Interventions to Improve the Cast Removal Experience for Children and Their Families: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion/Exclusion Criteria
2.2. Data Extraction
2.3. Critical Appraisal
3. Results
3.1. Interventions
3.2. Outcomes
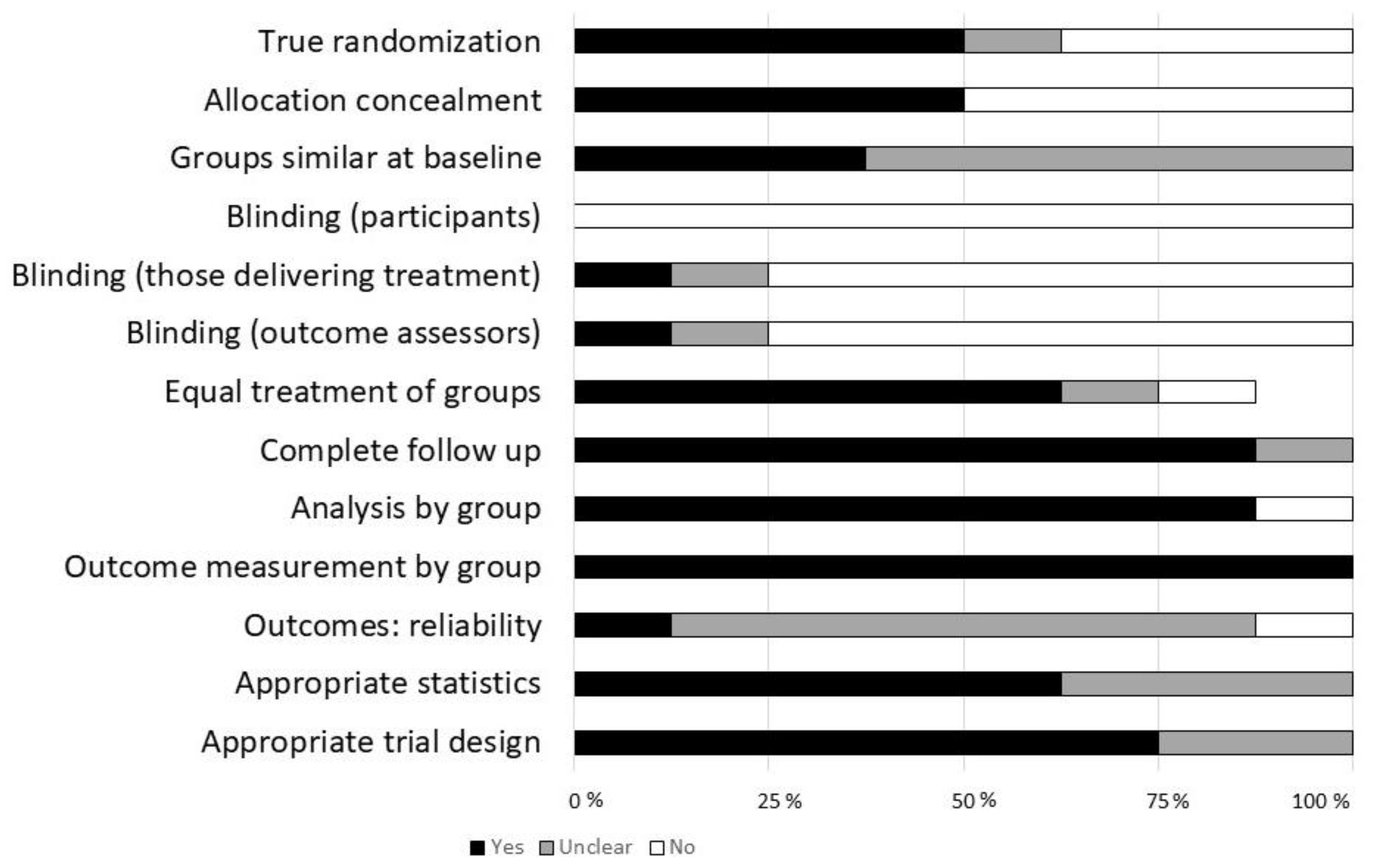
3.3. Critical Appraisal
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| exp infant/or exp child/or adolescent/ |
| child health/or infant health/or adolescent health/ |
| exp child health services/or adolescent health services/ |
| exp pediatrics/or exp pediatricians/or exp nurses, pediatric/or pediatric nurse practitioners/or pediatric assistants/or adolescent medicine/or hospitals, pediatric/or exp pediatric nursing/ |
| (p?ediatric*).tw,kf |
| (infant* or infancy).tw,kf |
| (baby* or babies).tw,kf |
| (neonat* or newborn* or new-born*).tw,kf |
| (child* or kid or kids).tw,kf |
| (schoolchild* or school age* or schoolage* or primary school* or elementary school* or secondary school* or high school* or highschool*).tw,kf |
| (preschool or pre-school or toddler or kindergar* or nursery).tw,kf |
| (adoles* or teen* or youth or youths or young people or young person* or young adult* or pre-teen* or preteen*).tw,kf |
| (boy* or girl*).tw,kf |
| or/1–13 |
| exp Anxiety/or exp fear/or stress, psychological/or frustration/ |
| exp Anxiety Disorders/or stress disorders, traumatic/or psychological trauma/or stress disorders, post-traumatic/or stress disorders, traumatic, acute/or exp phobic disorders/ |
| exp patient satisfaction/ |
| (anxiet* or stress disorder* or psychological* trauma* or ptsd or ptsds or post trauma* or posttrauma* or (stress* adj2 trauma*)).tw,kf |
| (anxious* or fear or fears or fearful* or nervous* or worrie* or worry* or angst or apprehensi* or panic* or phobic or phobia* or distress* or stress* or uncomfortable or discomfort* or frustrat* or unhapp*).tw,kf |
| ((patient* or parent* or family or child*) adj3 (experience* or satisf* or preparedness or dissatisf*)).tw,kf |
| or/15–20 |
| casts, surgical/ |
| ((fiberglass or fibreglass or cast or casts or casting or plaster* or spica) adj5 (remov* or room or clinic or saw or saws or sawing or cut or cuts or cutting)).tw,kf |
| ((cast or casts or casting or orthopedic* or fracture) adj3 (technician* or technologist*)).tw,kf |
| or/22–24 |
| 14 and 21 and 25 |
| 26 not (exp animals/not humans.sh) |
| limit 27 to yr=“1975-Current” |
References
- Rees, C.E. A Quick and Easy Method for the Removal of Plaster Casts. Calif. State J. Med. 1922, 20, 147. [Google Scholar]
- Lerwick, J.L. Minimizing pediatric healthcare-induced anxiety and trauma. World J. Clin. Pediatrics 2016, 5, 143–150. [Google Scholar] [CrossRef]
- Von Baeyer, C.L.; Marche, T.A.; Rocha, E.M.; Salmon, K. Children’s memory for pain: Overview and implications for practice. J. Pain 2004, 5, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.M.; Clough, V.; Gowda, A.S.; Tucker, M.C. Multimethod assessment of children’s distress during noninvasive outpatient medical procedures: Child and parent attitudes and factors. J. Pediatric Psychol. 2012, 37, 557–566. [Google Scholar] [CrossRef]
- Pate, J.T.; Blount, R.L.; Cohen, L.L.; Smith, A.J. Childhood Medical Experience and Temperament as Predictors of Adult Functioning in Medical Situations. Children’s Health Care 1996, 25, 281–298. [Google Scholar] [CrossRef]
- Lee Smith, M. Interventions to Minimize Distress during Pediatric Primary Care Visits: A Systematic Literature Review; Brigham Young University: Provo, UT, USA, 2014; Volume 4. [Google Scholar]
- Maclaren, J.E.; Cohen, L.L. Interventions for paediatric procedure-related pain in primary care. Paediatr. Child Health 2007, 12, 111–116. [Google Scholar] [PubMed]
- Trottier, E.D.; Doré-Bergeron, M.J.; Chauvin-Kimoff, L.; Baerg, K.; Ali, S. Managing pain and distress in children undergoing brief diagnostic and therapeutic procedures. Paediatr. Child Health 2019, 24, 509–535. [Google Scholar] [CrossRef]
- The Hospital for Sick Children (SickKids). Acute Pain: How to Treat and Manage in Young Children. Available online: https://www.aboutkidshealth.ca/article?contentid=3637&language=english (accessed on 15 August 2020).
- Wiggins, C.E.; Brown, K.D. Hearing protection and cast saw noise. J. South Orthop. Assoc. 1996, 5, 1–4. [Google Scholar] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Systematic reviews of effectiveness. In Joanna Briggs Institute Reviewer’s Manual; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Carmichael, K.D.; Westmoreland, J. Effectiveness of ear protection in reducing anxiety during cast removal in children. Am. J. Orthop. (Belle Mead NJ) 2005, 34, 43–46. [Google Scholar]
- Johnson, J.E.; Kirchhoff, K.T.; Endress, M.P. Altering children’s distress behavior during orthopedic cast removal. Nurs. Res. 1975, 24, 404–410. [Google Scholar] [CrossRef]
- Johnson, J.; Kirchhoff, K.; Endress, M. Easing children’s fright during health care procedures. Am. J. Matern. Child Nurs. 1976, 1, 206–210. [Google Scholar] [CrossRef]
- Katz, K.; Fogelman, R.; Attias, J.; Baron, E.; Soudry, M. Anxiety reaction in children during removal of their plaster cast with a saw. J. Bone Joint Surg. Br. 2001, 83, 388–390. [Google Scholar] [CrossRef]
- Ko, J.S.; Whiting, Z.; Nguyen, C.; Liu, R.W.; Gilmore, A. A Randomized Prospective Study Of The Use Of Ipads In Reducing Anxiety During Cast Room Procedures. Iowa Orthop. J. 2016, 36, 128–132. [Google Scholar]
- Liu, R.W.; Mehta, P.; Fortuna, S.; Armstrong, D.G.; Cooperman, D.R.; Thompson, G.H.; Gilmore, A. A randomized prospective study of music therapy for reducing anxiety during cast room procedures. J. Pediatric Orthop. 2007, 27, 831–833. [Google Scholar] [CrossRef] [PubMed]
- Mahan, S.T.; Harris, M.S.; Lierhaus, A.M.; Miller, P.E.; DiFazio, R.L. Noise Reduction to Reduce Patient Anxiety During Cast Removal: Can We Decrease Patient Anxiety With Cast Removal by Wearing Noise Reduction Headphones During Cast Saw Use? Orthop. Nurs. 2017, 36, 271–278. [Google Scholar] [CrossRef]
- Schlechter, J.A.; Avik, A.L.; DeMello, S. Is there a role for a child life specialist during orthopedic cast room procedures? A prospective-randomized assessment. J. Pediatric Orthop. B 2017, 26, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.L.; Ip, W.Y.; Kwok, B.M.C.; Choi, K.C.; Ng, B.K.W.; Chan, C.W.H. Effects of therapeutic play on children undergoing cast-removal procedures: A randomised controlled trial. BMJ Open 2018, 8, e021071. [Google Scholar] [CrossRef]
- Lazarus, R.S. Emotions and adaptation: Conceptual and empirical relations. In Nebraska Symposium on Motivation; Arnold, W.J., Ed.; University of Nebraska Press: Lincoln, NE, USA, 1968; Volume 16, pp. 175–269. [Google Scholar]
- Schachter, S.; Singer, J.E. Cognitive, social, and physiological determinants of emotional state. Psychol. Rev. 1962, 69, 379–399. [Google Scholar] [CrossRef] [PubMed]
- Piaget, J. The Psychology of Intelligence; Routledge & Kegan: London, UK, 1971. [Google Scholar]
- Lazarus, R.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Piaget, J. The Origins of Intelligence in Children; W.W. Norton & Company Inc.: New York, NY, USA, 1963. [Google Scholar]
- Trotman, G.P.; Veldhuijzen van Zanten, J.J.C.S.; Davies, J.; Möller, C.; Ginty, A.T.; Williams, S.E. Associations between heart rate, perceived heart rate, and anxiety during acute psychological stress. Anxiety Stress Coping 2019, 32, 711–727. [Google Scholar] [CrossRef] [PubMed]
- Domecq, J.P.; Prutsky, G.; Elraiyah, T.; Wang, Z.; Nabhan, M.; Shippee, N.; Brito, J.P.; Boehmer, K.; Hasan, R.; Firwana, B.; et al. Patient engagement in research: A systematic review. BMC Health Serv. Res. 2014, 14, 89. [Google Scholar] [CrossRef] [PubMed]
- Manafo, E.; Petermann, L.; Mason-Lai, P.; Vandall-Walker, V. Patient engagement in Canada: A scoping review of the ’how’ and ‘what’ of patient engagement in health research. Health Res. Policy Syst. 2018, 16, 5. [Google Scholar] [CrossRef] [PubMed]
- Slattery, P.; Saeri, A.K.; Bragge, P. Research co-design in health: A rapid overview of reviews. Health Res. Policy Syst. 2020, 18, 17. [Google Scholar] [CrossRef]

| Reference (First Author [ref]) | Year, Country | Study Site | Age of Participants (Range) | Sample Size (Male/Female) | Procedure(s) During Which Intervention Was Tested |
|---|---|---|---|---|---|
| Carmichael [17] | 2005; US | Not specified | 0–18 | 100 (62/48) | Cast removal |
| Johnson [18,19] | 1975 and 1976; US | Children’s hospital, orthopedic fracture clinic | 6–11 | 84 (52/32) | Cast removal |
| Katz [20] | 2001; Israel | Not specified | 5–6 | 20 (not specified) | Cast removal, forearm fracture |
| Ko [21] | 2016; US | Orthopedic clinic | 1–18 | 146 (84/62) | Cast room procedures (cast removal, cast placement, cast overwrap, splint placement, fracture reduction, joint injection, dressing change, suture removal, aspiration, external fixator structural change, pin removal) |
| Liu [22] | 2007; US | Hospital orthopedic clinic | 0–10 | 69 (not specified) | Cast room procedures (cast removal, cast application, pin removal, suture removal) |
| Mahan [23] | 2017; US | Outpatient orthopedic clinic | 2–10 | 50 (32/18) | Cast removal |
| Schlechter [24] | 2017; US | Orthopedic clinic | 2–10 | 86 (not specified) | Cast room procedures (splint removal, initial cast placement, fracture manipulation, pin removal, cast removal) |
| Wong [25] | 2017; China | Regional teaching hospital, orthopedic outpatient clinic | 3–12 Randomization stratified by age (3–7, 8–12) | 208 (135/73) | Cast removal |
| Study (First Author, [Ref]) | Why (Rationale/Theory, Goal) | What (Intervention (I); Control (C)) | Possible Physical/Psychological Strategies Involved 1 | How It Was Implemented (Mode; When and How Much) | Who Provided | Tailoring |
|---|---|---|---|---|---|---|
| Physical | ||||||
| Carmichael [17] | Rationale: Noise and vibration of saw likely contribute to anxiety during cast removal. This may be improved with ear protection. Goal: Study the impact of hearing protection on anxiety in children of different age groups. | I: Noise reducing hearing protection during cast removal. C: No hearing protection. | Noise reduction | Hearing protection was given to children prior to starting cast removal procedure. | NR | NR |
| Katz [20] | Rationale: A serious adverse event had occurred during cast removal at the study author’s institution. Goal: To address a gap in the literature on anxiety and anxiety reduction during cast removal in children. | I: Noise reducing hearing protection during cast removal C: No hearing protection. | Noise reduction | Hearing protection was given during cast removal. | NR | NR |
| Psychological | ||||||
| Johnson [18,19] | Theory: Informed by work linking cognitive processes and emotions/ behaviour (Lazarus, RS [26]; Schachter and Singer [27]), as well as author’s previous research demonstrating impact of interactions tailored to patient’s emotional needs. Builds on authors own research related to preparatory sensory-based information. Piaget’s theory of cognitive development informed the participant age inclusion criteria [28]. Goal: To affect the emotional response to cast removal through cognitive processes. | I: Recorded description of sensations during cast removal. C1: Recorded description of procedure of cast removal. C2: No recording. | Preparatory information | Children heard recordings (via headphones) prior to procedure. | Study nurse | NR |
| Ko [21] | Rationale: Electronic devices had been found to reduce anxiety during other health care procedures but had not been evaluated during cast room procedures. Goal: Determine if use of iPads reduce anxiety during cast removal. | I1: iPad with video I2: iPad with game. C: No iPad | Distraction | iPads were given to the patients as they went into the cast room to use during the procedure. | NR | Intervention group participants could choose from a list of available videos or games. |
| Liu [22] | Rationale: Anxiety and other adverse events can occur during cast removal. Hearing protection may be beneficial but not all children can wear headphones. Music therapy has demonstrated some effectiveness in other settings. Goal: Study the impact of soothing music in cast room with children. | I: Background lullaby music in the cast room clinic. C: No music. | Music therapy | Cast rooms were randomized to music or no music; music was playing when participant entered room. | Not applicable | NR |
| Schlechter [24] | Rationale: CCLS have been found to improve children’s health care experience in certain settings, but the role and impact of CCLS within the cast room had not been previously described/studied. Goal: Describe the impact of a CCLS in the cast room setting | I: Certified Child Life Specialist (CCLS) present. C: No CCLS present. | Preparatory information; play; distraction | CCLS present and interacting with child during procedure. | CCLS | CCLS used variety of methods (not documented consistently). |
| Wong [25] | Theory: Theory of stress and coping (Lazarus and Coleman [29]). Theory of cognitive development (Piaget [30]) used to determine age ranges. Rationale: Therapeutic play to improve a child’s sense of control during cast room procedures may assist with coping and reduce anxiety. Goal: To study the effect of therapeutic play on anxiety for children undergoing cast removal. | I: Preparation and distraction play plus standard care. C: Standard care (nurse provided preparatory information; reassurance) | Preparatory information; play; distraction | Preparation play was delivered before cast removal; distraction play during procedure. | Hospital play specialist | Play methods tailored to child’s preferences; parent presence and involvement supported. |
| Combined physical & psychological | ||||||
| Mahan [23] | Rationale: Loud cast saws can contribute to anxiety in children during cast removal; and anxiety may lead to behaviours that can result in injury (e.g., pulling away). Using headphones combined with a device has not been studied. Goal: Reduce exposure to noise to reduce anxiety during cast removal and improve parent satisfaction. | I: Noise cancelling headphones with electronic device (music/video, videogames). C: Standard care | Noise reduction; distraction | Headphones were used before, during and after cast removal. | Not specified | Families were asked to bring own device with child’s preferred media; could also borrow device from facility. |
| Study (First Author [Ref]) | Outcome Measures | Findings |
|---|---|---|
| Physical | ||
| Carmichael [17] | Heart Rate (HR) Mean arterial pressure (MAP) | Age combined data: less increase in HR in intervention vs. control (8.4% vs. 14.4%; p = 0.04). Non-significant (NS) differences MAP. Age stratified data: non-significant trend toward smaller increase in HR with intervention in younger children (<13 y). NS difference MAP. Author’s conclusion: Using hearing protections appeared to have a positive effect on HR but not MAP. Younger children appear to benefit more. |
| Katz [20] | HR | Less increase in HR intervention vs. control (11.1% vs. 26.9%; p =< 0.01) Author’s conclusion: Hearing protection reduced anxiety during cast removal as measured by HR. |
| Psychological | ||
| Johnson [18,19] | Stick figure score (fear) Observed and scored behaviour (distress) HR | Fear prior to cast removal was associated with distress scores across all groups (p < 0.001). Fear prior to cast removal was associated with fear during the procedure (p < 0.001). Participants in the sensation-based information group had lower distress scores than the no information control group (p < 0.025). Significant increase in HR (from waiting room to during procedure) in control group and procedure-based intervention group; NS increase in HR in the sensation-based intervention group. Author’s conclusion: Sensation-based preparatory messages can reduce distress during cast removal; baseline fear level is an important factor in fear and distress during the procedure. |
| Ko [21] | HR | Higher HR in intervention group (video game) before procedure. Decrease in HR from waiting room to before procedure in intervention group (video) for all procedures, and when cast removal analysed separately (p < 0.05), however increase in HR in intervention (video) group during procedure (p = 0.047). Author’s conclusion: Using an iPad with video may assist with lowering HR before the procedure, but the sound of the cast saw during the procedure may eliminate this benefit. |
| Liu [22] | HR | A more favourable change in HR from the waiting room to procedure room in intervention group, across all procedures (−2.7 bpm vs. 4.7 bpm. p = 0.001) and in sub-group analysis (cast removal or cast application). A more favourable change in HR for the intervention group was also observed from waiting room to during procedure, across procedures (15.3 bpm vs. 22.5 bpm; p = 0.05); no differences observed when analysed by sub-groups. No difference in change in HR between groups at other time points (before intervention to during intervention; before intervention to after intervention). Author’s conclusion: Soft lullaby music may improve young children’s experience in the cast room, when entering the cast room and during procedures. |
| Schlechter [24] | HR Behavioural scale (study specific) Parent survey | NS differences in HR between groups. More favourable behavioural score in intervention group (p < 0.01). NS difference in parent surveys (experience, child behaviour) between groups. Author’s conclusion: Certified Child Life Specialist presence seems to positively effect cast room experience based on the study-specific behavior scale that was used. |
| Wong [25] | Visual Analogue Scale-Anxiety (VAS-A): Ages 3–7 years Chinese version of the State Anxiety Scale for Children (CSAS-C): Ages 8–12 years Children’s Emotional Manifestation Scale (CEMS) (emotional behavior) Satisfaction scale (parent; technician) HR | VAS-A, ages 3–7 years: Significant difference in change in anxiety (before procedure to after), favouring intervention group (p = 0.010). CSAS-C, ages 8–12 years: NS difference between intervention and control. CEMS: Emotional behaviour during the cast removal favoured intervention groups (p < 0.001). Parent and cast technician satisfaction higher with intervention group (p = 0.02; p < 0.001 respectively). Stratified by age group: NS difference between groups for 3–7 years old; significantly lower HR in intervention group before and during procedure for 8–12 year-olds (p = 0.037). Author’s conclusion: Therapeutic play can reduce anxiety and improve experience (including parent and technician satisfaction) of cast removal. |
| Combined (physical and psychological) | ||
| Mahan [23] | Faces, Legs, Activity, Cry, Consolability scale (FLACC) HR Parent anxiety and satisfaction | NS differences in FLACC before or after procedure between groups; lower FLACC during procedure in intervention group (p = 0.03). Lower HR before (p = 0.02) and after the procedure (p = 0.005) in intervention group. Older age was associated with lower HR before, during and after procedure across groups, and lower FLACC scores during procedure. No differences in parent anxiety or satisfaction between groups. Author’s conclusion: Headphones and device use can improve children’s anxiety during cast removal. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maharjan, P.; Murdock, D.; Tielemans, N.; Goodall, N.; Temple, B.; Askin, N.; Wittmeier, K. Interventions to Improve the Cast Removal Experience for Children and Their Families: A Scoping Review. Children 2021, 8, 130. https://doi.org/10.3390/children8020130
Maharjan P, Murdock D, Tielemans N, Goodall N, Temple B, Askin N, Wittmeier K. Interventions to Improve the Cast Removal Experience for Children and Their Families: A Scoping Review. Children. 2021; 8(2):130. https://doi.org/10.3390/children8020130
Chicago/Turabian StyleMaharjan, Pramila, Dustin Murdock, Nicholas Tielemans, Nancy Goodall, Beverley Temple, Nicole Askin, and Kristy Wittmeier. 2021. "Interventions to Improve the Cast Removal Experience for Children and Their Families: A Scoping Review" Children 8, no. 2: 130. https://doi.org/10.3390/children8020130
APA StyleMaharjan, P., Murdock, D., Tielemans, N., Goodall, N., Temple, B., Askin, N., & Wittmeier, K. (2021). Interventions to Improve the Cast Removal Experience for Children and Their Families: A Scoping Review. Children, 8(2), 130. https://doi.org/10.3390/children8020130






