Culinary Education Programs for Children in Low-Income Households: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Data Sources
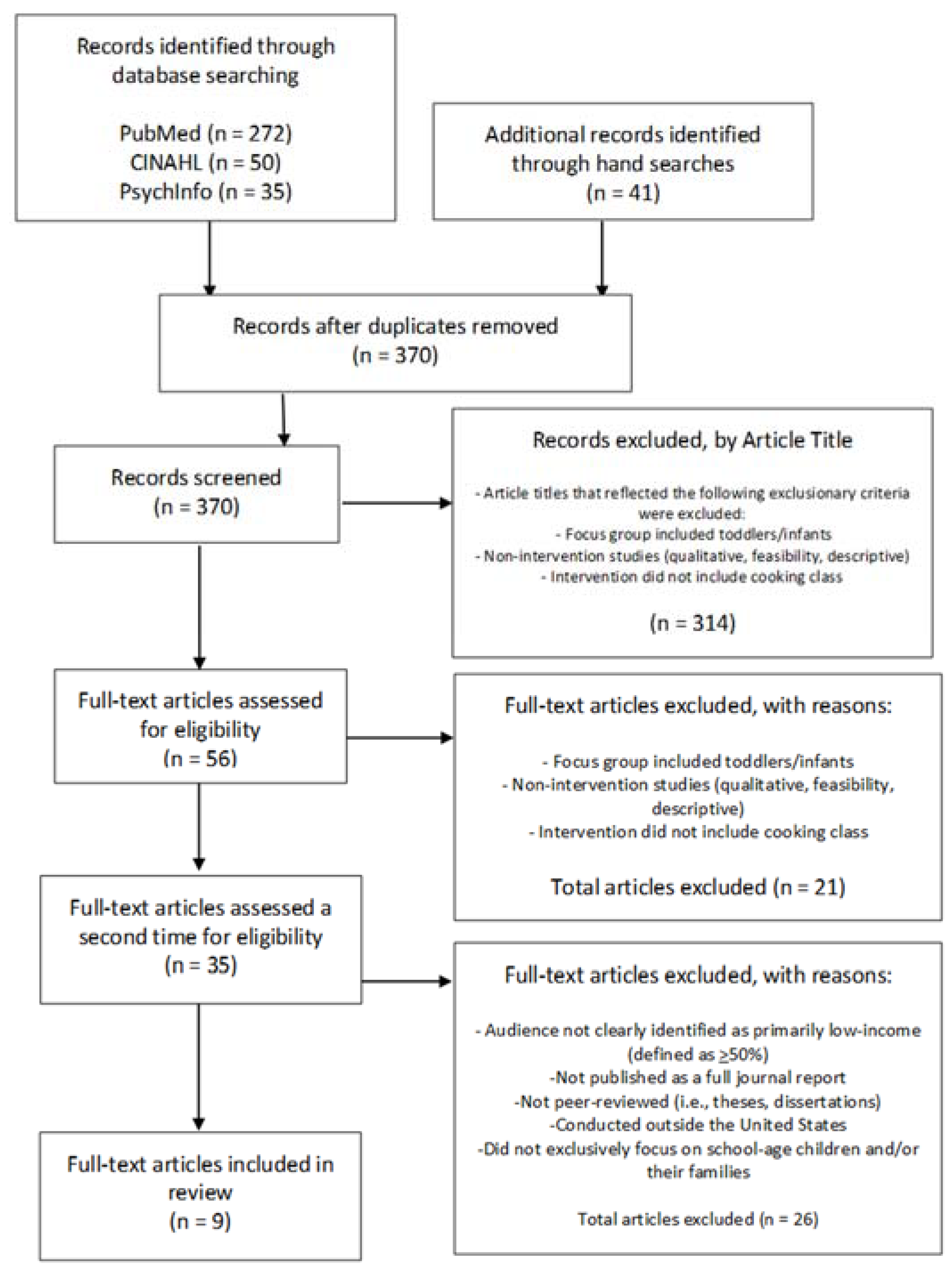
2.2. Study Selection
2.3. Data Extraction
3. Results
4. Discussion
5. Conclusions
6. Implications for Research and Practice
Author Contributions
Funding
Conflicts of Interest
References
- Fryar, C.D.; Carroll, M.D.; Ogden, C.L. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2015–2016. Available online: https://www.cdc.gov/nchs/data/hestat/obesity_child_15_16/obesity_child_15_16.htm (accessed on 13 January 2020).
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017, 2017, 1–8. [Google Scholar]
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of obesity among youths by household income and education level of head of household-United States 2011–2014. Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Healthy People 2020. Available online: https://www.healthypeople.gov/ (accessed on 13 January 2020).
- Clifford Astbury, C.; Penney, T.L.; Adams, J. Comparison of individuals with low versus high consumption of home-prepared food in a group with universally high dietary quality: A cross-sectional analysis of the UK National Diet & Nutrition Survey (2008–2016). Int. J. Behav. Nutr. Phys. Act. 2019, 16, 9. [Google Scholar] [CrossRef] [PubMed]
- Tumin, R.; Anderson, S.E. Television, home-cooked meals, and family meal frequency: Associations with adult obesity. J. Acad Nutr. Diet. 2017, 117, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.I.; Perry, C.L.; Story, M.; Neumark-Sztainer, D. Food preparation by young adults is associated with better diet quality. J. Am. Diet Assoc. 2006, 106, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.I.; Story, M.; Eisenberg, M.E.; Neumark-Sztainer, D. Food preparation and purchasing roles among adolescents: Associations with sociodemographic characteristics and diet quality. J. Am. Diet Assoc. 2006, 106, 211–218. [Google Scholar] [CrossRef]
- Berge, J.M.; MacLehose, R.F.; Larson, N.; Laska, M.; Neumark-Sztainer, D. Family food preparation and its effects on adolescent dietary quality and eating patterns. J. Adolesc. Health 2016, 59, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Van der Horst, K.; Ferrage, A.; Rytz, A. Involving children in meal preparation. Effects on food intake. Appetite 2014, 79, 18–24. [Google Scholar] [CrossRef]
- Mills, S.; White, M.; Brown, H.; Wrieden, W.; Kwasnicka, D.; Halligan, J.; Robalino, S.; Adams, J. Health and social determinants and outcomes of home cooking: A systematic review of observational studies. Appetite 2017, 111, 116–134. [Google Scholar] [CrossRef]
- Ziauddeen, N.; Page, P.; Penney, T.L.; Nicholson, S.; Kirk, S.F.; Almiron-Roig, E. Eating at food outlets and leisure places and “on the go” is associated with less-healthy food choices than eating at home and in school in children: Cross-sectional data from the UK National Diet and Nutrition Survey Rolling Program (2008–2014). Am. J. Clin. Nutr. 2018, 107, 992–1003. [Google Scholar] [CrossRef]
- Cullen, K.W.; Bishop, R.G.; de Moor, C. Fat practices and consumption among African-American adolescent Boy Scouts: The impact of meal source. Ethn. Dis. 2002, 12, 193–198. [Google Scholar] [PubMed]
- Lachat, C.; Nago, E.; Verstraeten, R.; Roberfroid, D.; Van Camp, J.; Kolsteren, P. Eating out of home and its association with dietary intake: A systematic review of the evidence. Obes. Rev. 2012, 13, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Poti, J.M.; Popkin, B.M. Trends in energy intake among US children by eating location and food source, 1977–2006. J. Am. Diet Assoc. 2011, 111, 1156–1164. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Whitley, M.I.; Graubard, B.I. Away from home meals: Associations with biomarkers of chronic disease and dietary intake in American adults, NHANES 2005–2010. Int. J. Obes. 2015, 39, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Zick, C.D.; Stevens, R.B. Trends in Americans’ food-related time use: 1975–2006. Public Health Nutr. 2010, 13, 1064–1072. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.P.; Ng, S.W.; Popkin, B.M. Trends in US home food preparation and consumption: Analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutr. J. 2013, 12, 45. [Google Scholar] [CrossRef]
- McKinsey & Company. The Changing Market for Food Delivery. Available online: https://www.mckinsey.com/industries/technology-media-and-telecommunications/our-insights/the-changing-market-for-food-delivery (accessed on 27 January 2020).
- Statista. Main Reasons People Order Pick up and/or Delivery Food the United States in 2018. Available online: https://www.statista.com/statistics/959112/reasons-for-ordering-takeout-food-us/ (accessed on 27 January 2020).
- Bowers, D. Cooking trends echo changing roles of women. Food Rev. 2000, 23, 23–29. [Google Scholar] [CrossRef]
- U.S. Census Bureau. The Majority of Children Live with Two Parents, Census Bureau Reports. Available online: https://www.census.gov/newsroom/press-releases/2016/cb16-192.html (accessed on 27 January 2020).
- Christian, T.J. Trade-offs between commuting time and health-related activities. J. Urban Health 2012, 89, 746–757. [Google Scholar] [CrossRef]
- Lavelle, F.; McGowan, L.; Spence, M.; Caraher, M.; Raats, M.M.; Hollywood, L.; Dowell, D.; Cloat, A.; Mooney, E.; Dean, M. Barriers and facilitators to cooking from ‘scratch’ using basic or raw ingredients: A qualitative interview study. Appetite 2016, 107, 383–391. [Google Scholar] [CrossRef]
- Share Our Strength’s Cooking Matters. It’s Dinnertime: A Report on Low-Income Families’ Efforts to Plan, Shop for and Cook Healthy Meals. Available online: https://cookingmatters.org/ItsDinnertime (accessed on 13 January 2020).
- Dave, J.M.; Thompson, D.I.; Svendsen-Sanchez, A.; Cullen, K.W. Perspectives on barriers to eating healthy among food pantry clients. Health Equity 2017, 1, 28–34. [Google Scholar] [CrossRef]
- Hilmers, A.; Hilmers, D.C.; Dave, J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am. J. Public Health 2012, 102, 1644–1654. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place. 2010, 16, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Wingert, K.; Zachary, D.A.; Fox, M.; Gittelsohn, J.; Surkan, P.J. Child as change agent. The potential of children to increase healthy food purchasing. Appetite 2014, 81, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, F.; Spence, M.; Hollywood, L.; McGowan, L.; Surgenor, D.; McCloat, A.; Mooney, E.; Caraher, M.; Raats, M.; Dean, M. Learning cooking skills at different ages: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 119. [Google Scholar] [CrossRef] [PubMed]
- Quelly, S.B. Helping with meal preparation and children’s dietary intake: A literature review. J. Sch. Nurs. 2019, 35, 51–60. [Google Scholar] [CrossRef]
- Hersch, D.; Perdue, L.; Ambroz, T.; Boucher, J.L. The impact of cooking classes on food-related preferences, attitudes, and behaviors of school-aged children: A systematic review of the evidence, 2003–2014. Prev. Chronic Dis. 2014, 11, E193. [Google Scholar] [CrossRef]
- Muzaffar, H.; Metcalfe, J.J.; Fiese, B. Narrative review of culinary interventions with children in schools to promote healthy eating: Directions for future research and practice. Curr. Dev. Nutr. 2018, 2, nzy016. [Google Scholar] [CrossRef]
- Pham, M.T.; Rajic, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef]
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Available online: http://www.prisma-statement.org/ (accessed on 26 February 2020).
- Bell, B.M.; Martinez, L.; Gotsis, M.; Lane, H.C.; Davis, J.N.; Antunez-Castillo, L.; Ragusa, G.; Spruijt-Metz, D. Virtual Sprouts: A virtual gardening pilot intervention increases self-efficacy to cook and eat fruits and vegetables in minority youth. Games Health J. 2018, 7, 127–135. [Google Scholar] [CrossRef]
- Chen, Q.; Goto, K.; Wolff, C.; Bianco-Simeral, S.; Gruneisen, K.; Gray, K. Cooking up diversity. Impact of a multicomponent, multicultural, experiential intervention on food and cooking behaviors among elementary-school students from low-income ethnically diverse families. Appetite 2014, 80, 114–122. [Google Scholar] [CrossRef]
- Cunningham-Sabo, L.; Lohse, B. Impact of a school-based cooking curriculum for fourth-grade students on attitudes and behaviors is influenced by gender and prior cooking experience. J. Nutr. Educ. Behav. 2014, 46, 110–120. [Google Scholar] [CrossRef] [PubMed]
- D’Adamo, C.R.; McArdle, P.F.; Balick, L.; Peisach, E.; Ferguson, T.; Diehl, A.; Bustad, K.; Bowden, B.; Pierce, B.A.; Berman, B.M. Spice MyPlate: Nutrition education focusing upon spices and herbs improved diet quality and attitudes among urban high school students. Am. J. Health Promot. 2016, 30, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Martinez, L.C.; Spruijt-Metz, D.; Gatto, N.M. LA Sprouts: A 12-week gardening, nutrition, and cooking randomized control trial improves determinants of dietary behaviors. J. Nutr. Educ. Behav. 2016, 48, 2–11.e1. [Google Scholar] [CrossRef] [PubMed]
- Gatto, N.M.; Martinez, L.C.; Spruijt-Metz, D.; Davis, J.N. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr Obes. 2017, 12, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Jarpe-Ratner, E.; Folkens, S.; Sharma, S.; Daro, D.; Edens, N.K. An experiential cooking and nutrition education program increases cooking self-efficacy and vegetable consumption in children in grades 3–8. J. Nutr. Educ. Behav. 2016, 48, 697–705.e1. [Google Scholar] [CrossRef]
- Liquori, T.; Koch, P.D.; Contento, I.R.; Castle, J. The Cookshop Program: Outcome evaluation of a nutrition education program linking lunchroom food experiences with classroom cooking experiences. J. Nutr. Educ. 1998, 30, 302–313. [Google Scholar] [CrossRef]
- Overcash, F.; Ritter, A.; Mann, T.; Mykerezi, E.; Redden, J.; Rendahl, A.; Vickers, Z.; Reicks, M. Impacts of a vegetable cooking skills program among low-income parents and children. J. Nutr. Educ. Behav. 2018, 50, 795–802. [Google Scholar] [CrossRef]
- Harris, A.D.; McGregor, J.C.; Perencevich, E.N.; Furuno, J.P.; Zhu, J.; Peterson, D.E.; Finkelstein, J. The use and interpretation of quasi-experimental studies in medical informatics. J. Am. Med. Inform. Assoc. 2006, 13, 16–23. [Google Scholar] [CrossRef]
- Handley, M.A.; Lyles, C.R.; McCulloch, C.; Cattamanchi, A. Selecting and improving quasi-experimental designs in effectiveness and implementation research. Annu. Rev. Public Health 2018, 39, 5–25. [Google Scholar] [CrossRef]
- Institute for Policy Studies. Income Inequality in the United States. Available online: https://inequality.org/facts/income-inequality/ (accessed on 28 January 2020).
- Kumanyika, S.K.; Whitt-Glover, M.C.; Gary, T.L.; Prewitt, T.E.; Odoms-Young, A.M.; Banks-Wallace, J.; Beech, B.M.; Hughes-Halbert, C.; Karanja, N.; Lancaster, K.J.; et al. Expanding the obesity research paradigm to reach African American communities. Prev. Chronic. Dis. 2007, 4, A112. [Google Scholar]
- Melius, J.; Barr-Anderson, D.J.; Orekoya, O. Consideration of factors influencing weight outcomes among U.S. racial-ethnic minority populations in the social work literature. Soc. Work Public Health 2019, 34, 158–175. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice Hall: Englewood Cliffs, NJ, USA, 1986; ISBN 9780138156145. [Google Scholar]
- Baranowski, T.; Perry, C.L.; Parcel, G.S. How individuals, environments, and health behaviors interact. In Health Behavior and Health Education: Theory, Research and Practice, 3rd ed.; Glanz, K., Rimer, B.K., Lewis, F.M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2002; pp. 165–184. [Google Scholar]
- Murimi, M.W.; Kanyi, M.; Mupfudze, T.; Amin, M.R.; Mbogori, T.; Aldubayan, K. Factors influencing efficacy of nutrition education interventions: A systematic review. J. Nutr. Educ. Behav. 2017, 49, 142–165.e1. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, P.J.; Carraca, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute; U.S. Department of Health and Human Services; National Institutes of Health. Theory at a Glance: A Guide for Health Promotion Practice, 2nd ed.; U.S. Government Printing Office: Washington, DC, USA, 2005.
- Michie, S.; Prestwich, A. Are interventions theory-based? Development of a theory coding scheme. Health Psychol. 2010, 29. [Google Scholar] [CrossRef] [PubMed]
- Concannon, T.W.; Meissner, P.; Grunbaum, J.A.; McElwee, N.; Guise, J.M.; Santa, J.; Conway, P.H.; Daudelin, D.; Morrato, E.H.; Leslie, L.K. A new taxonomy for stakeholder engagement in patient-centered outcomes research. J. Gen. Intern. Med. 2012, 27, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Morton, K.L.; Atkin, A.J.; Corder, K.; Suhrcke, M.; Turner, D.; van Sluijs, E.M. Engaging stakeholders and target groups in prioritising a public health intervention: The Creating Active School Environments (CASE) online Delphi study. BMJ Open 2017, 7, e013340. [Google Scholar] [CrossRef] [PubMed]
- Boaz, A.; Hanney, S.; Borst, R.; O’Shea, A.; Kok, M. How to engage stakeholders in research: Design principles to support improvement. Health Res. Policy Syst. 2018, 16, 60. [Google Scholar] [CrossRef] [PubMed]
- Gruber, K.J.; Haldeman, L.A. Using the family to combat childhood and adult obesity. Prev. Chronic. Dis. 2009, 6, A106. [Google Scholar] [PubMed]
- Lenhart, A.; Kahne, J.; Middaugh, E.; Macgill, A.R.; Evans, C.; Vitak, J. Teens, Video Games and Civics: Teens’ Gaming Experiences are Diverse and Include Significant Social Interaction and Civic Engagement. Available online: http://www.pewinternet.org/2008/09/16/teens-video-games-and-civics/ (accessed on 28 January 2020).
- Pew Research Center. Mobile Fact Sheet. Available online: https://www.pewresearch.org/internet/fact-sheet/mobile/ (accessed on 28 January 2020).
- Rideout, V.J.; Foehr, U.G.; Roberts, D.F. Generation M2: Media in the Lives of 8- to 18-Year-Olds. Available online: http://files.eric.ed.gov/fulltext/ED527859.pdf (accessed on 28 January 2020).
- Thompson, D.; Bhatt, R.; Vazquez, I.; Cullen, K.W.; Baranowski, J.; Baranowski, T.; Liu, Y. Creating action plans in a serious video game increases and maintains child fruit-vegetable intake: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 39. [Google Scholar] [CrossRef]
- Pearson. Student Mobile Device Survey 2015: National Report: Students in Grades 4-12. Available online: https://www.pearsoned.com/wp-content/uploads/2015-Pearson-Student-Mobile-Device-Survey-Grades-4-12.pdf (accessed on 13 January 2020).
- Steckler, A.; Linnan, L. Process evaluation for public health interventions and research: An overview. In Process Evaluation for Public Health, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 2002; pp. 1–24. [Google Scholar]
- Heerman, W.J.; JaKa, M.M.; Berge, J.M.; Trapl, E.S.; Sommer, E.C.; Samuels, L.R.; Jackson, N.; Haapala, J.L.; Kunin-Batson, A.S.; Olson-Bullis, B.A.; et al. The dose of behavioral interventions to prevent and treat childhood obesity: A systematic review and meta-regression. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 157. [Google Scholar] [CrossRef] [PubMed]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Anderson, C.; Carmack, C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am. J. Prev. Med. 1998, 15, 266–297. [Google Scholar] [CrossRef]
- Wu, Y.P.; Thompson, D.; Aroian, K.J.; McQuaid, E.L.; Deatrick, J.A. Commentary: Writing and evaluating qualitative research reports. J. Pediatr. Psychol. 2016, 41, 493–505. [Google Scholar] [CrossRef]
| Author (Year) | Study Name | Research Design | Data Collection Schedule | Recruitment Focus | Sample Size | Income/SES Criterion | Participant Race/Ethnicity | Recruitment Location | Geographic Location | Data Collection Method | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bell et al. [36] (2018) | Virtual Sprouts | two group design; quasi-experimental; pilot intervention | pre+post (child only) | child (predominantly minority, underserved; 3–5 grades) | 180 (control = 64, intervention = 116) | public elementary charter schools in LA; participants: 92% treatment/73% control eligible to receive free lunch | Latino 9.5% tx/11.3% control; White 0% tx/1.6% control; Black 63% tx/58.1% control; Native American 0.9% tx/0% control; Mixed Race 25.9% tx/29% control; Other. 9% tx/0% control | School (n = 2) | Los Angeles, CA | survey | + self-efficacy to eat FV; + self-efficacy to cook FV |
| Chen et al. [37] (2014) | Cooking up Diversity | two group design; quasi-experimental; mixed methods | pre+post (child + parent); post-intervention focus groups (parent only) | both (K-2 students) | 1204 (control = 600; intervention = 604) | low-income schools where majority of students were eligible to receive free/reduced price meals program; participants: nearly 80% qualified for free/reduced price meals | Latino/Hispanic 32.4%; Hmong 9.1%; White 42.3%; Other 16.2% | School (n = 6) | Northern California | survey; focus group discussions | + familiarity, preferences, and consumption of vegetables and increased involvement with food prep at home; + parental appreciation of new foods/recipes |
| Cunningham-Sabo et al. [38] (2014) | Cooking with Kids | (2 cohorts); 3 group design; quasi-experimental | pre+post (child only) | child (4th grade) | 961 (completed both pre and post-survey) | schools had to have ≥50% of students eligible for free/reduced price school meals; participants: SES not provided | Hispanic 84.1%; White 10.1%; American Indian 2.8%; American Indian 2.8%; Black 1.1%; Asian 0.6%; NA 1.3% | School (n = 11) | Santa Fe, NM | survey | +FV preferences +cooking self-efficacy and attitudes in students without cooking experience (mostly males) |
| D’Adamo et al. [39] (2016) | Spice MyPlate | quasi-experimental; two group design | baseline, 3, 6, and 10 weeks after baseline (child only) | child | 110 | School—free/reduced price meal participation (School A = 75%; School B = 74%); participants—SES not provided | African American 87.3% tx/63.6% control; White 1.8% tx/12.7% control; Hispanic 0% tx/3.6% control; Asian/Pacific Islander 0% tx/3.6% control; Native American 3.6% tx/0% control; Other 1.8% tx/9.1% control | school (n = 2) (grades 9–12) | East Baltimore, MD | 3-day food record, survey | Spice MyPlate intervention was feasible; + whole grains, and protein foods intake; + attitudes towards eating vegetables, whole grains, lean protein, and low-fat dairy |
| Davis et al. [40] (2016) | LA Sprouts | RCT | pre+post (child only) | child (3rd–5th grade) | 304 (control = 137; intervention = 167) | school eligibility: ≥75% received free/reduced price lunches; participants—89% control/91% treatment eligible for free/reduced price lunch | Hispanic 88.8% control/88.6% tx; Asian 1.5% control /0.6% tx; Non-Hispanic Black 0% control/2.4% tx; Non-Hispanic White 1.5% control/1.2% tx; Other 8.2% control/7.2% tx | after-school program (n = 4)—LA’s Better Educated Students for Tomorrow | Los Angeles, CA | Questionnaire | + Scores for identification of vegetables, and nutrition and gardening knowledge for LA Sprouts participants; + More likely for LA Sprouts participants to garden at home |
| Gatto et al. [41] (2017) | LA Sprouts | 2 group RCT | pre+post (child only) | child (3–5 grades) | 319 (control = 147; intervention = 172) | school eligibility: ≥75% received free lunch program; participants—89% control/91% treatment eligible for free/reduced price lunch | Hispanic/Latino 89% tx/88.8% control | after-school program n = 4)—LA’s Better Educated Students for Tomorrow | Los Angeles, CA | food frequency questionnaire, anthropo-metrics, optional fasting blood sample | LA Sprouts participants had greater reduction in BMI z-scores, and waist circumference; − Number of LA Sprouts participants with metabolic syndrome; + Dietary fiber intake for LA Sprouts participants; − Decreased vegetable intake for all study participants, but LA Sprouts participants had smaller decreases |
| Jarpe-Ratner et al. [42] (2016) | Common Threads | quasi-experimental | pre+post (child + parent) | child (grades 3–8) | 271 | ≥80% of students eligible for free/reduced price lunch; participants—94% eligible for free/reduced price lunch | (analyzed sample) African American 44%; Hispanic 42%; White 7%; Other 7% | School (n = 18) | Chicago, IL | survey | + FV consumption, nutrition knowledge, cooking self-efficacy, exposure to new foods, and cooking at home for students; + Family conversations about healthy foods, frequency children prepared dinner, parent perception on ability to prepare health meal, and importance parents place on family meal; sustained effect at post 2 |
| Liquori et al. [43] (1998) | The Cookshop Program | quasi-experimental design | pre+post (child only) | child (K-6 grades) | 590 | schools: low-income school district; participant SES not provided | not provided for participants; however, recruited from schools that were 85% African American and 15% Hispanic | School (n = 2) | Central Harlem community of NYC | survey; visual inspection of plate waste | + (CS) preferences, knowledge, and plate waste in both younger and older children and on behavioral intention in younger children and cooking self-efficacy in older children; + (FEL) knowledge for both age groups |
| Overcash et al. [44] (2018) | Cooking Matters for Families | one group; quasi-experimental | pre+post (child + parent) | both | 89 | family qualified for public assistance; participants—61% had low/very low food security | White 12%; Black/African American 34%; Asian/Pacific Islander/American Indian 4%; Other 41%; Mixed race 9%; Hispanic ethnicity 43% | Subsidized housing, churches, schools, and community centers (# of participating organizations not identified) | Minneapolis-St Paul, MN | survey | + Parental cooking confidence, healthy food prep, child self-efficacy, vegetable variety and home vegetable availability |
| Author (Year) | Theoretical Framework (s) | Stakeholder Involvement | Adaptation for Low SES |
|---|---|---|---|
| Bell et al. [36] (2018) | Self Determination Theory, Social Cognitive Theory | formative research with stakeholders to develop the program | extension of previous nutrition/cooking/gardening program for urban Latino upper elementary aged children; formative work with stakeholders (observation, focus groups, surveys, prototyping, concept testing) |
| Chen et al. [37] (2014) | none described | parents, bicultural staff members who had experience providing cooking classes to Hmong/Latino adults participated in recipe development | Local, ethnic produce items were featured. Ingredients were affordable and provided to students. Equipment such as cutting boards and aprons were provided |
| Cunningham-Sabo et al. [38] (2014) | none described | none described | bilingual curriculum, affordable ingredients; focus on diverse cultural traditions |
| D’Adamo et al. [39] (2016) | none described | students, teachers, community-based health professionals involved in curriculum development | spices selected based on accessibility, cultural acceptability, affordability, palatability, versatility, health benefits, familiarity, novelty |
| Davis et al. [40] (2016) | Social Cognitive Theory and Self Determination Theory | pilot tested with 4th and 5th grade students; tested again in cluster RCT with predominantly low-income Hispanic 3rd–5th grade students | lessons were culturally tailored |
| Gatto et al. [41] (2017) | self-efficacy | pilot tested with predominantly low-income Hispanic students prior to finalizing program | none described although developed for urban Latino upper elementary aged children |
| Jarpe-Ratner et al. [42] (2016) | none described | none described | recipes designed to be affordable, flexible, and consistent with dietary guidelines (2010) |
| Liquori et al. [43] (1998) | Social Cognitive Theory | pilot tested classroom and lunchroom components—adjusted based on results and feedback | pilot tested classroom and lunchroom components—adjusted based on results and feedback |
| Overcash et al. [44] (2018) | Social Cognitive Theory | none described | designed for low-income families (no information provided on how this was accomplished) |
| Author (Year) | Components | Primary Intervention Focus | Delivery Mode | Parent Involve-ment * | # of Sessions | Session Length | Program Duration | Program Leader(s) | Leader Training | Delivery Location(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| Bell et al. [36] (2018) | program focus—nutrition education, cooking, gardening; Game: cooking and gardening; classroom curriculum: nutrition education; cooking demonstrations; practice; reflection; family home activities—materials provided | child | game (played in class on tablet), in-class lessons, in-home activities | +++ | 3 game sessions, 3 class lessons, 3 in-home activities | Games and lessons were each an hour long, and in-home activities spanned the course of 3 days per week | 3 weeks | game (independent); teacher (classroom); home (family) | Teachers were trained | Games played and lesson taught in classroom. The in-home activities were at home |
| Chen et al. [37] (2014) | Recipe demonstrations, recipe card info lessons, tasting activities. Family food kits were given to students to take home (cooking equipment, spices). Backpack of equipment also provided | both | classroom, home | +++ | 1 session per month (1–2 recipes) | 20 min to present in-class activities for one recipe | Feb–May | nutrition educator and teacher | none described | classroom and home |
| Cunningham-Sabo et al. [38] (2014) | cooking and/or tasting sessions | child | hands-on cooking classes and/or tasting sessions in classroom; classroom meals served in school cafeteria several times a month | + | 1 introductory session; 5 cooking and/or FV tasting sessions | 1 h introductory session; 2 h cooking sessions; 1 h tasting lessons | school year | Parents invited to volunteer. FV tastings led by classroom teachers. Cooking lessons led by Cooking with Kids food educators | none described | classroom; school cafeteria |
| D’Adamo et al. [39] (2016) | Spice MyPlate intervention was 6 weekly nutrition education sessions focused on using spices and herbs in a diet + a 1 h grocery tour + 2 h of cooking sessions | child | classroom lessons (health class), grocery tour, cooking sessions | − | 1 h standard nutrition education, 6 sessions of My Plate curriculum, 1 grocery tour, 2 h of cooking sessions | nutrition lessons were 1 h long, grocery tour was 1 h, and there was a total of 2 h of cooking sessions | 6 weeks | Chefs led the cooking sessions; Health Corps coordinator led the nutrition lessons | none mentioned | school (health class) |
| Davis et al. [40] (2016) | gardening, cooking, nutrition | child | hands-on, instructional | − | 12 | 90 min | 12 weeks | nutrition and garden educators with strong backgrounds in cooking, nutrition, gardening | none described | school (after-school program) |
| Gatto et al. [41] (2017) | gardening, cooking, nutrition | child | hands-on, demonstration | +++ (parallel program for parents) | 12 | 90 min | 12 weeks | educators with nutrition or gardening backgrounds | none described | school (school garden) |
| Jarpe-Ratner et al. [42] (2016) | nutrition education, culinary skills, and meal preparation, meal sharing, and discussion | child | hands-on, instructional | + | 10 per semester | 30-min lectures, 75-min instruction on culinary skills and prep, 15-min of meal sharing, conversation | 10 weeks in a school semester | chef-instructors | chef-instructors went through 2 h training by Common Threads staff | school (after-school program) |
| Liquori et al. [43] (1998) | school lunch component; classroom component (cooking and tasting sessions OR participatory activities without cooking and tasting); parent and community component | child | hands-on, instructional | +++ | − | 60-90 min for cook shop; 45 min for food and environment lessons | school year | food service staff led cafeteria component; classroom teachers, parents, and college students were Cook Shop instructors | Cook Shop instructors had two 3-h training sessions; food service staff had one 3 h training session; program staff met with parent assistants and volunteer college students before and after each session for training support | school |
| Overcash et al. [44] (2018) | demonstration, food preparation, nutrition education lessons, and a meal. Families were given a bag of groceries needed to prepare the meal at home | both | hands-on, instructional | +++ | 6 | 2 h | September 2014–June 2016 | chefs, nutrition educators | chefs and nutrition educators went through training sessions | 11 different host sites |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, P.P.; Mackey, G.; Callender, C.; Dave, J.M.; Olvera, N.; Alford, S.; Thompson, D. Culinary Education Programs for Children in Low-Income Households: A Scoping Review. Children 2020, 7, 47. https://doi.org/10.3390/children7050047
Li PP, Mackey G, Callender C, Dave JM, Olvera N, Alford S, Thompson D. Culinary Education Programs for Children in Low-Income Households: A Scoping Review. Children. 2020; 7(5):47. https://doi.org/10.3390/children7050047
Chicago/Turabian StyleLi, Priscilla P., Guisela Mackey, Chishinga Callender, Jayna M. Dave, Norma Olvera, Shana Alford, and Debbe Thompson. 2020. "Culinary Education Programs for Children in Low-Income Households: A Scoping Review" Children 7, no. 5: 47. https://doi.org/10.3390/children7050047
APA StyleLi, P. P., Mackey, G., Callender, C., Dave, J. M., Olvera, N., Alford, S., & Thompson, D. (2020). Culinary Education Programs for Children in Low-Income Households: A Scoping Review. Children, 7(5), 47. https://doi.org/10.3390/children7050047







