Nutritional Risks among Adolescent Athletes with Disordered Eating
Abstract
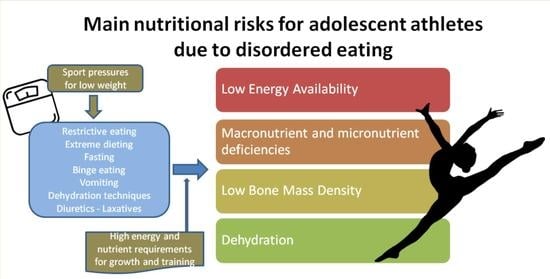
:1. Introduction
2. Materials and Methods
3. Results
3.1. Low Energy Availability
3.2. Macronutrient and Micronutrient Deficiencies
3.3. Low Bone Mass Density
3.4. Dehydration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A Foundation for Future Health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Delisle, H.; World Health Organization. Nutrition in Adolescence: Issues and Challenges for the Health Sector: Issues in Adolescent Health and Development; WHO: Geneva, Switzerland, 2005; ISBN 978-92-4-159366-3. [Google Scholar]
- Prentice, A.M.; Ward, K.A.; Goldberg, G.R.; Jarjou, L.M.; Moore, S.E.; Fulford, A.J.; Prentice, A. Critical Windows for Nutritional Interventions against Stunting. Am. J. Clin. Nutr. 2013, 97, 911–918. [Google Scholar] [CrossRef] [Green Version]
- Desbrow, B.; McCormack, J.; Burke, L.M.; Cox, G.R.; Fallon, K.; Hislop, M.; Logan, R.; Marino, N.; Sawyer, S.M.; Shaw, G.; et al. Sports Dietitians Australia Position Statement: Sports Nutrition for the Adolescent Athlete. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 570–584. [Google Scholar] [CrossRef]
- Bingham, M.E.; Borkan, M.; Quatromoni, P. Sports Nutrition Advice for Adolescent Athletes: A Time to Focus on Food. Am. J. Lifestyle Med. 2015, 9, 398–402. [Google Scholar] [CrossRef]
- Purcell, L.K. Sport Nutrition for Young Athletes. Paediatr. Child Health 2013, 18, 200–202. [Google Scholar] [CrossRef]
- Berg, E.K. Performance Nutrition for the Adolescent Athlete: A Realistic Approach. Clin. J. Sport Med. 2019, 29, 345–352. [Google Scholar] [CrossRef]
- Wells, K.R.; Jeacocke, N.A.; Appaneal, R.; Smith, H.D.; Vlahovich, N.; Burke, L.M.; Hughes, D. The Australian Institute of Sport (AIS) and National Eating Disorders Collaboration (NEDC) Position Statement on Disordered Eating in High Performance Sport. Br. J. Sports Med. 2020, 54, 1247–1258. [Google Scholar] [CrossRef] [PubMed]
- Unnithan, V.B.; Baxter-Jones, A.D.G. The Young Athlete. Nutr. Sport 2000, 7, 429–441. [Google Scholar]
- Bonci, C.M.; Bonci, L.J.; Granger, L.R.; Johnson, C.L.; Malina, R.M.; Milne, L.W.; Ryan, R.R.; Vanderbunt, E.M. National Athletic Trainers’ Association Position Statement: Preventing, Detecting, and Managing Disordered Eating in Athletes. J. Athl. Train. 2008, 43, 80–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundgot-Borgen, J.; Torstveit, M.K. Prevalence of Eating Disorders in Elite Athletes Is Higher than in the General Population. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2004, 14, 25–32. [Google Scholar] [CrossRef]
- Reardon, C.L.; Hainline, B.; Aron, C.M.; Baron, D.; Baum, A.L.; Bindra, A.; Budgett, R.; Campriani, N.; Castaldelli-Maia, J.M.; Currie, A.; et al. Mental Health in Elite Athletes: International Olympic Committee Consensus Statement. Br. J. Sports Med. 2019, 53, 667–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- Sundgot-Borgen, J.; Meyer, N.L.; Lohman, T.G.; Ackland, T.R.; Maughan, R.J.; Stewart, A.D.; Müller, W. How to Minimise the Health Risks to Athletes Who Compete in Weight-Sensitive Sports Review and Position Statement on Behalf of the Ad Hoc Research Working Group on Body Composition, Health and Performance, under the Auspices of the IOC Medical Commission. Br. J. Sports Med. 2013, 47, 1012–1022. [Google Scholar] [CrossRef] [PubMed]
- Sundgot-Borgen, J.; Torstveit, M.K. Aspects of Disordered Eating Continuum in Elite High-Intensity Sports. Scand. J. Med. Sci. Sports 2010, 20 (Suppl. 2), 112–121. [Google Scholar] [CrossRef] [PubMed]
- Martinsen, M.T.; Sundgot-Borgen, J. Higher Prevalence of Eating Disorders among Adolescent Elite Athletes than Controls. Med. Sci. Sports Exerc. 2013, 45, 1188–1197. [Google Scholar] [CrossRef] [Green Version]
- Mancine, R.P.; Gusfa, D.W.; Moshrefi, A.; Kennedy, S.F. Prevalence of Disordered Eating in Athletes Categorized by Emphasis on Leanness and Activity Type—A Systematic Review. J. Eat. Disord. 2020, 8, 47. [Google Scholar] [CrossRef]
- Jankauskiene, R.; Baceviciene, M. Body Image and Disturbed Eating Attitudes and Behaviors in Sport-Involved Adolescents: The Role of Gender and Sport Characteristics. Nutrients 2019, 11, 3061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nichols, J.F.; Rauh, M.J.; Barrack, M.T.; Barkai, H.-S.; Pernick, Y. Disordered Eating and Menstrual Irregularity in High School Athletes in Lean-Build and Nonlean-Build Sports. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 364–377. [Google Scholar] [CrossRef]
- Nichols, J.F.; Rauh, M.J.; Lawson, M.J.; Ji, M.; Barkai, H.-S. Prevalence of the Female Athlete Triad Syndrome among High School Athletes. Arch. Pediatr. Adolesc. Med. 2006, 160, 137–142. [Google Scholar] [CrossRef] [Green Version]
- Pernick, Y.; Nichols, J.F.; Rauh, M.J.; Kern, M.; Ji, M.; Lawson, M.J.; Wilfley, D. Disordered Eating among a Multi-Racial/Ethnic Sample of Female High-School Athletes. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2006, 38, 689–695. [Google Scholar] [CrossRef]
- Ranby, K.W.; Aiken, L.S.; MacKinnon, D.P.; Elliot, D.L.; Moe, E.L.; McGinnis, W.; Goldberg, L. A Mediation Analysis of the ATHENA Intervention for Female Athletes: Prevention of Athletic-Enhancing Substance Use and Unhealthy Weight Loss Behaviors. J. Pediatr. Psychol. 2009, 34, 1069–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosendahl, J.; Bormann, B.; Aschenbrenner, K.; Aschenbrenner, F.; Strauss, B. Dieting and Disordered Eating in German High School Athletes and Non-Athletes. Scand. J. Med. Sci. Sports 2009, 19, 731–739. [Google Scholar] [CrossRef]
- Schtscherbyna, A.; Soares, E.A.; de Oliveira, F.P.; Ribeiro, B.G. Female Athlete Triad in Elite Swimmers of the City of Rio de Janeiro, Brazil. Nutr. Burbank Los Angel. City Calif. 2009, 25, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Thein-Nissenbaum, J.M.; Rauh, M.J.; Carr, K.E.; Loud, K.J.; McGuine, T.A. Associations between Disordered Eating, Menstrual Dysfunction, and Musculoskeletal Injury among High School Athletes. J. Orthop. Sports Phys. Ther. 2011, 41, 60–69. [Google Scholar] [CrossRef]
- Toro, J.; Galilea, B.; Martinez-Mallén, E.; Salamero, M.; Capdevila, L.; Mari, J.; Mayolas, J.; Toro, E. Eating Disorders in Spanish Female Athletes. Int. J. Sports Med. 2005, 26, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Van Durme, K.; Goossens, L.; Braet, C. Adolescent Aesthetic Athletes: A Group at Risk for Eating Pathology? Eat. Behav. 2012, 13, 119–122. [Google Scholar] [CrossRef] [Green Version]
- Heradstveit, O.; Hysing, M.; Nilsen, S.A.; Bøe, T. Symptoms of Disordered Eating and Participation in Individual- and Team Sports: A Population-Based Study of Adolescents. Eat. Behav. 2020, 39, 101434. [Google Scholar] [CrossRef] [PubMed]
- Sundgot-Borgen, J. Eating Disorders, Energy Intake, Training Volume, and Menstrual Function in High-Level Modern Rhythmic Gymnasts. Int. J. Sport Nutr. 1996, 6, 100–109. [Google Scholar] [CrossRef] [Green Version]
- Nordin, S.M.; Harris, G.; Cumming, J. Disturbed Eating in Young, Competitive Gymnasts: Differences between Three Gymnastics Disciplines. Eur. J. Sport Sci. 2003, 3, 1–14. [Google Scholar] [CrossRef]
- Okano, G.; Holmes, R.A.; Mu, Z.; Yang, P.; Lin, Z.; Nakai, Y. Disordered Eating in Japanese and Chinese Female Runners, Rhythmic Gymnasts and Gymnasts. Int. J. Sports Med. 2005, 26, 486–491. [Google Scholar] [CrossRef]
- Donti, O.; Donti, A.; Gaspari, V.; Pleksida, P.; Psychountaki, M. Are They Too Perfect to Eat Healthy? Association between Eating Disorder Symptoms and Perfectionism in Adolescent Rhythmic Gymnasts. Eat. Behav. 2021, 41, 101514. [Google Scholar] [CrossRef]
- Giel, K.E.; Hermann-Werner, A.; Mayer, J.; Diehl, K.; Schneider, S.; Thiel, A.; Zipfel, S. Eating Disorder Pathology in Elite Adolescent Athletes. Int. J. Eat. Disord. 2016, 49, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Reel, J.J.; Petrie, T.A.; SooHoo, S.; Anderson, C.M. Weight Pressures in Sport: Examining the Factor Structure and Incremental Validity of the Weight Pressures in Sport—Females. Eat. Behav. 2013, 14, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.M.; Petrie, T.A.; Neumann, C.S. Effects of Sport Pressures on Female Collegiate Athletes: A Preliminary Longitudinal Investigation. Sport Exerc. Perform. Psychol. 2012, 1, 120–134. [Google Scholar] [CrossRef]
- Byrne, S.; McLean, N. Elite Athletes: Effects of the Pressure to Be Thin. J. Sci. Med. Sport 2002, 5, 80–94. [Google Scholar] [CrossRef]
- Nattiv, A.; Loucks, A.B.; Manore, M.M.; Sanborn, C.F.; Sundgot-Borgen, J.; Warren, M.P.; American College of Sports Medicine. American College of Sports Medicine Position Stand. The Female Athlete Triad. Med. Sci. Sports Exerc. 2007, 39, 1867–1882. [Google Scholar] [CrossRef] [PubMed]
- Female Athlete Issues for the Team Physician: A Consensus Statement—2017 Update. Med. Sci. Sports Exerc. 2018, 50, 1113–1122. [CrossRef] [PubMed]
- El Ghoch, M.; Soave, F.; Calugi, S.; Dalle Grave, R. Eating Disorders, Physical Fitness and Sport Performance: A Systematic Review. Nutrients 2013, 5, 5140–5160. [Google Scholar] [CrossRef] [Green Version]
- Joy, E.; Kussman, A.; Nattiv, A. 2016 Update on Eating Disorders in Athletes: A Comprehensive Narrative Review with a Focus on Clinical Assessment and Management. Br. J. Sports Med. 2016, 50, 154–162. [Google Scholar] [CrossRef] [Green Version]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Carter, S.; Constantini, N.; Lebrun, C.; Meyer, N.; Sherman, R.; Steffen, K.; Budgett, R.; et al. The IOC Consensus Statement: Beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 2014, 48, 491–497. [Google Scholar] [CrossRef]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.; Meyer, N.; et al. International Olympic Committee (IOC) Consensus Statement on Relative Energy Deficiency in Sport (RED-S): 2018 Update. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 316–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torstveit, M.K.; Sundgot-Borgen, J. Eating Disorders in Male and Female Athletes. In The Encyclopaedia of Sports Medicine; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2013; pp. 513–525. ISBN 978-1-118-69231-8. [Google Scholar]
- Sundgot-Borgen, J.; Danielsen, K.; Klungland-Torstveit, M. Female Former Elite Athletes Suffering from Eating Disorders during Their Career. A 15–20 Year Follow-Up. Med. Sci. Sports Exerc. 2012, 44, 267–958. [Google Scholar]
- Soric, M.; Misigoj-Durakovic, M.; Pedisic, Z. Dietary Intake and Body Composition of Prepubescent Female Aesthetic Athletes. Int. J. Sport Nutr. Exerc. Metab. 2008, 18, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Caine, D.; Lewis, R.; O’Connor, P.; Howe, W.; Bass, S. Does Gymnastics Training Inhibit Growth of Females? Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2001, 11, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Roemmich, J.N.; Sinning, W.E. Weight Loss and Wrestling Training: Effects on Nutrition, Growth, Maturation, Body Composition, and Strength. J. Appl. Physiol. 1997, 82, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.K.W.; Hecht, S.; Fitness, C. The Female Athlete Triad. Pediatrics 2016, 138, e20160922. [Google Scholar] [CrossRef] [Green Version]
- Soleimany, G.; Dadgostar, H.; Lotfian, S.; Moradi-Lakeh, M.; Dadgostar, E.; Movaseghi, S. Bone Mineral Changes and Cardiovascular Effects among Female Athletes with Chronic Menstrual Dysfunction. Asian J. Sports Med. 2012, 3, 53–58. [Google Scholar] [CrossRef] [Green Version]
- Hoch, A.Z.; Papanek, P.; Szabo, A.; Widlansky, M.E.; Schimke, J.E.; Gutterman, D.D. Association between the Female Athlete Triad and Endothelial Dysfunction in Dancers. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2011, 21, 119–125. [Google Scholar] [CrossRef]
- Beals, K.A.; Hill, A.K. The Prevalence of Disordered Eating, Menstrual Dysfunction, and Low Bone Mineral Density among US Collegiate Athletes. Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 1–23. [Google Scholar] [CrossRef]
- Greenleaf, C.; Petrie, T.A.; Carter, J.; Reel, J.J. Female Collegiate Athletes: Prevalence of Eating Disorders and Disordered Eating Behaviors. J. Am. Coll. Health J ACH 2009, 57, 489–495. [Google Scholar] [CrossRef]
- Dipasquale, L.; Petrie, T.A. Prevalence of Disordered Eating: A Comparison of Male and Female Collegiate Athletes and Nonathletes. J. Clin. Sport Psychol. 2013, 7, 186–197. [Google Scholar] [CrossRef] [Green Version]
- Anderson, C.M.; Petrie, T.A.; Neumann, C.S. Psychosocial Correlates of Bulimic Symptoms among NCAA Division-I Female Collegiate Gymnasts and Swimmers/Divers. J. Sport Exerc. Psychol. 2011, 33, 483–505. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.; Petrie, T.A. Prevalence of Disordered Eating and Pathogenic Weight Control Behaviors among NCAA Division I Female Collegiate Gymnasts and Swimmers. Res. Q. Exerc. Sport 2012, 83, 120–124. [Google Scholar] [CrossRef]
- Sundgot-Borgen, J. Prevalence of Eating Disorders in Elite Female Athletes. Int. J. Sport Nutr. 1993, 3, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Loucks, A.B. Energy Balance and Energy Availability. In The Encyclopaedia of Sports Medicine; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2013; pp. 72–87. ISBN 978-1-118-69231-8. [Google Scholar]
- Manore, M.; Cialdella-Kam, L.; Loucks, A. The Female Athlete Triad: Components, Nutrition Issues, and Health Consequences. J. Sports Sci. 2007, 25 (Suppl. 1), S61–S71. [Google Scholar] [CrossRef]
- Ihle, R.; Loucks, A.B. Dose-Response Relationships between Energy Availability and Bone Turnover in Young Exercising Women. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2004, 19, 1231–1240. [Google Scholar] [CrossRef]
- Beals, K.A. Eating Behaviors, Nutritional Status, and Menstrual Function in Elite Female Adolescent Volleyball Players. J. Am. Diet. Assoc. 2002, 102, 1293–1296. [Google Scholar] [CrossRef]
- Brown, A.; Jones, S.W.; Rowan, H. Baby-Led Weaning: The Evidence to Date. Curr. Nutr. Rep. 2017, 6, 148–156. [Google Scholar] [CrossRef] [Green Version]
- Souza, M.J.D.; Nattiv, A.; Joy, E.; Misra, M.; Williams, N.I.; Mallinson, R.J.; Gibbs, J.C.; Olmsted, M.; Goolsby, M.; Matheson, G.; et al. 2014 Female Athlete Triad Coalition Consensus Statement on Treatment and Return to Play of the Female Athlete Triad: 1st International Conference Held in San Francisco, California, May 2012 and 2nd International Conference Held in Indianapolis, Indiana, May 2013. Br. J. Sports Med. 2014, 48, 289. [Google Scholar] [CrossRef] [Green Version]
- Ackerman, K.E.; Misra, M. Amenorrhoea in Adolescent Female Athletes. Lancet Child Adolesc. Health 2018, 2, 677–688. [Google Scholar] [CrossRef]
- Thein-Nissenbaum, J.; Hammer, E. Treatment Strategies for the Female Athlete Triad in the Adolescent Athlete: Current Perspectives. Open Access J. Sports Med. 2017, 8, 85–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dwyer, J.; Eisenberg, A.; Prelack, K.; Song, W.O.; Sonneville, K.; Ziegler, P. Eating Attitudes and Food Intakes of Elite Adolescent Female Figure Skaters: A Cross Sectional Study. J. Int. Soc. Sports Nutr. 2012, 9, 53. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira Coelho, G.M.; de Farias, M.L.F.; de Mendonça, L.M.C.; de Mello, D.B.; Lanzillotti, H.S.; Ribeiro, B.G.; de Abreu Soares, E. The Prevalence of Disordered Eating and Possible Health Consequences in Adolescent Female Tennis Players from Rio de Janeiro, Brazil. Appetite 2013, 64, 39–47. [Google Scholar] [CrossRef]
- Da Costa, N.F.; Schtscherbyna, A.; Soares, E.A.; Ribeiro, B.G. Disordered Eating among Adolescent Female Swimmers: Dietary, Biochemical, and Body Composition Factors. Nutrition 2013, 29, 172–177. [Google Scholar] [CrossRef]
- Wood, K.L.; Barrack, M.T.; Gray, V.B.; Cotter, J.A.; Van Loan, M.D.; Rauh, M.J.; McGowan, R.; Nichols, J.F. Cognitive Dietary Restraint Score Is Associated with Lower Energy, Carbohydrate, Fat, and Grain Intake among Female Adolescent Endurance Runners. Eat. Behav. 2020, 40, 101460. [Google Scholar] [CrossRef]
- Hoch, A.Z.; Pajewski, N.M.; Moraski, L.; Carrera, G.F.; Wilson, C.R.; Hoffmann, R.G.; Schimke, J.E.; Gutterman, D.D. Prevalence of the Female Athlete Triad in High School Athletes and Sedentary Students. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2009, 19, 421–428. [Google Scholar] [CrossRef] [Green Version]
- Silva, M.-R.G.; Silva, H.-H.; Paiva, T. Sleep Duration, Body Composition, Dietary Profile and Eating Behaviours among Children and Adolescents: A Comparison between Portuguese Acrobatic Gymnasts. Eur. J. Pediatr. 2018, 177, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Braun, H.; von Andrian-Werburg, J.; Schänzer, W.; Thevis, M. Nutrition Status of Young Elite Female German Football Players. Pediatr. Exerc. Sci. 2018, 30, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Matt, S.A.; Barrack, M.T.; Gray, V.B.; Cotter, J.A.; Van Loan, M.D.; Rauh, M.J.; McGowan, R.; Nichols, J.F. Adolescent Endurance Runners Exhibit Suboptimal Energy Availability and Intakes of Key Nutrients. J. Am. Coll. Nutr. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Defeciani, L. Eating Disorders and Body Image Concerns Among Male Athletes. Clin. Soc. Work J. 2016, 44. [Google Scholar] [CrossRef]
- Vertalino, M.; Eisenberg, M.E.; Story, M.; Neumark-Sztainer, D. Participation in Weight-Related Sports Is Associated with Higher Use of Unhealthful Weight-Control Behaviors and Steroid Use. J. Am. Diet. Assoc. 2007, 107, 434–440. [Google Scholar] [CrossRef]
- Koehler, K.; Achtzehn, S.; Braun, H.; Mester, J.; Schaenzer, W. Comparison of Self-Reported Energy Availability and Metabolic Hormones to Assess Adequacy of Dietary Energy Intake in Young Elite Athletes. Appl. Physiol. Nutr. Metab. 2013, 38, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Deutz, R.C.; Benardot, D.; Martin, D.E.; Cody, M.M. Relationship between Energy Deficits and Body Composition in Elite Female Gymnasts and Runners. Med. Sci. Sports Exerc. 2000, 32, 659–668. [Google Scholar] [CrossRef]
- Melin, A.; Tornberg, Å.B.; Skouby, S.; Møller, S.S.; Sundgot-Borgen, J.; Faber, J.; Sidelmann, J.J.; Aziz, M.; Sjödin, A. Energy Availability and the Female Athlete Triad in Elite Endurance Athletes. Scand. J. Med. Sci. Sports 2015, 25, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Woods, A.L.; Garvican-Lewis, L.A.; Lundy, B.; Rice, A.J.; Thompson, K.G. New Approaches to Determine Fatigue in Elite Athletes during Intensified Training: Resting Metabolic Rate and Pacing Profile. PLoS ONE 2017, 12, e0173807. [Google Scholar] [CrossRef]
- Burke, L.M. Carbohydrate Needs of Athletes in Training. In The Encyclopaedia of Sports Medicine; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2013; pp. 102–112. ISBN 978-1-118-69231-8. [Google Scholar]
- Manore, M.M. Dietary Recommendations and Athletic Menstrual Dysfunction. Sports Med. 2002, 32, 887–901. [Google Scholar] [CrossRef]
- Woolf, K.; Manore, M. B-Vitamins and Exercise: Does Exercise Alter Requirements? Int. J. Sport Nutr. Exerc. Metab. 2006, 16, 453–484. [Google Scholar] [CrossRef]
- Ziegler, P.; Hensley, S.; Roepke, J.B.; Whitaker, S.H.; Craig, B.W.; Drewnowski, A. Eating Attitudes and Energy Intakes of Female Skaters. Med. Sci. Sports Exerc. 1998, 30, 583–586. [Google Scholar] [CrossRef]
- Barrack, M.T.; Rauh, M.J.; Barkai, H.-S.; Nichols, J.F. Dietary Restraint and Low Bone Mass in Female Adolescent Endurance Runners. Am. J. Clin. Nutr. 2008, 87, 36–43. [Google Scholar] [CrossRef]
- Golden, N.H.; Schneider, M.; Wood, C.; Nutrition, C.O.; Adolescence, C.O.; Obesity, S.O. Preventing Obesity and Eating Disorders in Adolescents. Pediatrics 2016, 138, e20161649. [Google Scholar] [CrossRef] [Green Version]
- Barrack, M.T.; Rauh, M.J.; Nichols, J.F. Prevalence of and Traits Associated with Low BMD among Female Adolescent Runners. Med. Sci. Sports Exerc. 2008, 40, 2015–2021. [Google Scholar] [CrossRef]
- Christo, K.; Prabhakaran, R.; Lamparello, B.; Cord, J.; Miller, K.K.; Goldstein, M.A.; Gupta, N.; Herzog, D.B.; Klibanski, A.; Misra, M. Bone Metabolism in Adolescent Athletes With Amenorrhea, Athletes With Eumenorrhea, and Control Subjects. Pediatrics 2008, 121, 1127–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skorseth, P.; Segovia, N.; Hastings, K.; Kraus, E. Prevalence of Female Athlete Triad Risk Factors and Iron Supplementation Among High School Distance Runners: Results From a Triad Risk Screening Tool. Orthop. J. Sports Med. 2020, 8, 2325967120959725. [Google Scholar] [CrossRef]
- Javed, A.; Tebben, P.J.; Fischer, P.R.; Lteif, A.N. Female Athlete Triad and Its Components: Toward Improved Screening and Management. Mayo Clin. Proc. 2013, 88, 996–1009. [Google Scholar] [CrossRef] [Green Version]
- Weimann, E.; Witzel, C.; Schwidergall, S.; Böhles, H.J. Peripubertal Perturbations in Elite Gymnasts Caused by Sport Specific Training Regimes and Inadequate Nutritional Intake. Int. J. Sports Med. 2000, 21, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Rauh, M.J.; Nichols, J.F.; Barrack, M.T. Relationships among Injury and Disordered Eating, Menstrual Dysfunction, and Low Bone Mineral Density in High School Athletes: A Prospective Study. J. Athl. Train. 2010, 45, 243–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thralls, K.J.; Nichols, J.F.; Barrack, M.T.; Kern, M.; Rauh, M.J. Body Mass-Related Predictors of the Female Athlete Triad Among Adolescent Athletes. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Barrack, M.T.; Van Loan, M.D.; Rauh, M.J.; Nichols, J.F. Physiologic and Behavioral Indicators of Energy Deficiency in Female Adolescent Runners with Elevated Bone Turnover. Am. J. Clin. Nutr. 2010, 92, 652–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tenforde, A.S.; Fredericson, M.; Sayres, L.C.; Cutti, P.; Sainani, K.L. Identifying Sex-Specific Risk Factors for Low Bone Mineral Density in Adolescent Runners. Am. J. Sports Med. 2015, 43, 1494–1504. [Google Scholar] [CrossRef] [PubMed]
- Nose-Ogura, S.; Yoshino, O.; Dohi, M.; Kigawa, M.; Harada, M.; Hiraike, O.; Onda, T.; Osuga, Y.; Fujii, T.; Saito, S. Risk Factors of Stress Fractures Due to the Female Athlete Triad: Differences in Teens and Twenties. Scand. J. Med. Sci. Sports 2019, 29, 1501–1510. [Google Scholar] [CrossRef]
- Committee on Sports Medicine and Fitness Promotion of Healthy Weight-Control Practices in Young Athletes. Pediatrics 2005, 116, 1557–1564. [CrossRef] [Green Version]
- Carl, R.L.; Johnson, M.D.; Martin, T.J.; Fitness, C. Promotion of Healthy Weight-Control Practices in Young Athletes. Pediatrics 2017, 140. [Google Scholar] [CrossRef] [Green Version]
- Oppliger, R.A.; Landry, G.L.; Foster, S.W.; Lambrecht, A.C. Bulimic Behaviors among Interscholastic Wrestlers: A Statewide Survey. Pediatrics 1993, 91, 826–831. [Google Scholar]
- Kiningham, R.B.; Gorenflo, D.W. Weight Loss Methods of High School Wrestlers. Med. Sci. Sports Exerc. 2001, 33, 810–813. [Google Scholar] [CrossRef]
- Petrie, H.J.; Stover, E.A.; Horswill, C.A. Nutritional Concerns for the Child and Adolescent Competitor. Nutr. Burbank Los Angel. City Calif. 2004, 20, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.; Volterman, K.A.; Timmons, B.W.; Wilk, B. Fluid Balance and Dehydration in the Young Athlete: Assessment Considerations and Effects on Health and Performance. Am. J. Lifestyle Med. 2012, 6, 489–501. [Google Scholar] [CrossRef]
- Rankin, J.W. Weight Loss and Gain in Athletes. Curr. Sports Med. Rep. 2002, 1, 208–213. [Google Scholar] [CrossRef]
- Jones, L.C.; Cleary, M.A.; Lopez, R.M.; Zuri, R.E.; Lopez, R. Active Dehydration Impairs Upper and Lower Body Anaerobic Muscular Power. J. Strength Cond. Res. 2008, 22, 455–463. [Google Scholar] [CrossRef]
- Judelson, D.A.; Maresh, C.M.; Anderson, J.M.; Armstrong, L.E.; Casa, D.J.; Kraemer, W.J.; Volek, J.S. Hydration and Muscular Performance: Does Fluid Balance Affect Strength, Power and High-Intensity Endurance? Sports Med. 2007, 37, 907–921. [Google Scholar] [CrossRef]
- Hayes, L.D.; Morse, C.I. The Effects of Progressive Dehydration on Strength and Power: Is There a Dose Response? Eur. J. Appl. Physiol. 2010, 108, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Logue, D.M.; Madigan, S.M.; Melin, A.; Delahunt, E.; Heinen, M.; Donnell, S.-J.M.; Corish, C.A. Low Energy Availability in Athletes 2020: An Updated Narrative Review of Prevalence, Risk, Within-Day Energy Balance, Knowledge, and Impact on Sports Performance. Nutrients 2020, 12, 835. [Google Scholar] [CrossRef] [Green Version]
- De Souza, M.J.; Koltun, K.J.; Williams, N.I. The Role of Energy Availability in Reproductive Function in the Female Athlete Triad and Extension of Its Effects to Men: An Initial Working Model of a Similar Syndrome in Male Athletes. Sports Med. 2019, 49, 125–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maïmoun, L.; Georgopoulos, N.A.; Sultan, C. Endocrine Disorders in Adolescent and Young Female Athletes: Impact on Growth, Menstrual Cycles, and Bone Mass Acquisition. J. Clin. Endocrinol. Metab. 2014, 99, 4037–4050. [Google Scholar] [CrossRef] [PubMed]
- Drew, M.; Vlahovich, N.; Hughes, D.; Appaneal, R.; Burke, L.M.; Lundy, B.; Rogers, M.; Toomey, M.; Watts, D.; Lovell, G.; et al. Prevalence of Illness, Poor Mental Health and Sleep Quality and Low Energy Availability Prior to the 2016 Summer Olympic Games. Br. J. Sports Med. 2018, 52, 47–53. [Google Scholar] [CrossRef]
- Areta, J.L.; Taylor, H.L.; Koehler, K. Low Energy Availability: History, Definition and Evidence of Its Endocrine, Metabolic and Physiological Effects in Prospective Studies in Females and Males. Eur. J. Appl. Physiol. 2021, 121, 1–21. [Google Scholar] [CrossRef]
- Koehler, K.; Hoerner, N.R.; Gibbs, J.C.; Zinner, C.; Braun, H.; De Souza, M.J.; Schaenzer, W. Low Energy Availability in Exercising Men Is Associated with Reduced Leptin and Insulin but Not with Changes in Other Metabolic Hormones. J. Sports Sci. 2016, 34, 1921–1929. [Google Scholar] [CrossRef] [Green Version]
- Fagerberg, P. Negative Consequences of Low Energy Availability in Natural Male Bodybuilding: A Review. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 385–402. [Google Scholar] [CrossRef]
- Kojima, C.; Ishibashi, A.; Tanabe, Y.; Iwayama, K.; Kamei, A.; Takahashi, H.; Goto, K. Muscle Glycogen Content during Endurance Training under Low Energy Availability. Med. Sci. Sports Exerc. 2020, 52, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Petrie, T.; Galli, N.; Greenleaf, C.; Reel, J.; Carter, J. Psychosocial Correlates of Bulimic Symptomatology among Male Athletes. Psychol. Sport Exerc. 2014, 15, 680–687. [Google Scholar] [CrossRef]
- Wasserfurth, P.; Palmowski, J.; Hahn, A.; Krüger, K. Reasons for and Consequences of Low Energy Availability in Female and Male Athletes: Social Environment, Adaptations, and Prevention. Sports Med. Open 2020, 6, 44. [Google Scholar] [CrossRef]
- Arnaoutis, G.; Kavouras, S.A.; Angelopoulou, A.; Skoulariki, C.; Bismpikou, S.; Mourtakos, S.; Sidossis, L.S. Fluid Balance During Training in Elite Young Athletes of Different Sports. J. Strength Cond. Res. 2015, 29, 3447–3452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kontele, I.; Vassilakou, T. Nutritional Risks among Adolescent Athletes with Disordered Eating. Children 2021, 8, 715. https://doi.org/10.3390/children8080715
Kontele I, Vassilakou T. Nutritional Risks among Adolescent Athletes with Disordered Eating. Children. 2021; 8(8):715. https://doi.org/10.3390/children8080715
Chicago/Turabian StyleKontele, Ioanna, and Tonia Vassilakou. 2021. "Nutritional Risks among Adolescent Athletes with Disordered Eating" Children 8, no. 8: 715. https://doi.org/10.3390/children8080715