Pain Symptomatology and Management in Pediatric Ehlers–Danlos Syndrome: A Review
Abstract
1. Introduction
2. Pain Characteristics
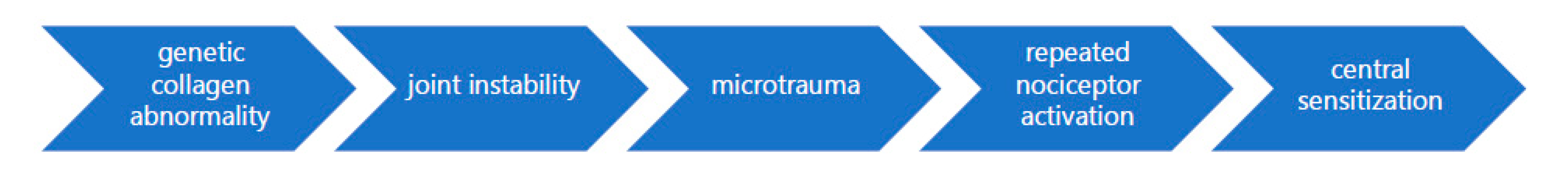
2.1. Etiology of Pain
2.2. Pain Intensity and Extent
2.3. Sites of Pain: Musculoskeletal
2.4. Sites of Pain: Non-Musculoskeletal
3. Pain Management Interventions
3.1. Interventions for Musculoskeletal Pain
3.2. Interventions for Non-Musculoskeletal Pain
4. Pain and Quality of Life in Pediatric EDS
5. Limitations of Research and Recommended Future Directions
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Beighton, P.; Paepe, A.D.; Steinmann, B.; Tsipouras, P.; Wenstrup, R.J. Ehlers-Danlos syndromes: Revised nosology, Villefranche, 1997. Am. J. Med. Genet. 1998, 77, 31–37. [Google Scholar] [CrossRef]
- Tinkle, B.; Castori, M.; Berglund, B.; Cohen, H.; Grahame, R.; Kazkaz, H.; Levy, H. Hypermobile Ehlers–Danlos syndrome (aka Ehlers–Danlos syndrome Type III and Ehlers–Danlos syndrome hypermobility type): Clinical description and natural history. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 48–69. [Google Scholar] [CrossRef]
- Voermans, N.C.; Knoop, H.; Bleijenberg, G.; van Engelen, B.G. Pain in Ehlers-Danlos syndrome is common, severe, and associated with functional impairment. J. Pain Symptom Manag. 2010, 40, 370–378. [Google Scholar] [CrossRef]
- Brady, A.F.; Demirdas, S.; Fournel-Gigleux, S.; Ghali, N.; Giunta, C.; Kapferer-Seebacher, I.; Kosho, T.; Mendoza-Londono, R.; Pope, M.F.; Rohrbach, M.; et al. The Ehlers–Danlos syndromes, rare types. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 70–115. [Google Scholar] [CrossRef]
- Castori, M.; Camerota, F.; Celletti, C.; Grammatico, P.; Padua, L. Ehlers–Danlos syndrome hypermobility type and the excess of affected females: Possible mechanisms and perspectives. Am. J. Med. Genet. A 2010, 152, 2406–2408. [Google Scholar] [CrossRef] [PubMed]
- Rombaut, L.; Malfait, F.; De Wandele, I.; Taes, Y.; Thijs, Y.; De Paepe, A.; Calders, P. Muscle mass, muscle strength, functional performance, and physical impairment in women with the hypermobility type of Ehlers-Danlos syndrome. Arthritis Care Res. 2012, 64, 1584–1592. [Google Scholar] [CrossRef] [PubMed]
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 international classification of the Ehlers–Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Chopra, P.; Tinkle, B.; Hamonet, C.; Brock, I.; Gompel, A.; Bulbena, A.; Francomano, C. Pain management in the Ehlers–Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Sacheti, A.; Szemere, J.; Bernstein, B.; Tafas, T.; Schechter, N.; Tsipouras, P. Chronic pain is a manifestation of the Ehlers-Danlos syndrome. J. Pain Symptom Manag. 1997, 14, 88–93. [Google Scholar] [CrossRef]
- Molander, P.; Novo, M.; Hållstam, A.; Löfgren, M.; Stålnacke, B.M.; Gerdle, B. Ehlers–Danlos Syndrome and Hypermobility Syndrome Compared with Other Common Chronic Pain Diagnoses—A Study from the Swedish Quality Registry for Pain Rehabilitation. J. Clin. Med. 2020, 9, 2143. [Google Scholar] [CrossRef]
- Lumley, M.A.; Jordan, M.; Rubenstein, R.; Tsipouras, P.; Evans, M.I. Psychosocial functioning in the Ehlers-Danlos syndrome. Am. J. Med. Genet. 1994, 53, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Baeza-Velasco, C.; Bulbena, A.; Polanco-Carrasco, R.; Jaussaud, R. Cognitive, emotional, and behavioral considerations for chronic pain management in the Ehlers–Danlos syndrome hypermobility-type: A narrative review. Disabil. Rehabil. 2019, 41, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Kobets, A.J.; Komlos, D.; Houten, J.K. Congenital cervical kyphosis in an infant with Ehlers-Danlos syndrome. Childs Nerv. Syst. 2018, 34, 1411–1415. [Google Scholar] [CrossRef] [PubMed]
- Castori, M.; Sperduti, I.; Celletti, C.; Camerota, F.; Grammatico, P. Symptom and joint mobility progression in the joint hypermobility syndrome (Ehlers-Danlos syndrome, hypermobility type). Clin. Exp. Rheumatol. 2011, 29, 998–1005. [Google Scholar]
- Adib, N.; Davies, K.; Grahame, R.; Woo, P.; Murray, K.J. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology 2005, 44, 744–750. [Google Scholar] [CrossRef]
- Holley, A.L.; Fussner, L.; Wilson, A.; Palermo, T. (261) Using the pediatric pain screening tool to predict longitudinal pain outcomes in treatment seeking youth with acute musculoskeletal pain. J. Pain 2017, 18, S41. [Google Scholar] [CrossRef]
- Pacey, V.; Adams, R.D.; Tofts, L.; Munns, C.F.; Nicholson, L.L. Joint hypermobility syndrome subclassification in paediatrics: A factor analytic approach. Arch. Dis. Child. 2015, 100, 8–13. [Google Scholar] [CrossRef]
- Scheper, M.C.; Nicholson, L.L.; Adams, R.D.; Tofts, L.; Pacey, V. The natural history of children with joint hypermobility syndrome and Ehlers–Danlos hypermobility type: A longitudinal cohort study. Rheumatology 2017, 56, 2073–2083. [Google Scholar] [CrossRef]
- Morlino, S.; Dordoni, C.; Sperduti, I.; Venturini, M.; Celletti, C.; Camerota, F.; Colombi, M.; Castori, M. Refining patterns of joint hypermobility, habitus, and orthopedic traits in joint hypermobility syndrome and Ehlers–Danlos syndrome, hypermobility type. Am. J. Med. Genet. A 2017, 173, 914–929. [Google Scholar] [CrossRef]
- Kumar, B.; Lenert, P. Joint hypermobility syndrome: Recognizing a commonly overlooked cause of chronic pain. Am. J. Med. 2017, 130, 640–647. [Google Scholar] [CrossRef]
- Schubert-Hjalmarsson, E.; Öhman, A.; Kyllerman, M.; Beckung, E. Pain, balance, activity, and participation in children with hypermobility syndrome. Pediatr. Phys. Ther. 2012, 24, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Castori, M.; Morlino, S.; Celletti, C.; Celli, M.; Morrone, A.; Colombi, M.; Camerota, F.; Grammatico, P. Management of pain and fatigue in the joint hypermobility syndrome (aka Ehlers–Danlos syndrome, hypermobility type): Principles and proposal for a multidisciplinary approach. Am. J. Med. Genet. A 2012, 158, 2055–2070. [Google Scholar] [CrossRef] [PubMed]
- Gedalia, A.; Brewer, E.J., Jr. Joint hypermobility in pediatric practice—A review. J. Rheumatol. 1993, 20, 371–374. [Google Scholar] [PubMed]
- Fatoye, F.; Palmer, S.; Macmillan, F.; Rowe, P.; van der Linden, M. Proprioception and muscle torque deficits in children with hypermobility syndrome. Rheumatology 2009, 48, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Pacey, V.; Tofts, L.; Adams, R.D.; Munns, C.F.; Nicholson, L.L. Exercise in children with joint hypermobility syndrome and knee pain: A randomised controlled trial comparing exercise into hypermobile versus neutral knee extension. Pediatr. Rheumatol. 2013, 11, 30. [Google Scholar] [CrossRef]
- Cheung, J.P.Y.; Fung, B.K.; Mak, K.C.; Leung, K.H. Multiple triggering in a girl with Ehlers-Danlos syndrome: Case report. J. Hand. Surg. Am. 2010, 35, 1675–1677. [Google Scholar] [CrossRef]
- Duong, L.; Flores, M. The Effects of Closed Kinetic Chain and Endurance Exercises on Reducing Pain in a Child with Ehlers-Danlos Syndrome: A Case Report. In Proceedings of the American Physical Therapy Association (APTA) Combined Sections Meeting, San Antonio, TX, USA, 15 February 2017. [Google Scholar]
- Castori, M.; Hakim, A. Contemporary approach to joint hypermobility and related disorders. Curr. Opin. Pediatr. 2017, 29, 640–649. [Google Scholar] [CrossRef]
- Ferrell, W.R.; Tennant, N.; Sturrock, R.D.; Ashton, L.; Creed, G.; Brydson, G.; Rafferty, D. Amelioration of symptoms by enhancement of proprioception in patients with joint hypermobility syndrome. Arthritis Rheum. J. Am. Coll. Rheumatol. 2004, 50, 3323–3328. [Google Scholar] [CrossRef]
- Rombaut, L.; Scheper, M.; De Wandele, I.; De Vries, J.; Meeus, M.; Malfait, F.; Engelbert, R.; Calders, P. Chronic pain in patients with the hypermobility type of Ehlers–Danlos syndrome: Evidence for generalized hyperalgesia. Clin. Rheumatol. 2015, 34, 1121–1129. [Google Scholar] [CrossRef]
- Ashmawi, H.A.; Freire, G.M.G. Peripheral and central sensitization. Rev Dor. 2016, 17, 31–34. [Google Scholar] [CrossRef]
- Walker, S.M.; Beggs, S.; Baccei, M.L. Persistent changes in peripheral and spinal nociceptive processing after early tissue injury. Exp. Neurol. 2016, 275, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.T.; Jagpal, A.; Koven, M.L.; Turek, C.E.; Golden, J.S.; Tinkle, B.T. Symptom complaints and impact on functioning in youth with hypermobile Ehlers–Danlos syndrome. J. Child Health Care 2019. [Google Scholar] [CrossRef] [PubMed]
- Castarlenas, E.; Jensen, M.P.; von Baeyer, C.L.; Miró, J. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents. Clin. J. Pain 2017, 33, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Egloff, N.; Häuser, W. Widespread pain and low widespread pain index scores among fibromyalgia-positive cases assessed with the 2010/2011 fibromyalgia criteria. J. Rheumatol. 2016, 43, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.M.; Pepin, M.J.; Stoler, J.M.; Kramer, D.E.; Spencer, S.A.; Stein, C.J. Musculoskeletal conditions in a pediatric population with Ehlers-Danlos syndrome. J. Pediatr. 2017, 181, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Mato, H.; Berde, T.; Hasson, N.; Grahame, R.; Maillard, S. A review of symptoms associated with Benign Joint Hypermobility Syndrome in children. Pediatr. Rheumatol. 2008, 6, 155. [Google Scholar] [CrossRef][Green Version]
- Walter, S.M. Case report: Ehlers-Danlos syndrome in an adolescent presenting with chronic daily headache. Surg. Neurol. Int. 2014, 5, 475. [Google Scholar] [CrossRef]
- Brown, S.C.; Stinson, J. Treatment of pediatric chronic pain with tramadol hydrochloride: Siblings with Ehlers-Danlos syndrome-Hypermobility type. Pain Res. Manag. 2004, 9, 209–211. [Google Scholar] [CrossRef]
- Moore, J.R.; Tolo, V.T.; Weiland, A.J. Painful subluxation of the carpometacarpal joint of the thumb in Ehlers-Danlos syndrome. J. Hand Surg. 1985, 10, 661–663. [Google Scholar] [CrossRef]
- Breahna, A.N.; Meads, B.M. Thumb Carpometacarpal Joint Stabilization in Ehlers-Danlos Syndrome-Case Report. Hand Surg. 2015, 20, 463–465. [Google Scholar] [CrossRef]
- Savasta, S.; Crispino, M.; Valli, M.; Calligaro, A.; Zambelloni, C.; Poggiani, C. Subependymal periventricular heterotopias in a patient with Ehlers-Danlos syndrome: A new case. J. Child Neurol. 2007, 22, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Hugon-Rodin, J.; Lebègue, G.; Becourt, S.; Hamonet, C.; Gompel, A. Gynecologic symptoms and the influence on reproductive life in 386 women with hypermobility type Ehlers-Danlos syndrome: A cohort study. Orphanet J. Rare Dis. 2016, 11, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Hurst, B.S.; Lange, S.S.; Kullstam, S.M.; Usadi, R.S.; Matthews, M.L.; Marshburn, P.B.; Templin, M.A.; Merriam, K.S. Obstetric and gynecologic challenges in women with Ehlers-Danlos syndrome. Obstet. Gynecol. 2014, 123, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Kahana, M.; Levy, A.; Ronnen, M.; Cohen, M.; Schewach-Millet, M. Painful Piezogenic Pedal Papules on a Child with Ehlers-Danlos Syndrome. Pediatr. Dermatol. 1985, 3, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Poppe, H.; Hamm, H. Piezogenic papules in Ehlers-Danlos syndrome. J. Pediatr. 2013, 163, 1788. [Google Scholar] [CrossRef] [PubMed]
- Moscoso, G. Congenital structural defects in the brain. In Fetal and Neonatal Neurology and Neurosurgery, 4th ed.; Levene, M.I., Chervenak, F.A., Eds.; Elsevier Health Sciences: Philadelphia, PA, USA, 2009; pp. 246–247. [Google Scholar]
- Jacome, D.E. Headache in Ehlers–Danlos syndrome. Cephalalgia 1999, 19, 791–796. [Google Scholar] [CrossRef]
- Reinstein, E.; Pariani, M.; Bannykh, S.; Rimoin, D.L.; Schievink, W.I. Connective tissue spectrum abnormalities associated with spontaneous cerebrospinal fluid leaks: A prospective study. Eur. J. Hum. Genet. 2013, 21, 386–390. [Google Scholar] [CrossRef]
- Fikree, A.; Chelimsky, G.; Collins, H.; Kovacic, K.; Aziz, Q. Gastrointestinal involvement in the Ehlers–Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 181–187. [Google Scholar] [CrossRef]
- Kovacic, K.; Chelimsky, T.C.; Sood, M.R.; Simpson, P.; Nugent, M.; Chelimsky, G. Joint hypermobility: A common association with complex functional gastrointestinal disorders. J. Pediatr. 2014, 165, 973–978. [Google Scholar] [CrossRef]
- Beighton, P.H.; Murdoch, J.L.; Votteler, T. Gastrointestinal complications of the Ehlers-Danlos syndrome. Gut 1969, 10, 1004–1008. [Google Scholar] [CrossRef]
- Hakim, A.J.; Grahame, R. Non-musculoskeletal symptoms in joint hypermobility syndrome. Indirect evidence for autonomic dysfunction? Rheumatology 2004, 43, 1194–1195. [Google Scholar] [CrossRef] [PubMed]
- Gazit, Y.; Nahir, A.M.; Grahame, R.; Jacob, G. Dysautonomia in the joint hypermobility syndrome. Am. J. Med. 2003, 115, 33–40. [Google Scholar] [CrossRef]
- Castori, M.; Camerota, F.; Celletti, C.; Danese, C.; Santilli, V.; Saraceni, V.M.; Grammatico, P. Natural history and manifestations of the hypermobility type Ehlers–Danlos syndrome: A pilot study on 21 patients. Am. J. Med. Genet. A 2010, 152, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.D.; Mouchli, M.A.; Valentin, N.; Deyle, D.; Pichurin, P.; Acosta, A.; Camilleri, M. Ehlers Danlos syndrome and gastrointestinal manifestations: A 20-year experience at Mayo Clinic. J. Neurogastroenterol. Motil. 2015, 27, 1657–1666. [Google Scholar] [CrossRef]
- Inayet, N.; Hayat, J.O.; Kaul, A.; Tome, M.; Child, A.; Poullis, A. Gastrointestinal symptoms in Marfan syndrome and hypermobile Ehlers-Danlos syndrome. Gastroenterol. Res. Pract. 2018. [Google Scholar] [CrossRef]
- Solomon, J.A.; Abrams, L.; Lichtenstein, G.R. GI manifestations of Ehlers-Danlos syndrome. Am. J. Gastroenterol. 1996, 91, 2282–2288. [Google Scholar]
- Davis, A.R.; Westhoff, C.L. Primary dysmenorrhea in adolescent girls and treatment with oral contraceptives. J. Pediatr. Adolesc. Gynecol. 2001, 14, 3–8. [Google Scholar] [CrossRef]
- Gilliam, E.; Hoffman, J.D.; Yeh, G. Urogenital and pelvic complications in the Ehlers-Danlos syndromes and associated hypermobility spectrum disorders: A scoping review. Clin. Genet. 2020, 97, 168–178. [Google Scholar] [CrossRef]
- Kahana, M.; Feinstein, A.; Tabachnic, E.; Schewach-Millet, M.; Engelberg, S. Painful piezogenic pedal papules in patients with Ehlers-Danlos syndrome. J. Am. Acad. Dermatol. 1987, 17, 205–209. [Google Scholar] [CrossRef]
- Van Straaten, E.A.; Van Langen, I.M.; Oorthuys, J.W.E.; Oosting, J. Piezogenic papules of the feet in healthy children and their possible relation with connective tissue disorders. Pediatr. Dermatol. 1991, 8, 277–279. [Google Scholar] [CrossRef]
- Henderson, F.C., Sr.; Austin, C.; Benzel, E.; Bolognese, P.; Ellenbogen, R.; Francomano, C.A.; Patel, S. Neurological and spinal manifestations of the Ehlers–Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 195–211. [Google Scholar] [CrossRef] [PubMed]
- Bonamichi-Santos, R.; Yoshimi-Kanamori, K.; Giavina-Bianchi, P.; Aun, M.V. Association of postural tachycardia syndrome and Ehlers-Danlos syndrome with mast cell activation disorders. Immuno. Allerg. Clin. 2018, 38, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.; Rosenfeld, W.; Ferguson, L.; Maitland, A.; Bolognese, P. Chiari malformation (CM) and/or tethered cord, idiopathic mast cell activation syndrome (MCAS), Ehlers-Danlos Syndrome (EDS), and Postural Orthostatic Tachycardia syndrome (POTS): A new pediatric disease cluster. Pediatrics 2019. [Google Scholar] [CrossRef]
- Murray, K.J. Hypermobility disorders in children and adolescents. Best Pract. Res. Clin. Rheumatol. 2006, 20, 329–351. [Google Scholar] [CrossRef]
- Kemp, S.; Roberts, I.; Gamble, C.; Wilkinson, S.; Davidson, J.E.; Baildam, E.M.; Cleary, A.G.; McCann, L.J.; Beresford, M.W. A randomized comparative trial of generalized vs targeted physiotherapy in the management of childhood hypermobility. Rheumatology 2010, 49, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.B.; Finkel, J.C.; Arquedas-Mohs, A.; Himelstein, B.P.; Schreiner, M.; Medve, R.A. Oral tramadol for the treatment of pain of 7–30 days’ duration in children. Anesth. Analg. 2003, 96, 78–81. [Google Scholar] [CrossRef]
- US Food and Drug Administration. FDA Drug Safety Communication: FDA Evaluating the Risks of Using the Pain Medicine Tramadol in Children Aged 17 and Younger. 2015; Volume 21. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-evaluating-risks-using-pain-medicine-tramadol-children-aged-17-and (accessed on 10 September 2020).
- Frohlich, L.; Wesley, A.; Wallen, M.; Bundy, A. Effects of neoprene wrist/hand splints on handwriting for students with joint hypermobility syndrome: A single system design study. Phys. Occup. Ther. Pediatr. 2012, 32, 243–255. [Google Scholar] [CrossRef]
- Seneviratne, S.L.; Maitland, A.; Afrin, L. Mast cell disorders in Ehlers–Danlos syndrome. Am. J. Med. Genet. C Semin Med. Genet. 2017, 175, 226–236. [Google Scholar] [CrossRef]
- Menezes, A.; Ryken, T.; Brockmeyer, D. Abnormalities of the craniocervical junction. In Pediatric Neurosurgery. Surgery of the Developing Nervous System, 4th ed.; McLone, D.G., Ed.; WB Saunders: Philadelphia, PA, USA, 2001; pp. 400–422. [Google Scholar]
- Palsson, O.S.; Whitehead, W.E. Psychological treatments in functional gastrointestinal disorders: A primer for the gastroenterologist. Clin. Gastroenterol. Hepatol. 2013, 11, 208–216. [Google Scholar] [CrossRef]
- Korterink, J.J.; Rutten, J.M.; Venmans, L.; Benninga, M.A.; Tabbers, M.M. Pharmacologic treatment in pediatric functional abdominal pain disorders: A systematic review. J. Pediatr. 2015, 166, 424–431. [Google Scholar] [CrossRef]
- Fikree, A.; Aktar, R.; Grahame, R.; Hakim, A.J.; Morris, J.K.; Knowles, C.H.; Aziz, Q. Functional gastrointestinal disorders are associated with the joint hypermobility syndrome in secondary care: A case-control study. J. Neurogastroenterol. Motil. 2015, 27, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Gompel, A. Les manifestations gynecologiques du syndrome d’Ehlers-Danlos Hypermobile. J. Readapt. Med Prat. Form. Med. Phys. Readapt. 2016, 36, 64–66. [Google Scholar] [CrossRef]
- Doukas, D.J.; Holmes, J.; Leonard, J.A. A nonsurgical approach to painful piezogenic pedal papules. Cutis 2004, 73, 339–340. [Google Scholar] [PubMed]
- Turkmani, M.G. Piezogenic pedal papules treated successfully with deoxycholic acid injection. JAAD Case Rep. 2018, 4, 582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rombaut, L.; Malfait, F.; De Paepe, A.; Rimbaut, S.; Verbruggen, G.; De Wandele, I.; Calders, P. Impairment and impact of pain in female patients with Ehlers-Danlos syndrome: A comparative study with fibromyalgia and rheumatoid arthritis. Arthritis Rheum. 2011, 63, 1979–1987. [Google Scholar] [CrossRef]
- Berglund, B.; Pettersson, C.; Pigg, M.; Kristiansson, P. Self-reported quality of life, anxiety and depression in individuals with Ehlers-Danlos syndrome (EDS): A questionnaire study. BMC Musculoskelet Disord. 2015, 16, 89. [Google Scholar] [CrossRef]
- Gaisl, T.; Giunta, C.; Bratton, D.J.; Sutherland, K.; Schlatzer, C.; Sievi, N.; Franzen, D.; Cistulli, P.A.; Rohrbach, M.; Kohler, M. Obstructive sleep apnoea and quality of life in Ehlers-Danlos syndrome: A parallel cohort study. Thorax 2017, 72, 729–735. [Google Scholar] [CrossRef]
- Scheper, M.C.; de Vries, J.E.; Verbunt, J.; Engelbert, R.H. Chronic pain in hypermobility syndrome and Ehlers–Danlos syndrome (hypermobility type): It is a challenge. J. Pain Res. 2015, 8, 591. [Google Scholar] [CrossRef]
- Mu, W.; Muriello, M.; Clemens, J.L.; Wang, Y.; Smith, C.H.; Tran, P.T.; Rowe, P.C.; Francomano, C.A.; Kline, A.D.; Bodurtha, J. Factors affecting quality of life in children and adolescents with hypermobile Ehlers-Danlos syndrome/hypermobility spectrum disorders. Am. J. Med. Genet. A 2019, 179, 561–569. [Google Scholar] [CrossRef]
- Engelbert, R.H.; van Bergen, M.; Henneken, T.; Helders, P.J.; Takken, T. Exercise tolerance in children and adolescents with musculoskeletal pain in joint hypermobility and joint hypomobility syndrome. Pediatrics 2006, 118, 690–696. [Google Scholar] [CrossRef]
- Eagleton, M.J. Arterial complications of vascular Ehlers-Danlos syndrome. J. Vasc. Surg. 2016, 64, 1869–1880. [Google Scholar] [CrossRef] [PubMed]
- Byers, P.H. Vascular Ehlers-Danlos Syndrome. In GeneReviews® [Internet]; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Eds.; University of Washington: Seattle, WA, USA, 2019; ISSN 2372-0697. [Google Scholar]
- Castori, M.; Dordoni, C.; Valiante, M.; Sperduti, I.; Ritelli, M.; Morlino, S.; Chiarelli, N.; Celletti, C.; Venturini, M.; Camerota, F.; et al. Nosology and inheritance pattern(s) of joint hypermobility syndrome and Ehlers-Danlos syndrome, hypermobility type: A study of intrafamilial and interfamilial variability in 23 Italian pedigrees. Am. J. Med. Genet. A 2014, 164, 3010–3020. [Google Scholar] [CrossRef] [PubMed]
- Malfait, F.; Hakim, A.J.; De Paepe, A.; Grahame, R. The genetic basis of the joint hypermobility syndromes. Rheumatology 2006, 45, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, A.M.C.; Dietrich, J.E. Gynecologic management of pediatric and adolescent patients with Ehlers-Danlos Syndrome. J. Pediatr. Adolesc. Gynecol. 2020, 33, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Hoffman, K.M.; Trawalter, S.; Axt, J.R.; Oliver, M.N. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc. Natl. Acad. Sci. USA 2016, 113, 4296–4301. [Google Scholar] [CrossRef]
- Goyal, M.K.; Kuppermann, N.; Cleary, S.D.; Teach, S.J.; Chamberlain, J.M. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. 2015, 169, 996–1002. [Google Scholar] [CrossRef]
- Meghani, S.H.; Green, C. Disparities in Pain and Pain Care. In Handbook of Pain and Palliative Care; Moore, R., Ed.; Springer International Publishing: Cham, Switzerland, 2018; pp. 821–834. ISBN 978-3-319-95369-4. [Google Scholar]
- Hewes, H.A.; Dai, M.; Mann, N.C.; Baca, T.; Taillac, P. Prehospital pain management: Disparity by age and race. Prehosp. Emerg. Care 2018, 22, 189–197. [Google Scholar] [CrossRef]
- Im, E.O. Ethnic differences in cancer pain experience. Nurs. Res. 2007, 56, 296. [Google Scholar] [CrossRef]
| Site of Pain | Authors | Populations Described |
|---|---|---|
| Musculoskeletal | ||
| Back | Mato et al., 2008 [37]; Stern et al., 2017 [36]; Tran et al., in press [33]; Walter, 2014 [38] | hEDS, JHS, cEDS, vEDS |
| Neck | Mato et al., 2008 [37]; Tran et al., in press [33]; Walter, 2014 [38] | hEDS, JHS, cEDS |
| Shoulders | Brown and Stinson, 2004 [39]; Schubert-Hjalmarsson et al., 2012 [21]; Stern et al., 2017 [36]; Tran et al., in press [33] | hEDS, JHS, cEDS, vEDS, |
| Wrists | Brown and Stinson, 2004 [39]; Mato et al., 2008 [37]; Schubert-Hjalmarsson et al., 2012 [21] | hEDS, JHS |
| Hips | Mato et al., 2008 [37] | JHS |
| Knees | Brown and Stinson, 2004 [39]; Mato et al., 2008 [37]; Schubert-Hjalmarsson et al., 2012 [21]; Stern et al., 2017 [36] | hEDS, JHS, cEDS, vEDS, |
| Feet | Mato et al., 2008 [37]; Schubert-Hjalmarsson et al., 2012 [21] | hEDS, JHS |
| Small joints (toes, fingers) | Brown and Stinson, 2004 [39]; Moore, Tolo and Weiland, 1985 [40] | hEDS |
| Non-Musculoskeletal | ||
| Headaches | Mato et al., 2008 [37]; Savasta et al., 2007 [42]; Tran et al., in press [33]; Walter, 2014 [38] | JHS, cEDS |
| Abdominal Pain | Mato et al., 2008 [37]; Pacey et al., 2015 [17] | hEDS, JHS |
| Dysmenorrhea | Hugon-Rodin et al., 2016 [43]; Hurst et al., 2014 [44] | hEDS, vEDS |
| Painful piezogenic pedal papules | Kahana et al., 1985 [45]; Poppe and Hamm, 2013 [46] | cEDS |
| Quality of Life Correlate | Sample Demographics (N, Illness Group) | Authors and Key Finding |
|---|---|---|
| Emotional Functioning | N = 34, hEDS | Tran et al., in press [33]: Anxiety, R = 0.50, Depression, R = 0.48 |
| School Functioning | N = 54, JHS | Mato et al., 2008 [37]: Only 35% attended school full time |
| Physical Functioning | N = 54, JHS | Mato et al., 2008 [37]: Only 6% of children completed gym class activities |
| N = 32, JHS | Engelbert et al., 2006 [84]: diminished peak maximal oxygen consumption as compared to those without JHS associated pain (Cohen’s d = 0.93) | |
| N = 125, JHS | Adib et al., 2005 [15]: 85% of children note exacerbation of pain with exercise |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feldman, E.C.H.; Hivick, D.P.; Slepian, P.M.; Tran, S.T.; Chopra, P.; Greenley, R.N. Pain Symptomatology and Management in Pediatric Ehlers–Danlos Syndrome: A Review. Children 2020, 7, 146. https://doi.org/10.3390/children7090146
Feldman ECH, Hivick DP, Slepian PM, Tran ST, Chopra P, Greenley RN. Pain Symptomatology and Management in Pediatric Ehlers–Danlos Syndrome: A Review. Children. 2020; 7(9):146. https://doi.org/10.3390/children7090146
Chicago/Turabian StyleFeldman, Estée C. H., Daniel P. Hivick, P. Maxwell Slepian, Susan T. Tran, Pradeep Chopra, and Rachel Neff Greenley. 2020. "Pain Symptomatology and Management in Pediatric Ehlers–Danlos Syndrome: A Review" Children 7, no. 9: 146. https://doi.org/10.3390/children7090146
APA StyleFeldman, E. C. H., Hivick, D. P., Slepian, P. M., Tran, S. T., Chopra, P., & Greenley, R. N. (2020). Pain Symptomatology and Management in Pediatric Ehlers–Danlos Syndrome: A Review. Children, 7(9), 146. https://doi.org/10.3390/children7090146





