The Effect of NUDT15, TPMT, APEX1, and ITPA Genetic Variations on Mercaptopurine Treatment of Pediatric Acute Lymphoblastic Leukemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Collection
2.2. Genotyping
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics, Genotype Data, and Allele Frequencies
3.2. Associations between Genetic Polymorphisms and 6-Mercaptopurine Related Toxicities and Intolerances
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kato, M.; Manabe, A. Treatment and biology of pediatric acute lymphoblastic leukemia. Pediatrics Int. Off. J. Jpn. Pediatr. Soc. 2018, 60, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Landier, W.; Hageman, L.; Chen, Y.; Kim, H.; Sun, C.L.; Kornegay, N.; Evans, W.E.; Angiolillo, A.L.; Bostrom, B.; et al. Systemic Exposure to Thiopurines and Risk of Relapse in Children With Acute Lymphoblastic Leukemia: A Children’s Oncology Group Study. JAMA Oncol. 2015, 1, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Wahlund, M.; Nilsson, A.; Kahlin, A.Z.; Broliden, K.; Myrberg, I.H.; Appell, M.L.; Berggren, A. The Role of TPMT, ITPA, and NUDT15 Variants during Mercaptopurine Treatment of Swedish Pediatric Patients with Acute Lymphoblastic Leukemia. J. Pediatr. 2020, 216, 150–157.e1. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Hon, Y.Y.; Chu, Y.; Van de Poll, M.E.; Relling, M.V. Assay of 6-mercaptopurine and its metabolites in patient plasma by high-performance liquid chromatography with diode-array detection. J. Chromatogr. B Biomed. Sci. Appl. 1999, 732, 459–468. [Google Scholar] [CrossRef]
- Brem, R.; Karran, P. Oxidation-mediated DNA cross-linking contributes to the toxicity of 6-thioguanine in human cells. Cancer Res. 2012, 72, 4787–4795. [Google Scholar] [CrossRef] [PubMed]
- Valerie, N.C.; Hagenkort, A.; Page, B.D.; Masuyer, G.; Rehling, D.; Carter, M.; Bevc, L.; Herr, P.; Homan, E.; Sheppard, N.G.; et al. NUDT15 Hydrolyzes 6-Thio-DeoxyGTP to Mediate the Anticancer Efficacy of 6-Thioguanine. Cancer Res. 2016, 76, 5501–5511. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.E.; Hon, Y.Y.; Bomgaars, L.; Coutre, S.; Holdsworth, M.; Janco, R.; Kalwinsky, D.; Keller, F.; Khatib, Z.; Margolin, J.; et al. Preponderance of thiopurine S-methyltransferase deficiency and heterozygosity among patients intolerant to mercaptopurine or azathioprine. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2001, 19, 2293–2301. [Google Scholar] [CrossRef] [PubMed]
- Schmiegelow, K.; Forestier, E.; Kristinsson, J.; Söderhäll, S.; Vettenranta, K.; Weinshilboum, R.; Wesenberg, F. Thiopurine methyltransferase activity is related to the risk of relapse of childhood acute lymphoblastic leukemia: Results from the NOPHO ALL-92 study. Leukemia 2009, 23, 557–564. [Google Scholar] [CrossRef]
- Relling, M.V.; Altman, R.B.; Goetz, M.P.; Evans, W.E. Clinical implementation of pharmacogenomics: Overcoming genetic exceptionalism. Lancet Oncol. 2010, 11, 507–509. [Google Scholar] [CrossRef][Green Version]
- Chang, J.G.; Lee, L.S.; Chen, C.M.; Shih, M.C.; Wu, M.C.; Tsai, F.J.; Liang, D.C. Molecular analysis of thiopurine S-methyltransferase alleles in South-east Asian populations. Pharmacogenetics 2002, 12, 191–195. [Google Scholar] [CrossRef]
- Moradveisi, B.; Muwakkit, S.; Zamani, F.; Ghaderi, E.; Mohammadi, E.; Zgheib, N.K. ITPA, TPMT, and NUDT15 Genetic Polymorphisms Predict 6-Mercaptopurine Toxicity in Middle Eastern Children With Acute Lymphoblastic Leukemia. Front. Pharmacol. 2019, 10, 916. [Google Scholar] [CrossRef]
- Yang, S.K.; Hong, M.; Baek, J.; Choi, H.; Zhao, W.; Jung, Y.; Haritunians, T.; Ye, B.D.; Kim, K.J.; Park, S.H.; et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat. Genet. 2014, 46, 1017–1020. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.J.; Landier, W.; Yang, W.; Liu, C.; Hageman, L.; Cheng, C.; Pei, D.; Chen, Y.; Crews, K.R.; Kornegay, N.; et al. Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 1235–1242. [Google Scholar] [CrossRef]
- Kakuta, Y.; Naito, T.; Onodera, M.; Kuroha, M.; Kimura, T.; Shiga, H.; Endo, K.; Negoro, K.; Kinouchi, Y.; Shimosegawa, T. NUDT15 R139C causes thiopurine-induced early severe hair loss and leukopenia in Japanese patients with IBD. Pharm. J. 2016, 16, 280–285. [Google Scholar] [CrossRef]
- Kakuta, Y.; Kawai, Y.; Okamoto, D.; Takagawa, T.; Ikeya, K.; Sakuraba, H.; Nishida, A.; Nakagawa, S.; Miura, M.; Toyonaga, T.; et al. NUDT15 codon 139 is the best pharmacogenetic marker for predicting thiopurine-induced severe adverse events in Japanese patients with inflammatory bowel disease: A multicenter study. J. Gastroenterol. 2018, 53, 1065–1078. [Google Scholar] [CrossRef]
- Moriyama, T.; Nishii, R.; Perez-Andreu, V.; Yang, W.; Klussmann, F.A.; Zhao, X.; Lin, T.N.; Hoshitsuki, K.; Nersting, J.; Kihira, K.; et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat. Genet. 2016, 48, 367–373. [Google Scholar] [CrossRef]
- Asada, A.; Nishida, A.; Shioya, M.; Imaeda, H.; Inatomi, O.; Bamba, S.; Kito, K.; Sugimoto, M.; Andoh, A. NUDT15 R139C-related thiopurine leukocytopenia is mediated by 6-thioguanine nucleotide-independent mechanism in Japanese patients with inflammatory bowel disease. J. Gastroenterol. 2016, 51, 22–29. [Google Scholar] [CrossRef]
- Kim, H.T.; Choi, R.; Won, H.H.; Choe, Y.H.; Kang, B.; Lee, K.; Koo, H.H.; Yoo, K.H.; Kim, Y.H.; Lee, S.Y. NUDT15 genotype distributions in the Korean population. Pharm. Genom. 2017, 27, 197–200. [Google Scholar] [CrossRef]
- Stocco, G.; Cheok, M.H.; Crews, K.R.; Dervieux, T.; French, D.; Pei, D.; Yang, W.; Cheng, C.; Pui, C.H.; Relling, M.V.; et al. Genetic polymorphism of inosine triphosphate pyrophosphatase is a determinant of mercaptopurine metabolism and toxicity during treatment for acute lymphoblastic leukemia. Clin. Pharmacol. Ther. 2009, 85, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Sumi, S.; Marinaki, A.M.; Arenas, M.; Fairbanks, L.; Shobowale-Bakre, M.; Rees, D.C.; Thein, S.L.; Ansari, A.; Sanderson, J.; De Abreu, R.A.; et al. Genetic basis of inosine triphosphate pyrophosphohydrolase deficiency. Hum. Genet. 2002, 111, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Marsh, S.; King, C.R.; Ahluwalia, R.; McLeod, H.L. Distribution of ITPA P32T alleles in multiple world populations. J. Hum. Genet. 2004, 49, 579–581. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, H.; Seo, H.; Park, Y.; Min, B.J.; Seo, M.E.; Park, K.D.; Shin, H.Y.; Kim, J.H.; Kang, H.J. APEX1 Polymorphism and Mercaptopurine-Related Early Onset Neutropenia in Pediatric Acute Lymphoblastic Leukemia. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2018, 50, 823–834. [Google Scholar] [CrossRef]
- McNeill, D.R.; Lam, W.; DeWeese, T.L.; Cheng, Y.C.; Wilson, D.M., 3rd. Impairment of APE1 function enhances cellular sensitivity to clinically relevant alkylators and antimetabolites. Mol. Cancer Res. MCR 2009, 7, 897–906. [Google Scholar] [CrossRef]
- Schultz, K.R.; Pullen, D.J.; Sather, H.N.; Shuster, J.J.; Devidas, M.; Borowitz, M.J.; Carroll, A.J.; Heerema, N.A.; Rubnitz, J.E.; Loh, M.L.; et al. Risk- and response-based classification of childhood B-precursor acute lymphoblastic leukemia: A combined analysis of prognostic markers from the Pediatric Oncology Group (POG) and Children’s Cancer Group (CCG). Blood 2007, 109, 926–935. [Google Scholar] [CrossRef]
- Smith, M.; Arthur, D.; Camitta, B.; Carroll, A.J.; Crist, W.; Gaynon, P.; Gelber, R.; Heerema, N.; Korn, E.L.; Link, M.; et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1996, 14, 18–24. [Google Scholar] [CrossRef]
- Schmiegelow, K.; Nersting, J.; Nielsen, S.N.; Heyman, M.; Wesenberg, F.; Kristinsson, J.; Vettenranta, K.; Schrøeder, H.; Weinshilboum, R.; Jensen, K.L.; et al. Maintenance therapy of childhood acute lymphoblastic leukemia revisited-Should drug doses be adjusted by white blood cell, neutrophil, or lymphocyte counts? Pediatr. Blood Cancer 2016, 63, 2104–2111. [Google Scholar] [CrossRef] [PubMed]
- Schmiegelow, K.; Nielsen, S.N.; Frandsen, T.L.; Nersting, J. Mercaptopurine/Methotrexate maintenance therapy of childhood acute lymphoblastic leukemia: Clinical facts and fiction. J. Pediatr. Hematol. Oncol. 2014, 36, 503–517. [Google Scholar] [CrossRef]
- Jung, Y.S.; Cheon, J.H.; Park, J.J.; Moon, C.M.; Kim, E.S.; Lee, J.H.; Kim, S.W.; Kim, J.H.; Hong, S.P.; Kim, T.I.; et al. Correlation of genotypes for thiopurine methyltransferase and inosine triphosphate pyrophosphatase with long-term clinical outcomes in Korean patients with inflammatory bowel diseases during treatment with thiopurine drugs. J. Hum. Genet. 2010, 55, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Cheon, J.H.; Kim, J.H.; Kim, B.Y.; Kim, S.W.; Hong, S.Y.; Eun, C.S.; Hong, S.S.; Byeon, J.S.; Kim, T.I.; Han, D.S.; et al. Allele frequency of thiopurine methyltransferase and inosine triphosphate pyrophosphatase gene polymorphisms in Korean patients with inflammatory bowel diseases. Hepato-Gastroenterology 2009, 56, 421–423. [Google Scholar]
- Tanaka, Y.; Kato, M.; Hasegawa, D.; Urayama, K.Y.; Nakadate, H.; Kondoh, K.; Nakamura, K.; Koh, K.; Komiyama, T.; Manabe, A. Susceptibility to 6-MP toxicity conferred by a NUDT15 variant in Japanese children with acute lymphoblastic leukaemia. Br. J. Haematol. 2015, 171, 109–115. [Google Scholar] [CrossRef]
- Yi, E.S.; Choi, Y.B.; Choi, R.; Lee, N.H.; Lee, J.W.; Yoo, K.H.; Sung, K.W.; Lee, S.Y.; Koo, H.H. NUDT15 Variants Cause Hematopoietic Toxicity with Low 6-TGN Levels in Children with Acute Lymphoblastic Leukemia. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2018, 50, 872–882. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, T.; Yang, Y.L.; Nishii, R.; Ariffin, H.; Liu, C.; Lin, T.N.; Yang, W.; Lin, D.T.; Yu, C.H.; Kham, S.; et al. Novel variants in NUDT15 and thiopurine intolerance in children with acute lymphoblastic leukemia from diverse ancestry. Blood 2017, 130, 1209–1212. [Google Scholar] [CrossRef] [PubMed]
- Nishii, R.; Moriyama, T.; Janke, L.J.; Yang, W.; Suiter, C.C.; Lin, T.N.; Li, L.; Kihira, K.; Toyoda, H.; Hofmann, U.; et al. Preclinical evaluation of NUDT15-guided thiopurine therapy and its effects on toxicity and antileukemic efficacy. Blood 2018, 131, 2466–2474. [Google Scholar] [CrossRef]
- Tatsumi, G.; Kawahara, M.; Imai, T.; Nishishita-Asai, A.; Nishida, A.; Inatomi, O.; Yokoyama, A.; Kakuta, Y.; Kito, K.; Andoh, A. Thiopurine-mediated impairment of hematopoietic stem and leukemia cells in NUDT15(R138C) knock-in mice. Leukemia 2020, 34, 882–894. [Google Scholar] [CrossRef]
- Simone, P.D.; Pavlov, Y.I.; Borgstahl, G.E. ITPA (inosine triphosphate pyrophosphatase): From surveillance of nucleotide pools to human disease and pharmacogenetics. Mutat. Res. 2013, 753, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Li, L.; Yang, P.; Yang, L.; Zheng, J.E.; Zhou, Y.; Han, Y. Optimal predictor for 6-mercaptopurine intolerance in Chinese children with acute lymphoblastic leukemia: NUDT15, TPMT, or ITPA genetic variants? BMC Cancer 2018, 18, 516. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, G.; Kotur, N.; Krstovski, N.; Lazic, J.; Zukic, B.; Stankovic, B.; Janic, D.; Katsila, T.; Patrinos, G.P.; Pavlovic, S.; et al. Variants in TPMT, ITPA, ABCC4 and ABCB1 Genes As Predictors of 6-mercaptopurine Induced Toxicity in Children with Acute Lymphoblastic Leukemia. J. Med. Biochem. 2018, 37, 320–327. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | |
|---|---|
| Total number of patients, n (%) | 83 |
| Sex, n (%) | |
| Female | 27 (32.5) |
| Male | 56 (67.5) |
| Risk group, n (%) | |
| Standard risk | 52 (62.7) |
| High risk | 25 (30.1) |
| Very high risk | 6 (7.2) |
| Age at diagnosis, median (range) | 8.3 (1.0–16.2) |
| Leukemia type, n (%) | |
| B-ALL | 68 (81.9) |
| T-ALL | 8 (9.6) |
| Mixed-type | 4 (4.8) |
| Unclassified | 3 (3.6) |
| Cytogenetic abnormality, n (%) | |
| Normal | 28 (33.7) |
| Hyperdiploidy | 13 (15.7) |
| t(12;21)(p13;q22); ETV6-RUNX1 | 12 (14.5) |
| t(4;11)(q21;q23); MLL-AFF1 | 3 (3.6) |
| t(1;19)(q23;p13.3); TCF3-PBX1 | 3 (3.6) |
| t(9;22)(q34;q11.2); BCR-ABL1 | 1 (1.2) |
| Hypodiploidy | 1 (1.2) |
| Other/unknown | 22 (26.5) |
| Neutropenia (mean ± SD) | |
| ANC at 14th day (/mm3) | 708.8 ± 824.1 |
| ANC at 28th day (/mm3) | 188.6 ± 383.4 |
| Days of ANC < 1 × 103/mm3 (n = 76) | 268.3 ± 224.8 |
| Days of ANC < 0.5 × 103/mm3 (n = 70) | 136.8 ± 132.0 |
| Days of febrile neutropenia (n = 61) | 6.1 ± 5.3 |
| 6-MP dose (mg/m2, mean ± SD) | |
| First maintenance | 75 |
| Second maintenance | 51.6 ± 19.1 |
| Sixth maintenance | 48.5 ± 16.5 |
| Final maintenance | 45.3 ± 15.3 |
| 6-MP dose intensity * | |
| Second maintenance | 70.0 ± 24.8 |
| Sixth maintenance | 66.3 ± 22.5 |
| Final maintenance | 61.7 ± 21.0 |
| Maximum AST, (IU, mean ± SD) | 303.9 ± 220.7 |
| Maximum ALT, (IU, mean ± SD) | 636.3 ± 458.6 |
| Genotype, n (%) | |
| NUDT15 55_56insGAGTCG (rs746071566) | |
| Wild | 74 (89.2) |
| 55_56insGAGTCG | 9 (10.8) |
| NUDT15 c.415C>T (rs116855232) | |
| CC | 67 (80.7) |
| CA | 16 (19.3) |
| ITPA c.94C>A (rs1127354) | |
| CC | 62 (74.7) |
| CA | 21 (25.3) |
| ITPA c.IVS2+21A>C (rs7270101) | |
| AA | 82 (98.8) |
| AC | 1 (1.2) |
| APEX1 c.190A>G (rs2307486) | |
| AA | 74 (89.2) |
| AG | 9 (10.8) |
| TPMT | |
| *1/*1 | 82 (98.8) |
| *1/*3 | 1 (1.2) |
| NUDT15 c.415C>T + ITPA c.94C>A | 5 (6.0) |
| NUDT15 c.415C>T + APEX1 c.190A>G | 1 (1.2) |
| TPMT *1/*3 + ITPA c.94C>A | 1 (1.2) |
| ITPA c.94C>A + APEX1 c.190A>G | 2 (2.4) |
| ITPA rs1127354 | APEX1 rs2307486 | NUDT15 rs116855232 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Charcteristics | Genotype | CC (n = 62) CA (n = 21) | p | Genotype | AA (n = 74) AG (n = 9) | p | Genotype | CC (n = 67) CT (n = 16) | p * |
| 14th day ANC (/mm3) | CC | 1588.2 ± 1175.2 | 0.539 | AA | 1730.8 ± 1577.8 | 0.070 | CC | 1688.1 ± 1627.5 | 0.884 |
| CA | 1850.4 ± 2269.3 | AG | 814.5 ± 740.1 | CT | 1421.5 ± 1087.5 | ||||
| 28th day ANC (/mm3) | CC | 1482.2 ± 1112.5 | 0.379 | AA | 1425.9 ± 1169.3 | 0.677 | CC | 1561.5 ± 1223.8 | 0.095 |
| CA | 1274.4 ± 1246.7 | AG | 1443.8 ± 960.6 | CT | 892.4 ± 478.8 | ||||
| Days of ANC < 1 × 103/mm3 | CC | 260.5 ± 228.3 | 0.540 | AA | 262.4 ± 223.6 | 0.451 | CC | 263.9 ± 224.8 | 0.564 |
| CA | 290.1 ± 218.3 | AG | 321.6 ± 244.0 | CT | 285.9 ± 231.2 | ||||
| Days of ANC < 0.5 × 103/mm3 | CC | 127.3 ± 130.9 | 0.317 | AA | 131.6 ± 128.2 | 0.377 | CC | 133.9 ± 130.2 | 0.527 |
| CA | 163.2 ± 134.6 | AG | 182.8 ± 165.1 | CT | 148.3 ± 142.7 | ||||
| Days of febrile neutropenia | CC | 6.00 ± 5.56 | 0.608 | AA | 5.9 ± 5.3 | 0.383 | CC | 5.7 ± 5.1 | 0.102 |
| CA | 6.52 ± 4.70 | AG | 7.5 ± 5.1 | CT | 7.5 ± 6.0 | ||||
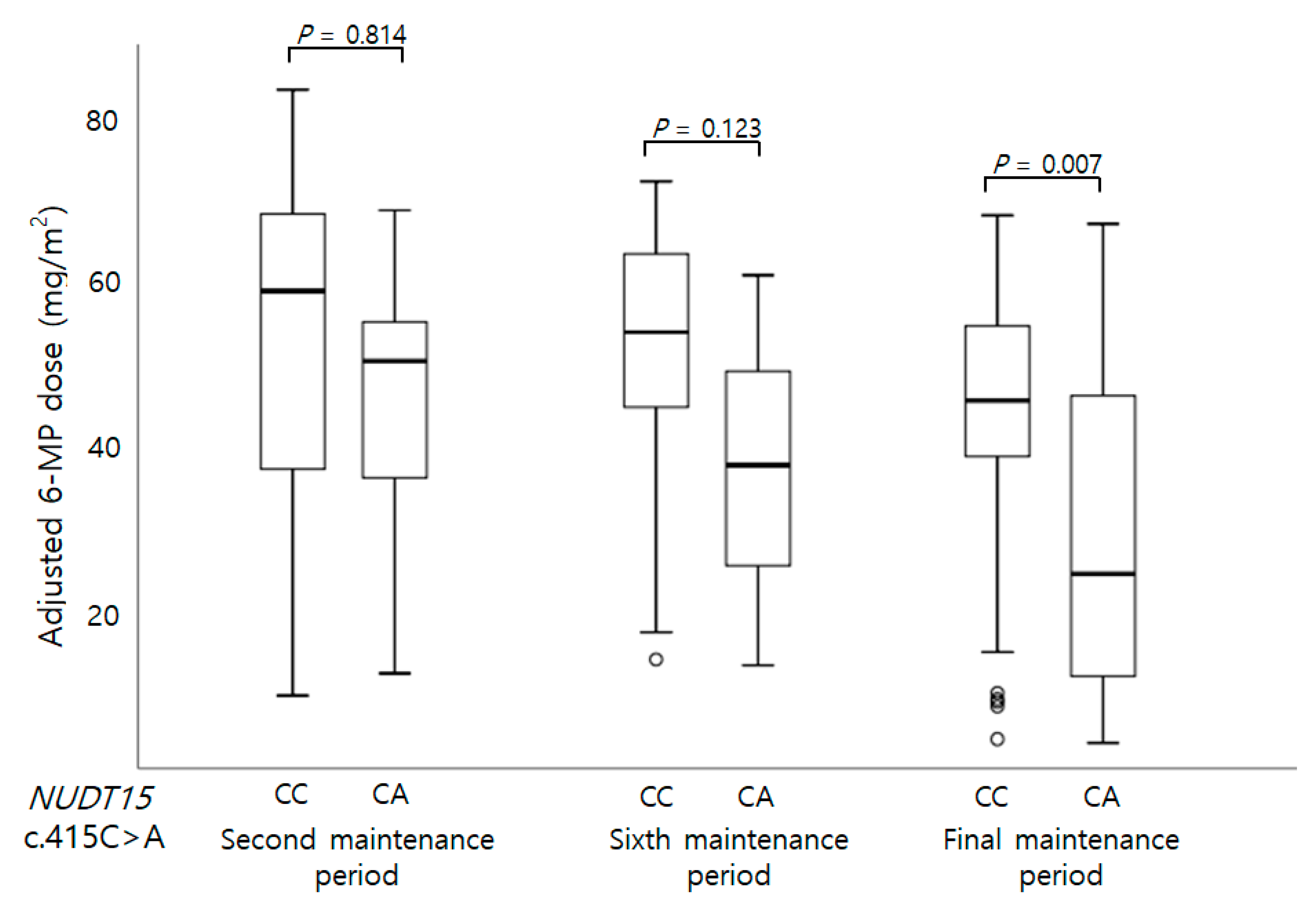
| 6-MP dose at second maintenance period (mg/m2) | CC | 50.5 ± 7.45 | 0.319 | AA | 51.4 ± 19.1 | 0.837 | CC | 53.0 ± 19.5 | 0.814 |
| CA | 54.6 ± 19.0 | AG | 52.8 ± 19.3 | CT | 45.6 ± 15.9 | ||||
| 6-MP dose at sixth maintenance period (mg/m2) | CC | 48.3 ± 16.7 | 1.000 | AA | 47.9 ± 17.1 | 0.615 | CC | 51.0 ± 15.6 | 0.123 |
| CA | 48.8 ± 16.4 | AG | 54.1 ± 6.7 | CT | 38.1 ± 16.3 | ||||
| 6-MP dose at final maintenance treatment (mg/m2) | CC | 45.6 ± 15.5 | 0.912 | AA | 45.0 ± 15.8 | 0.928 | CC | 47.7 ± 13.8 | 0.007 |
| CA | 44.5 ± 14.9 | AG | 47.7 ± 8.8 | CT | 35.4 ± 17.6 | ||||
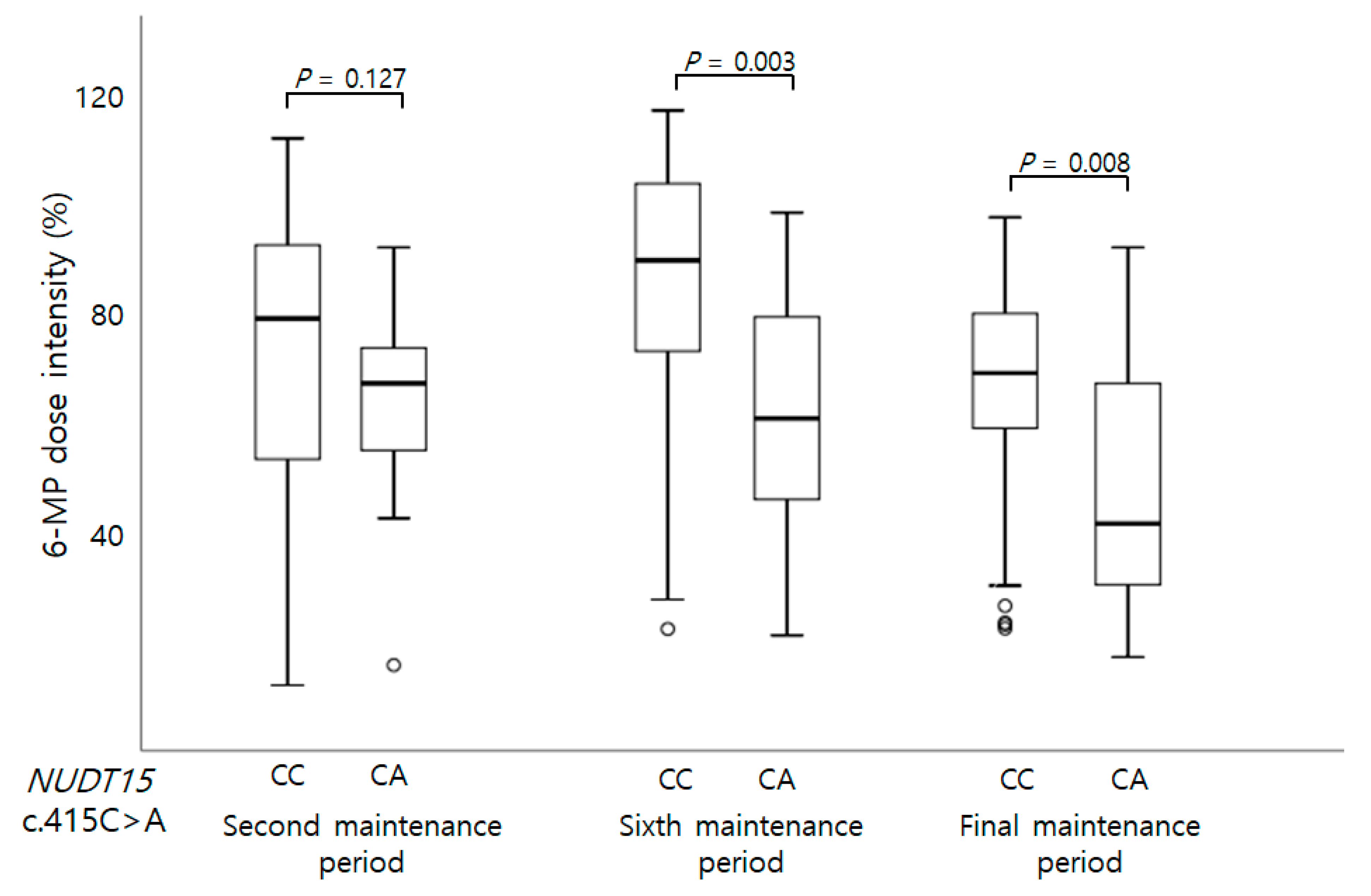
| 6-MP dose intensity † at second maintenance period (%) | CC | 68.1 ± 25.6 | 0.235 | AA | 67.0 ± 24.8 | 0.877 | CC | 72.7 ± 24.3 | 0.127 |
| CA | 75.2 ± 21.9 | AG | 70.4 ± 25.8 | CT | 59.2 ± 24.2 | ||||
| 6-MP dose intensity † at sixth maintenance period (%) | CC | 65.5 ± 23.1 | 0.788 | AA | 65.6 ± 23.3 | 0.797 | CC | 70.6 ± 20.1 | 0.003 |
| CA | 68.2 ± 21.0 | AG | 72.1 ± 9.0 | CT | 49.4 ± 23.6 | ||||
| 6-MP dose intensity † at final maintenance period (%) | CC | 61.6 ± 21.8 | 0.792 | AA | 61.5 ± 21.7 | 0.866 | CC | 65.9 ± 17.8 | 0.008 |
| CA | 61.8 ± 18.7 | AG | 63.6 ± 11.7 | CT | 45.5 ± 24.5 | ||||
| Maximum AST | CC | 298.3 ± 210.6 | 0.883 | AA | 305.7 ± 227.5 | 0.785 | CC | 308.1 ± 218.0 | 0.727 |
| CA | 646.6 ± 485.1 | AG | 286.8 ± 154.6 | CT | 286.6 ± 237.5 | ||||
| Maximum ALT | CC | 646.7 ± 485.1 | 0.974 | AA | 655.0 ± 474.0 | 0.255 | CC | 658.0 ± 478.4 | 0.427 |
| CA | 606.9 ± 383.6 | AG | 467.3 ± 240.9 | CT | 549.1 ± 369.1 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.M.; Shim, Y.J.; Kim, D.-H.; Jung, N.; Ha, J.-S. The Effect of NUDT15, TPMT, APEX1, and ITPA Genetic Variations on Mercaptopurine Treatment of Pediatric Acute Lymphoblastic Leukemia. Children 2021, 8, 224. https://doi.org/10.3390/children8030224
Lee JM, Shim YJ, Kim D-H, Jung N, Ha J-S. The Effect of NUDT15, TPMT, APEX1, and ITPA Genetic Variations on Mercaptopurine Treatment of Pediatric Acute Lymphoblastic Leukemia. Children. 2021; 8(3):224. https://doi.org/10.3390/children8030224
Chicago/Turabian StyleLee, Jae Min, Ye Jee Shim, Do-Hoon Kim, Nani Jung, and Jung-Sook Ha. 2021. "The Effect of NUDT15, TPMT, APEX1, and ITPA Genetic Variations on Mercaptopurine Treatment of Pediatric Acute Lymphoblastic Leukemia" Children 8, no. 3: 224. https://doi.org/10.3390/children8030224
APA StyleLee, J. M., Shim, Y. J., Kim, D.-H., Jung, N., & Ha, J.-S. (2021). The Effect of NUDT15, TPMT, APEX1, and ITPA Genetic Variations on Mercaptopurine Treatment of Pediatric Acute Lymphoblastic Leukemia. Children, 8(3), 224. https://doi.org/10.3390/children8030224






