Longitudinal Analysis (1994–2020) of Prevalence and Trends of Underweight in Polish Children
Abstract
:1. Introduction
2. Materials and Methods
Statistics
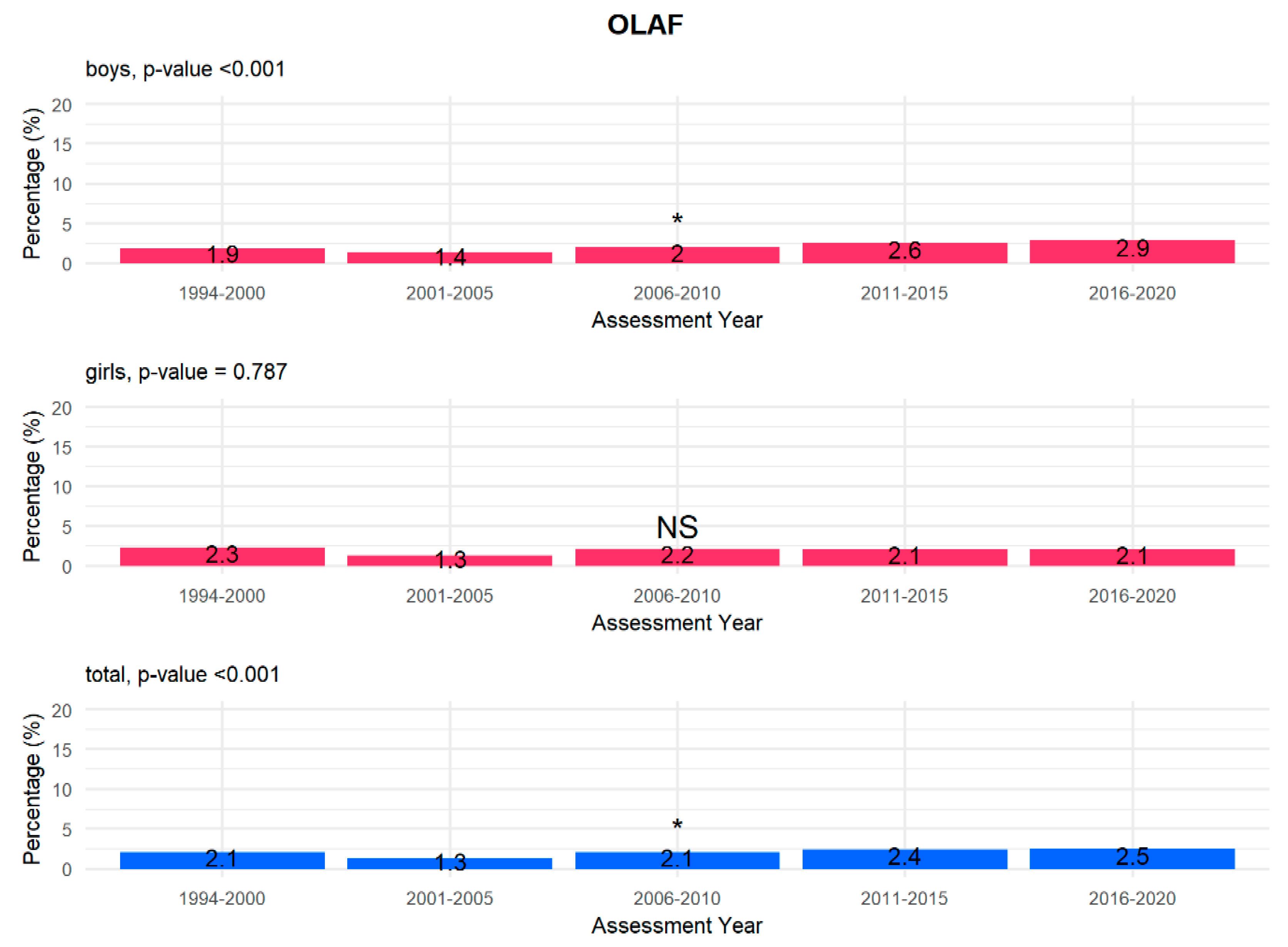
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Fact Sheets—Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 17 September 2020).
- Bhutta, Z.A.; Berkley, J.A.; Bandsma, R.H.; Kerac, M.; Trehan, I.; Briend, A. Severe childhood malnutrition. Nat. Rev. Dis. Primer 2017, 3, 17067. [Google Scholar] [CrossRef] [PubMed]
- Jarosz, M.; Rychlik, E. The problem of malnutrition in Poland and across the world. Postępy Nauk Med. 2012, 12, 917–923. [Google Scholar]
- Products—Health E Stats—Prevalence of Underweight among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2015–2016. Available online: https://www.cdc.gov/nchs/data/hestat/underweight_child_15_16/underweight_child_15_16.htm (accessed on 21 September 2020).
- Garrido-Miguel, M.; Martínez-Vizcaíno, V.; Oliveira, A.; Martínez-Andrés, M.; Sequí-Domínguez, I.; Hernández-Castillejo, L.E.; Cavero-Redondo, I. Prevalence and trends of underweight in European children and adolescents: A systematic review and meta-analysis. Eur. J. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Selzer, R.; Caust, J.; Hibbert, M.; Bowes, G.; Patton, G. The association between secondary amenorrhea and common eating disordered weight control practices in an adolescent population. J. Adolesc. Health 1996, 19, 56–61. [Google Scholar] [CrossRef]
- Country Nutrition Profiles. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/europe/ (accessed on 30 June 2021).
- Vizcaino, V.M.; Martínez, M.S.; Pacheco, B.N.; López, M.S.; García-Prieto, J.C.; Niño, C.T.; Palencia, N.A.; Aguilar, F.S.; Rodríguez-Artalejo, F. Trends in excess of weight, underweight and adiposity among Spanish children from 2004 to 2010: The Cuenca Study. Public Health Nutr. 2012, 15, 2170–2174. [Google Scholar] [CrossRef] [Green Version]
- Defining Childhood Obesity|Overweight & Obesity|CDC. Available online: https://www.cdc.gov/obesity/childhood/defining.html (accessed on 22 May 2021).
- Chabros, E.; Charzewska, J.; Wajszczyk, B.; Chwojnowska, Z. Częstość występowania niedoborowej masy ciała u młodzieży warszawskiej w wieku pokwitania w ostatnich 3 dekadach [Frequency of underweight in Warsaw adolescents in the last 3 decades]. Probl. Hig. Epidemiol. 2011, 92, 99–102. [Google Scholar]
- Kowal, M.; Woz, R.; Bac, A. Prevalence of underweight in children and adolescents (aged 3–18 years) from Kraków (Poland) in 1983 and 2010. Public Health Nutr. 2019, 22, 2210–2219. [Google Scholar] [CrossRef]
- Body Mass Index-for-Age (BMI-for-Age). Available online: https://www.who.int/toolkits/child-growth-standards/standards/body-mass-index-for-age-bmi-for-age (accessed on 22 May 2021).
- Kułaga, Z.; Grajda, A.; Gurzkowska, B.; Gozdz, M.; Wojtyło, M.; Swiader-Lesniak, A.; Różdżyńska-Świątkowska, A.; Litwin, M. Polish 2012 growth references for preschool children. Eur. J. Pediatr. 2013, 172, 753–761. [Google Scholar] [CrossRef] [Green Version]
- de Ruiter, I.; Olmedo-Requena, R.; Sánchez-Cruz, J.J.; Jiménez-Moleón, J.J. Trends in Child Obesity and Underweight in Spain by Birth Year and Age, 1983 to 2011. Rev. Esp. Cardiol. Engl. Ed. 2017, 70, 646–655. [Google Scholar] [CrossRef]
- Sjöberg, A.; Lissner, L.; Albertsson-Wikland, K.; Mårild, S. Recent anthropometric trends among Swedish school children: Evidence for decreasing prevalence of overweight in girls. Acta Paediatr. 2008, 97, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, G.; Rossi, S.; Kelly, C.; Vereecken, C.; Ahluwalia, N.; Giacchi, M.V. Trends in thinness prevalence among adolescents in ten European countries and the USA (1998–2006): A cross-sectional survey. Public Health Nutr. 2014, 17, 2207–2215. [Google Scholar] [CrossRef] [Green Version]
- Chourdakis, M.; Hecht, C.; Gerasimidis, K.; Joosten, K.F.; Karagiozoglou-Lampoudi, T.; Koetse, H.A.; Ksiazyk, J.; Lazea, C.; Shamir, R.; Szajewska, H.; et al. Malnutrition risk in hospitalized children: Use of 3 screening tools in a large European population. Am. J. Clin. Nutr. 2016, 103, 1301–1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarnivala, H.; Pokka, T.; Soininen, R.; Möttönen, M.; Harila-Saari, A.; Niinimäki, R. Trends in age- and sex-adjusted body mass index and the prevalence of malnutrition in children with cancer over 42 months after diagnosis: A single-center cohort study. Eur. J. Pediatr. 2020, 179, 91–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouzaki, M.; Bronsky, J.; Gupte, G.; Hojsak, I.; Jahnel, J.; Pai, N.; Quiros-Tejeira, R.E.; Wieman, R.; Sundaram, S. Nutrition Support of Children with Chronic Liver Diseases: A Joint Position Paper of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 498–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roszko-Kirpsza, I.; Olejnik, B.J.; Zalewska, M.; Marcinkiewicz, S.; Maciorkowska, E. Wybrane nawyki żywieniowe a stan odżywienia dzieci i młodzieży regionu Podlasia [Selected dietary habits and nutritional status of children and adolescents of the Podlasie region]. Probl. Hig. Epidemiol. 2011, 92, 799–805. [Google Scholar]
- Kolarzyk, E.; Janik, A.; Kwiatkowski, J. Zwyczaje żywieniowe dzieci w wieku przedszkolnym. [Nutritional habits of pre-school children]. Probl. Hig. Epidemiol. 2008, 89, 531–536. [Google Scholar]
- Janina Olejnik, B.; Roszko-Kirpsza, I.; Marcinkiewicz, S.; Maciorkowska, E. Uwarunkowania środowiskowe a stan odżywienia dzieci i młodzieży województwa podlaskiego [Environmental conditions and the nutritional status of children and adolescents in Podlaskie Voivodeship]. Pediatr. Pol. 2012, 87, 41–46. [Google Scholar] [CrossRef]
- Kelishadi, R.; Ardalan, G.; Gheiratmand, R.; Majdzadeh, R.; Hosseini, S.M.; Gouya, M.M.; Razaghi, E.M.; Delavari, A.; Motaghian, M.; Barekati, H.; et al. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008, 34, 44–54. [Google Scholar] [CrossRef]
- Rysha, A.; Gjergji, T.M.; Ploeger, A. Nutritional status of preschool children attending kindergartens in Kosovo. J. Health Popul. Nutr. 2017, 36, 26. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Ríos, M.; Santiago-Pérez, M.I.; Leis, R.; Malvar, A.; Suanzes, J.; Hervada, X. Prevalence of malnutrition in Spanish schoolchildren. An. Pediatr. 2018, 89, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Dereń, K.; Nyankovskyy, S.; Nyankovska, O.; Łuszczki, E.; Wyszyńska, J.; Sobolewski, M.; Mazur, A. The prevalence of underweight, overweight and obesity in children and adolescents from Ukraine. Sci. Rep. 2018, 8, 3625. [Google Scholar] [CrossRef] [PubMed]
- Malczyk, E. Stan odżywienia dzieci i młodzieży w Polsce na podstawie piśmiennictwa z ostatnich 10 lat (2005–2015). [Nutritional status of children and youth in Poland on basis of literature from last ten years (2005–2015). Ann. Acad. Med. Silesiensis 2016, 70, 56–65. [Google Scholar] [CrossRef]


| Total | Girls | Boys | p Value | |
|---|---|---|---|---|
| n | 67,842 (100%) | 32,752(48.28%) | 35,090 (51.72%) | |
| Mean age (SD) | 6.551 (0.357) | 6.549 (0.356) | 6.553 (0.359) | 0.164 |
| Mean weight (SD) | 23.420 (4.289) | 23.099 (4.205) | 23.719 (4.344) | <0.001 |
| Mean hight (SD) | 121.371 (5.551) | 120.865 (5.524) | 121.844 (5.534) | <0.001 |
| Mean BMI * z-score WHO ** (SD) | −0.145 (1.169) | −0.096 (1.080) | −0.192 (1.244) | <0.001 |
| Mean BMI * z-score OLAF *** (SD) | −0.078 (0.976) | −0.059 (0.973) | −0.096 (1.080) | <0.001 |
| WHO | OLAF | |||
|---|---|---|---|---|
| GIRLS | n | Mean BMI WHO z-Score (SD) | n | Mean BMI OLAF z-Score (SD) |
| 1994–2000 | 175 | −2.644 (0.974) | 200 | −2.824 (1.562) |
| 2001–2005 | 70 | −2.458 (0.492) | 77 | −2.541 (0.607) |
| 2006–2010 | 137 | −2.362 (0.379) | 155 | −2.426 (0.477) |
| 2011–2015 | 121 | −2.395 (0.379) | 151 | −2.413 (0.432) |
| 2016–2020 | 70 | −2.361 (0.317) | 85 | −2.395 (0.362) |
| WHO | OLAF | |||
|---|---|---|---|---|
| BOYS | n | Mean WHO z-Score (SD) | n | Mean OLAF z-Score (SD) |
| 1994–2000 | 179 | −2.673 (1.114) | 180 | −2.960 (2.866) |
| 2001–2005 | 84 | −2.577 (0.711) | 82 | −2.670 (1.082) |
| 2006–2010 | 162 | −2.420 (0.403) | 150 | −2.450 (0.422) |
| 2011–2015 | 202 | −2.502 (0.568) | 195 | −2.552 (1.131) |
| 2016–2020 | 119 | −2.394 (0.330) | 125 | −2.373 (0.346) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lemanowicz-Kustra, A.; Borkowska, A.; Brzeziński, M.; Wyszomirski, A.; Szlagatys-Sidorkiewicz, A. Longitudinal Analysis (1994–2020) of Prevalence and Trends of Underweight in Polish Children. Children 2021, 8, 643. https://doi.org/10.3390/children8080643
Lemanowicz-Kustra A, Borkowska A, Brzeziński M, Wyszomirski A, Szlagatys-Sidorkiewicz A. Longitudinal Analysis (1994–2020) of Prevalence and Trends of Underweight in Polish Children. Children. 2021; 8(8):643. https://doi.org/10.3390/children8080643
Chicago/Turabian StyleLemanowicz-Kustra, Aleksandra, Anna Borkowska, Michał Brzeziński, Adam Wyszomirski, and Agnieszka Szlagatys-Sidorkiewicz. 2021. "Longitudinal Analysis (1994–2020) of Prevalence and Trends of Underweight in Polish Children" Children 8, no. 8: 643. https://doi.org/10.3390/children8080643
APA StyleLemanowicz-Kustra, A., Borkowska, A., Brzeziński, M., Wyszomirski, A., & Szlagatys-Sidorkiewicz, A. (2021). Longitudinal Analysis (1994–2020) of Prevalence and Trends of Underweight in Polish Children. Children, 8(8), 643. https://doi.org/10.3390/children8080643







