Family Functioning in Families of Adolescents with Mental Health Disorders: The Role of Parenting Alliance
Abstract
1. Introduction
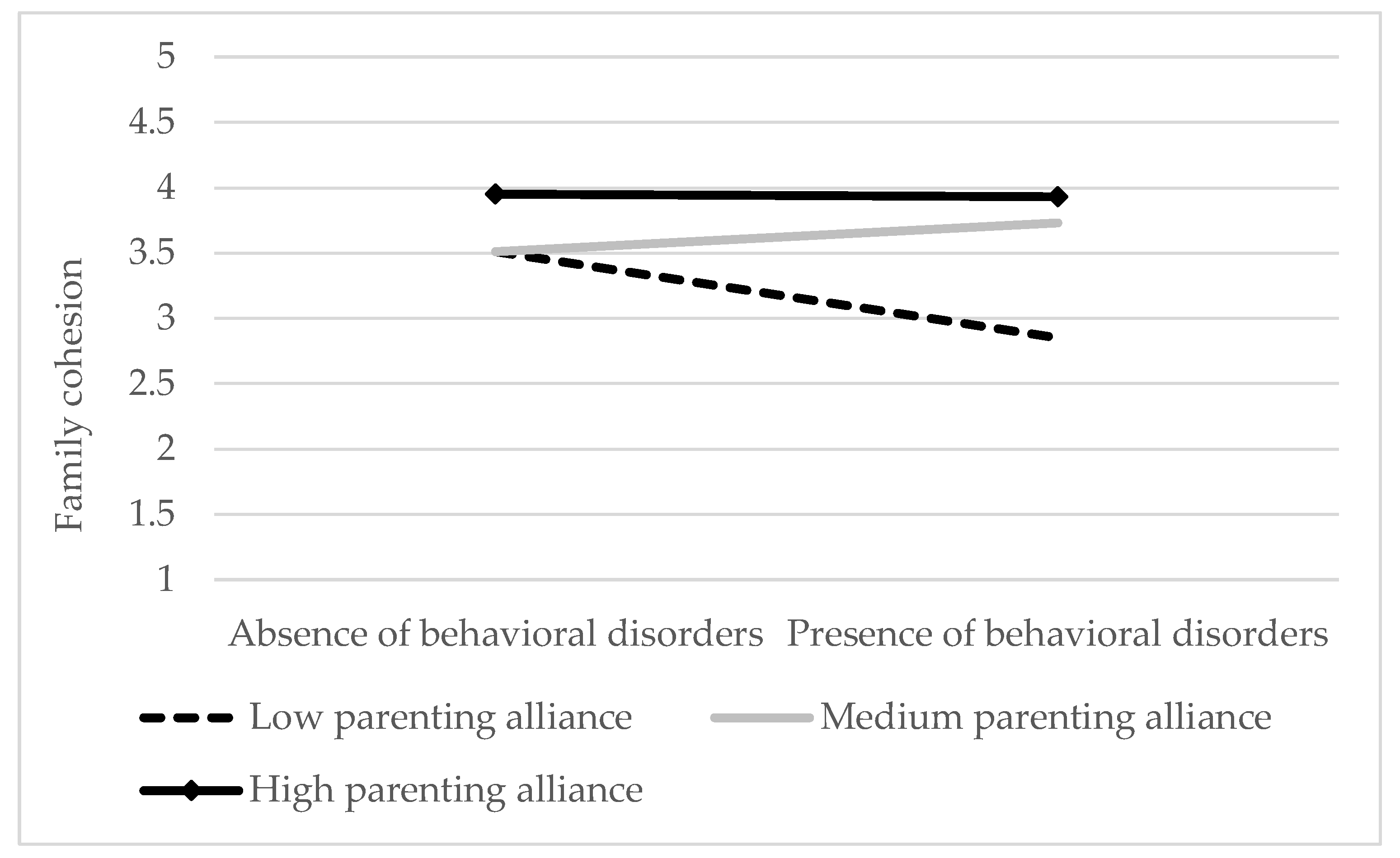
- To analyze the predictive role of emotional/behavioral disorders and parenting alliance on family cohesion.
- To examine the moderating effect of parenting alliance on the relationship between emotional and behavioral disorders and family cohesion.
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analyses
3. Results
Predictive Role of Disorders on Family Cohesion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Hofstra, M.B.; van der Ende, J.; Verhulst, F.C. Child and adolescent problems predict DSM-IV disorders in adulthood: A 14-year follow-up of a Dutch epidemiological sample. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Bongers, I.L.; Koot, H.M.; van der Ende, J.; Verhulst, F.C. Predicting young adult social functioning from developmental trajectories of externalizing behaviour. Psychol. Med. 2008, 38, 989–999. [Google Scholar] [CrossRef]
- Musitu, G.; Buelga, S.; Lila, M.; Cava, M.J. Familia y Adolescencia, 1st ed.; Síntesis: Madrid, Spain, 2001; ISBN 8477388938. [Google Scholar]
- Lubenko, J.; Sebre, S. Longitudinal associations between adolescent behaviour problems and perceived family relationships. Procedia Soc. Behav. Sci. 2010, 5, 785–790. [Google Scholar] [CrossRef][Green Version]
- Jaworska, N.; MacQueen, G. Adolescence as a unique developmental period. J. Psychiatry Neurosci. 2015, 40, 291–293. [Google Scholar] [CrossRef]
- Branje, S. Development of parent-adolescent relationships: Conflict interactions as a mechanism of change. Child Dev. Perspect. 2018, 12, 171–176. [Google Scholar] [CrossRef]
- Sameroff, A.J.; McKenzie, M.J. Research strategies for capturing transactional models of development: The limits of the possible. Dev. Psychopathol. 2003, 15, 613–640. [Google Scholar] [CrossRef]
- Serbin, L.A.; Kingdon, D.; Ruttle, P.L.; Stack, D.M. The impact of children’s internalizing and externalizing problems on parenting: Transactional processes and reciprocal change over time. Dev. Psychopathol. 2015, 27, 969–986. [Google Scholar] [CrossRef] [PubMed]
- Besemer, S.; Loeber, R.; Hinshaw, S.P.; Pardini, D.A. Bidirectional associations between externalizing behavior problems and maladaptive parenting within parent-son dyads across childhood. J. Abnorm. Child Psychol. 2016, 44, 1387–1398. [Google Scholar] [CrossRef] [PubMed]
- Roskam, I.; Stievenart, M.; de Mol, J. The transactional process between the relationships with caregivers and children’s externalizing behavior. J. Appl. Dev. Psychol. 2016, 42, 31–39. [Google Scholar] [CrossRef]
- Pardini, D.A.; Fite, P.J.; Burke, J.D. Bidirectional associations between parenting practices and conduct problems in boys from childhood to adolescence: The moderating effect of age and African-american ethnicity. J. Abnorm. Child Psychol. 2008, 36, 647–662. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Shelton, K.H.; Elgar, F.J. Prospective associations between the family environment, family cohesion, and psychiatric symptoms among adolescent girls. Child Psychiatry Hum. Dev. 2014, 45, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Preyde, M.; van Donge, C.; Carter, J.; Lazure, K. Parents of youth in intensive mental health treatment: Associations between emotional and behavioral disorders and parental sense of competence. Child Adolesc. Soc. Work. J. 2015, 32, 317–327. [Google Scholar] [CrossRef]
- Hughes, E.K.; Gullone, E. Internalizing symptoms and disorders in families of adolescents: A review of family systems literature. Clin. Psychol. Rev. 2008, 28, 92–117. [Google Scholar] [CrossRef] [PubMed]
- Brière, F.N.; Archambault, K.; Janosz, M. Reciprocal prospective associations between depressive symptoms and perceived relationship with parents in early adolescence. Can. J. Psychiatry 2013, 58, 169–176. [Google Scholar] [CrossRef]
- Olson, D.H.; Sprenkle, D.H.; Russell, C.S. Circumplex model of marital and family systems: I. Cohesion and adaptability dimensions, family types and clinical applications. Fam. Process. 1979, 18, 3–28. [Google Scholar] [CrossRef]
- Baer, J. Is family cohesion a risk or protective factor during adolescent development? J. Marriage Fam. 2002, 64, 668–675. [Google Scholar] [CrossRef]
- Goodrum, N.M.; Smith, D.W.; Hanson, R.F.; Moreland, A.D.; Saunders, B.E.; Kilpatrick, D.G. Longitudinal relations among adolescent risk behavior, family cohesion, violence exposure, and mental health in a national sample. J. Abnorm. Child Psychol. 2020, 48, 1455–1469. [Google Scholar] [CrossRef]
- Marsiglia, F.F.; Parsai, M.; Kulis, S. Effects of familism and family cohesion on problem behaviors among adolescents in Mexican inmigrant families in the Southwest United States. J. Ethn. Cult. Divers. Soc. Work 2009, 18, 203–220. [Google Scholar] [CrossRef] [PubMed]
- Scrimgeour, M.B.; Blandon, A.Y.; Stifter, C.A.; Buss, K.A. Cooperative coparenting moderates the association between parenting practices and children’s prosocial behavior. J. Fam. Psychol. 2013, 27, 506–511. [Google Scholar] [CrossRef]
- Frascarolo, F.; Despland, J.N.; Tissot, H.; Favez, N. Le coparentage, un concept clé pour évaluer le fonctionnement familial. Psychothérapies 2012, 32, 15–22. [Google Scholar] [CrossRef]
- Kwan, R.W.H.; Kwok, S.Y.C.L.; Ling, C.C.Y. The moderating roles of parenting self-efficacy and co-parenting alliance on marital satisfaction among Chinese fathers and mothers. J. Child Fam. Stud. 2015, 24, 3506–3515. [Google Scholar] [CrossRef]
- Riina, E.M.; McHale, S.M. Bidirectional influences between dimensions of coparenting and adolescent adjustment. J. Youth Adolesc. 2014, 43, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Teubert, D.; Pinquart, M. The association between coparenting and child adjustment: A meta-analysis. Parent. Sci. Pract. 2010, 10, 286–307. [Google Scholar] [CrossRef]
- Schoppe, S.J.; Mangelsdorf, S.C.; Frosch, C.A. Coparenting, family process, and family structure: Implications for preschoolers’ externalizing behavior problems. J. Fam. Psychol. 2001, 3, 526–545. [Google Scholar] [CrossRef]
- Marchand, J.F.; Hock, E. Mothers’ and fathers’ depressive symptoms and conflict-resolution strategies in the marriage and children’s externalizing and internalizing behaviors. J. Genet. Psychol. 2003, 164, 227–239. [Google Scholar] [CrossRef]
- Cui, M.; Donnellan, M.B.; Conger, R.D. Reciprocal influences between parents’ marital problems and adolescent internalizing and externalizing behavior. Dev. Psychol. 2007, 43, 1544–1552. [Google Scholar] [CrossRef]
- Majdanzic, M.; de Vente, W.; Feinberg, M.E.; Aktar, E.; Bögels, S.M. Bidirectional associations between coparenting relations and family member anxiety: A review and conceptual model. Clin. Child Fam. Psychol. Rev. 2012, 15, 28–42. [Google Scholar] [CrossRef]
- Raffaele, L.M.; Loker, T.; Fefer, S.; Wolgemuth, J.; Mann, A. “Either come together or fall apart”: Coparenting young children with challenging behaviors. Couple Fam. Psychol. 2015, 4, 74–91. [Google Scholar] [CrossRef]
- Olson, D.H.; Portner, J.; Lavee, Y. Manual de la Escala de Cohesión y Adaptabilidad Familiar (FACES III Manual); Life Innovation: Minneapolis, MN, USA, 1985. [Google Scholar]
- Abidin, R.R.; Brunner, J.F. Development of a Parenting Alliance Inventory. J. Clin. Child Psychol. 1995, 24, 31–40. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G. Multiple Regression: Testing and Interpreting Interactions; Sage: London, UK, 1991; ISBN 0-8039-3605-2. [Google Scholar]
- Gowers, S.G.; Bryan, C. Families of children with a mental disorder. In Families and Mental Disorders: From Burden to Empowerment; Sartorius, N., Leff, J., López-Ibor, J.J., Maj, M., Okasha, A., Eds.; John Wiley & Sons Ltd.: West Sussex, UK, 2005; pp. 127–160. [Google Scholar]
- McHale, J.P. Overt and covert coparenting processes in the family. Fam. Process. 1997, 36, 183–201. [Google Scholar] [CrossRef]
- Favez, N.; Widmer, E.D.; Doan, M.T.; Tissot, H. Coparenting in stepfamilies: Maternal promotion of family cohesiveness with partner and with father. J. Child Fam. Stud. 2015, 24, 3268–3278. [Google Scholar] [CrossRef]
- Feinberg, M.E. The internal structure and ecological context of coparenting: A framework for research and intervention. Parent. Sci. Pract. 2003, 3, 95–131. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The construct of resilience: A critical valuation and guidelines for future work. Child Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef]
- Haley, J. Trastornos de la Emancipación Juvenil y Terapia Familiar; McGraw-Hill: New York, NY, USA, 1985; ISBN 9789505184729. [Google Scholar]

| Step | β | t/F | ΔF | asr2/ΔR2 |
|---|---|---|---|---|
| 1 | 3.19 | 3.19 | 0.06 | |
| Child’s gender | −0.31 | −1.31 | 0.02 | |
| Child’s age | −0.18 * | −2.40 | 0.08 | |
| 2 | 3 | −0.19 | 0.02 | |
| Child’s gender | −0.17 | −0.69 | 0.01 | |
| Child’s age | −0.14 * | −1.75 | 0.04 | |
| Behavioral disorder | −0.40 | −1.57 | 0.03 | |
| 3 | 13.02 | 10.03 | 0.32 | |
| Child’s gender | −0.10 | −0.51 | <0.01 | |
| Child’s age | −0.14 * | −2.14 | 0.04 | |
| Behavioral disorder | −0.09 | −0.42 | 0.03 | |
| Parenting alliance | 0.81 ** | 6.19 | 0.32 | |
| 4 | 13 | –0.02 | 0.06 | |
| Child’s gender | −0.12 | −0.65 | <0.01 | |
| Child’s age | −0.16 * | −2.59 | 0.05 | |
| Behavioral disorder | 0.20 | 0.10 | <0.01 | |
| Parenting alliance | 0.49 * | 2.88 | 0.06 | |
| Behavioral disorder X Parenting alliance | 0.71 * | 2.79 | 0.06 |
| Step | β | t/F | ΔF | asr2/ΔR2 |
|---|---|---|---|---|
| 1 | 3.19 | 3.19 | 0.06 | |
| Child’s gender | −0.31 | −1.31 | 0.02 | |
| Child’s age | −0.18 * | −2.40 | 0.08 | |
| 2 | 2.10 | −1.08 | −0.01 | |
| Child’s gender | −0.30 | −1.30 | 0.02 | |
| Child’s age | −0.19 * | −2.38 | 0.08 | |
| Emotional disorder | −0.04 | −0.15 | <0.01 | |
| 3 | 13.22 | 11.12 | 0.36 | |
| Child’ gender | −0.13 | −0.69 | <0.01 | |
| Child’s age | −0.14 * | −2.26 | 0.04 | |
| Emotional disorder | 0.16 | 0.79 | 0.01 | |
| Parenting alliance | 0.84 ** | 6.54 | 0.35 | |
| 4 | 12.30 | −0.92 | 0.04 | |
| Child’s gender | −0.02 | −0.11 | <0.01 | |
| Child’s age | −0.12 | −1.96 | <0.01 | |
| Emotional disorder | 0.05 | 0.23 | <0.01 | |
| Parenting alliance | 0.99 ** | 7.04 | 0.39 | |
| Emotional disorder X Parenting alliance | −0.76 * | −2.30 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baena, S.; Jiménez, L.; Lorence, B.; Hidalgo, M.V. Family Functioning in Families of Adolescents with Mental Health Disorders: The Role of Parenting Alliance. Children 2021, 8, 222. https://doi.org/10.3390/children8030222
Baena S, Jiménez L, Lorence B, Hidalgo MV. Family Functioning in Families of Adolescents with Mental Health Disorders: The Role of Parenting Alliance. Children. 2021; 8(3):222. https://doi.org/10.3390/children8030222
Chicago/Turabian StyleBaena, Sofía, Lucía Jiménez, Bárbara Lorence, and Mᵃ Victoria Hidalgo. 2021. "Family Functioning in Families of Adolescents with Mental Health Disorders: The Role of Parenting Alliance" Children 8, no. 3: 222. https://doi.org/10.3390/children8030222
APA StyleBaena, S., Jiménez, L., Lorence, B., & Hidalgo, M. V. (2021). Family Functioning in Families of Adolescents with Mental Health Disorders: The Role of Parenting Alliance. Children, 8(3), 222. https://doi.org/10.3390/children8030222






