Recommendations for a Pediatric Pain Education Curriculum for Physical and Occupational Therapists: Scoping Review and Survey
Abstract
:1. Introduction
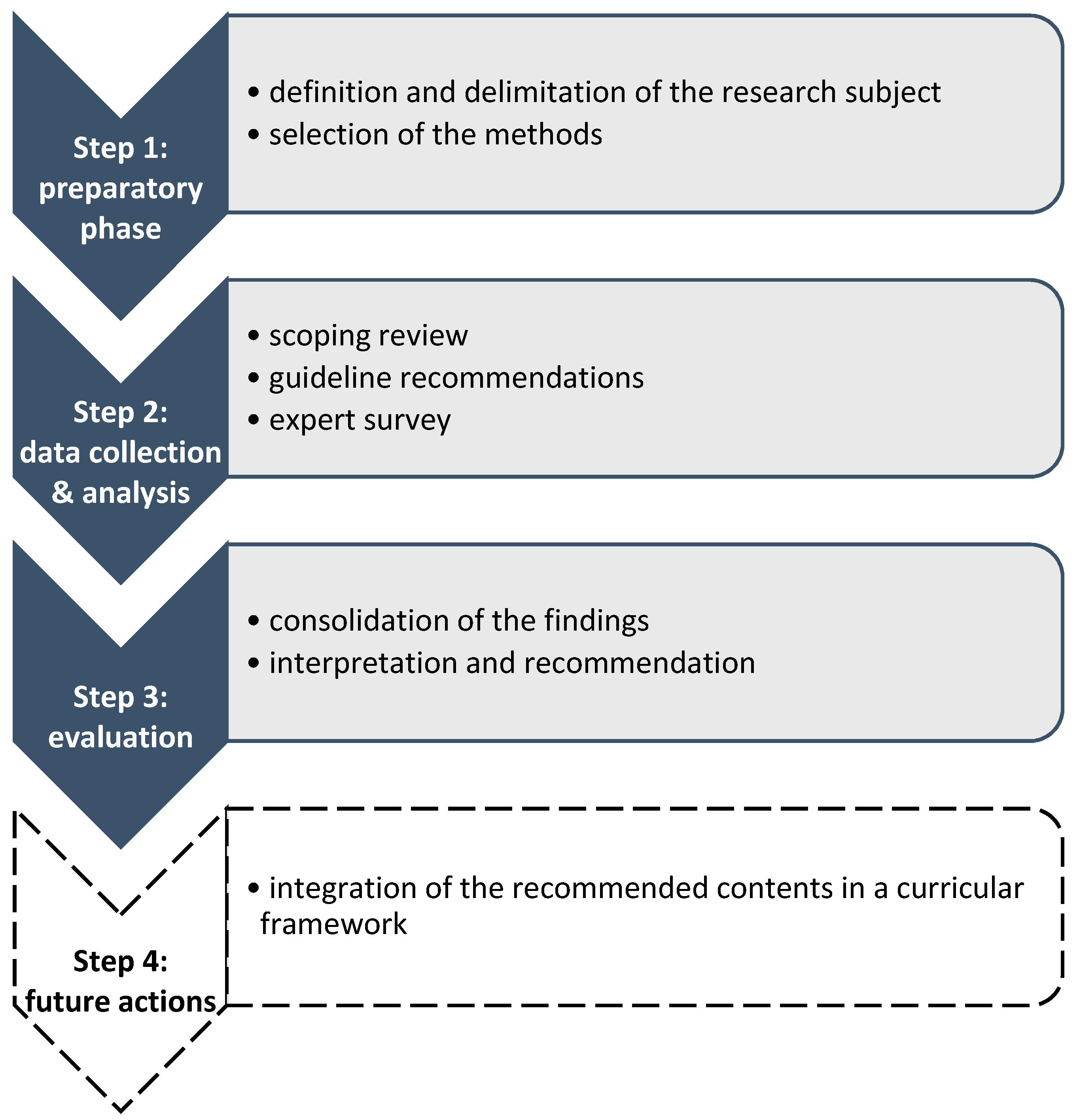
2. Materials and Methods
2.1. Theoretical Framework of the Study
2.2. Scoping Review
2.2.1. Search Strategy
2.2.2. Selection Criteria
2.2.3. Data Extraction and Critical Appraisal
2.3. Survey
2.3.1. Development of the Survey Instrument
2.3.2. Participating Experts
2.3.3. Analysis
3. Results
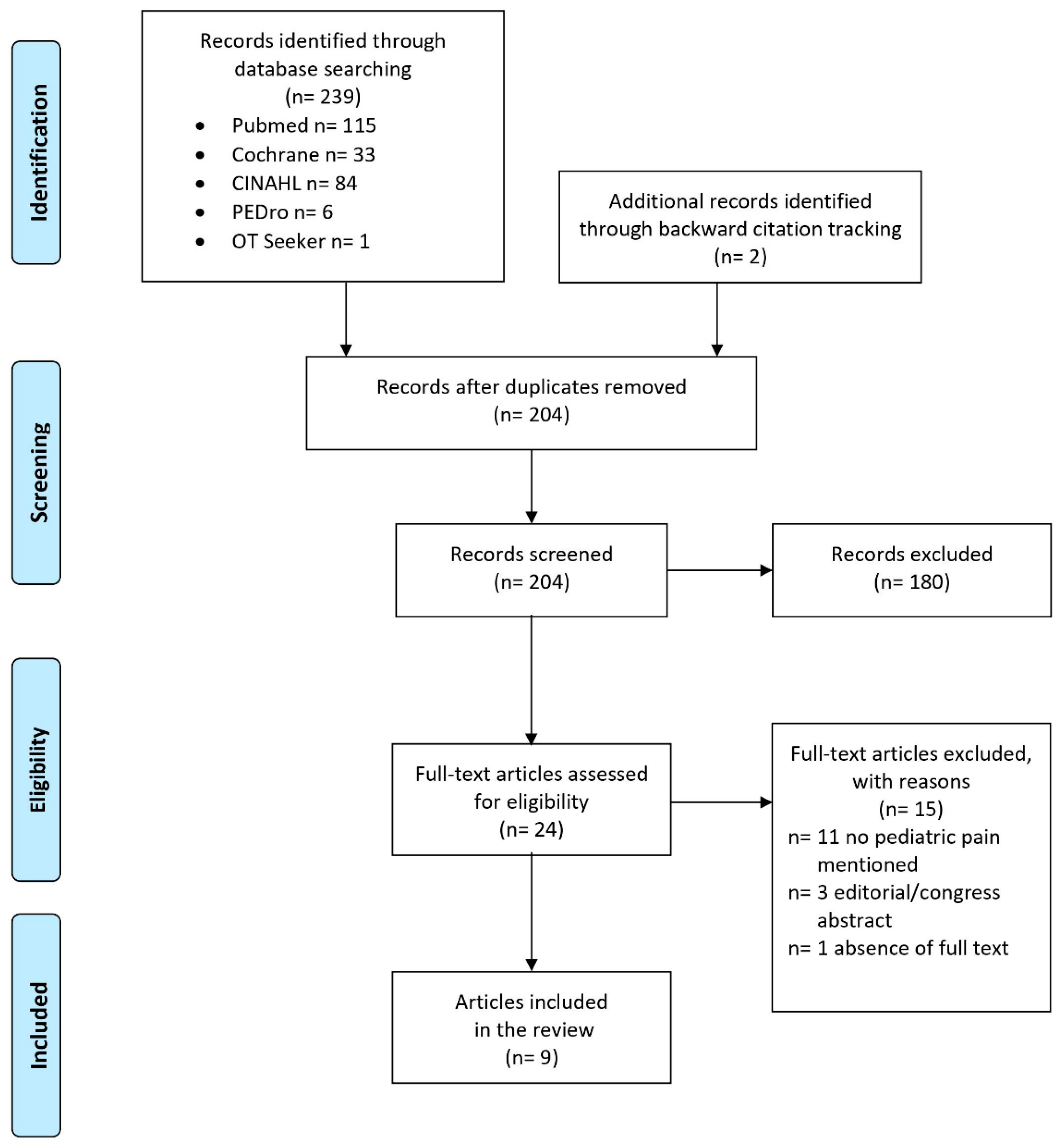
3.1. Results of the Scoping Review
3.1.1. Study Selection
3.1.2. Study Characteristics and Contents
3.1.3. Pediatric Pain Contents
3.1.4. Critical Appraisal of the Included Studies
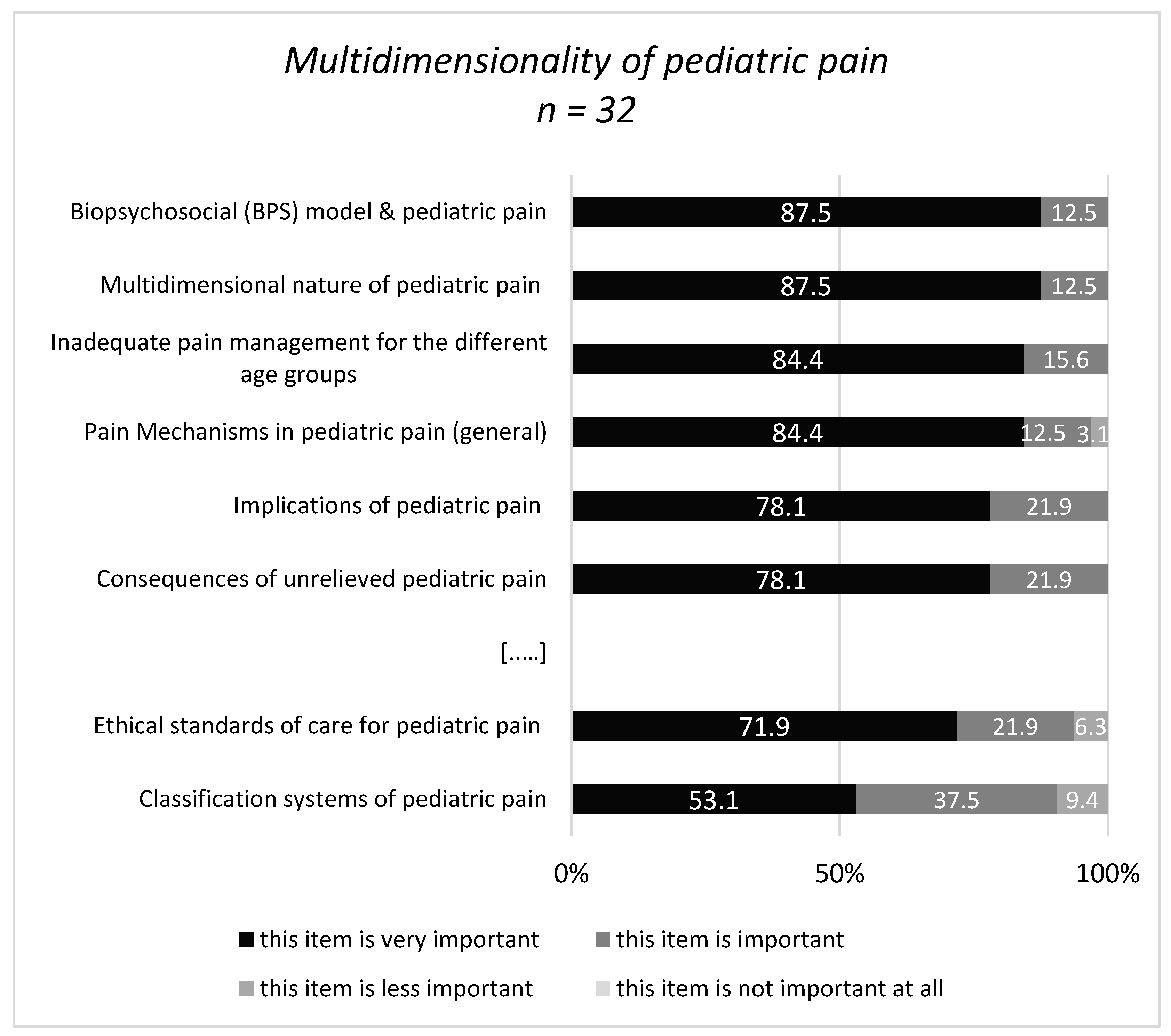
3.2. Results of the Survey
3.2.1. Sample Characteristics
3.2.2. Specialized Pain Management Courses
“Understanding the neuroscience behind chronic pain and learning different ways to speak of it to families and children using metaphors, stories, toys, etc. …”(#150; OT)
“… Difference in pain management in children vs adults”(#180; Medicine)
“… it is important to take into account how the child experiences pain, and whenever possible to ask them and let them “tell” what their day-to-day life is like, of course, without losing sight of the family’s opinion…”(#193; PT)
“…Considerations of language and it’s use, ways to simplify and enhance interventions to be understood by young people… The role of parents, attachment and family system functioning on pediatric pain…”(#352; OT)
“… empathy and feeling with the problems of acute and chronic pain in children …”(#248; Nursing)
“… Be able … to coach the child and her/his family in adopting valued life goals.”(#267; Psychology)
“… Affinity with this population, determination, enthusiasm and not careful in treating pediatric pain…”(#286; PT)
“It would be nice if there was specific training, not just for physical and occupational therapists, but for a whole multidisciplinary team...”(#248; Nursing)
“Ability to work in concert with a multi-disciplinary team including understanding how to communicate and maximize collaboration with physicians and psychologists.”(#133; PT)
“… Attachment and role of developmental trauma on development (including how this impacts threat detection) …”(#352; OT)
“… vulnerable populations (indigenous, remote and rural regions, co-morbid mental health, in justice systems; socially dislocated)”(#225; PT)
“…Yes—general developmental trajectories, underlying neurodevelopmental disorders and their interaction with persistent pain disorders, e.g., Autism …”(#352; OT)
“I think it’s also important to teach assessment using a conceptual framework like … interpretation of the ICF model…”(#133; PT)
“…Concept of Pain Inventory (COPI) for identifying and addressing specific conceptual ‘gaps’ and misconceptions…”(#347; PT)
“… too often the diagnosis is made too late and there is poor (too little) proper follow-up from the various disciplines...”(#248; Nursing)
“…Use of reward/reinforcement to increase adherence to treatment/exercise program…”(#222; Psychology)
“… Yes, occupational therapists should be able to tailor activity to be both developmentally sensitive and aligned with patient interests…”(#352; OT)
“...teach children to mobilize again and motivate them to move...”(#248; Nursing)
“We focus on self-management strategies and do not teach or promote aquatic therapy (unless the patient is a swimmer), TENS, heat, massage or ice.”(#133; PT)
“It is important to understand the complex presentations, particularly those which are associated with high levels of misinformation, distress or stigma in the community.”(#352; OT)
“Managing pain for children and adolescents with complex neurological impairment such as cerebral palsy or autism spectrum disorder.”(#157; OT)
“Setting—school context—how interventions can be delivered in this setting…”(#222; Psychology)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eccleston, C.; Fisher, E.; Howard, R.F.; Slater, R.; Forgeron, P.; Palermo, T.M.; Birnie, K.A.; Anderson, B.J.; Chambers, C.T.; Crombez, G.; et al. Delivering transformative action in paediatric pain: A Lancet Child & Adolescent Health Commission. Lancet Child Adolesc. Health 2021, 5, 47–87. [Google Scholar] [PubMed]
- Stevens, B.J.; Abbott, L.K.; Yamada, J.; Harrison, D.; Stinson, J.; Taddio, A.; Barwick, M.; Latimer, M.; Scott, S.D.; Rashotte, J.; et al. Epidemiology and management of painful procedures in children in Canadian hospitals. CMAJ Can. Med. Assoc. J. 2011, 183, E403–E410. [Google Scholar] [CrossRef] [Green Version]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Mathews, L. Pain in children: Neglected, unaddressed and mismanaged. Indian J. Palliat. Care 2011, 17, S70–S73. [Google Scholar] [CrossRef]
- Fitzgerald, M.; Walker, S.M. Infant pain management: A developmental neurobiological approach. Nat. Clin. Pract. Neurol. 2009, 5, 35–50. [Google Scholar] [CrossRef]
- Belavy, D.L.; van Oosterwijck, J.; Clarkson, M.; Dhondt, E.; Mundell, N.L.; Miller, C.T.; Owen, P.J. Pain sensitivity is reduced by exercise training: Evidence from a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 120, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, A.; Laekeman, M.; Egan Moog, M.; Dieterich, A.V. “On the move”—Prevention of chronic pain with physical activity and movement: [„On the Move“—Prävention chronischer Schmerzen durch körperliche Aktivität und Bewegung]. Schmerz 2021, 35, 14–20. [Google Scholar] [CrossRef]
- Caes, L.; Fisher, E.; Clinch, J.; Eccleston, C. Current Evidence-Based Interdisciplinary Treatment Options for Pediatric Musculoskeletal Pain. Curr. Treat. Options Rheumatol. 2018, 4, 223–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kichline, T.; Cushing, C.C. A systematic review and quantitative analysis on the impact of aerobic exercise on pain intensity in children with chronic pain. Child. Health Care 2019, 48, 244–261. [Google Scholar] [CrossRef]
- Nijhof, L.N.; Nap-van der Vlist, M.M.; van de Putte, E.M.; van Royen-Kerkhof, A.; Nijhof, S.L. Non-pharmacological options for managing chronic musculoskeletal pain in children with pediatric rheumatic disease: A systematic review. Rheumatol. Int. 2018, 38, 2015–2025. [Google Scholar] [CrossRef] [Green Version]
- Harrison, L.E.; Pate, J.W.; Richardson, P.A.; Ickmans, K.; Wicksell, R.K.; Simons, L.E. Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. J. Clin. Med. 2019, 8, 1267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stahlschmidt, L.; Zernikow, B.; Wager, J. Specialized Rehabilitation Programs for Children and Adolescents with Severe Disabling Chronic Pain: Indications, Treatment and Outcomes. Children 2016, 3, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hechler, T.; Kanstrup, M.; Holley, A.L.; Simons, L.E.; Wicksell, R.; Hirschfeld, G.; Zernikow, B. Systematic Review on Intensive Interdisciplinary Pain Treatment of Children With Chronic Pain. Pediatrics 2015, 136, 115–127. [Google Scholar] [CrossRef] [Green Version]
- Hurley-Wallace, A.; Wood, C.; Franck, L.S.; Howard, R.F.; Liossi, C. Paediatric pain education for health care professionals. Pain Rep. 2019, 4, e701. [Google Scholar] [CrossRef]
- Briggs, E.V.; Carr, E.C.J.; Whittaker, M.S. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur. J. Pain 2011, 15, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Leegaard, M.; Valeberg, B.T.; Haugstad, G.K.; Utne, I. Survey of Pain Curricula for Healthcare Professionals in Norway. Nord. J. Nurs. Res. 2014, 34, 42–45. [Google Scholar] [CrossRef] [Green Version]
- Reyes, A.N.; Brown, C.A. Occupational therapists’ pain knowledge: A national survey. Disabil. Rehabil. 2016, 38, 1309–1317. [Google Scholar] [CrossRef] [PubMed]
- Plomp, T. Educational Design Research: An Introduction. In Educational Design Research: Part A: An Introduction; Plomp, T., Nieveen, N., Eds.; The Netherlands Institute for Curriculum Development (SLO): Enschede, The Netherlands, 2013; pp. 10–51. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Equator Network. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. The EQUATOR Network (equator-network.org). Available online: https://www.equator-network.org/reporting-guidelines/prisma-scr/ (accessed on 11 December 2020).
- IASP. IASP Interprofessional Pain Curriculum Outline. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2057 (accessed on 8 January 2021).
- IASP. IASP Curriculum Outline on Pain for Physical Therapy. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2055 (accessed on 7 January 2021).
- IASP. IASP Curriculum Outline on Pain for Occupational Therapy. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=7069 (accessed on 7 January 2021).
- EFIC. European Pain Federation—Core Curriculum for the European Diplom in Pain Physiotherapy. Available online: https://europeanpainfederation.org/wp-content/uploads/2018/10/EFIC-Pain-Physiotherapy-Curriculum1.pdf (accessed on 7 January 2021).
- NVK; Nederlandse Vereniging voor Kindergeneeskunde. Somatisch Onvoldoende Verklaarde Lichamelijke Klachten (SOLK) Bij kinderen (Somatically Unexplained Physical Complaints): Richtlijn. Available online: https://www.nvk.nl/themas/kwaliteit/richtlijnen/richtlijn?componentid=6488085&tagtitles=Maag-Darm-Leverziekten%2B(MDL),Neonatologie,Sociale%2Ben%2BPsychosociale%2Bkindergeneeskunde (accessed on 7 January 2021).
- The Scottish Government. Management of Chronic Pain in Children and Young People: A National Clinical Guideline; The Scottish Government: Edinburgh, UK, 2018. [Google Scholar]
- Draheim, N.; Ebinger, F.; Schnöbel-Müller, E.; Wolf, B.; Häuser, W. Definition, diagnostics and therapy of chronic widespread pain and the (so-called) fibromyalgia syndrome in children and adolescents [Definition, Diagnostik und Therapie von chronischen Schmerzen in mehreren Körperregionen und des (sog.) Fibromyalgiesyndroms bei Kindern und Jugendlichen: Aktualisierte Leitlinie 2017]. Schmerz 2017, 31, 296–307. [Google Scholar] [PubMed]
- Williams, G.; Howard, R.F.; Liossi, C. Persistent postsurgical pain in children and young people: Prediction, prevention, and management. Pain Rep. 2017, 2, e616. [Google Scholar] [CrossRef]
- González-María, E.; Fuentelsaz-Gallego, C.; Moreno-Casbas, T.; Gil-Rubio, P.; Herreros-López, P.; on behalf of the work group of the Clinical Practice Guideline for Pain Management in Children With Cancer. Clinical Practice Guideline for Pain Management in Children with Cancer. Available online: http://www.criscancer.org (accessed on 8 January 2021).
- World Health Organization. Guidelines on the Management of Chronic Pain in Children; World Health Organization: Geneva, Switzerland; Available online: https://apps.who.int/iris/handle/10665/337999 (accessed on 7 January 2021).
- Leiner, D.J. SoSci Survey. Available online: https://www.soscisurvey.de (accessed on 15 March 2021).
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken, 12th ed.; Beltz: Weinheim, Germany, 2015. [Google Scholar]
- Hoeger Bement, M.K.; Sluka, K.A. The current state of physical therapy pain curricula in the United States: A faculty survey. J. Pain 2015, 16, 144–152. [Google Scholar] [CrossRef] [Green Version]
- Rochman, D.L.; Sheehan, M.J.; Kulich, R.J. Evaluation of a pain curriculum for occupational therapists: Experiences from a master’s-level graduate program over six years. Disabil. Rehabil. 2013, 35, 1933–1940. [Google Scholar] [CrossRef]
- Hoeger Bement, M.K.; St Marie, B.J.; Nordstrom, T.M.; Christensen, N.; Mongoven, J.M.; Koebner, I.J.; Fishman, S.M.; Sluka, K.A. An interprofessional consensus of core competencies for prelicensure education in pain management: Curriculum application for physical therapy. Phys. Ther. 2014, 94, 451–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scudds, R.J.; Scudds, R.A.; Simmonds, M.J. Pain in the physical therapy (pt) curriculum: A faculty survey. Physiother. Theory Pract. 2001, 17, 239–256. [Google Scholar] [CrossRef]
- Hunter, J.; Watt-Watson, J.; McGillion, M.; Raman-Wilms, L.; Cockburn, L.; Lax, L.; Stinson, J.; Cameron, A.; Dao, T.; Pennefather, P.; et al. An interfaculty pain curriculum: Lessons learned from six years experience. Pain 2008, 140, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Wideman, T.H.; Miller, J.; Bostick, G.; Thomas, A.; Bussières, A.; Wickens, R.H. The current state of pain education within Canadian physiotherapy programs: A national survey of pain educators. Disabil. Rehabil. 2020, 42, 1332–1338. [Google Scholar] [CrossRef] [PubMed]
- Hush, J.M.; Nicholas, M.; Dean, C.M. Embedding the IASP pain curriculum into a 3-year pre-licensure physical therapy program: Redesigning pain education for future clinicians. Pain Rep. 2018, 3, e645. [Google Scholar] [CrossRef] [PubMed]
- Miró, J.; Castarlenas, E.; Solé, E.; Martí, L.; Salvat, I.; Reinoso-Barbero, F. Pain curricula across healthcare professions undergraduate degrees: A cross-sectional study in Catalonia, Spain. BMC Med. Educ. 2019, 19, 307. [Google Scholar] [CrossRef] [Green Version]
- van Lankveld, W.; Afram, B.; Staal, J.B.; van der Sande, R. The IASP pain curriculum for undergraduate allied health professionals: Educators defining competence level using Dublin descriptors. BMC Med. Educ. 2020, 20, 60. [Google Scholar] [CrossRef] [Green Version]
- Center for Evidence-Based Management (CEBMa). What Is Critical Appraisal?—Center for Evidence Based Management. Available online: https://cebma.org/resources-and-tools/what-is-critical-appraisal/ (accessed on 28 April 2021).
- Artino, A.R.; Durning, S.J.; Sklar, D.P. Guidelines for Reporting Survey-Based Research Submitted to Academic Medicine. Acad. Med. J. Assoc. Am. Med. Coll. 2018, 93, 337–340. [Google Scholar] [CrossRef]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [Green Version]
- Watt-Watson, J.; Hogans, B.; Carr, E.; Gordon, D. IASP FACT SHEET No. 3 Pain Curriculum Design Models and Implementation Approaches. Available online: https://sbed.org.br/wp-content/uploads/2019/02/factsheet3paincurriculumdesignmodelsenglish2.pdf (accessed on 22 March 2021).
- SickKids. Online Paediatric Pain Curriculum. Available online: https://www.sickkids.ca/en/care-services/centres/pain-centre/#oppc (accessed on 28 March 2021).
- ChildKind. Pediatric Pain (PRN) Curriculum. Available online: https://childkindinternational.org/resources/pediatric-pain-prn-curriculum/ (accessed on 28 March 2021).
- Odell, S.; Logan, D.E. Pediatric pain management: The multidisciplinary approach. J. Pain Res. 2013, 6, 785–790. [Google Scholar] [CrossRef] [Green Version]
- Genik, L.M.; McMurtry, C.M.; Marshall, S.; Rapoport, A.; Stinson, J. Massage therapy for symptom reduction and improved quality of life in children with cancer in palliative care: A pilot study. Complement. Ther. Med. 2020, 48, 102263. [Google Scholar] [CrossRef]
- Radossi, A.L.; Taromina, K.; Marjerrison, S.; Diorio, C.J.; Similio, R.; Njuguna, F.; Afungchwi, G.M.; Ladas, E.J. A systematic review of integrative clinical trials for supportive care in pediatric oncology: A report from the International Society of Pediatric Oncology, T&CM collaborative. Support. Care Cancer 2018, 26, 375–391. [Google Scholar] [PubMed]
- Johnston, C.; Campbell-Yeo, M.; Disher, T.; Benoit, B.; Fernandes, A.; Streiner, D.; Inglis, D.; Zee, R. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst. Rev. 2017, 2, CD008435. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; McGrath, T.; Drendel, A.L. An Evidence-Based Approach to Minimizing Acute Procedural Pain in the Emergency Department and Beyond. Pediatr. Emerg. Care 2016, 32, 36–42. [Google Scholar] [CrossRef] [Green Version]
- Thrane, S.E.; Wanless, S.; Cohen, S.M.; Danford, C.A. The Assessment and Non-Pharmacologic Treatment of Procedural Pain From Infancy to School Age Through a Developmental Lens: A Synthesis of Evidence With Recommendations. J. Pediatr. Nurs. 2016, 31, e23–e32. [Google Scholar] [CrossRef] [Green Version]
- Krauss, B.S.; Calligaris, L.; Green, S.M.; Barbi, E. Current concepts in management of pain in children in the emergency department. Lancet 2016, 387, 83–92. [Google Scholar] [CrossRef]
- van Meulenbroek, T.; Huijnen, I.P.J.; Simons, L.E.; Conijn, A.E.A.; Engelbert, R.H.H.; Verbunt, J.A. Exploring the underlying mechanism of pain-related disability in hypermobile adolescents with chronic musculoskeletal pain. Scand. J. Pain 2021, 21, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Elvén, M.; Dean, E.; Söderlund, A. Augmented behavioral medicine competencies in physical therapy students’ clinical reasoning with a targeted curriculum: A final-semester cohort-comparison study. Physiother. Theory Pract. 2021, 1–12. [Google Scholar] [CrossRef]
- Hurtubise, K.; Brousselle, A.; Noel, M.; Camden, C. What really matters in pediatric chronic pain rehabilitation? Results of a multi-stakeholder nominal group technique study. Disabil. Rehabil. 2020, 42, 1675–1686. [Google Scholar] [CrossRef] [PubMed]
- Finley, G.A.; MacLaren Chorney, J.; Campbell, L. Not small adults: The emerging role of pediatric pain services. Can. J. Anaesth. J. Can. D’Anesthesie 2014, 61, 180–187. [Google Scholar] [CrossRef]
- Koechlin, H.; Locher, C.; Prchal, A. Talking to Children and Families about Chronic Pain: The Importance of Pain Education-An Introduction for Pediatricians and Other Health Care Providers. Children 2020, 7, 179. [Google Scholar] [CrossRef]
- Emerson, N.D.; Bursch, B. Communicating with Youth about Pain: Developmental Considerations. Children 2020, 7, 184. [Google Scholar] [CrossRef] [PubMed]
- Deutsches Kinderschmerzzentrum (DKSZ). Understanding Pain—And What’s To Be Done About It in 10 Minutes: Den Schmerz Verstehen—Und Was zu Tun Ist in 10 Minuten! Available online: https://www.deutsches-kinderschmerzzentrum.de/ueber-uns/videos/den-schmerz-verstehen/ (accessed on 17 March 2021).
- Pain in Motion. A Journey to Learn about Pain. (English). Available online: www.paininmotion.be/storage/app/media/materials/oct-18/A%20JOURNEY%20TO%20LEARN%20ABOUT%20PAIN_FINAL.pdf (accessed on 17 March 2021).
- Pesquisa em Dor Kids. Uma Jornada para Entender a Dor. (Portugues/Luso-Brasileiro). Available online: http://pesquisaemdor.com.br/?page_id=84 (accessed on 27 March 2021).
- Deutsche Schmerzgesellschaft e.V. Eine Geschichte Über Den Schmerz: (German). Available online: https://www.schmerzgesellschaft.de/topnavi/die-gesellschaft/arbeitskreise/schmerz-und-bewegung/ziele-1 (accessed on 27 March 2021).
- PNE4KIDS Program (English; Dutch; Danish). Available online: http://www.paininmotion.be/pne4kids (accessed on 8 May 2021).
- Pas, R.; Meeus, M.; Malfliet, A.; Baert, I.; van Oosterwijck, S.; Leysen, L.; Nijs, J.; Ickmans, K. Development and feasibility testing of a Pain Neuroscience Education program for children with chronic pain: Treatment protocol. Braz. J. Phys. Ther. 2018, 22, 248–253. [Google Scholar] [CrossRef]
- Friedrichsdorf, S.J.; Goubert, L. Pediatric pain treatment and prevention for hospitalized children. Pain Rep. 2020, 5, e804. [Google Scholar] [CrossRef]
- Gai, N.; Naser, B.; Hanley, J.; Peliowski, A.; Hayes, J.; Aoyama, K. A practical guide to acute pain management in children. J. Anesth. 2020, 34, 421–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfingsten, M.; Arnold, B.; Böger, A.; Brinkschmidt, T.; Casser, H.-R.; Irnich, D.; Kaiser, U.; Klimczyk, K.; Lutz, J.; Schiltenwolf, M.; et al. Recommendations on structural and process parameters of the ad hoc commission “Interdisciplinary Multimodal Pain Therapy” of the German Pain Society (Deutsche Schmerzgesellschaft e. V.): [Sektorenübergreifende interdisziplinäre multimodale Schmerztherapie: Empfehlungen zu Struktur-und Prozessparametern der Ad-hoc-Kommission „Interdisziplinäre Multimodale Schmerztherapie“ der Deutschen Schmerzgesellschaft e. V.]. Schmerz 2019, 33, 191–203. [Google Scholar]
- Höfel, L.; Draheim, N.; Haas, J.-P.; Ebinger, F. Medical pain care for children and adolescents with chronic pain in Germany: An inventory: [Schmerzmedizinische Versorgung chronisch schmerzkranker Kinder und Jugendlicher in Deutschland: Eine Bestandsaufnahme]. Schmerz 2021, 35, 94–102. [Google Scholar] [CrossRef]
- Steketee, C.; Lee, A.; Moran, M.; Rogers, G. Towards a theoretical framework for curriculum development in health professional education. Focus Health Prof. Educ. 2013, 14, 64–77. [Google Scholar]
| Author | Aim | Country | Education Level | Accreditation | Evaluation years | Reference to IASP Pain Curricula | Discipline | Duration | Reference to Pediatric Pain Contents | Focus | Deficits Described | Survey/Interview Description & Poss. Response Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hoeger Bement & Sluka, 2015 [33] | To determine the extent of pain education in current Doctorate of PTschools. | USA | Doctoral level | Yes | 2012–2013 | IASP PTcurr. & 4 IASP Domains. | PT | Contact hours: mean 31 h ± 1.8 (SD) range: 5–115 h stand-alone course: n = 11 (6%). | Lowest coverage: assessment of pain across the life span (68%). | Basic science mechanisms/pain concepts/pain assessment & management/adequacy of pain curriculum. | Pain management in the young/46% were aware of the IASP curriculum. | Survey consisted of 10 questions/addressing directors or appropriate persons; n = 216 PT schools; response = 62% (n = 137). |
| Rochman et al. 2013 [34] | To test OT students’ pain knowledge and to determine specific topics to improve existing OT curricula. | USA | Master’s-level | --- | 2004–2009 | IASP OT/PT & inter-professional curr. | OT | 2 sessions of 2-h pain course embedded in a 13 weeks procedural clinical reasoning class & additional examples of clinical pain management in the course. | Correct answers: regarding children’s pain sensitivity & pain memory: 59.8% in pre- & 80.9% in post-test. | - Basics of pain management: misconceptions, myths, theories, taxonomy definitions, measurements, - OT & pain management: assessment methods/OTs role in pain team/case study. | Pain in special populations, e.g., children/ there is need for lecturers with special expertise in pain. | Survey of pain knowledge and attitudes prior to and following a pain course using the COBS adapted for OT & PT; n = 194 first-year OT students of n = 1 university response = 100%. |
| Hoeger Bement et al. 2014 [35] | To identify how core competencies for pain can be applied to the PT curriculum. | USA & Canada | Entry level | --- | --- | IASP PT & inter-professional curr. & 4 IASP Domains. | PT | Integration of competencies into a PT curriculum & additional stand-alone course on pain recommended. | Using specific pain assessments for special patient populations e.g., infants & improving pain management throughout the life span. | Description of PT core competencies for prelicensure education in pain management. | Innovative evidence based initiatives. | Based on expert consensus-derived pain management core competencies for health professional education. |
| Scudds et al. 2001 [36] | To determine the current status of pain topics in PT curricula. | North America & Canada | Master’s-level | Yes | 1997 | IASP OT & PT curr. | PT | Modal amount of time spent on pain = 4 h & 11/107 stand-alone courses. | 23.8% stated adequate time spent on pain in children. | Basic science mechanisms/pain assessment & management/time spent on pain topics. | Knowledge of curr. (21.9%); inadequate time for pain topics (43.3%) & pediatric pain inadequately covered (76.2%). | Survey of n = 169 PT programs using the Pain Survey Instrument/ target population = program directors or faculty members/ response rate = 63.3% (n = 107/169). |
| Hunter et al. 2008 [37] | To describe innovations based on comprehensive evaluations of outcomes of IPC implementation. | Canada (Toronto) | Undergraduate level | --- | 2002–2007 | IASP core & discipline-specific curr. | OT/PT & other disciplines. | Mandatory, stand-alone course = 20 h & 1 uni-professional discipline-specific session. | Optional: pain in children (1 h30) 1 case focus on childhood arthritic pain. | A flexible curriculum: choice of sessions/variety of patient cases/reduced didactic hours. | Students applied their learning in a surrogate clinical situation. | Survey among students, clinician-facilitators and faculty. Including the Daily Content and Process Questionnaire/Pain Knowledge & Beliefs Questionnaire & Comprehensive Plan Evaluation/n = 6 Health Science Faculties. |
| Wideman et al. 2020 [38] | To determine the current state of pain education across PT programs. | Canada | Master’s-level | Yes | 2016 | IASP PT curr.; 3 IASP Domains. | PT | Median 18 h (range 8–65 h) stand-alone course in 2 programs. | 28.6% addressed assessment & management of pediatric pain in sufficient depth. | % of items addressed in the programs: Domain1= 35.7%; Domain 2 = 50%; Domain 3 = 35.7% | Integration of curriculum themes: 38.6% full; 52.6% partial; 10.5% not. | Survey of all the national PT programs (=14), targeting 57 themes n = 16 pain educators. |
| Hush et al. 2018 [39] | To describe the embedding of the 2012 IASP PT curriculum into a PT program. | Australia | Doctoral level | --- | 2012–2017 | IASP PT curr. (2012) & 4 IASP Domains. | PT | Integrated in the PT curriculum. | Skills training emphasises the provision of … evidence-based health care across the lifespan. | 95 items of IASP curriculum successfully embedded/Special tools: six core concepts of pain & a clinical model of pain education. | Provision of training and resources to upskill teachers is critical. | Special tools developed with leading pain education specialists. Evaluation: students’ knowledge & skills: NPQ-R, APP tool, Mastery Checklist & clinical simulation exams; n = 1 PT program. |
| Miro et al. 2019 [40] | To describe the content of pain curricula in healthcare & veterinary education programs. | Spain: Catalonia | Undergraduate level | Yes | 2018 | IASP inter-professional curr. & 4 IASP Domains. | OT/PT & other disciplines. | 84% courses mandatory PT: M = 97 h (SD = 34; range = 34–129); OT: M= 13 h (SD = 9; range 7–20). | 4% embedded pediatric pain PT: n = 2 (2%) OT: n = 1 (6.7%) (n = number of responders). | Overview pain contents in 10 disciplines IASP curr contents: Domain 1= 17%; Domain 2= 21%; Domain 3= 10%; Domain 4= 14%. | Pain education not adequate & no interprofessional program. | Survey included 31 questions/addressing n = 1564 course leaders of n = 11 universities response n = 550 (35%). |
| van Lankveld et al. 2020 [41] | To describe needed competency levels for an interprofessional pain education core curriculum. | NL national & international panels | Undergraduate level | --- | 2016 | IASP inter-professional pain curr. (2012) 4 IASP Domains. | OT/PT & other disciplines. | Targeted is a stand-alone interprofessional pain education course. | Pediatric pain was excluded due to <70% agreement. | % of items selected for: Domain 1 = 66.6%; Domain 2 = 78%; Domain 3= 76%; Domain 4= 41%. | Exclusion of pain in infants although 79% of panel b rated inclusion. | 7 national (panel 1) & 15 international experts (panel 2) rated the curriculum items; inclusion of items with >70% agreement. |
| Authors | Hoeger Bement & Sluka, 2015 | Rochman et al. 2013 | Hoeger Bement et al. 2014 | Scudds et al. 2001 | Hunter et al. 2008 | Wideman et al. 2020 | Hush et al. 2018 | Miro et al. 2019 | van Lankveld et al. 2020 |
|---|---|---|---|---|---|---|---|---|---|
| Reference | [33] | [34] | [35] | [36] | [37] | [38] | [39] | [40] | [41] |
| Introduction | |||||||||
| 1. Were the aims/objectives of the study clear? | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Methods | |||||||||
| 2. Was the questionnaire clearly described or is the questionnaire available? | √ | √ | n/a | √ | √ | √ | n/a | √ | √ * |
| 3. Was the way of contacting the respondents described? | √ | √ | n/a | √ | √ | √ | n/a | √ | √ |
| 4. Was a pilot test conducted? | √ | n/a | n/a | √ | n/a | √ | n/a | √ | * |
| 5. Was there a description of the data analysis? | √ | √ | n/a | p | √ | √ | n/a | √ | √ |
| Results | |||||||||
| 6. Was there a description of the characteristics of the survey responders? | √ | p | n/a | p | √ | p | n/a | √ | √ |
| 7.Was the response rate depicted? | √ | √ | n/a | √ | √ | √ | n/a | √ | √ |
| 8. Were the results presented clearly and comprehensibly? | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Discussion | |||||||||
| 9. Were the authors’ discussions and conclusions justified by the results? | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 10. Were the limitations of the study discussed? | √ | p | n/a | √ | p | √ | n/a | √ | √ |
| 1. Multidimensional Nature of Pediatric Pain | Ratings (%) | Guidelines (%) |
| Epidemiology of pediatric pain | 53.1 | 100 |
| Theories of pediatric pain | ||
| ● Biopsychosocial model & pediatric pain | 87.5 * | 100 * |
| ● Definition of pediatric pain | 71.9 | 85.7 |
| ● Classification systems of pediatric pain | 53.1 | 71.4 |
| Pain mechanism in pediatric pain | ||
| ● The multidimensional nature of pediatric pain | 87.5 * | 100 * |
| ● Implications of pediatric pain | 78,1 | 71.4 |
| ● Consequences of unrelieved pediatric pain | 78.1 | 48.9 |
| Ethical principles & pediatric pain | ||
| ● Ethical standards of care for pediatric pain | 71.9 | 57.1 |
| ● Inadequate pain management for the different age groups: premature babies, neonates, infants, children & adolescents | 84.4 * | 85.7 * |
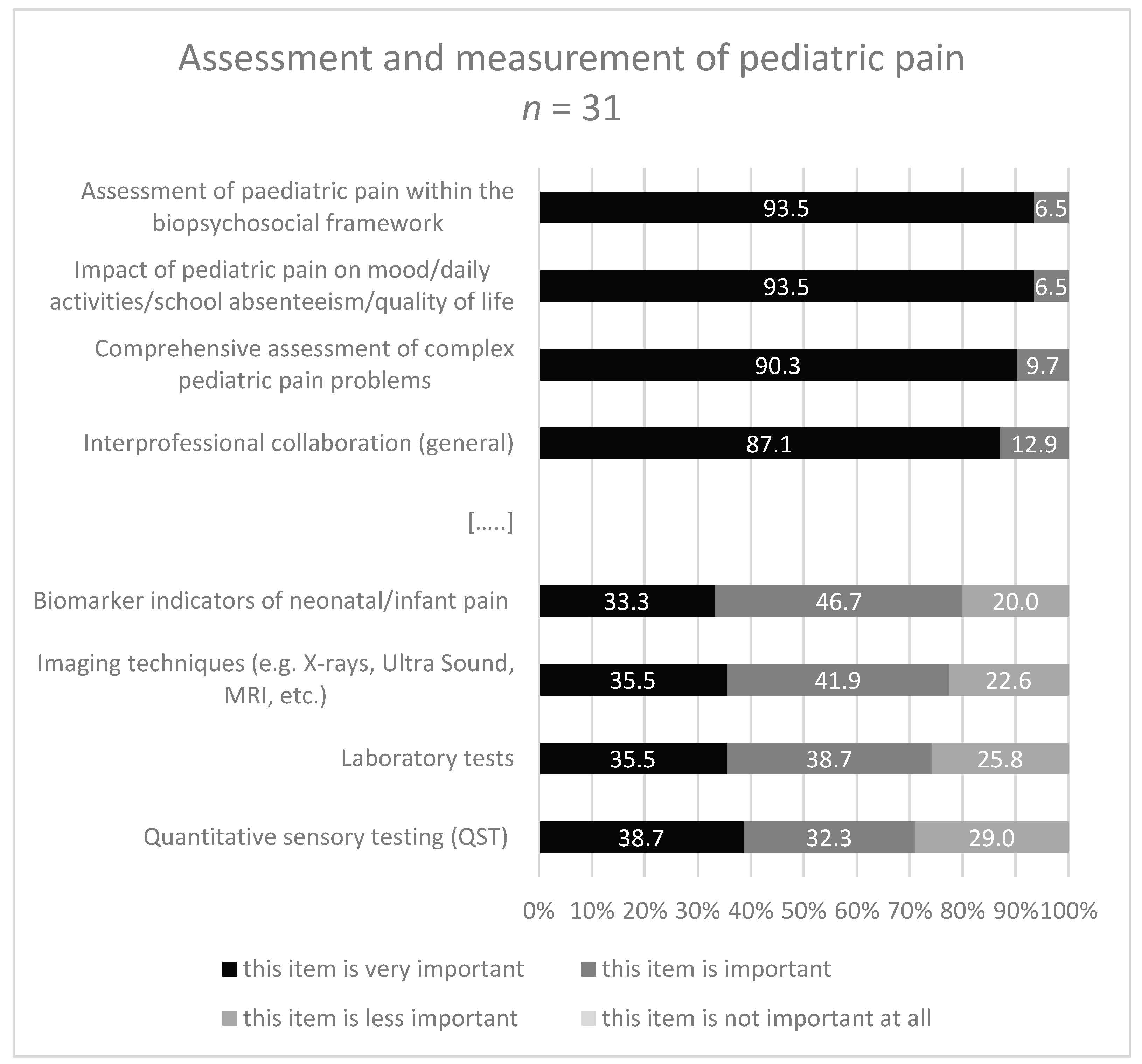
| 2. Assessment and measurement of pediatric pain | ||
| Assessment of pediatric pain within the biopsychosocial framework | 93.5 * | 100 * |
| Interprofessional collaboration | 87.1 | 100 |
| ● Comprehensive assessment of complex pediatric pain problems | 90.3 * | 100 * |
| ● Consideration of appropriate assessment and measurement methods for neonates, infants, children and adolescents including parents if necessary | 83.9 | 100 |
| History taking of pediatric pain | ||
| ● Pediatric pain location, grade of pain, contributing factors, etc. | 77.4 | 83.3 |
| ● Impact of pediatric pain on mood/daily activities/school absenteeism/quality of life | 93.5 * | 100 * |
| ● History of previous pediatric pain and treatment | 80.6 | 83.3 |
| ● Possible comorbidities influencing pediatric pain | 83.9 | 83.3 |
| ● Characteristics of the child/adolescent/familian occurrence of symptoms, environment | 80.6 | 100 |
| Physical examination of pediatric pain | 71.0 | 66.7 |
| Investigations: Laboratory test/Imaging techniques etc. | 35.5§ | 50.0§ |
| Use of child adapted standardized ools/questionnaires/assessment instruments | 70.9 | 100 |
| Use of parents adapted tools/questionnaires/assessment instruments | 77.4 | 66.7 |
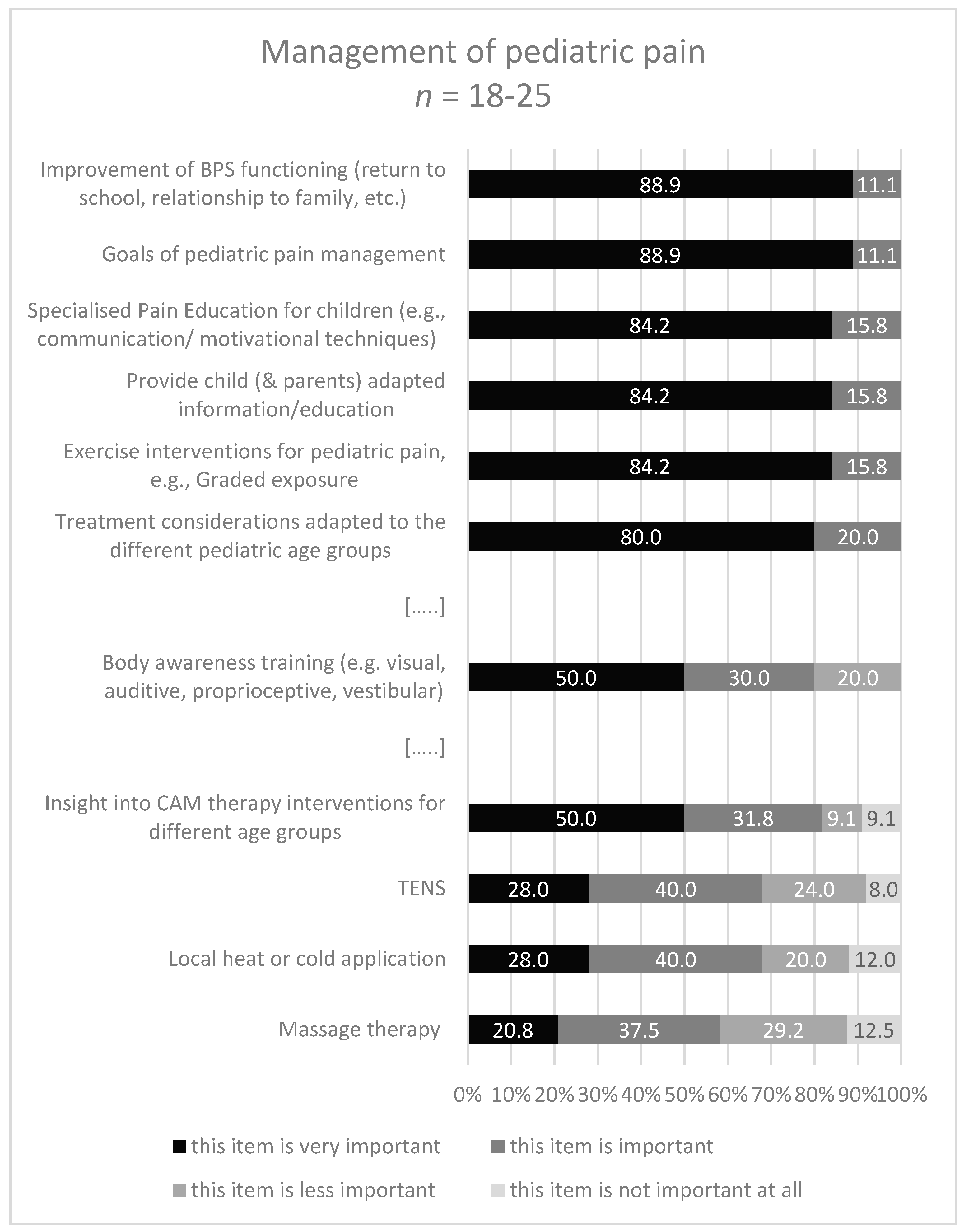
| 3. Management of pediatric pain | ||
| Goals of pediatric pain management: | 88.9 * | 100 * |
| ● Prevention and/or reduction of pediatric pain intensity | 57.9 | 100 |
| ● Improvement of bio-, psycho-, social functioning (return to school, relationship to family etc.) | 88.9 * | 85.7 * |
| Pediatric pain management planning decisions | 73.7 | 100 |
| ● Develop and monitor a child- (& parents-) centred management plan including realistic goals | 72.2 | 100 |
| ● Provide child (& parents) adapted information/education | 84.2 * | 100 * |
| Treatment considerations adapted to the different pediatric age groups | 80.0 | 100 |
| ● Specialized pain education for children (including communication & motivational techniques | 84.2 * | 100 * |
| ● Physical interventions adapted for different pediatric age groups | 73.7 | 100 |
| ● Exercise interventions for pediatric pain, e.g., Graded exposure | 84.2 * | 100 * |
| ● Insight into the opportunities of psychological interventions adapted to different pediatric age groups | 65.0 | 100 |
| ● Insight into the opportunities of medical/pharmacological interventions adapted to different ages | 59.1 | 100 |
| ● Insight into the opportunities of CAM (=complement & alternative therapy interventions) for different pediatric age groups | 50.0§ | 42.9§ |
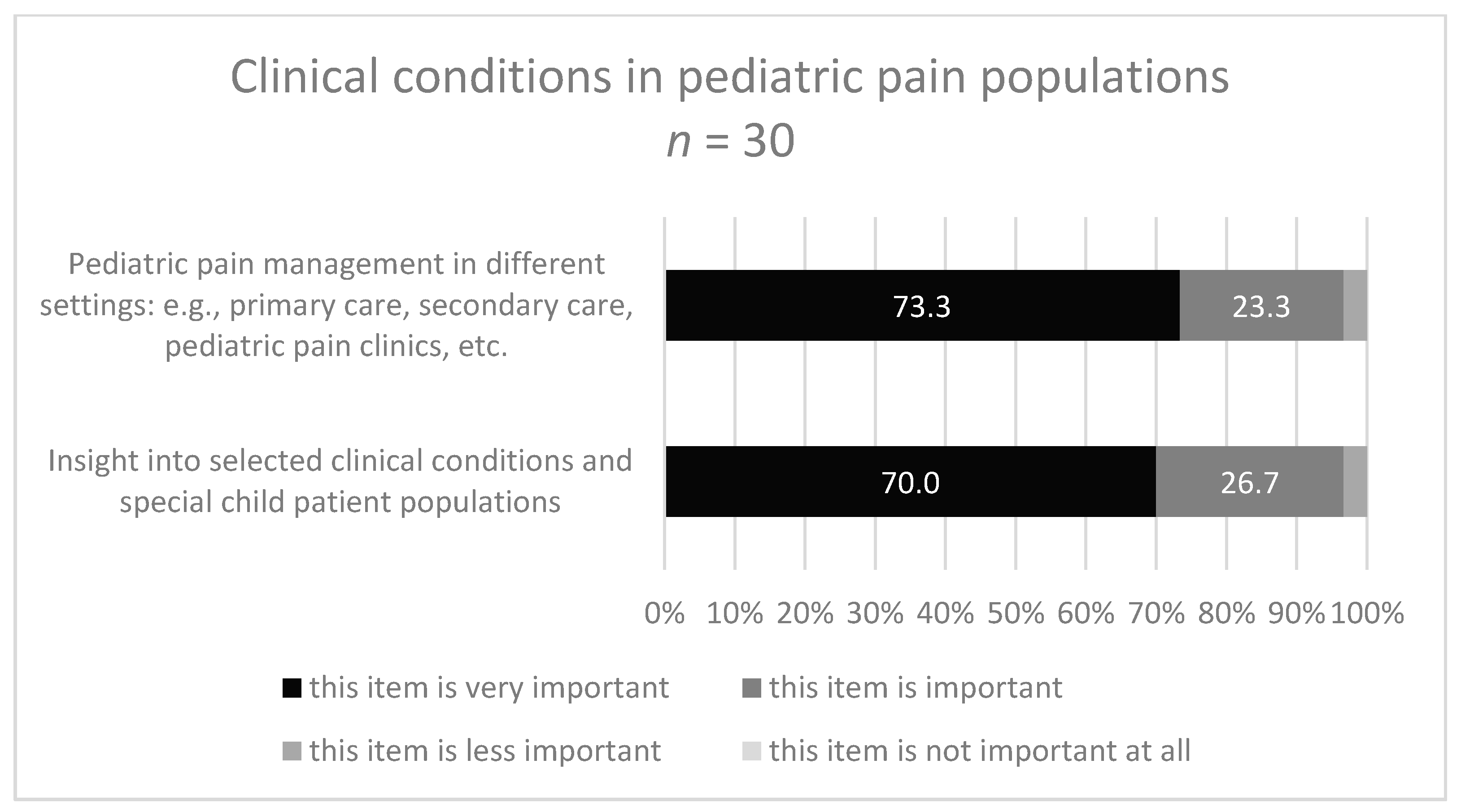
| 4. Specific clinical conditions in pediatric pain populations | ||
| Insight into selected clinical conditions and special child patient populations | 70.0 | 85.7 |
| Pediatric pain management in different settings: e.g., primary care, secondary care, pediatric pain clinics, etc. | 73.3 | 85.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laekeman, M.; Schäfer, A.; Moog, M.E.; Kuss, K. Recommendations for a Pediatric Pain Education Curriculum for Physical and Occupational Therapists: Scoping Review and Survey. Children 2021, 8, 390. https://doi.org/10.3390/children8050390
Laekeman M, Schäfer A, Moog ME, Kuss K. Recommendations for a Pediatric Pain Education Curriculum for Physical and Occupational Therapists: Scoping Review and Survey. Children. 2021; 8(5):390. https://doi.org/10.3390/children8050390
Chicago/Turabian StyleLaekeman, Marjan, Axel Schäfer, Martina Egan Moog, and Katrin Kuss. 2021. "Recommendations for a Pediatric Pain Education Curriculum for Physical and Occupational Therapists: Scoping Review and Survey" Children 8, no. 5: 390. https://doi.org/10.3390/children8050390
APA StyleLaekeman, M., Schäfer, A., Moog, M. E., & Kuss, K. (2021). Recommendations for a Pediatric Pain Education Curriculum for Physical and Occupational Therapists: Scoping Review and Survey. Children, 8(5), 390. https://doi.org/10.3390/children8050390