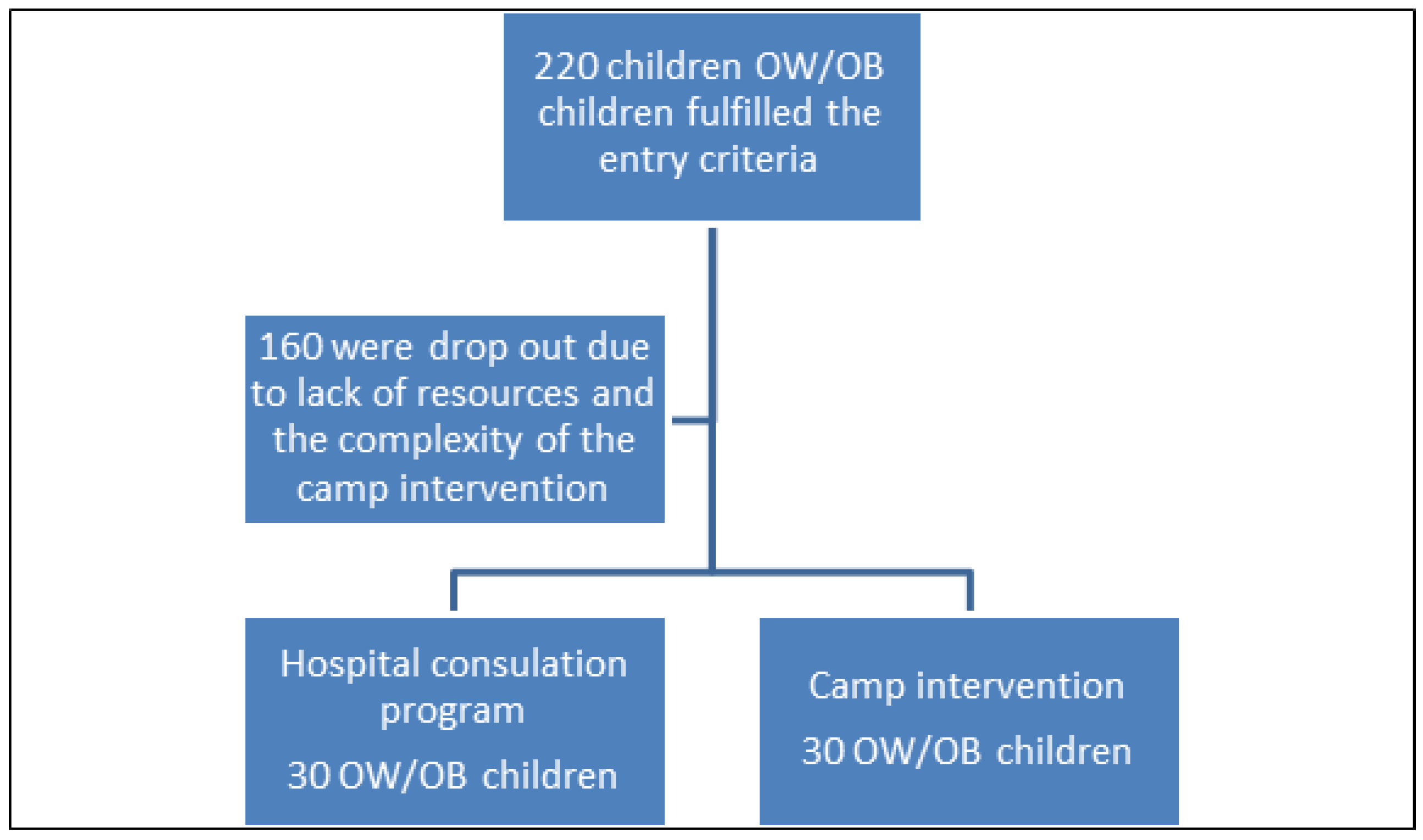
2.2. Participants
2.3. Measures
2.4. Hospital Consultation Program
2.5. Camp Intervention
2.6. Data Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guideline: Assessing and Managing Children at Primary Health-Care Facilities to Prevent Overweight and Obesity in the Context of the Double burDen of Malnutrition n.d. Available online: https://www.who.int/publications/i/item/9789241550123 (accessed on 26 October 2021).
- Barlow, S.E. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120 (Suppl. 4), S164–S192. [Google Scholar] [CrossRef]
- Childhood Obesity Facts, Overweight & Obesity, CDC n.d. Available online: https://www.cdc.gov/obesity/data/childhood.html (accessed on 14 October 2021).
- Hassapidou, M.; Tzotzas, T.; Makri, E.; Pagkalos, I.; Kaklamanos, I.; Kapantais, E.; Abrahamian, A.; Polymeris, A.; Tziomalos, K. Prevalence and geographic variation of abdominal obesity in 7- and 9-year-old children in Greece; World Health Organization Childhood Obesity Surveillance Initiative 2010. BMC Public Health 2017, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Starc, G.; Pérez, N.; Rito, A.I.; Kunešová, M.; et al. Prevalence of Severe Obesity among Primary School Children in 21 European Countries. Obes. Facts 2019, 12, 244–258. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- De Onis, M.; Blössner, M.; Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 2010, 92, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Mantzoros, C.S.; Rifas-Shiman, S.L.; Williams, C.J.; Fargnoli, J.L.; Kelesidis, T.; Gillman, M.W. Cord Blood Leptin and Adiponectin as Predictors of Adiposity in Children at 3 Years of Age: A Prospective Cohort Study. Pediatrics 2009, 123, 682–689. [Google Scholar] [CrossRef]
- Stavrou, S.; Critselis, E.; Darviri, C.; Charmandari, E.; Nicolaides, N.C.; Chrousos, G.P. Paediatric stress: From neuroendocrinology to contemporary disorders. Eur. J. Clin. Investig. 2017, 47, 262–269. [Google Scholar] [CrossRef]
- Birch, L.L.; Fisher, J.O. Development of eating behaviors among children and adolescents. Pediatrics 1998, 101, 539–549. [Google Scholar] [CrossRef]
- Birch, L.L.; Davison, K.K. Family Environmental Factors Influencing the Developing Behavioral Controls of Food Intake and Childhood Overweight. Pediatr. Clin. N. Am. 2001, 48, 893–907. [Google Scholar] [CrossRef]
- Farajian, P.; Risvas, G.; Panagiotakos, D.B.; Zampelas, A. Food sources of free sugars in children’s diet and identification of lifestyle patterns associated with free sugars intake: The GRECO (Greek Childhood Obesity) study. Public Health Nutr. 2016, 19, 2326–2335. [Google Scholar] [CrossRef][Green Version]
- Mantzoros, C.S. Nutrition and Metabolism, 1st ed.; Humana Press: Totowa, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Association between fast-food consumption and lifestyle characteristics in Greek children and adolescents; results from the EYZHN (National Action for Children’s Health) programme. Public Health Nutr. 2018, 21, 3386–3394. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Maher, C.; Matricciani, L.; Olds, T. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int. J. Obes. 2013, 37, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Golden, N.H.; Schneider, M.; Wood, C.; Committee on Nutrition; Committee on Adolescence; Obesity, S.O. Preventing Obesity and Eating Disorders in Adolescents. Pediatrics 2016, 138, e20161649. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef] [PubMed]
- El Mikati, H.K.; Boateng, A.O.; McKinney, B.M.; Haberlin-Pittz, K.; Pike, J.; Perry, P.; Hannon, T.S.; Yazel-Smith, L. Forever-Fit Summer Camp: The Impact of a 6-Week Summer Healthy Lifestyle Day Camp on Anthropometric, Cardiovascular, and Physical Fitness Measures in Youth With Obesity. J. Prim. Care Community Health 2020, 11, 2150132720903888. [Google Scholar] [CrossRef]
- Cooper, C.; Sarvey, S.; Collier, D.; Willson, C.; Green, I.; Pories, M.L.; Rose, M.A.; Escott-Stump, S.; Pories, W. For comparison: Experience with a children’s obesity camp. Surg. Obes. Relat. Dis. 2006, 2, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Larsen, K.T.; Huang, T.; Ried-Larsen, M.; Andersen, L.B.; Heidemann, M.; Møller, N.C. A Multi-Component Day-Camp Weight-Loss Program Is Effective in Reducing BMI in Children after One Year: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0157182. [Google Scholar] [CrossRef]
- Benestad, B.; Karlsen, T.-I.; Småstuen, M.C.; Lekhal, S.; Hertel, J.K.; Steinsbekk, S.; Kolotkin, R.L.; Ødegård, R.A.; Hjelmesæth, J. Health-related quality of life after camp-based family obesity treatment: An RCT. BMJ Paediatr. Open 2019, 3, e000413. [Google Scholar] [CrossRef]
- Block, G.; Subar, A.F. Estimates of nutrient intake from a food frequency questionnaire: The 1987 National Health Interview Survey. J. Am. Diet. Assoc. 1992, 92, 969–977. [Google Scholar] [CrossRef]
- Raper, N.; Perloff, B.; Ingwersen, L.; Steinfeldt, L.; Anand, J. An overview of USDA’s Dietary Intake Data System. J. Food Compos. Anal. 2004, 17, 545–555. [Google Scholar] [CrossRef]
- Sallis, J.F.; Buono, M.J.; Roby, J.J.; Micale, F.G.; Nelson, J.A. Seven-day recall and other physical activity self-reports in children and adolescents. Med. Sci. Sports Exerc. 1993, 25, 99–108. [Google Scholar] [CrossRef]
- O’Donovan, G.; Blazevich, A.; Boreham, C.; Cooper, A.; Crank, H.; Ekelund, U.; Fox, K.R.; Gately, P.J.; Giles-Corti, B.; Gill, J.M.R.; et al. The ABC of Physical Activity for Health: A consensus statement from the British Association of Sport and Exercise Sciences. J. Sports Sci. 2010, 28, 573–591. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.P.; Kirschenbaum, D.S. Immersion treatment of childhood and adolescent obesity: The first review of a promising intervention. Obes. Rev. 2010, 12, 37–49. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; Von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef]
- Benestad, B.; Lekhal, S.; Småstuen, M.C.; Hertel, J.K.; Halsteinli, V.; Ødegård, R.A.; Hjelmesæth, J. Camp-based family treatment of childhood obesity: Randomised controlled trial. Arch. Dis. Child. 2016, 102, 303–310. [Google Scholar] [CrossRef]
- Brandt, G.; Maschhoff, T.; Chandler, N.S. A residential camp experience as an approach to adolescent weight management. Adolescence 1980, 15, 807–822. [Google Scholar]
- Gately, P.J.; Cooke, C.B.; Barth, J.H.; Bewick, B.M.; Radley, D.; Hill, A.J. Children’s Residential Weight-Loss Programs Can Work: A Prospective Cohort Study of Short-Term Outcomes for Overweight and Obese Children. Pediatrics 2005, 116, 73–77. [Google Scholar] [CrossRef]
- Jirapinyo, P.; Wongarn, R.; Limsathayourat, N.; Bunnag, A.; Chockvivatvanit, S. A summer camp for childhood obesity in Thailand. J. Med. Assoc. Thail. Chotmaihet Thangphaet 1995, 78, 238–246. [Google Scholar]
- Evans, E.W.; Wing, R.R.; Pierre, D.F.; Howie, W.C.; Brinker, M.; Jelalian, E. Testing the effect of summer camp on excess summer weight gain in youth from low-income households: A randomized controlled trial. BMC Public Health 2020, 20, 1732. [Google Scholar] [CrossRef] [PubMed]
- George, G.L.; Schneider, C.; Kaiser, L. Healthy Lifestyle Fitness Camp: A Summer Approach to Prevent Obesity in Low-Income Youth. J. Nutr. Educ. Behav. 2016, 48, 208–212.e1. [Google Scholar] [CrossRef] [PubMed]
- Banchonhatakit, P.; Banchonhattakit, P.; Tanasugarn, C.; Pradipasen, M.; Miner, K.R.; Nityasuddhi, D. Ectiveness of school network for childhood obesity prevention (SNOCOP) in primary schools of Saraburi Province, Thailand. Southeast Asian J. Trop Med. Public Health 2009, 40, 816–834. [Google Scholar]
- Timlin, M.T.; Pereira, M.A.; Story, M.; Neumark-Sztainer, D. Breakfast Eating and Weight Change in a 5-Year Prospective Analysis of Adolescents: Project EAT (Eating among Teens). Pediatrics 2008, 121, e638–e645. [Google Scholar] [CrossRef]
- Velde, S.J.T.; Twisk, J.W.R.; Brug, J. Tracking of fruit and vegetable consumption from adolescence into adulthood and its longitudinal association with overweight. Br. J. Nutr. 2007, 98, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.; Krølner, R.; Klepp, K.-I.; Lytle, L.; Brug, J.; Bere, E.; Due, P. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part I: Quantitative studies. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 22. [Google Scholar] [CrossRef]
- Vereecken, C.; The HBSC Eating & Dieting Focus Group; Dupuy, M.; Rasmussen, M.; Kelly, C.; Nansel, T.R.; Al Sabbah, H.; Baldassari, D.; Jordan, M.D.; Maes, L.; et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int. J. Public Health 2009, 54, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Gately, P.; Cooke, C.; Butterly, R.; Mackreth, P.; Carroll, S. The effects of a children’s summer camp programme on weight loss, with a 10 month follow-up. Int. J. Obes. 2000, 24, 1445–1452. [Google Scholar] [CrossRef]
- Thompson, D.; Baranowski, T.; Cullen, K.; Watson, K.; Liu, Y.; Canada, A.; Bhatt, R.; Zakeri, I. Food, fun, and fitness internet program for girls: Pilot evaluation of an e-Health youth obesity prevention program examining predictors of obesity. Prev. Med. 2008, 47, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Faith, M.S.; Van Horn, L.; Appel, L.J.; Burke, L.E.; Carson, J.A.S.; Franch, H.; Jakicic, J.M.; Kral, T.V.; Young, C.O.C.D.I.T.; Wansink, B.; et al. Evaluating Parents and Adult Caregivers as “Agents of Change” for Treating Obese Children: Evidence for Parent Behavior Change Strategies and Research Gaps. Circulation 2012, 125, 1186–1207. [Google Scholar] [CrossRef]
- Kosti, R.I.; Kanellopoulou, A.; Fragkedaki, E.; Notara, V.; Giannakopoulou, S.-P.; Antonogeorgos, G.; Rojas-Gil, A.P.; Kornilaki, E.N.; Lagiou, A.; Panagiotakos, D.B. The Influence of Adherence to the Mediterranean Diet among Children and Their Parents in Relation to Childhood Overweight/Obesity: A Cross-Sectional Study in Greece. Child. Obes. 2020, 16, 571–578. [Google Scholar] [CrossRef]
| Total Sample (n = 60) | Boys (n = 26) | Girls (n = 34) | p-Value | |
|---|---|---|---|---|
| Age (years) | 10.93 ± 2.18 | 11.69 ± 1.85 | 10.35 ± 2.25 | 0.017 |
| Weight (kg) | 65.77 ± 17.24 | 68.54 ± 15.51 | 63.65 ± 18.39 | 0.280 |
| Height (cm) | 151.63 ± 13.10 | 156.85 ± 13.40 | 147.65 ± 11.54 | 0.006 |
| BMI (kg/m2) | 28.07 ± 4.19 | 27.44 ± 3.02 | 28.55 ± 4.90 | 0.287 |
| Camp Intervention | Hospital Intervention | ||||||
|---|---|---|---|---|---|---|---|
| Before Intervention | After Intervention | p * | Before Intervention | After Intervention | p * | p§ | |
| Gender (Male, %) | 13 (43.3%) | 13 (43.3%) | >0.999 † | ||||
| Weight (kg) a | 65.77 ± 17.38 | 63.63 ± 16.70 | <0.001 | 65.63 ± 17.21 | 64.80 ± 16.74 | <0.001 | - |
| BMI (kg/m2) a | 28.07 ± 4.23 | 27.17 ± 3.88 | <0.001 | 28.07 ± 4.23 | 27.21 ± 3.68 | <0.001 | - |
| BMI z-score a | 2.13 ± 0.30 | 2.06 ± 0.30 | <0.001 | 2.13 ± 0.30 | 2.10 ± 0.30 | <0.001 | - |
| Absolute change in weight (kg) a | −2.13 ± 1.22 | −0.83 ± 0.83 | <0.001 | ||||
| Absolute change in BMI (kg/m2) | −0.91 ± 0.50 | −0.38 ±0.36 | <0.001 | ||||
| Absolute change in BMI z-score a | −0.08 ± 0.05 | −0.03 ± 0.03 | <0.001 | ||||
| Time duration of weight retention (in months) a | 4.17 ± 1.42 | 2.03 ± 1.79 | <0.001 | ||||
| Physical activity score a | 2.46 ± 0.79 | 3.82 ± 0.77 | <0.001 * | 2.50 ± 0.82 | 2.50 ± 0.82 | >0.999 * | - |
| Sweet consumption (per week) a | 3.13 ± 0.86 | 1.97±0.93 | <0.001 * | 3.13 ± 0.86 | 2.73 ± 0.98 | 0.031 * | - |
| Soda consumption (per week) a | 3.30 ± 1.29 | 0.73 ± 0.69 | <0.001 * | 3.30 ± 1.29 | 3.30 ± 1.29 | >0.999 * | - |
| Absolute change in weekly sweet consumption a | −1.17 ± 1.23 | −0.40 ± 0.97 | 0.007 § | ||||
| Absolute change in weekly soda consumption a | −2.57 ± 1.57 | 0.00 ± 0.00 | <0.001 § | ||||
| Absolute change in physical activity score a | 1.33 ± 0.88 | 0.00 ± 0.00 | <0.001 § | ||||
| Breakfast (yes, per day) b | 43.3 | 96.7 | <0.001 ‡ | 60.0 | 73.3 | 0.125 ‡ | |
| Fruit/day (at least one portion) b | 40.0 | 93.3 | <0.001 ‡ | 40.0 | 56.7 | 0.063 ‡ | |
| Vegetables/day (at least one portion) b | 76.7 | 96.7 | 0.031 ‡ | 76.7 | 76.7 | >0.999 ‡ | |
| Delivery (yes, per week) b | 60.0 | 30.0 | 0.004 ‡ | 80.0 | 80.0 | >0.999 ‡ | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papageorgiou, A.L.; Efthymiou, V.; Giannouli, A.; Xekouki, P.; Kranioti, C.C.; Chrousos, G.P. Comparison of Hospital Consultation and Summer Camp Lifestyle Intervention Programs for Sustained Body Weight Loss in Overweight/Obese Greek Children. Children 2022, 9, 86. https://doi.org/10.3390/children9010086
Papageorgiou AL, Efthymiou V, Giannouli A, Xekouki P, Kranioti CC, Chrousos GP. Comparison of Hospital Consultation and Summer Camp Lifestyle Intervention Programs for Sustained Body Weight Loss in Overweight/Obese Greek Children. Children. 2022; 9(1):86. https://doi.org/10.3390/children9010086
Chicago/Turabian StylePapageorgiou, Anna L., Vasiliki Efthymiou, Aikaterini Giannouli, Paraskevi Xekouki, Christina C. Kranioti, and George P. Chrousos. 2022. "Comparison of Hospital Consultation and Summer Camp Lifestyle Intervention Programs for Sustained Body Weight Loss in Overweight/Obese Greek Children" Children 9, no. 1: 86. https://doi.org/10.3390/children9010086
APA StylePapageorgiou, A. L., Efthymiou, V., Giannouli, A., Xekouki, P., Kranioti, C. C., & Chrousos, G. P. (2022). Comparison of Hospital Consultation and Summer Camp Lifestyle Intervention Programs for Sustained Body Weight Loss in Overweight/Obese Greek Children. Children, 9(1), 86. https://doi.org/10.3390/children9010086







