Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review
Abstract
1. Introduction
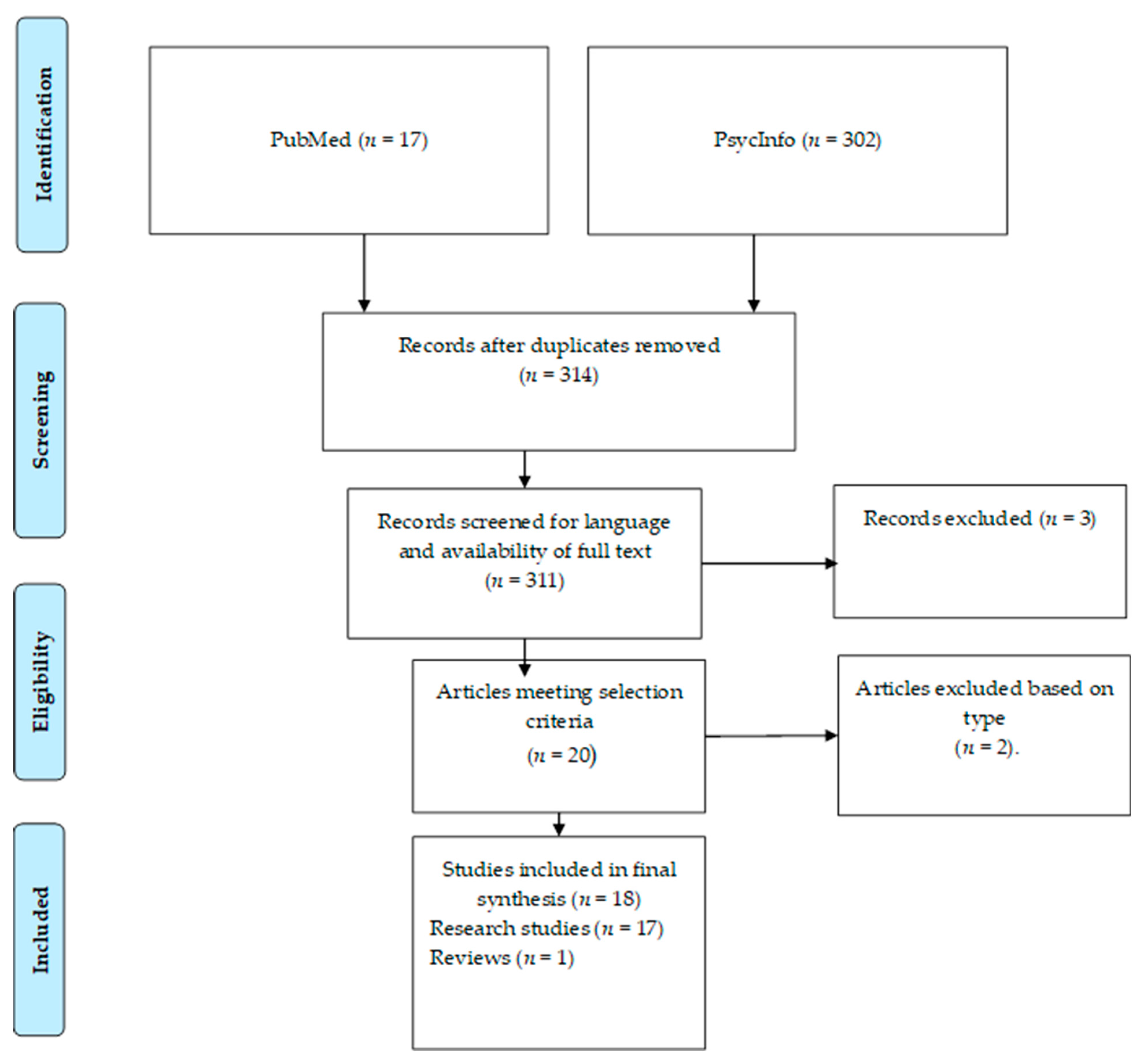
2. Method
3. Results
3.1. Participants
3.2. Measures
3.3. Findings of the Studies of Non-Clinical Populations
3.4. Findings in the Studies of Clinical Populations
4. Discussion
4.1. Limitations
4.2. Future Research Directions
4.3. Implications in clinical practice
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pignatelli, A.M.; Wampers, M.; Loriedo, C.; Biondi, M.; Vanderlinden, J. Childhood neglect in eating disorders: A systematic review and meta-analysis. J. Trauma Dissociation 2017, 18, 100–115. [Google Scholar] [CrossRef] [PubMed]
- Vidaña, A.G.; Forbush, K.T.; Barnhart, E.L.; Mildrum Chana, S.; Chapa, D.A.N.; Richson, B.; Thomeczek, M.L. Impact of trauma in childhood and adulthood on eating-disorder symptoms. Eat. Behav. 2020, 39, 101426. [Google Scholar] [CrossRef] [PubMed]
- Backhlom, K.; Isomaa, R.; Birgegard, A. The prevalence and impact of trauma history in eating disorders patients. Eur. J. Psychotraumatol. 2013, 4, 1–8. [Google Scholar] [CrossRef]
- Caslini, M.; Bartoli, F.; Crocamo, C.; Dakanalis, A.; Clerici, M.; Carrà, G. Disentangling the association between child abuse and eating disorders: A systematic review and meta-analysis. Psychosom. Med. 2016, 78, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Palmisano, G.L.; Innamorati, M.; Vanderlinden, J. Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. J. Behav. Addict. 2016, 5, 11–31. [Google Scholar] [CrossRef] [PubMed]
- Palmisano, G.L.; Innamorati, M.; Susca, G.; Traetta, D.; Sarracino, D.; Vanderlinden, J. Childhood traumatic experiences and dissociative phenomena in eating disorders: Level and dissociation with the severity of binge eating symptoms. J. Trauma Dissociation 2017, 10, 1–20. [Google Scholar] [CrossRef]
- Smolak, L.; Murnen, S. A meta-analytic examination of the relationship between child sexual abuse and eating disorders. Int. J. Eat. Disord. 2002, 31, 136–150. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Claes, L.; De Cuyper, K.; Vrieze, E. Dissociation and dissociative disorders. In Encyclopedia of Feeding and Eating Disorders; Wade, T., Ed.; Springer: Singapore, 2015. [Google Scholar]
- Racine, S.E.; Wildes, J.E. Emotion dysregulation and anorexia nervosa: An exploration of the role of childhood abuse. Int. J. Eat. Disord. 2015, 48, 55–58. [Google Scholar] [CrossRef]
- Everill, J.T.; Waller, G. Reported sexual abuse and eating psychopathology: A review of the evidence for a causal link. Int. J. Eat. Disord. 1995, 18, 1–11. [Google Scholar] [CrossRef]
- Dunkley, D.M.; Masheb, R.M.; Grilo, C.M. Childhood maltreatment, depressive symptoms, and body dissatisfaction in patients with binge eating disorder: The mediating role of self-criticism. Int. J. Eat. Disord. 2010, 43, 274–281. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Vanderreycken, W.; Van Dyck, R.; Vertommen, H. Dissociative experiences and trauma in eating disorders. Int. J. Eat. Disord. 1993, 13, 187–193. [Google Scholar] [CrossRef]
- Fuller-Tyszkiewicz, M.; Mussap, A.J. The relationship between dissociation and binge eating. J. Trauma Dissociation 2008, 9, 445–462. [Google Scholar] [CrossRef]
- Scheffers, M.; Hoek, M.; Bosscher, R.J.; Van Duijin, M.A.J.; Schoevers, R.A.; Van Busschbach, J.T. Negative body experience in women with early childhood trauma: Associations with trauma severity and dissociation. Eur. J. Psychotraumatol. 2017, 8, 1322892. [Google Scholar] [CrossRef] [PubMed]
- Moulton, S.J.; Newman, E.; Power, K.; Swanson, V.; Day, K. Childhood trauma and eating psychopathology: A mediating role for dissociation and emotion dysregulation. Child. Abuse Negl. 2015, 39, 167–174. [Google Scholar] [CrossRef]
- Ordoñez-Camblor, N.; Fonseca-Pedrero, E.; Paino, M.; García-Álvarez, L.; Pizarro-Ruiz, J.P.; Lemos-Giráldez, S. Evaluación de experiencias traumáticas tempranas en adultos. Pap. Psicol. 2016, 37, 36–44. [Google Scholar]
- Kent, A.; Waller, G. Childhood emotional abuse and eating pathology. Clin. Psychol Rev. 2000, 20, 887–903. [Google Scholar] [CrossRef]
- Moher, D.; Linerati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders; American Psychiatric Association: Washington, DC, USA, 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders; American Psychiatric Association: Washington, DC, USA, 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5TM); American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Kent, A.; Waller, G.; Dagnan, D. A greater role of emotional than physical or sexual abuse in predicting disordered eating attitudes: The role of mediating variables. Int. J. Abuse Eat. 1999, 25, 159–167. [Google Scholar] [CrossRef]
- Waller, G.; Ohaian, V.; Meyer, C.; Everill, J.; Rouse, H. The utility of dimensional and categorical approaches to understanding dissociation in the eating disorders. Br. J. Clin. Psychol. 2001, 40, 387–398. [Google Scholar] [CrossRef]
- Waller, G.; Meyer, C.; Ohanian, V.; Elliot, P.; Dickson, C.; Sellings, J. The psychopathology of bulimic women who report childhood sexual abuse: The mediating role of core beliefs. J. Nerv. Ment. Dis. 2001, 189, 700–708. [Google Scholar] [CrossRef]
- Hund, A.; Espelage, D.L. Childhood sexual abuse, disordered eating, alexithymia and general distress: A mediation model. J. Couns Psychol. 2005, 52, 559–573. [Google Scholar] [CrossRef]
- Preti, A.; Incani, I.; Camboni, M.V.; Petretto, D.R.; Marsala, C. Sexual abuse and eating disorders symptoms: The mediator role of bodily dissatisfaction. Compr. Psychiatry 2006, 47, 475–481. [Google Scholar] [CrossRef]
- Kong, S.; Bernstein, K. Childhood trauma as a predictor of eating psychopathology and its mediating variables in patients with eating disorders. J. Clin. Nurs. 2009, 18, 1897–1907. [Google Scholar] [CrossRef]
- Hopwood, C.; Ansell, E.B.; Fehon, D.C.; Grilo, C.M. The mediational significance of negative/depressive affect in the relationship of childhood maltreatment and eating disorder features in adolescent psychiatric inpatients. Eat. Weight Disord. 2011, 16, 9–16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mills, P.; Newman, E.F.; Cossar, J.; Murray, G. Emotional maltreatment and disordered eating in adolescents: Testing the mediating role of emotion regulation. Child. Abuse Negl. 2015, 39, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Feinson, M.C.; Hornik-Lurie, T. “Not good enough” Exploring self-criticism’s role as mediator between childhood emotional abuse & adult binge eating. Eat. Behav. 2016, 23, 1–6. [Google Scholar]
- Feinson, M.C.; Hornik-Lurie, T. Binge eating & childhood emotional abuse: A mediating role for anger. Appetite 2016, 105, 487–493. [Google Scholar]
- Minnich, A.M.; Gordon, K.H.; Kwan, M.Y.; Troop-Gordon, W. Examining the mediating role of alexithymia in the association between childhood neglect and disordered eating behaviors in men and women. Psychol. Men Masc. 2017, 18, 414–421. [Google Scholar] [CrossRef]
- Malinauskiene, V.; Malinauskas, R. Lifetime traumatic experiences and disorders eating among university students: The role of posttraumatic stress symptoms. BioMed Res. Int. 2018, 9814358. [Google Scholar]
- Monteleone, A.M.; Cascino, G.; Pellegrino, F.; Ruzzi, V.; Patriciello, G.; Marone, L.; De Felice, G.; Monteleone, P.; Maj, M. The association between childhood maltreatment and eating disorder psychopathology: A mixed-model investigation. Eur. Psychiatry 2019, 61, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Khalil, R.B.; Sleilaty, G.; Richa, S.; Seneque, M.; Iceta, S.; Rodgers, R.; Alacreu-Crespo, A.; Maimoun, L.; Lefebvre, P.; Renard, E.; et al. The Impact of Retrospective Childhood Maltreatment on Eating Disorders as Mediated by Food Addiction: A Cross-Sectional Study. Nutrients 2020, 28, 2969. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, D.P.; Stein, J.A.; Newcomb, M.D.; Walker, E.; Pogge, D.; Ahluvalia, T.; Zule, W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child. Abuse Negl. 2003, 27, 1205–1222. [Google Scholar] [CrossRef]
- Sanders, B.; Becker-Lausen, B. The measurement of psychological maltreatment: Early data on the Child Abuse and Trauma Scale. Child. Abuse Negl. 1995, 19, 315–323. [Google Scholar] [CrossRef]
- Carlson, E.B.; Putnam, M.D. An update on the Dissociative Experiences Scale. Dissociation Prog. Dissociative Disord. 1993, 6, 16–25. [Google Scholar]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Philips, K.F.V.; Power, M.J. A new self-report measure of emotion regulation in adolescents: The Regulation of Emotions Questionnaire. Clin. Psychol. Psychother. 2007, 14, 145–156. [Google Scholar] [CrossRef]
- Rosenberg, M. Conceiving the Self; Basic Books: New York, NY, USA, 1979. [Google Scholar]
- Beck, A.T.; Steer, R. Manual for the Revised Beck Depression Inventory; Psychological Corporation: San Antonio, TX, USA, 1987. [Google Scholar]
- Beck, A.T.; Steer, R.; Gabin, M.G. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Spielberger, C.D. STAI: Manual for the State-Trait. Anxiety Inventory; Consulting Psychology Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 61, 361–370. [Google Scholar] [CrossRef]
- Derrogatis, L.R. BSI: Administration, Scoring, and Procedures Manual for the Brief Symptoms Imventory, 3rd ed.; National Computer Systems: Minneapolis, MN, USA, 1993. [Google Scholar]
- Bagby, R.M.; Parker, J.D.A.; Taylor, G.J. The twenty- item Toronto Alexithymia Scale-1: Item selection and cross- validation of the factor structure. J. Psychosom. Res. 1994, 38, 23–32. [Google Scholar] [CrossRef]
- Probst, M.; Vandereycken, W.; VanCoppellone, H.; Vanderlinden, J. The body attitude test for patients with an eating disorder: Psychometric characteristics of a new questionnaire. Eat. Disord. J. Treat. Prev. 1995, 3, 133–144. [Google Scholar] [CrossRef]
- Cooper, P.J.; Taylor, M.J.; Cooper, Z.; Fairburn, C.G. The development and validation of the Body Shape Questionnaire. Int. J. Eat. Disord. 1987, 6, 485–494. [Google Scholar] [CrossRef]
- Weis, D.S. The Impact of Event Scale Revised. In Assessing Psychological Trauma and PTSD; Wilson, P.J., Keane, T.M., Eds.; Guildford Press: New York, NY, USA, 2004; pp. 168–189. [Google Scholar]
- Young, J.E. Cognitive Therapy for Personality Disorders: A Schema-Focused Approach, 3rd ed.; Professional Resource Press: Sarasota, FL, USA, 1999. [Google Scholar]
- Rabito-Alcón, M.F.; Baile, J.I.; Vanderlinden, J. Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study. Children 2020, 5, 274. [Google Scholar] [CrossRef] [PubMed]
| First Author and Years of Publication | Country | Sample | ED Diagnosis in Clinical Population Studies | Mediators | Questionnaires Used to Assess Mediators |
|---|---|---|---|---|---|
| Kent, 1999 [24] | UK | 236 adults NCS | - | Anxiety and dissociation | DES and HADS |
| Waller, 2001 [25] | UK | 170 adults CS and 203 adults NCS | Bulimia nervosa, anorexia nervosa, and binge eating disorder | Dissociation | DES II |
| Waller 2001 [26] | 61 adults CS | Bulimia nervosa, anorexia nervosa, and binge eating disorder | Dissociation, core beliefs, and depressive symptomatology | DES II, YSQ, and BDI | |
| Hund, 2005 [27] | USA | 608 adults NCS | - | General distress and alexithymia | STAI and TAS-20 |
| Preti, 2006 [28] | Italy | 126 adults NCS | - | Body dissatisfaction | BAT |
| Kong, 2009 [29] | South Korea | 73 adolescents and adults CS | Anorexia nervosa, bulimia nervosa, and eating disorder not otherwise specified | Depressive symptomatology | BDI |
| Dunkley, 2010 [11] | USA | 170 adults CS | Binge eating disorder | Self-criticism and body dissatisfaction | RSES and BSQ |
| Hopwood, 2011 [30] | USA | 148 adolescents CS | Not specified but including EDs | Depressive symptomatology | BDI |
| Mills, 2015 [31] | UK | 222 adolescents NCS | - | Difficulties regulating emotions | REQ |
| Moulton, 2015 [15] | UK | 142 adults NCS | - | Difficulties regulating emotions and dissociation | DERS and DES II |
| Racine, 2015 [9] | USA | 188 adolescent and adults CS | Anorexia nervosa | Difficulties regulating emotions | DERS |
| Feinson, 2016 [32] | Israel | 498 adults NCS | - | Self-criticism, anxiety, and depressive symptomatology | RSES and BSQ |
| Feinson, 2016 [33] | Israel | 476 adults NCS | - | Self-criticism, anger, anxiety, and depressive symptomatology | RSES and BSQ |
| Minnich, 2017 [34] | USA | 1344 adults NCS | Alexithymia | TAS-20 | |
| Malinauskiene, 2018 [35] | Lithuania | 614 adults NCS | Symptoms of post-traumatic stress | IES-R | |
| Monteleone, 2019 [36] | Italy | 228 adults CS | Anorexia nervosa restricting type and anorexia nervosa binge-purging type | Interoceptive awareness and inefficiency | STAI and EDI-2 |
| Khalil, 2020 [37] | France | 231 adults CS | Anorexia nervosa, bulimia nervosa, binge eating disorder, and other types of eating disorders | Food addiction | YFAS 2.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabito-Alcón, M.F.; Baile, J.I.; Vanderlinden, J. Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review. Children 2021, 8, 114. https://doi.org/10.3390/children8020114
Rabito-Alcón MF, Baile JI, Vanderlinden J. Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review. Children. 2021; 8(2):114. https://doi.org/10.3390/children8020114
Chicago/Turabian StyleRabito-Alcón, María F., José I. Baile, and Johan Vanderlinden. 2021. "Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review" Children 8, no. 2: 114. https://doi.org/10.3390/children8020114
APA StyleRabito-Alcón, M. F., Baile, J. I., & Vanderlinden, J. (2021). Mediating Factors between Childhood Traumatic Experiences and Eating Disorders Development: A Systematic Review. Children, 8(2), 114. https://doi.org/10.3390/children8020114







