Tackling Childhood Stunting in the Eastern Mediterranean Region in the Context of COVID-19
Abstract
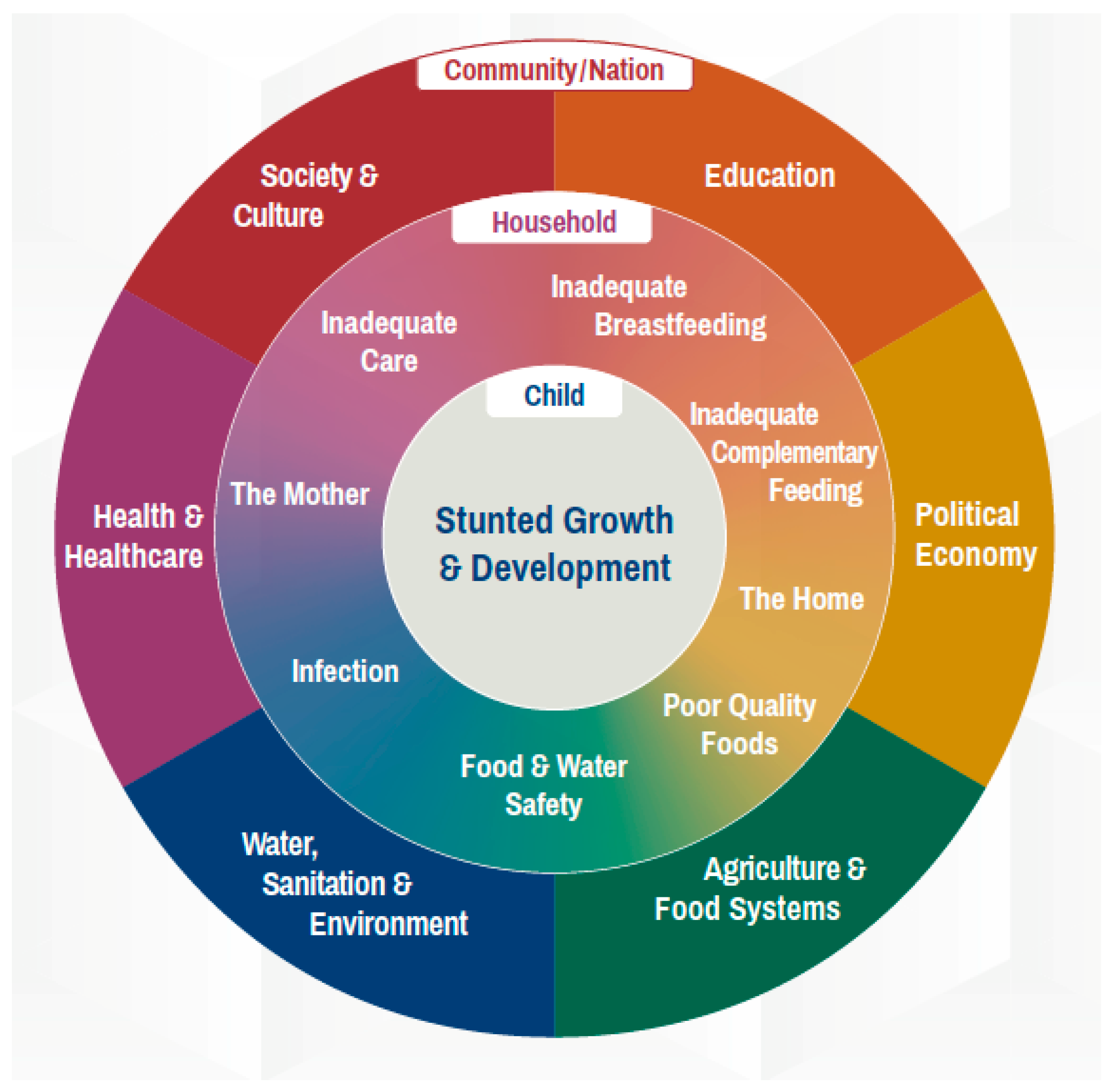
1. Introduction
2. Materials and Methods
3. Results
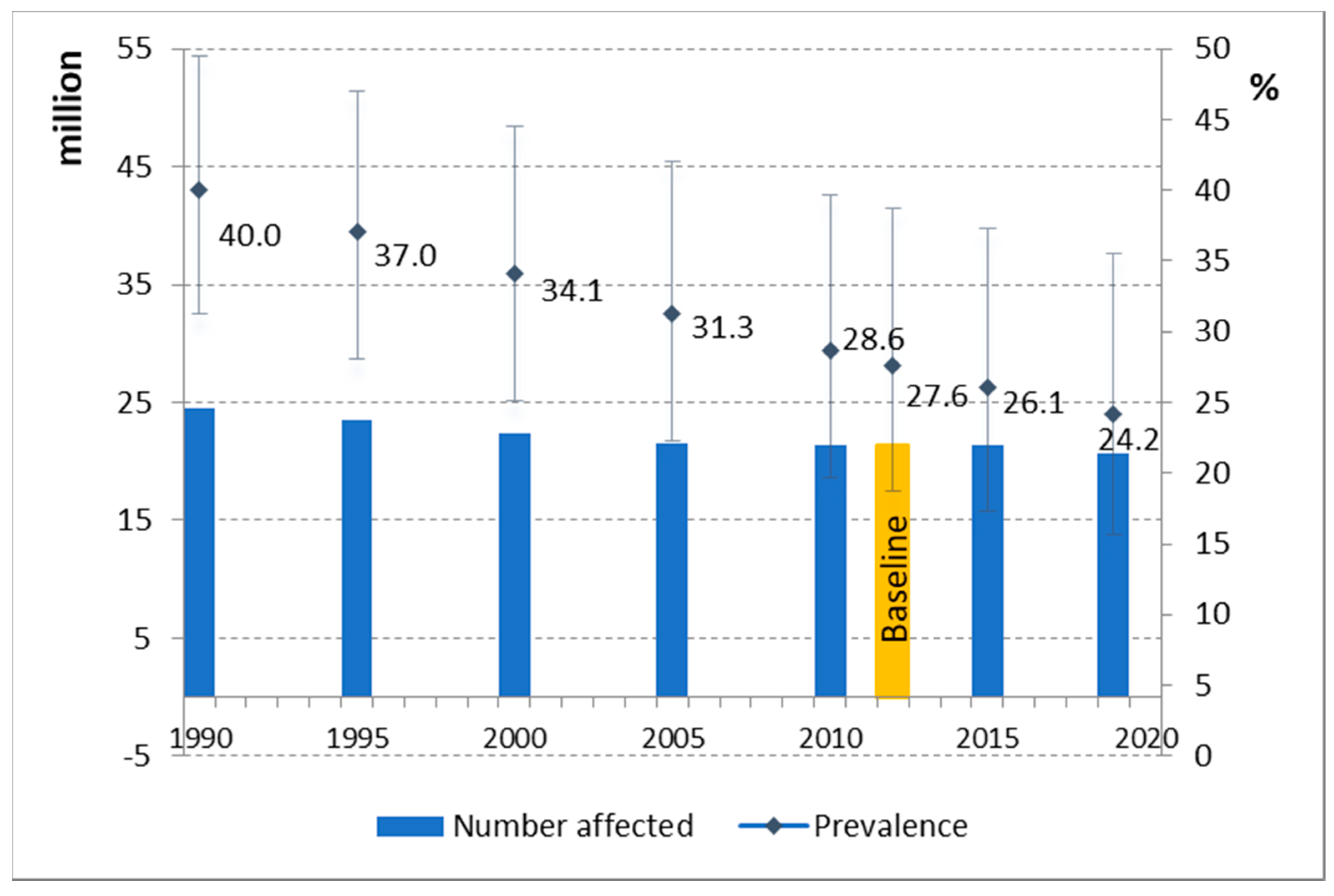
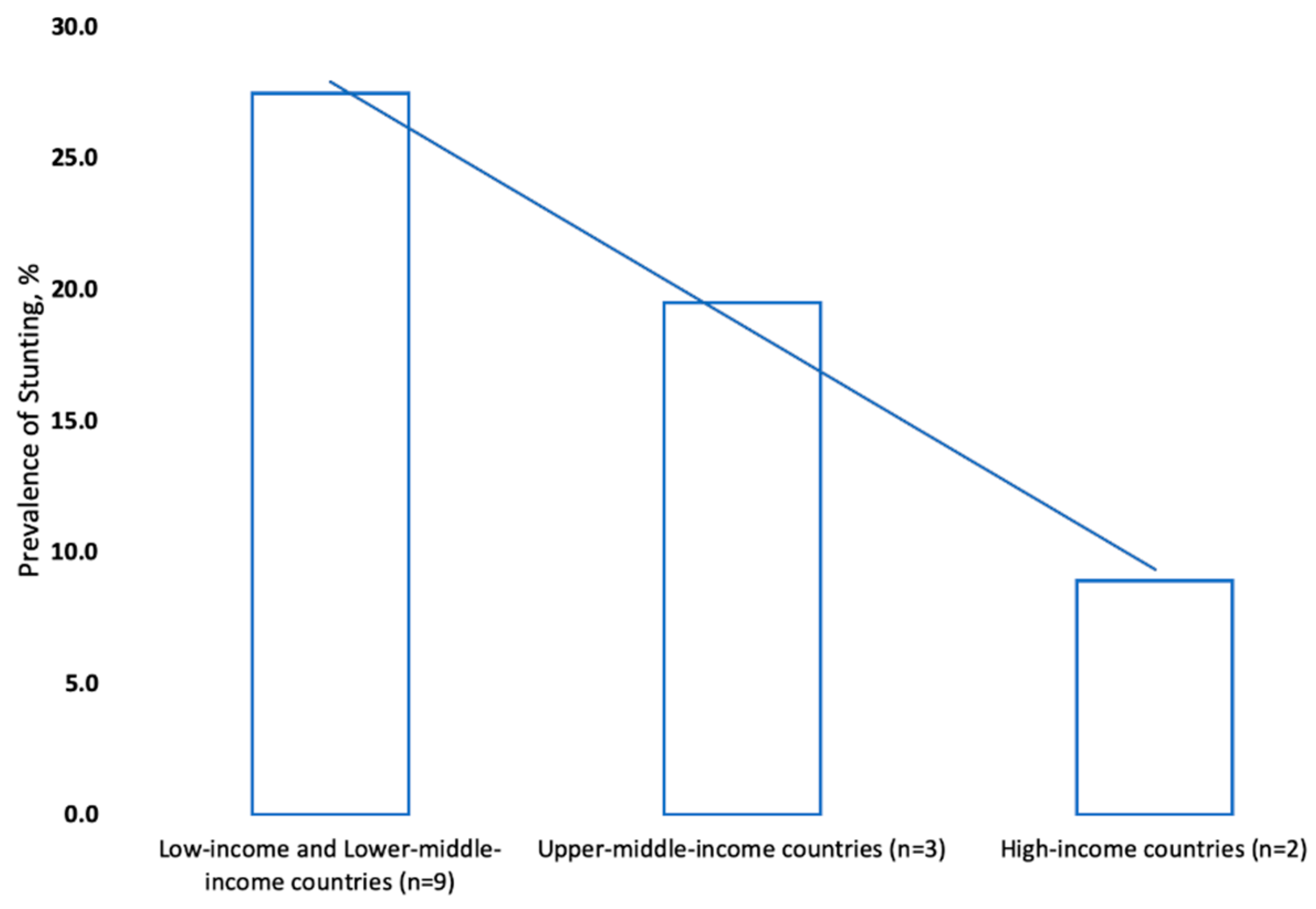
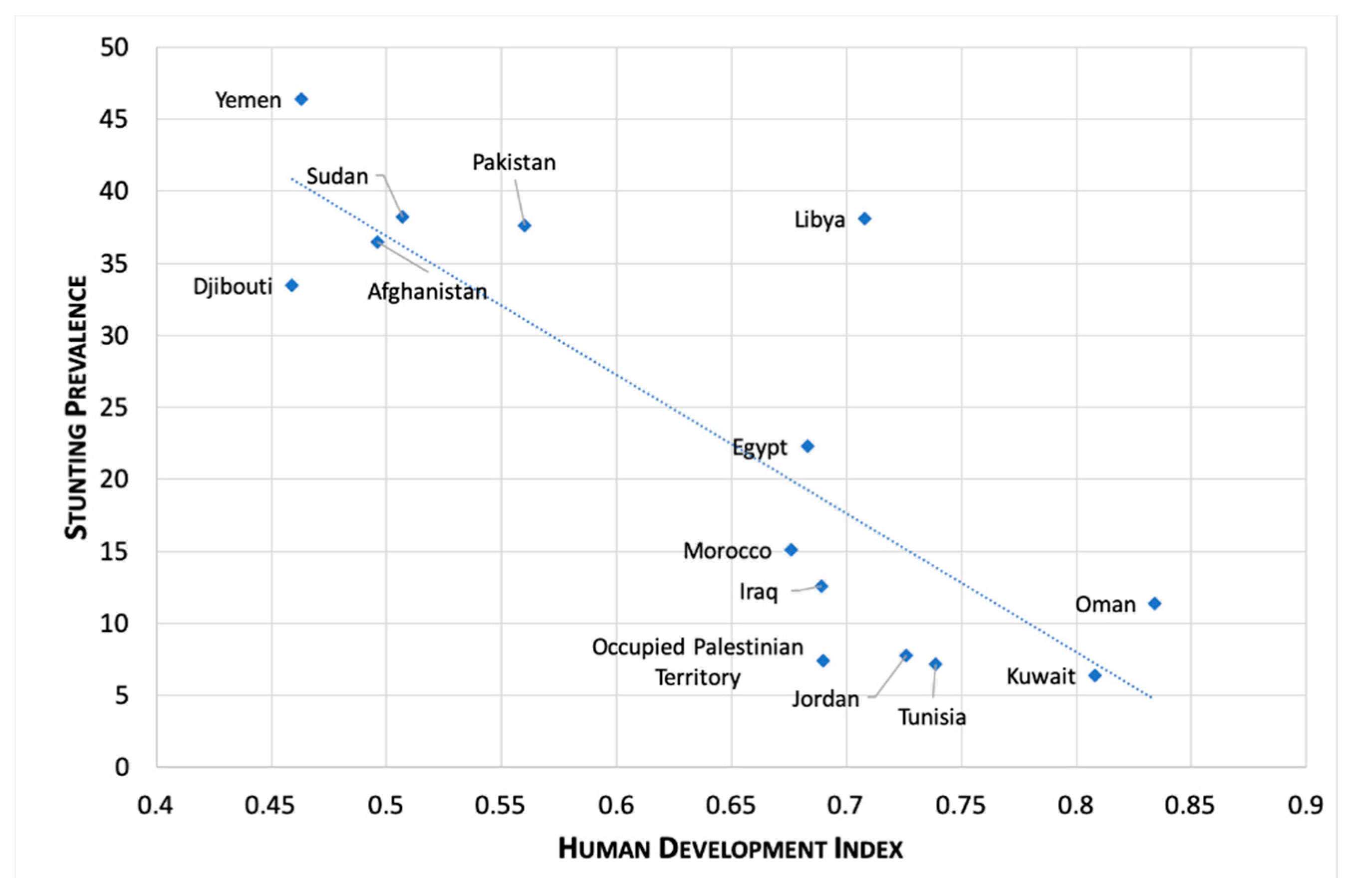
3.1. Childhood Stunting in the Eastern Mediterranean Region
3.2. Multisectoral Policy Responses to Prevent Stunting
3.2.1. Health
3.2.2. Education
3.2.3. Agriculture
3.2.4. Water and Sanitation
4. Discussion
4.1. Priority Actions to Tackle Stunting
4.2. Country Experience in Reducing Stunting
4.3. Tackling Stunting and Other Forms of Malnutrition
4.4. Barriers and Challenges to Nutrition Action in the Context of COVID-19
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- United Nations Children’s Fund (UNICEF); World Health Organization; International Bank for Reconstruction and Development; The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Food and Agriculture Organization; United Nations Children’s Fund; World Food Programme; World Health Organization. Joint Statement by FAO, UNICEF, WFP, WHO on Nutrition during the COVID-19 Pandemic in the Middle East and North Africa, Eastern Mediterranean and Arab Regions; WHO Regional Office for the Eastern Mediterranean Region: Cairo, Egypt; Amman, Jordan, 2020. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-For-Height and Body Mass Index-For Age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- World Health Organization. Global Nutrition Targets 2025: Stunting Policy Brief; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- United Nations Children’s Fund. The State of the World’s Children 2013. Children with Disabilities; UNICEF: New York, NY, USA, 2013. [Google Scholar]
- Walker, S.; Chang, S.C.; Powell, C.; Simonoff, E.; Grantham-McGregor, S. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J. Nutr. 2007, 137, 2464–2469. [Google Scholar] [CrossRef] [PubMed]
- Black, R.; Victora, C.; Walker, S.; Bhutta, Z.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Matorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Hoddinott, J.; Alderman, H.; Behrman, J.R.; Haddad, L.; Horton, S. The economic rationale for investing in stunting reduction. Matern. Child Nutr. 2013, 9 (Suppl. 2), 69–82. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.; Adair, L.; Fall, C.; Hallal, P.; Martorell, R.; Richter, L.; Sachdev, H. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- The World Bank. Repositioning Nutrition as Central to Development: A Strategy for Large-Scale Action; The World Bank: Washington, DC, USA, 2006. [Google Scholar]
- Grantham-Mcgregor, S.; Cheung, Y.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- World Health Assembly Resolution WHA65.6. Comprehensive implementation plan on maternal, infant and young child nutrition. In Proceedings of the Sixty-Fifth World Health Assembly, Geneva, Switzerland, 21–26 May 2012; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- WHO Regional Office for the Mediterranean. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030; WHO: Cairo, Egypt, 2019. [Google Scholar]
- World Health Organization; United Nations Children’s Fund (UNICEF). Discussion Paper: The Extension of the 2025 Maternal, Infant and Young Child Nutrition Targets to 2030; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization. Stunted Growth and Development: Context, Causes and Consequences; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Black, R.; Allen, L.; Bhutta, Z.; Caulfield, L.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations; World Health Organization. Framework for Action: Outcome Document of the Second International Conference on Nutrition; FAO: Rome, Italy, 2014. [Google Scholar]
- United Nations General Assembly. UN Resolution on the UN Decade of Action on Nutrition; A/RES/70/259; United Nations: New York, NY, USA, 2015. [Google Scholar]
- World Health Organization. Reducing Stunting in Children: Equity Considerations for Achieving the Global Nutrition Targets 2025; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. On Setting and Implementing a Stunting Reduction Agenda: Action Points for Country Programme Implementers; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- United Nations Children’s Fund (UNICEF); World Health Organization. Global Nutrition Monitoring Framework: Operational Guidance for Tracking Progress in Meeting Targets for 2025; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- De Onis, M.; Blossner, M.; Borghi, E.; Morris, R.; Frongillo, E. Methodology for estimating regional and global trends of child malnutrition. Int. J. Epidemiol. 2004, 33, 1260–1270. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; United Nations Children’s Fund (UNICEF). Methodology for Monitoring Progress towards the Global Nutrition Targets for 2025: Technical Report by the WHO-UNICEF Expert Advisory Group on Nutrition Monitoring Team; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Development Initiatives. 2020 Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives Poverty Research Ltd.: Bristol, UK, 2020. [Google Scholar]
- World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 4 August 2020).
- United Nations Development Program. Human Development Index. Available online: http://hdr.undp.org/en/content/human-development-index-hdi (accessed on 4 August 2020).
- World Health Organization. Global Nutrition Policy Review 2016–2017; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Essential Nutrition Actions: Mainstreaming Nutrition through the Life-Course; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organization. Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition; WHO: Geneva, Switzerland, 2014; pp. 7–9. [Google Scholar]
- UNICEF-WHO-The World Bank: Joint Child Malnutrition Estimates—Levels and Trends. Available online: https://www.who.int/publications/i/item/jme-2020-edition (accessed on 2 March 2020).
- De Onis, M.; Borghi, E.; Arimond, M.; Webb, P.; Croft, T.; Saha, K.; De-Regil, L.; Thuita, F.; Heidkamp, R.; Krasevec, J.; et al. Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutr. 2018, 22, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Government of Egypt. Egypt National Multisectoral Action Plan for Prevention and Control on Noncommunicable Diseases 2017–2021; Government of Egypt: Cairo, Egypt, 2017.
- State of Qatar Supreme Council of Health. Qatar National Nutrition and Physical Activity Action Plan 2017–2022; Qatar Ministry of Public Health: Doha, Qatar, 2017.
- General Directorate Nutrition. National Nutrition Policy, Strategies and Action Plan 2017–2022; Palestinian Ministry of Public Health: Ramallah, Israel, 2016.
- Ministry of Health and Prevention. National Action Plan in Nutrition (2017–2021); United Arab Emirates Government: Abu Dhabi, UAE, 2017.
- Saudi Food and Drug Authority. Strategy of Regulating Healthy Food; SFDA: Riyadh, Saudi Arabia, 2018. [Google Scholar]
- Ministry of Planning, Development and Reform; World Food Programme. Pakistan Multi-Sectoral Nutrition Strategy (PMNS 2018–25); Government of Pakistan: Islamabad, Pakistan, 2018.
- Casanovas, M.; Lutter, C.; Mangasaryan, N.; Mwadime, R.; Hajeebhoy, N.; Aguilar, A.; Kopp, C.; Rico, L.; Ibiett, G.; Andia, D.; et al. Multi-sectoral interventions for healthy growth. Matern. Child Nutr. 2013, 9, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.; Iannotti, L.; Dewey, K.; Michaelsen, K.; Onyango, A. Contextualising complementary feeding in a broader framework for stunting prevention. Matern. Child Nutr. 2013, 9, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Pan-American Health Organization. Guiding Principles for the Complementary Feeding of the Breastfed Child; PAHO/WHO: Washington, DC, USA, 2003. [Google Scholar]
- World Health Organization. Guiding Principles for Feeding Non-Breastfed Children 6–24 Months of Age; WHO: Geneva, Switzerland, 2005. [Google Scholar]
- Food and Agriculture Organization; International Fund for Agricultural Development; United Nations Children’s Fund; World Food Programme; World Health Organization. The State of Food Security and Nutrition in the World 2020: Transforming Food Systems for Affordable Healthy Diets; FAO: Rome, Italy, 2020. [Google Scholar]
- Codex Alimentarius Commission. Principles and Guidelines for National Food Control Systems; CAC/GL 82-2013; Food and Agriculture Organization of the United Nations: Rome, Italy; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- WHO Regional Office for the Eastern Mediterranean. Food and Nutrition Surveillance Systems—Technical Guide for the Development of a Food and Nutrition Surveillance System; WHO: Cairo, Egypt, 2013. [Google Scholar]
- Sheikholeslam, R.; Kimiagar, M.; Siasi, F.; Abdollahi, Z.; Jazayeri, A.; Keyghobadi, K.; Ghaffarpoor, M.; Noroozi, F.; Kalantari, N.; Minaei, M.; et al. Multidisciplinary intervention for reducing malnutrition among children in the Islamic Republic of Iran. East. Mediterr. Health J. 2004, 10, 844–852. [Google Scholar] [PubMed]
- Ministry of Health. National Survey on Population and Family Health; Ministry of Health: Rabat, Morocco, 2018.
- Ministry of Health. National Nutrition Program; Ministry of Health: Rabat, Morocco, 2019.
- United Nations Children’s Fund, Division of Data, Analysis, Planning and Monitoring. UNICEF Global Databases: Infant and Young Child Feeding-Exclusive Breastfeeding, Predominant Breastfeeding; UNICEF: New York, NY, USA, 2020. [Google Scholar]
- Haut Commissariat au Plan. Les Indicateurs Sociaux du Maroc; Direction de la Statistique: Rabat, Morocco, 2018.
- Food and Agriculture Organization of the United Nations. Near East and North Africa: 2019 Regional Overview of Food Security and Nutrition. Rethinking Food Systems for Healthy Diets and Improved Nutrition; FAO: Rome, Italy, 2020. [Google Scholar]
- Food and Agriculture Organization of the United Nations. COVID-19 and Its Impact on Food Security in the Near East and North Africa: How to Respond; FAO: Cairo, Egypt, 2020. [Google Scholar]
- United Nations Children’s Fund (UNICEF); World Health Organization. UNICEF-WHO Low Birthweight Estimates: Levels and Trends 2000–2015; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- UN Secretary General. Policy Brief: The Impact of COVID-19 on Food Security and Nutrition; United Nations: New York, NY, USA, 2020. [Google Scholar]
- United Nations’ Children’s Fund; World Health Organization Regional Office for the Eastern Mediterranean. The Potential Impact of Health Care Disruption on Child Mortality in the Middle East and North Africa Due to COVID-19; UNICEF: New York, NY, USA; WHO: Amman, Jordan, 2020. [Google Scholar]
| Country | Baseline (% (Year)) | Latest (% (Year)) | Pre-Baseline AARR | Current AARR | Required AARR to Reach the 2025 Target |
|---|---|---|---|---|---|
| Afghanistan | 40.4 (2013) | 38.2 (2018) | 1.1 | 4.4 | |
| Bahrain | (a) | ||||
| Djibouti | 33.5 (2012) | 33.5 (2012) | −2.1 | 4.2 | |
| Egypt | 30.7 (2008) | 22.3 (2014) | −3.3 | 5.2 | 5.6 |
| Iran | 6.8 (2011) | 6.8 (2011) | 0.6 | 4.4 | |
| Iraq | 22.1 (2011) | 12.6 (2018) | 2.3 | 7.7 | 5.3 |
| Jordan | 7.8 (2012) | 7.8 (2012) | 4.2 | 1.7 | 3.2 |
| Kuwait | 4.3 (2012) | 6.4 (2017) | −0.8 | −4.5 | 2.5 |
| Lebanon | (a) | ||||
| Libya | 21 (2007) | 38.1 (2014) | 5.7 | 3.7 | |
| Morocco | 14.9 (2011) | 15.1 (2017) | 5.3 | −0.2 | 3.8 |
| Oman | 9.8 (2009) | 11.4 (2017) | 4.7 | −2.5 | 6.4 |
| Occupied Palestinian Territory | 10.9 (2010) | 7.4 (2014) | 3.4 | 9.2 | 4.8 |
| Pakistan | 43 (2011) | 37.6 (2018) | −0.4 | 2.2 | 4.9 |
| Qatar | (a) | 5.7 | |||
| Saudi Arabia | 9.3 (2005) | 5.7 | 4 | ||
| Somalia | 25.3 (2009) | 25.3 (2009) | 0.5 | 6.1 | |
| Sudan | 34.1 (2010) | 38.2 (2014) | 2.9 | −2.9 | 5.2 |
| Syria | 27.9 (2010) | 27.9 (2010) | −0.4 | 2.6 | |
| Tunisia | 10.1 (2012) | 8.4 (2018) | 4.2 | 3.0 | 3.8 |
| United Arab Emirates | No data | No data | |||
| Yemen | 46.6 (2011) | 46.4 (2013) | 2.7 | 0.2 | 4.7 |
| Area of Action | Specific Interventions |
|---|---|
| Promoting healthy diets |
|
| Protecting, promoting and supporting breastfeeding |
|
| Care of low-birth weight and very low birth weight infants |
|
| Appropriate complementary feeding |
|
| Growth monitoring and assessment |
|
| Vitamin A supplementation |
|
| Zinc supplementation in the management of diarrhea |
|
| Nutritional care of women during pregnancy and postpartum |
|
| Specific conditions |
|
| Emergencies |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jawaldeh, A.A.; Doggui, R.; Borghi, E.; Aguenaou, H.; Ammari, L.E.; Abul-Fadl, A.; McColl, K. Tackling Childhood Stunting in the Eastern Mediterranean Region in the Context of COVID-19. Children 2020, 7, 239. https://doi.org/10.3390/children7110239
Jawaldeh AA, Doggui R, Borghi E, Aguenaou H, Ammari LE, Abul-Fadl A, McColl K. Tackling Childhood Stunting in the Eastern Mediterranean Region in the Context of COVID-19. Children. 2020; 7(11):239. https://doi.org/10.3390/children7110239
Chicago/Turabian StyleJawaldeh, Ayoub Al, Radhouene Doggui, Elaine Borghi, Hassan Aguenaou, Laila El Ammari, Azza Abul-Fadl, and Karen McColl. 2020. "Tackling Childhood Stunting in the Eastern Mediterranean Region in the Context of COVID-19" Children 7, no. 11: 239. https://doi.org/10.3390/children7110239
APA StyleJawaldeh, A. A., Doggui, R., Borghi, E., Aguenaou, H., Ammari, L. E., Abul-Fadl, A., & McColl, K. (2020). Tackling Childhood Stunting in the Eastern Mediterranean Region in the Context of COVID-19. Children, 7(11), 239. https://doi.org/10.3390/children7110239









