SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports
Abstract
1. Introduction
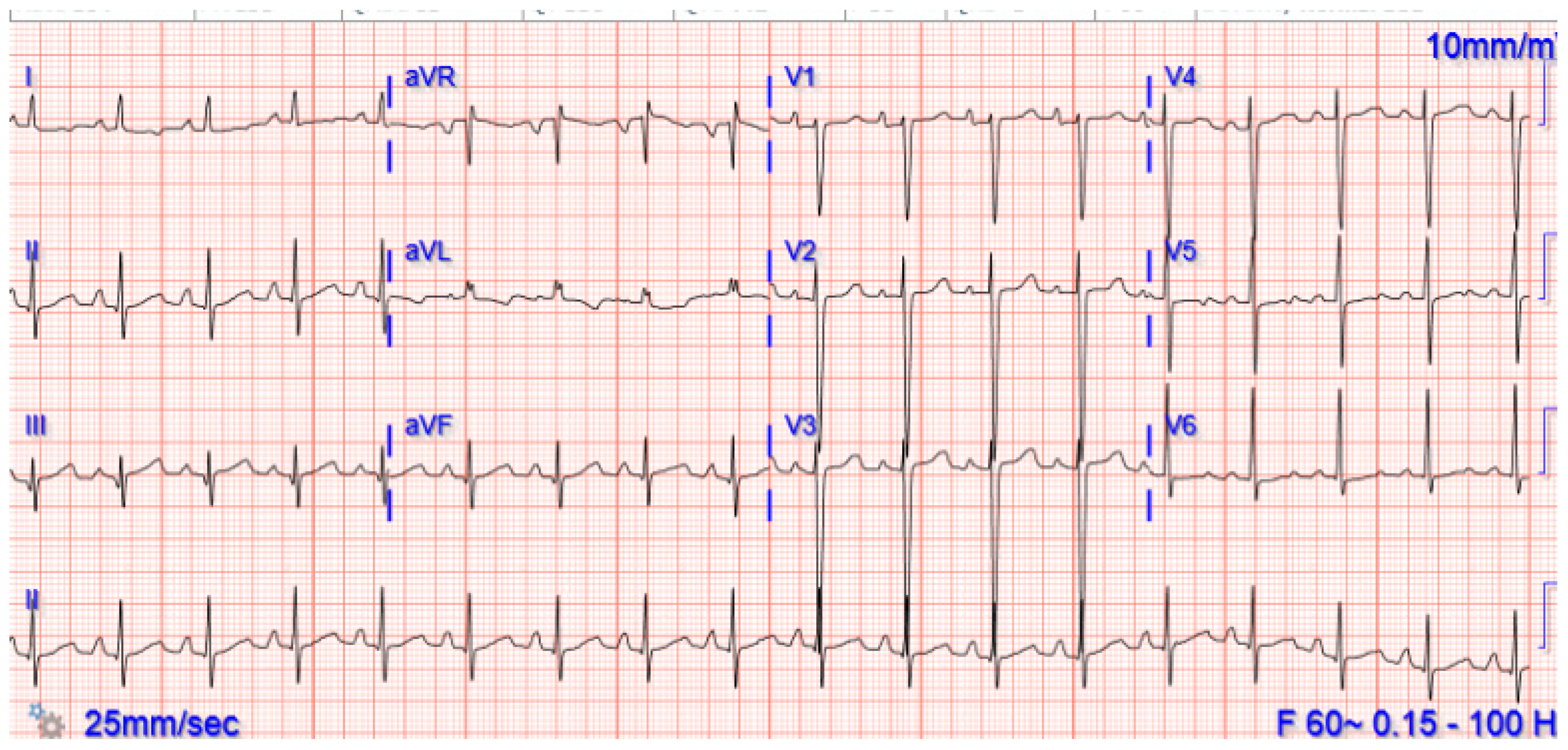
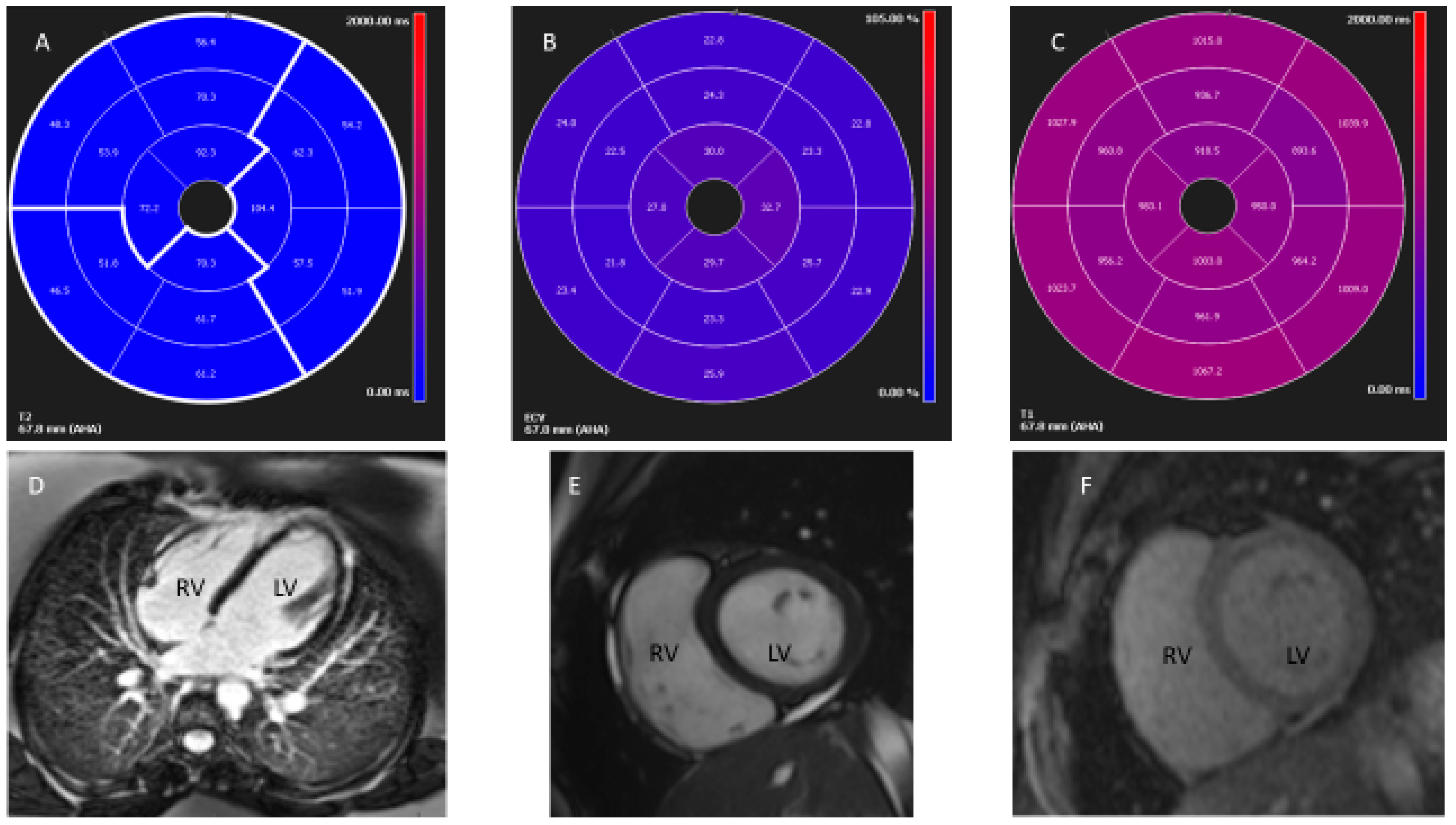
2. Case Presentation
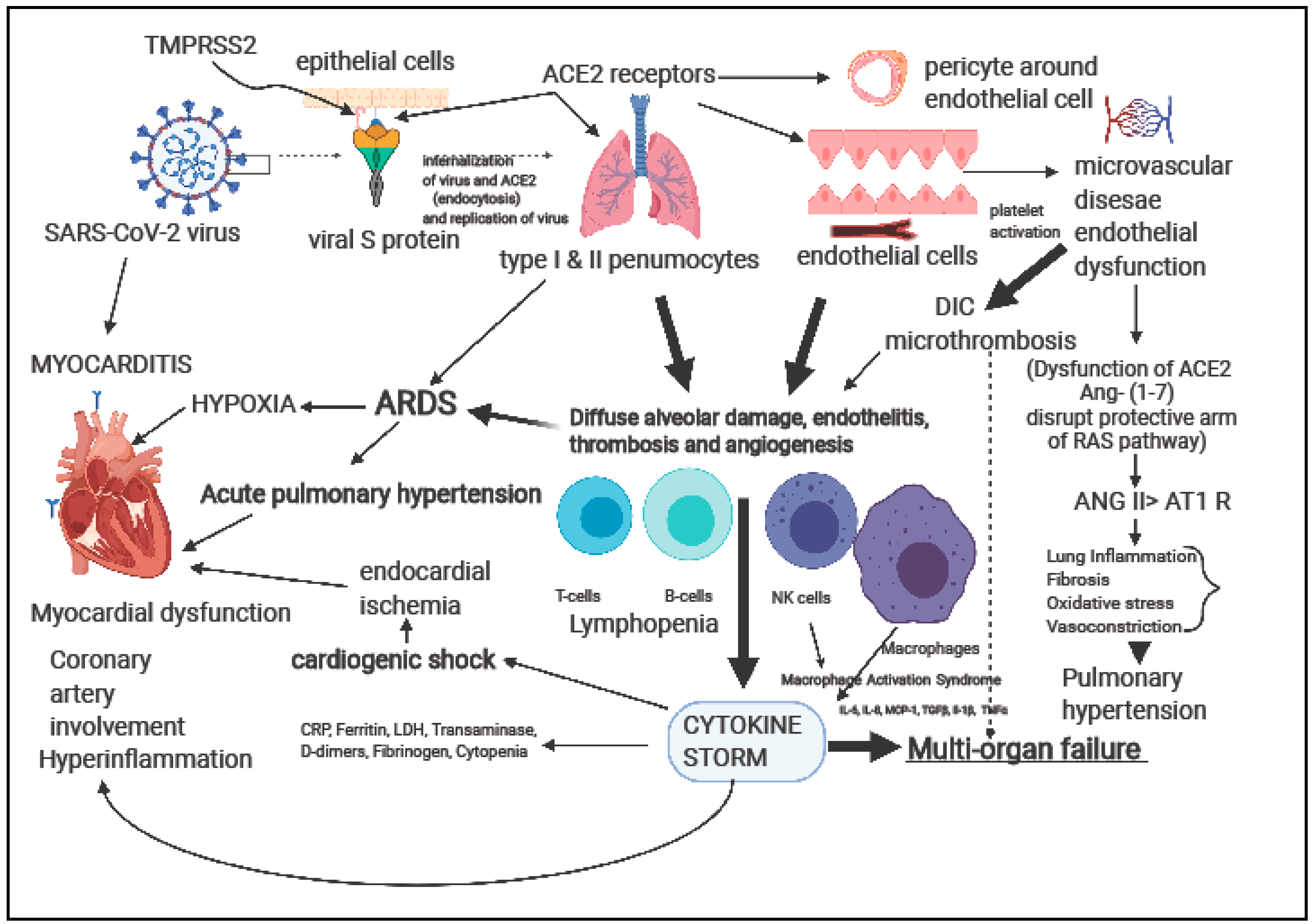
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Financial Disclosure
References
- Das, B.B.; Tejtel, S.K.S.; Deshpande, S.; Shekerdemian, L.S. Cardiac presentation of coronavirus disease 2019 (COVID-19) in adults and children. Tex. Heart Inst. J. 2021, 48, e20-7395. [Google Scholar]
- Clark, D.E.; Parikh, A.; Dendy, J.M.; Diamond, A.B.; George-Durett, K.; Fish, F.A.; Soslow, J.H. COVID-19 myocardial pathology evaluation in athletes with cardiac magnetic resonance (COMPETE CMR). Circulation 2021, 143, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in myocarditis: A JACC White Paper. JACC 2009, 53, 1475–1487. [Google Scholar]
- Jeserich, M.; Föll, D.; Olschewski, M.; Kimmel, S.; Friedrich, M.G.; Bode, C.; Geibel, A. Evidence of myocardial edema in patients with nonischemic dilated cardiomyopathy. Clin. Cardiol. 2012, 35, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Jeserich, M.; Konstantinides, S.; Olschewski, M.; Pavlik, G.; Bode, C.; Geibel, A. Diagnosis of early myocarditis after respiratory or gastrointestinal tract viral infection: Insights from cardiovascular magnetic resonance. Clin. Res. Cardiol. 2010, 99, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.M.; Barkhausen, J.; Bucciarelli-Ducci, C.; Flamm, S.D.; Kim, R.J.; Nagel, E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 Update. J. Cardiovasc. Magn. Reson. 2020, 22, 17. [Google Scholar] [CrossRef]
- Radunski, U.K.; Lund, G.K.; Sharing, D.; Bohnen, S.; Stehning, S.; Schnackenburg, B.; Avanesov, M.; Tahir, E.; Adam, G.; Blankenberg, S.; et al. T1, and T2 mapping cardiovascular resonance imaging technique reveal unapparent myocardial injury in patients with myocarditis. Clin Res. Cardiol. 2017, 106, 10–17. [Google Scholar] [CrossRef]
- Bohnen, S.; Radunski, U.K.; Lund, G.K.; Kandolf, R.; Stehning, C.; Schnackenburg, B.; Adam, G.; Blankenberg, S.; Muellerleile, K. Performance of T1 and T2 Mapping Cardiovascular Magnetic Resonance to Detect Active Myocarditis in Patients With Recent-Onset Heart Failure. Circ. Cardiovasc. Imaging 2015, 8, e003073. [Google Scholar] [CrossRef]
- Friedrich, M.G. Why Edema is a matter of the heart. Circ. Cardiovasc. Imaging 2017, 10, e006062. [Google Scholar] [CrossRef]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID19 and cardiovascular disease: From basic mechanism to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef]
- Esposito, A.; Palmisano, A.; Natale, L.; Ligabue, G.; Peretto, G.; Lovato, L.; Vignale, D.; Fiocchi, F.; Marano, R.; Russo, V. Cardiac magnetic resonance characterization of myocarditis-like acute cardiac syndrome in COVID-19. JACC Cardiovasc. Imaging 2020, 13, 2457–2479. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Andreas, M.; et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Karamitsos, T.D.; Arvanitaki, A.; Karvounis, H.; Neubauer, S.; Ferreira, V.M. Myocardial tissue characterization and fibrosis by imaging. JACC Cardiovasc. Imaging 2020, 13, 1221–1234. [Google Scholar]
- The European Society of Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. Available online: https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance (accessed on 22 April 2021).
- Tavazzi, G.; Pellegrini, C.; Marreli, M.; Belliato, M.; Sciutti, F.; Bottazzi, A.; Sepe, P.A.; Resasco, T.; Camporotondo, R.; Bruno, R. Myocardial localization of Coronavirus in COVID-19 cardiogenic shock. Eur. J. Heart Fail. 2020, 22, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Lindner, D.; Fitzek, A.; Brauninger, H.; Aleschcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.; et al. Association of cardiac infection with SARS-CoV-2 confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020, 5, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhao, P.; Tang, D.; Zhu, T.; Han, R.; Chan, C.; Liu, W.; Zeng, H.; Tao, Q.; Xia, L. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc. Imaging 2020, 13, 2330–2339. [Google Scholar] [CrossRef]
- Starekova, J.; Bluemke, D.A.; Bradham, W.S.; Bradham, W.S.; Eckhardt, L.L.; Brist, T.M.; Kusmirek, J.E.; Purtell, C.S.; Schiebler, M.L.; Reeder, S.B. Evaluation of myocarditis in competitive student-athletes recovering from coronavirus disease 2019 with cardiac magnetic resonance imaging. JAMA Cardiol. 2021, e207444. [Google Scholar] [CrossRef]
- Malek, L.A.; Narczak, M.; Milosz-Wieczorek, B.; Konopka, M.; Braksator, W.; Drygas, W.; Krzywański, J. Cardiac involvement in consecutive elite athletes recovered from COVID-19: A magnetic resonance study. J. Magn. Reson. Imaging 2021. [Google Scholar] [CrossRef]
- Maron, B.J.; Udelson, J.E.; Bonow, R.O.; Nishimura, R.A.; Ackerman, M.J.; Estes, N.M., III. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 3, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, and other cardiomyopathies, and myocarditis: A scientific statement from the American Heart Association and American College of Cardiology. Circulation 2015, 132, e273–e280. [Google Scholar]
- Kim, J.H.; Levine, B.D.; Phelan, D.; Emery, M.S.; Martinenz, M.W.; Chung, E.H.; Thompson, P.D.; Baggish, A.L. Coronavirus Disease 2019 and athletic heart: Emerging perspectives on pathology, risks, and return to play. JAMA Cardiol. 2021, 6, 219–227. [Google Scholar] [CrossRef]
- Raukar, N.P.; Cooper, L.T. Implications of SARS-CoV-2-associated myocarditis in the medical evaluation of athletes. Sports Health 2021, 13, 145–148. [Google Scholar] [CrossRef] [PubMed]
- AAP Recommendations in “COVID-19 Interim Guidance: Return to Sports”. Available online: https://www.aappublications.org/news/2020/12/04/sportsguidance120420 (accessed on 30 January 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, B.B. SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports. Children 2021, 8, 427. https://doi.org/10.3390/children8060427
Das BB. SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports. Children. 2021; 8(6):427. https://doi.org/10.3390/children8060427
Chicago/Turabian StyleDas, Bibhuti B. 2021. "SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports" Children 8, no. 6: 427. https://doi.org/10.3390/children8060427
APA StyleDas, B. B. (2021). SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports. Children, 8(6), 427. https://doi.org/10.3390/children8060427






