A Novel Tool to Assess Basic Activities of Daily Living in Spanish Preschoolers
Abstract
1. Introduction
1.1. Activities of Daily Living Conceptualization and Development
1.2. Underlying Factors in Activities of Daily Living
1.3. Activities of Daily Living in Early Education and Early Intervention Services
1.4. Assessment of Activities of Daily Living in Preschoolers
1.5. Aim
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instruments and Procedure
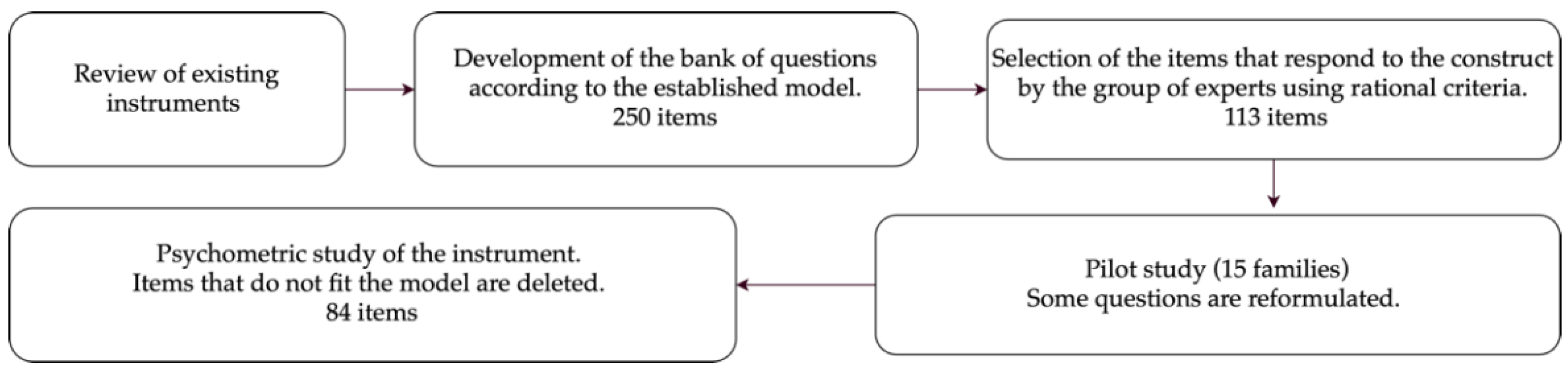
2.3.1. Creation of the Basic Activities of Daily Living Assessment in Preschoolers
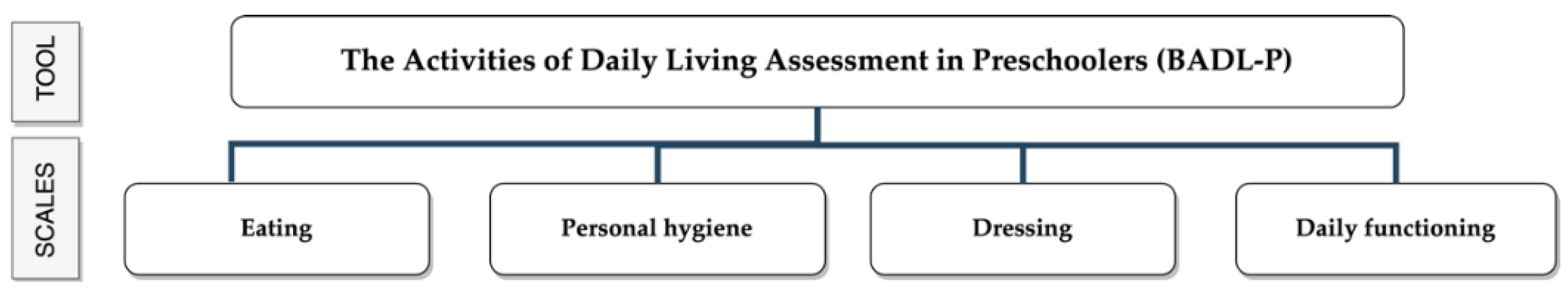
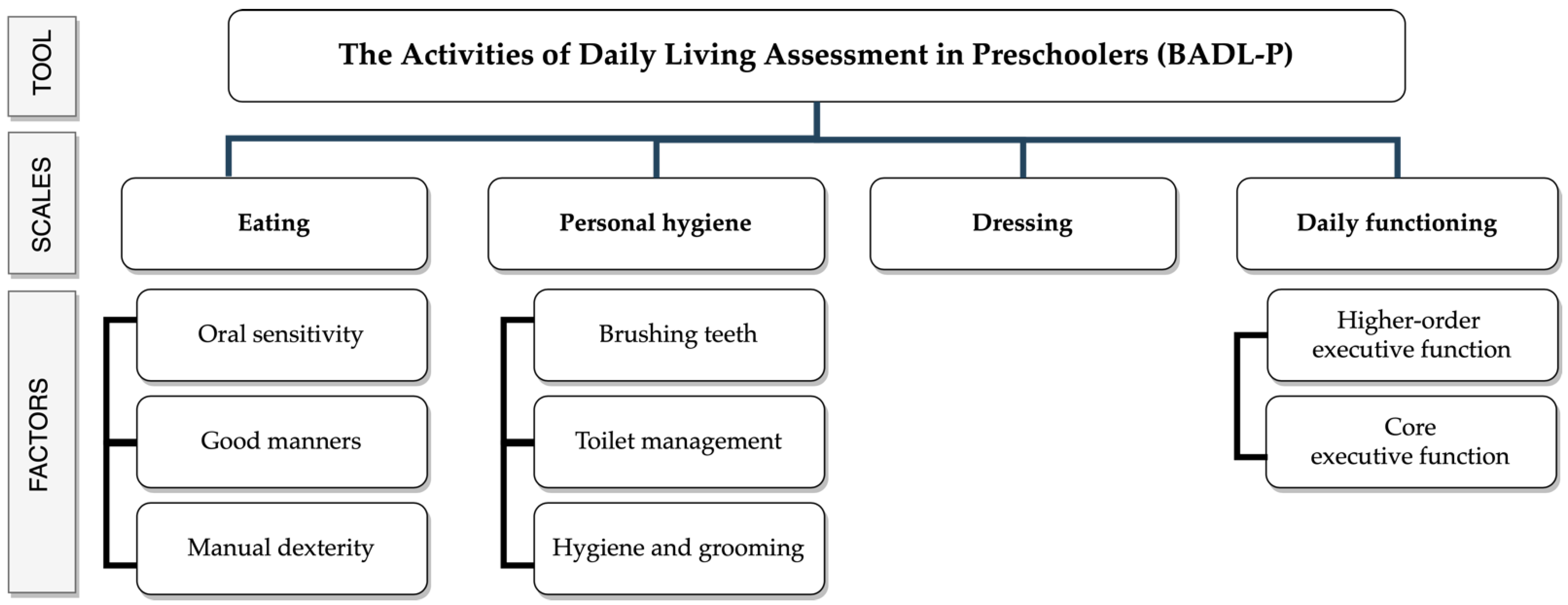
2.3.2. Description of the Basic Activities of Daily Living Assessment in Preschoolers Tool
2.4. Ethical Approval
2.5. Statistics
3. Results
3.1. Item Analysis and Internal Structure of the Questionnaire
3.1.1. Eating Scale
3.1.2. Personal Hygiene Scale
3.1.3. Dressing Scale
3.1.4. Daily Functioning Scale
3.2. Correlations between Factors
3.3. Goodness-of-Fit Indices
3.4. Reliability
3.5. Results According to Sociometric Variables and Questionnaire Structure
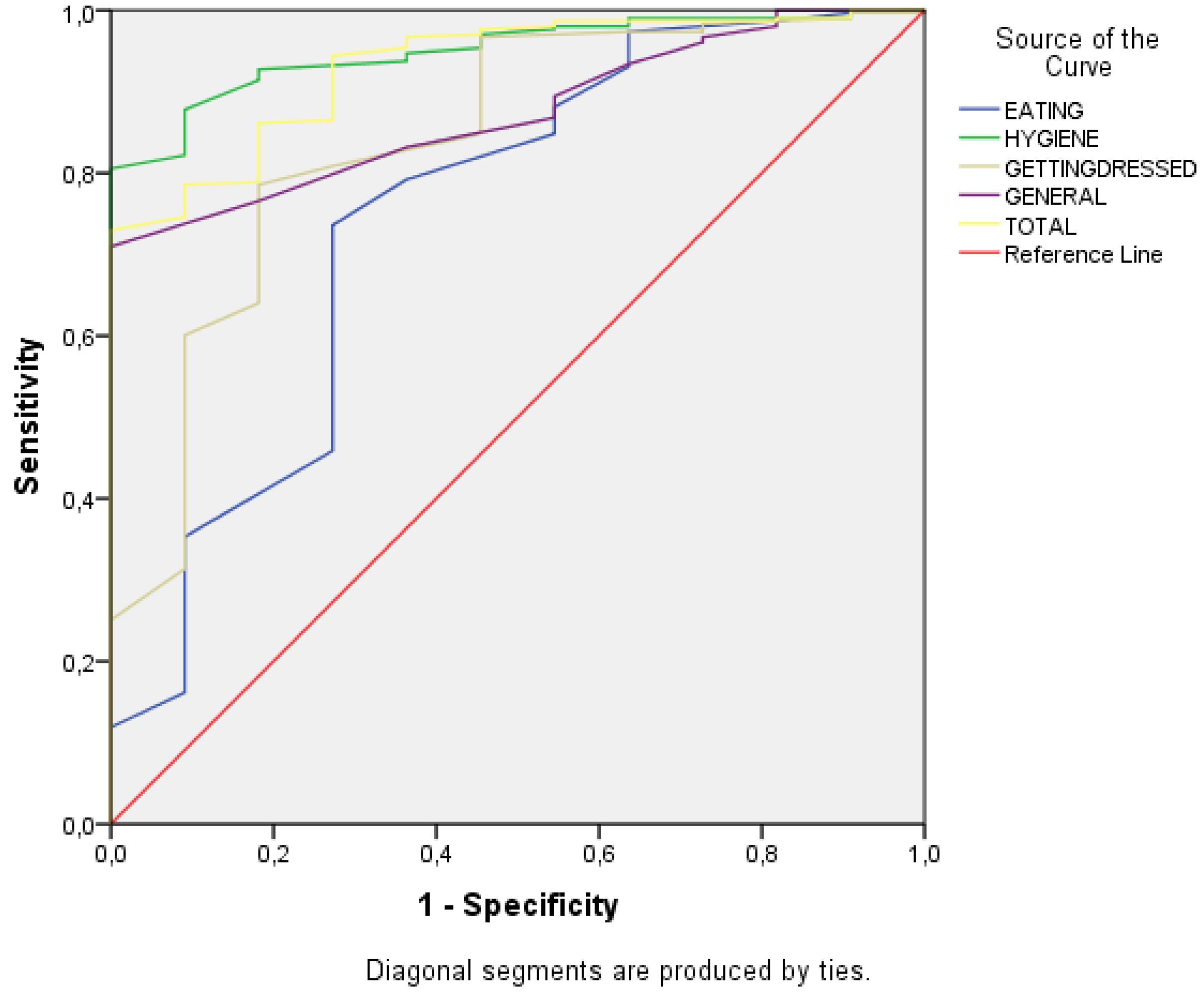
3.6. The Basic Activities of Daily Living Assessment in Preschoolers Discrimination Ability between Typically Developing Participants and a Sample of ASD Participants
4. Discussion
4.1. The Basic Activities of Daily Living Assessment in Preschoolers Theoretical Model
4.2. The Basic Activities of Daily Living Assessment in Preschoolers and Other Tools
4.3. The Basic Activities of Daily Living Assessment in Preschoolers Psychometric Properties
4.4. Limitations and Future Lines
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gronski, M.; Doherty, M. Interventions Within the Scope of Occupational Therapy Practice to Improve Activities of Daily Living, Rest, and Sleep for Children Ages 0–5 Years and Their Families: A Systematic Review. Am. J. Occup. Ther. 2020, 74, 7402180010p1–7402180010p33. [Google Scholar] [CrossRef]
- American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process—Third Edtion. Am. J. Occup. Ther. 2017, 68, S1–S48. [Google Scholar] [CrossRef]
- Romero, D.M. Actividades de la vida diaria desde una perspectiva evolutiva. In Actividades de la Vida Diaria; Moruno, P., Romero, D.M., Eds.; Masson: Barcelona, Spain, 2006; pp. 23–34. [Google Scholar]
- Edemekong, P.F.; Bomgaars, D.L.; Sukumaran, S.; Levy, S.B. Activities of Daily Living; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Delval, J.A. El Desarrollo Humano; Siglo Veintiuno Editores: Mexico DF, Mexico, 2006; ISBN 978-968-23-1990-7. [Google Scholar]
- Duncan, E.A.S. Foundations for Practice in Occupational Therapy; Elsevier Health Sciences: Saint Louis, MO, USA, 2014; ISBN 978-0-7020-4661-2. [Google Scholar]
- Moruno Miralles, P.; Romero Ayuso, D.M. Actividades de la Vida Diaria; Masson: Madrid, Spain, 2006; ISBN 978-84-458-1561-8. [Google Scholar]
- Rodger, S.; Ziviani, J. (Eds.) Occupational Therapy with Children: Understanding Children’s Occupations and Enabling Participation; Blackwell Pub: Oxford, UK; Malden, MA, USA, 2006; ISBN 978-1-4051-2456-0. [Google Scholar]
- Rodger, S.; Ziviani, J. Hand Function in the Child: Foundations for Remediation, 2nd ed.; Henderson, A., Pehoski, C., Eds.; Mosby/Elsevier: Saint Louis, MO, USA, 2006; ISBN 978-0-323-03186-8. [Google Scholar]
- Shepherd, J. Self care: A primary occupation. I can do it myself! In Kids Can Be Kids: A Childhood Occupations Approach; FA Davis: Baltimore, MD, USA, 2012; pp. 125–158. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- Gantschnig, B.E.; Page, J.; Nilsson, I.; Fisher, A.G. Detecting Differences in Activities of Daily Living Between Children With and Without Mild Disabilities. Am. J. Occup. Ther. 2013, 67, 319–327. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bal, V.H.; Kim, S.-H.; Cheong, D.; Lord, C. Daily Living Skills in Individuals with Autism Spectrum Disorder from 2 to 21 Years of Age. Autism 2015, 19, 774–784. [Google Scholar] [CrossRef]
- Van der Linde, B.W.; van Netten, J.J.; Otten, B.; Postema, K.; Geuze, R.H.; Schoemaker, M.M. Activities of Daily Living in Children With Developmental Coordination Disorder: Performance, Learning, and Participation. Phys. Ther. 2015, 95, 1496–1506. [Google Scholar] [CrossRef]
- Günal, A.; Bumin, G.; Huri, M. The Effects of Motor and Cognitive Impairments on Daily Living Activities and Quality of Life in Children with Autism. J. Occup. Ther. Sch. Early Interv. 2019, 1–11. [Google Scholar] [CrossRef]
- Goyal, N.; Siddiqui, S.; Chatterjee, U.; Kumar, D.; Siddiqui, A. Neuropsychology of Prefrontal Cortex. Indian J. Psychiatry 2008, 50, 202. [Google Scholar] [CrossRef]
- Best, J.R.; Miller, P.H. A Developmental Perspective on Executive Function: Development of Executive Functions. Child. Dev. 2010, 81, 1641–1660. [Google Scholar] [CrossRef]
- Miyake, A.; Friedman, N.P.; Emerson, M.J.; Witzki, A.H.; Howerter, A.; Wager, T.D. The Unity and Diversity of Executive Functions and Their Contributions to Complex “Frontal Lobe” Tasks: A Latent Variable Analysis. Cogn. Psychol. 2000, 41, 49–100. [Google Scholar] [CrossRef]
- Tirapu Ustárroz, J.; Bausela Herreras, E.; Cordero Andrés, P. Modelo de funciones ejecutivas basado en análisis factoriales en población infantil y escolar: Metaanálisis. Rev. Neurol. 2018, 67, 215. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. The early development of executive functions. In Lifespan Cognition: Mechanisms of Change; Oxford University Press: New York, NY, USA, 2006; pp. 466–503. [Google Scholar]
- Martos Pérez, J.; Paula Pérez, I. Una aproximación a las funciones ejecutivas en el trastorno del espectro autista. Rev. Neurol. 2011, 52, S147. [Google Scholar] [CrossRef]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef]
- Aydmune, Y.S.; Introzzi, I.M.; Zamora, E.V.; Lipina, S.J. Diseño, Implementación y Análisis de Transferencia de Una Tarea de Entrenamiento de Inhibición Cognitiva Para Niños Escolares. Un Estudio Piloto. Psicl. Educ. 2018, 24, 63–74. [Google Scholar] [CrossRef]
- Collins, A.; Koechlin, E. Reasoning, Learning, and Creativity: Frontal Lobe Function and Human Decision-Making. PLoS Biol. 2012, 10, e1001293. [Google Scholar] [CrossRef] [PubMed]
- García-Molina, A.; Enseñat-Cantallops, A.; Tirapu-Ustárroz, J.; Roig-Rovira, T. Maduración de La Corteza Prefrontal y Desarrollo de Las Funciones Ejecutivas Durante Los Primeros Cinco Años de Vida. Rev. Neurol. 2009, 48, 435. [Google Scholar] [CrossRef] [PubMed]
- Papazian, O.; Alfonso, I.; Luzondo, R.J. Trastornos de Las Funciones Ejecutivas. Rev. Neurol. 2006, 42, 45–50. [Google Scholar] [CrossRef]
- Howard, S.J.; Vasseleu, E. Self-Regulation and Executive Function Longitudinally Predict Advanced Learning in Preschool. Front. Psychol. 2020, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Howard, S.J.; Vasseleu, E.; Batterham, M.; Neilsen-Hewett, C. Everyday Practices and Activities to Improve Pre-School Self-Regulation: Cluster RCT Evaluation of the PRSIST Program. Front. Psychol. 2020, 11, 137. [Google Scholar] [CrossRef]
- Romero-Ayuso, D.; Toledano-González, A.; Segura-Fragoso, A.; Triviño-Juárez, J.M.; Rodríguez-Martínez, M.C. Assessment of Sensory Processing and Executive Functions at the School: Development, Reliability, and Validity of EPYFEI-Escolar. Front. Pediatr. 2020, 8, 275. [Google Scholar] [CrossRef] [PubMed]
- Fogel, Y.; Rosenblum, S.; Josman, N. Environmental Factors and Daily Functioning Levels among Adolescents with Executive Function Deficits. Br. J. Occup. Ther. 2020, 83, 88–97. [Google Scholar] [CrossRef]
- Kellegrew, D.H. Constructing Daily Routines: A Qualitative Examination of Mothers With Young Children With Disabilities. Am. J. Occup. Ther. 2000, 54, 252–259. [Google Scholar] [CrossRef]
- Aguilar-Yamuza, B.; Raya-Trenas, A.F.; Pino-Osuna, M.J.; Herruzo-Cabrera, J. Relación Entre El Estilo de Crianza Parental y La Depresión y Ansiedad En Niños Entre 3 y 13 Años. RPCNA 2019, 6, 36–43. [Google Scholar] [CrossRef]
- Ministerio de Educación y Ciencia. Orden ECI/3960/2007, de 19 de Diciembre, por la que se Establece el Currículo y se Regula la Ordenación de la Educación Infantil; Ministerio de Educación y Ciencia: Madrid, Spain, 2007; Volume 5, pp. 1016–1036.
- Ministerio de Educación. Decreto 4/2008, de 11 de enero, por el que se aprueba el Currículo de Educación Infantil para la Comunidad Autónoma de Extremadura; Ministerio de Educación: Madrid, Spain, 2008; Volume 12, pp. 1226–1276.
- Lipkin, P.H.; Macias, M.M. Promoting Optimal Development: Identifying Infants and Young Children With Developmental Disorders Through Developmental Surveillance and Screening. Pediatrics 2020, 145, e20193449. [Google Scholar] [CrossRef]
- Filipek, P.A.; Accardo, P.J.; Ashwal, S.; Baranek, G.T.; Cook, E.H.; Dawson, G.; Gordon, B.; Gravel, J.S.; Johnson, C.P.; Kallen, R.J.; et al. Practice Parameter: Screening and Diagnosis of Autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000, 55, 468–479. [Google Scholar] [CrossRef]
- Federación Estatal de Asociaciones de Profesionales de Atención Temprana. Libro Blanco de La Atención Temprana; Real Patronato sobre Discapacidad: Madrid, Spain, 2005. [Google Scholar]
- Heredia, M.C. Influencia del contexto familiar y social en el desarrollo del niño y sus alteraciones. In Psicopatología, Riesgo y Tratamiento de los Problemas Infantiles; Gómez-Maqueo, E.L., Heredia, M.C., Eds.; Manual Moderno: Mexico DF, Mexico, 2014; pp. 27–48. [Google Scholar]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Encuesta Nacional de Salud: España 2011/12. Salud Mental y Calidad de Vida En La Población Infantil. Serie Informes monográficos No. 2; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2014. [Google Scholar]
- Díaz Sánchez, C. Guía Básica Sobre Atención Temprana y Transformación. Cuadernos de Buenas Prácticas; Plena Inclusión: Madrid, Spain, 2019. [Google Scholar]
- Mcwilliam, R. Metanoia En Atención Temprana: Transformación a Un Enfoque Centrado En La Familia. Rev. Latinoam. Educ. Inclusiva 2016, 10, 133–153. [Google Scholar] [CrossRef]
- McWilliam, R.A. Routines-Based Early Intervention: Supporting Young Children and Their Families; Paul H. Brookes: Baltimore, MD, USA, 2010; ISBN 978-1-59857-062-5. [Google Scholar]
- Hughes-Scholes, C.H.; Gavidia-Payne, S. Development of a Routines-Based Early Childhood Intervention Model. Educ. Rev. 2016, 141–154. [Google Scholar] [CrossRef]
- Sparrow, S.S.; Cichetti, D.V.; Balla, D.A. Vineland Adaptive Behavior Scales, 2nd ed.; American Guidance Service: Circle Pines, MN, USA, 2005. [Google Scholar]
- Sparrow, S.S.; Cichetti, D.V.; Saulnier, C.A. Vineland Adaptive Behavior Scales, 3rd ed.; Pearson: San Antonio, TX, USA, 2016. [Google Scholar]
- Harrison, P.L.; Oakland, T. Adaptive Behavior Assessment System, 2nd ed.; Psychological Corp.: San Antonio, TX, USA, 2003; ISBN 978-0-15-400452-9. [Google Scholar]
- Harrosin, P.; Oakland, T. Adaptive Behavior Assessment System, 3rd ed.; Pearson: San Antonio, TX, USA, 2015. [Google Scholar]
- Morreau, L.E.; Bruininks, R.H.; Montero Centeno, D. Inventario de Destrezas Adaptativas (CALS): Manual; Instituto de Ciencias de la Educación: Oaxaca de Juárez, Spain; Universidad de Deusto, Mensajero: Bilbao, Spain, 2006; ISBN 978-84-271-2480-6. [Google Scholar]
- Bruininks, R.K.; Hill, B.K.; Weatherman, R.F.; Woodcock, R.W. Inventary for Client and Agency Planning; The Riverside Pub. Co.: Chicago, IL, USA, 1986. [Google Scholar]
- Haley, S.M.; Coster, W.J.; Dumas, H.M.; Fragala-Pinkham, M.A.; Moed, R. PEDI-CAT: Development, Standardization and Administration Manual; Boston University: Boston, MA, USA, 2012. [Google Scholar]
- de la Cruz, M.V.; González Criado, M.; Newborg, J. Battelle, Inventario de Desarrollo: Manual de Aplicación; TEA: Madrid, Spain, 1996; ISBN 978-84-7174-421-0. [Google Scholar]
- Sánchez, F.; Santamaría, P.; Fernández-Pinto, I.; Arribas, D. Escalas de Desarrollo Merrill-Palmer Revisadas; TEA: Madrid, Spain, 2011. [Google Scholar]
- Romero, D.M. Actividades de La Vida Diaria. An. Psicol. 2007, 23, 264–271. [Google Scholar]
- World Medical Association. A Fifth Amendment for the Declaration of Helsinki. Lancet 2000, 356, 1123. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Lorenzo-Seva, U. Program FACTOR at 10: Origins, Development and Future Directions. Psicothema 2017, 236–240. [Google Scholar] [CrossRef]
- Watkins, M.W. Exploratory Factor Analysis: A Guide to Best Practice. J. Black Psychol. 2018, 44, 219–246. [Google Scholar] [CrossRef]
- Lloret, S.; Ferreres, A.; Hernández, A.; Tomás, I. The Exploratory Factor Analysis of Items: Guided Analysis Based on Empirical Data and Software. An. Psicol. 2017, 33, 417–432. [Google Scholar] [CrossRef]
- Lorenzo-Seva, U.; Ferrando, P.J. FACTOR v. 10.10.02. Windows; Universitat Rovira i Virgili: Tarragona, Spain, 2020. [Google Scholar]
- Lorenzo-Seva, U.; Ferrando, P.J. FACTOR 9.2: A Comprehensive Program for Fitting Exploratory and Semiconfirmatory Factor Analysis and IRT Models. Appl. Psychol. Meas. 2013, 37, 497–498. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Lorenzo-Seva, U. El Análisis Factorial Exploratorio de Los Ítems: Algunas Consideraciones Adicionales. An. Psicol. 2014, 30, 1170–1175. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: User’s Reference Guide, 2nd ed.; Scientific Software International: Chicago, IL, USA, 1996. [Google Scholar]
- Frías-Navarro, M.D.F.; Pascual-Soler, M.P. Prácticas del análisis factorial exploratorio (AFE) en la investigación sobre conducta del consumidor y marketing. Suma Psicol. 2012, 19, 47–58. [Google Scholar]
- Beavers, A.S.; Lounsbury, J.W.; Richards, J.K.; Huck, S.W.; Skolits, G.J.; Esquivel, S.L. Practical Considerations for Using Exploratory Factor Analysis in Educational Research. PARE 2013, 18, 1–13. [Google Scholar]
- Ferrando, P.J.; Anguiano-Carrasco, C. El análisis factorial como técnica de investigación en psicología. Pap. Psicólogo 2010, 31, 18–33. [Google Scholar]
- Gadermann, A.; Guhn, M.; Zumbo, B.D. Ordinal Alpha. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 4513–4515. ISBN 978-94-007-0752-8. [Google Scholar]
- Dominguez-Lara, S. Fiabilidad y alfa ordinal. Actas Urológicas Españolas 2018, 42, 140–141. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, MI, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Barrios-Fernández, S.; Gozalo, M.; García-Gómez, A.; Romero-Ayuso, D.; Hernández-Mocholí, M.Á. A New Assessment for Activities of Daily Living in Spanish Schoolchildren: A Preliminary Study of Its Psychometric Properties. Int. J. Environ. Res. Public Health 2020, 17, 2673. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, N.; Jackson, J.; Revueltas Roux, A.; Moriguchi, Y.; Auyeung, B. Differentiation in Prefrontal Cortex Recruitment during Childhood: Evidence from Cognitive Control Demands and Social Contexts. Dev. Cogn. Neurosci. 2019, 36, 100629. [Google Scholar] [CrossRef]
- Jefferson, A.; Paul, R.; Ozonoff, A.; Cohen, R. Evaluating Elements of Executive Functioning as Predictors of Instrumental Activities of Daily Living (IADLs). Arch. Clin. Neuropsychol. 2006, 21, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Poncet, F.; Swaine, B.; Dutil, E.; Chevignard, M.; Pradat-Diehl, P. How Do Assessments of Activities of Daily Living Address Executive Functions: A Scoping Review. Neuropsychol. Rehabil. 2017, 27, 618–666. [Google Scholar] [CrossRef]
- American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain & Process 2nd Edition. Am. J. Occup. Ther. 2008, 62, 625–683. [Google Scholar] [CrossRef]
- American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am. J. Occup. Ther. 2020, 74, 7412410010p1. [Google Scholar] [CrossRef]
- Montero, D.; Fernández-Pinto, I. ABAS® II: Sistema Para la Evaluación de la Conducta Adaptativa: Manual; TEA: Madrid, Spain, 2013; ISBN 978-84-15262-76-3. [Google Scholar]
- Johnson-Martín, N.M.; Jens, K.G.; Attermeier, S.M.; Hacker, B.J. Curriculo Carolina; TEA: Madrid, Spain, 1997. [Google Scholar]
- Fragala-Pinkham, M.A.; Miller, P.E.; Dumas, H.M.; Shore, B.J. Development and Validation of Equations to Link Pediatric Evaluation of Disability Inventory (PEDI) Functional Skills Scores to PEDI-Computer Adaptive Test Scores for Youth with Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2020, 40, 106–120. [Google Scholar] [CrossRef]
- Dzhambov, A.M. Perceived Benefits of Nature Questionnaire: Preliminary Results. Ecopsychology 2014, 6, 109–115. [Google Scholar] [CrossRef]
- Leveau, L.M. Bird Traits in Urban–Rural Gradients: How Many Functional Groups Are There? J. Ornithol. 2013, 154, 655–662. [Google Scholar] [CrossRef]
- Ginns, P.; Marsh, H.W.; Behnia, M.; Cheng, J.H.S.; Scalas, L.F. Using Postgraduate Students’ Evaluations of Research Experience to Benchmark Departments and Faculties: Issues and Challenges. Br. J. Educ. Psychol. 2009, 79, 577–598. [Google Scholar] [CrossRef]
- Ficapal-Cusí, P.; Boada-Grau, J.; Torrent-Sellens, J. Spanish Adaptation of the Internal Functioning of the Work Teams Scale (QFI-22). Psicothema 2014, 26, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Maki, W.S.; Buchanan, E. Latent Structure in Measures of Associative, Semantic, and Thematic Knowledge. Psychon. Bull. Rev. 2008, 15, 598–603. [Google Scholar] [CrossRef][Green Version]
- Özer, B.U.; Saçkes, M.; Tuckman, B.W. Psychometric Properties of the Tuckman Procrastination Scale in a Turkish Sample. Psychol. Rep. 2013, 113, 874–884. [Google Scholar] [CrossRef]
- Barbu, O.C.; Marx, R.W.; Yaden, D.B.; Levine-Donnerstein, D. Measuring Approaches to Learning in Preschoolers: Validating the Structure of an Instrument for Teachers and Parents. Education 2016, 44, 698–714. [Google Scholar] [CrossRef]
- Begega, A.; Méndez López, M.; de Iscar, M.J.; Cuesta-Izquierdo, M.; Solís, G.; Fernández-Colomer, B.; Álvarez, L.; Méndez, M.; Arias, J.L. Assessment of the Global Intelligence and Selective Cognitive Capacities in Preterm. Psicothema 2010, 22, 648–653. [Google Scholar]
- Daset, L.R.; Fernandez-Pintos, M.E.; Costa-Ball, D.; López-Soler, C.; Vanderplasschen, W.P. Development and validation of adolescent self-report: ADA. Ciencias Psicol. 2015, 9, 85–104. [Google Scholar]
- Ortuño-Sierra, J.; Fonseca-Pedrero, E.; Paino, M.; Sastre i Riba, S.; Muñiz, J. Screening Mental Health Problems during Adolescence: Psychometric Properties of the Spanish Version of the Strengths and Difficulties Questionnaire. J. Adolesc. 2015, 38, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Campelo, P.; Bragado-Álvarez, C.; Hernández-Lloreda, M.J.; Sánchez-Bernardos, M.L. The Spanish Version of the Body Image Scale (S-BIS): Psychometric Properties in a Sample of Breast and Gynaecological Cancer Patients. Support. Care Cancer 2015, 23, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Hennegan, J.; Nansubuga, A.; Smith, C.; Redshaw, M.; Akullo, A.; Schwab, K.J. Measuring Menstrual Hygiene Experience: Development and Validation of the Menstrual Practice Needs Scale (MPNS-36) in Soroti, Uganda. BMJ Open 2020, 10, e034461. [Google Scholar] [CrossRef]
- Stene, K.L.; Dow-Fleisner, S.J.; Ermacora, D.; Agathen, J.; Falconnier, L.; Stager, M.; Wells, S.J. Measuring the Quality of Care in Kinship Foster Care Placements. Child. Youth Serv. Rev. 2020, 116, 105136. [Google Scholar] [CrossRef]
- Pucciarelli, G.; Årestedt, K.; Simeone, S.; Bolgeo, T.; Alvaro, R.; Vellone, E. Psychometric Characteristics of the WHOQOL-SRPB Scale in a Population of Stroke Survivors and Caregivers. Qual. Life Res. 2020, 29, 1973–1985. [Google Scholar] [CrossRef]
- Rosen, C.; Chase, K.A.; Perona-Garcelán, S.; Marvin, R.W.; Sharma, R.P. The Psychometric Properties of the DAIMON Scale, a Translation from Spanish to English: An Instrument to Measure the Relationship with and between Voices. Psychosis 2020, 12, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Kottorp, A.; Bernspang, B.; Fisher, A.G. Activities of Daily Living in Persons with Intellectual Disability: Strengths and Limitations in Specific Motor and Process Skills. Aust. Occup. Ther. J. 2003, 50, 195–204. [Google Scholar] [CrossRef]
- Rosenblum, S.; Frisch, C.; Deutsh-Castel, T.; Josman, N. Daily Functioning Profile of Children with Attention Deficit Hyperactive Disorder: A Pilot Study Using an Ecological Assessment. Neuropsychol. Rehabil. 2015, 25, 402–418. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Proceedings of the The United Nations Conference Sustainable Development (UNCSD or “Rio+20”), Rio de Janiero, Brazil, 20–22 June 2012.
| Age | Feeding | Personal Hygiene | Getting Dressed |
|---|---|---|---|
| 3 years | Uses spoon and fork. Drinks safely. | Turns taps. Handles clothes before the toilet. | Takes off his shoes. Takes off his shirt. |
| 4 years | Uses the napkin. Mature spoon and fork grip. | Washes hands and face. Soaps his body. | Puts on top clothes. Buttons up. |
| 5 years | Cuts with the knife. Eats by himself. | Brushes his teeth. Cleans himself in the toilet. | Puts shoes on the right foot. Dresses unsupervised. |
| 6 years | Spreads with a knife. All skills are improved. | Blows his nose. Washes hands before eating. | Laces shoes. Handles zippers. |
| Preschool—First Stage | Preschool—Second Stage |
|---|---|
| Area 1. Awakening of personal identity: • Exploration and identification of the parts of the body, pointing and naming them in activities of daily living such as dressing or personal hygiene. Area 2. Personal well-being and daily life: • Progressive adaptation of one’s biological rhythms to socially established routines. • Identification of basic needs such as thirst, hygiene, sleep, satisfying them independently or asking for help. • Acquisition of basic habits and rules regarding food, cleanliness, resting or clothing, identifying utensils and spaces and using them properly. • Satisfaction from participating in activities of daily living, progressively assuming responsibility. • Confidence in one’s possibilities to solve tasks and overcoming difficulties with help. | Area 1. The body and the image itself: • Identification, regulation, and control of the basic needs of the body. Area 3. Activities of daily living: • Performing activities of daily living with progressive independence and the creation of habits. • Initiative, organization, planning, attention, constancy, and regulation skills while performing activities of daily living. Area 4. Personal care and health: • Actions to improve health and well-being for oneself and others. • Healthy habits: body hygiene, food and resting. • Appropriate use of spaces and utensils. • Preference for a well-groomed appearance. • Collaboration in the maintenance of clean and tidy environments. • Respect for the social rules during meals, resting and hygiene, with progressive initiative in their fulfilment. |
| Item | Factorial Weight | ||
|---|---|---|---|
| Factor 1: Oral sensitivity. | |||
| The child is reluctant to try new foods. | 0.820 | ||
| The child is unwilling to eat food with some textures. | 0.843 | ||
| The child shows disgust when certain foods are within his mouth. | 0.500 | ||
| Factor 2: Good manners. | |||
| The child tests the food carefully to check its temperature. | 0.394 | ||
| The child chews with his mouth closed. | 0.508 | ||
| The child chews food until crushed before swallowing. | 0.343 | ||
| The child maintains a proper posture during mealtime. | 0.685 | ||
| The child keeps seated at the table during mealtime. | 0.774 | ||
| The child uses napkins properly. | 0.417 | ||
| The child tries to maintain good manners during mealtime. | 0.676 | ||
| Factor 3: Manual dexterity while eating. | |||
| The child can open wrappers. | 0.380 | ||
| The child uses tools to open containers. | 0.450 | ||
| The child uses a knife to spread. | 0.747 | ||
| The child uses a knife to cut food. | 0.884 | ||
| The child uses several cutleries in a coordinated way. | 0.792 | ||
| The child can serve food from a bowl or tray. | 0.652 | ||
| Item | Factorial Weight | ||
|---|---|---|---|
| Factor 1: Brushing teeth. | |||
| The child brushes his teeth after eating without being told by an adult. | 0.545 | ||
| The child brushes for at least one minute. | 0.839 | ||
| The child brushes most or all areas of his mouth. | 0.836 | ||
| The child spits into the wash when brushing his teeth. | 0.808 | ||
| The child checks there are no traces of paste left in his mouth or face. | 0.493 | ||
| The child leaves the sink clean and picks up everything after brushing. | 0.453 | ||
| Factor 2: Toilet management. | |||
| The child stays poopless at night. | 0.688 | ||
| The child stays dry at night, without peeing. | 0.510 | ||
| The child keeps clean during the day, without pooping himself. | 0.726 | ||
| The child keeps dry during the day, without peeing himself. | 0.746 | ||
| The child communicates his need to go to the bathroom. | 0.713 | ||
| The child acceptably gets clean with toilet paper. | 0.384 | ||
| The child can lower or raise his clothes to use the toilet. | 0.449 | ||
| The child lowers the lid and pulls the chain. | 0.431 | ||
| The child cares about his privacy. | 0.313 | ||
| Factor 3: Hygiene and grooming. | |||
| The child collaborates using cologne or moisturizer. | 0.359 | ||
| The child keeps his nails clean. | 0.408 | ||
| The child brushes his hair. | 0.579 | ||
| The child checks his appearance before leaving home. | 0.479 | ||
| The child is aware when he needs to wipe his nose. | 0.540 | ||
| The child blows his nose. | 0.468 | ||
| The child checks and adjusts the water temperature | 0.575 | ||
| The child when washing his hands, spreads soap and water in his hands. | 0.540 | ||
| The child when washing his hands, uses an adequate amount of soap. | 0.519 | ||
| The child when washing his hands, wipes himself completely dry. | 0.467 | ||
| The child washes his face. | 0.677 | ||
| In the shower, soaps up all over the body. | 0.848 | ||
| In the shower, rinses until all foam is removed. | 0.835 | ||
| In the shower, uses the towel until is relatively dry. | 0.714 | ||
| In the shower, lathers his hair in an acceptable way. | 0.635 | ||
| Item | Factorial Weight |
|---|---|
| The child makes sure that the label of the clothes is in the right place. | 0.566 |
| The child put. his socks properly. | 0.736 |
| The child puts footwear on his feet. | 0.699 |
| The child places a shoe on the right foot. | 0.657 |
| The child removes shoes with fasteners. | 0.320 |
| The child removes simple garments without closures. | 0.538 |
| The child undresses completely, including using zippers on garments. | 0.717 |
| The child takes off his clothes, leaving them on the right side. | 0.523 |
| The child puts on a coat or an open garment. | 0.624 |
| The child puts on stretching pants. | 0.733 |
| The child puts on a T-shirt or an upper garment. | 0.738 |
| The child gets dressed without help (not including closures). | 0.838 |
| The child puts on accessories. | 0.518 |
| The child clasps snap buttons. | 0.691 |
| The child zips up and down. | 0.648 |
| The child zips clothes up. | 0.693 |
| The child can unbutton. | 0.756 |
| The child opens buttons. | 0.775 |
| The child undoes his shoes’ lacing. | 0.542 |
| The child ties a knot in his shoes. | 0.499 |
| The child gets dressed without help (closures and accessories). | 0.817 |
| Item | Factorial Weight | |
|---|---|---|
| Factor 1: Higher-order executive function. | ||
| The child begins his activities of daily living in a reasonable time from the adult’s direction. | 0.517 | |
| The child can perform his activities of daily living without the help of an adult. | 0.554 | |
| The child persists in their activities of daily living although he finds difficulties. | 0.306 | |
| The child finishes his activities of daily living at an appropriate time. | 0.521 | |
| The child becomes aware of the mistakes he makes in his activities. | 0.559 | |
| The child tries to solve problems while performing an activity. | 0.732 | |
| The child performs his daily activities without unnecessary stops. | 0.642 | |
| The child performs his daily activities in a logical order. | 0.649 | |
| Factor 2: Core executive function. | ||
| The child gets frustrated quickly when cannot perform an activity. | 0.428 | |
| The child has more tantrums than expected for his age. | 0.459 | |
| The child has difficulties to get adapted to changes in the environment. | 0.533 | |
| The child has difficulties to adapt changes in his routine. | 0.622 | |
| The child has difficulties moving from one activity to move on to another. | 0.506 | |
| The child often leaves his activities of daily living unfinished. | 0.344 | |
| The child loses his attention performing his activities if there is some noise. | 0.555 | |
| The child spins or rocks excessively, making it difficult to do his activities. | 0.654 | |
| The child does not perform his activities properly due to excessive movement. | 0.546 | |
| Eating Scale | Personal Hygiene Scale | Dressing Scale | Daily Functioning | |||||
|---|---|---|---|---|---|---|---|---|
| Oral Sensitivity | Good Manners | Manual Dexterity | Brushing Teeth | Toilet Management | Hygiene | Dressing | Higher-Order EF | |
| Good Manners | −0.07 | |||||||
| Manual Dexterity | −0.00 | 0.18 ** | ||||||
| Brushing teeth | −0.03 | 0.28 ** | 0.40 ** | |||||
| Toilet management | −0.01 | 0.23 ** | 0.30 ** | 0.42 ** | ||||
| General hygiene | −0.01 | 0.39 ** | 0.46 ** | 0.48 ** | 0.49 ** | |||
| Dressing | −0.04 | 0.30 ** | 0.50 ** | 0.42 ** | 0.43 ** | 0.63 ** | ||
| Higher-order EF | −0.02 | 0.49 ** | 0.32 ** | 0.39 ** | 0.35 ** | 0.44 ** | 0.47 ** | |
| Core EF | −0.14 * | 0.25 ** | −0.05 ** | 0.06 | 0.09 ** | 0.05 | 0.07 | 0.19 ** |
| Indices | Cut-off | Eating Scale | Personal Hygiene Scale | Dressing Scale | Daily Functioning Scale |
|---|---|---|---|---|---|
| Chi-squared probability p (χ2) | >0.05 | 0.000 | 0.000 | 0.000 | 0.009 |
| CFI | >0.90 | 0.982 | 0.982 | 0.987 | 0.975 |
| NNFI | >0.90 | 0.972 | 0.986 | 0.988 | 0.981 |
| RMSEA | <0.06 | 0.039 | 0.039 | 0.050 | 0.034 |
| RMSR | <0.08 | 0.060 | 0.073 | 0.083 | 0.069 |
| Eating Scale | Personal Hygiene Scale | Dressing Scale | Daily Functioning Scale | |||||
|---|---|---|---|---|---|---|---|---|
| Manual Dexterity Factor | Good Manners Factor | Oral Sensitivity Factor | Toilet Management Factor | Brushing Factor | Grooming Factor | Dressing | Higher-Order EF Factor | Core EF Factor |
| 0.81 | 0.74 | 0.76 | 0.80 | 0.82 | 0.88 | 0.94 | 0.78 | 0.76 |
| Eating Scale | Personal Hygiene Scale | Dressing Scale | Daily Functioning Scale | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex | Oral Sensitivity | Good Manners | Manual Dexterity | Brushing | Toilet Management | General Hygiene | Dressing | Higher-Order EF Factor | Core EF Factor |
| Boys | 5.3 ± 1.4 | 17.7 ± 2.1 | 10.6 ± 3.1 | 13.6 ± 2.6 | 24.3 ± 2.2 | 35.1 ± 6.0 | 50.9 ± 7.8 | 19.4 ± 2.7 | 12.5 ± 3.2 |
| Girls | 5.5 ± 1.3 | 17.9 ± 2.1 | 10.5 ± 3.5 | 13.7 ± 2.7 | 24.9 ± 2.5 | 35.7 ± 6.0 | 52.1 ± 6.9 | 19.7 ± 2.5 | 13.7 ± 3.0 |
| t | −1.21 | −0.48 | 0.30 | −0.14 | −2.04 | −0.82 | −1.51 | −0.83 | −3.40 |
| p | 0.22 | 0.62 | 0.76 | 0.88 | 0.04 * | 0.41 | 0.131 | 0.40 | 0.001 ** |
| d | 0.19 | 0.12 | 0.11 | 0.04 | 0.56 | 0.57 | 1.29 | 0.25 | 1.22 |
| Eating Scale | Personal Hygiene Scale | Dressing Scale | Daily Functioning Scale | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Years | Oral Sensitivity | Good Manners | Manual Dexterity | Brushing | Toilet Management | General Hygiene | Dressing | Higher-OrderEF Factor | Core EF Factor |
| 3–4 | 5.4 ± 1.2 | 17.3 ± 2.2 | 9.0 ± 2.9 | 12.6 ± 2.8 | 23.9 ± 3.1 | 32.9 ± 6.4 | 46.9 ± 7.3 | 18.7 ± 2.2 | 12.7 ± 2.9 |
| 5–6 | 5.4 ± 1.4 | 18.1 ± 2.0 | 11.6 ± 3.1 | 14.3 ± 2.3 | 25.0 ± 1.7 | 37.1 ± 5.1 | 54.5 ± 5.7 | 20.1 ± 2.7 | 13.3 ± 3.3 |
| t | −0.01 | −3.1 | −7.0 | −5.4 | −3.8 | −6.2 | −10.1 | −4.5 | −1.5 |
| p | 0.992 | 0.002 ** | 0.000 ** | 0.000 ** | 0.000 ** | 0.000 ** | 0.000 ** | 0.000 ** | 0.111 |
| d | 0.00 | 0.77 | 2.56 | 1.72 | 1.08 | 4.21 | 7.67 | 1.33 | 0.59 |
| Scales | Typical | ASD | AUC (CI 95%) | p | d |
|---|---|---|---|---|---|
| Eating | 33.9 ± 4.4 | 29.1 ± 5.6 | 0.74 (0.57–0.91) | 0.005 | 0.936 |
| Hygiene | 73.8 ± 9.2 | 51.6 ± 11 | 0.95 (0.91–0.98) | 0.000 | 2.327 |
| Dressing | 51.5 ± 7.4 | 39 ± 10.1 | 0.84 (0.71–0.96) | 0.000 | 1.406 |
| General | 32.7 ± 0.4.5 | 25.7 ± 4.6 | 0.87 (0.81–0.93) | 0.000 | 1.613 |
| Total | 192 ± 20.3 | 145.5 ± 25.6 | 0.93 (0.87–0.98) | 0.000 | 2.088 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrios-Fernandez, S.; Gozalo, M.; Garcia-Gomez, A.; Carlos-Vivas, J.; Romero-Ayuso, D. A Novel Tool to Assess Basic Activities of Daily Living in Spanish Preschoolers. Children 2021, 8, 496. https://doi.org/10.3390/children8060496
Barrios-Fernandez S, Gozalo M, Garcia-Gomez A, Carlos-Vivas J, Romero-Ayuso D. A Novel Tool to Assess Basic Activities of Daily Living in Spanish Preschoolers. Children. 2021; 8(6):496. https://doi.org/10.3390/children8060496
Chicago/Turabian StyleBarrios-Fernandez, Sabina, Margarita Gozalo, Andres Garcia-Gomez, Jorge Carlos-Vivas, and Dulce Romero-Ayuso. 2021. "A Novel Tool to Assess Basic Activities of Daily Living in Spanish Preschoolers" Children 8, no. 6: 496. https://doi.org/10.3390/children8060496
APA StyleBarrios-Fernandez, S., Gozalo, M., Garcia-Gomez, A., Carlos-Vivas, J., & Romero-Ayuso, D. (2021). A Novel Tool to Assess Basic Activities of Daily Living in Spanish Preschoolers. Children, 8(6), 496. https://doi.org/10.3390/children8060496











