Association between Regional Tissue Oxygenation and Body Temperature in Term and Preterm Infants Born by Caesarean Section
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Postnatal Stabilization and Temperature Management
2.3. Near-Infrared Spectroscopy
2.4. Data Collection
2.5. Group Stratification
2.6. Statistics
3. Results
3.1. Characteristics
3.2. Oxygenation
3.3. Body Temperature
3.4. Respiratory Support
3.5. Short-Term Outcome
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization; Maternal; Newborn Health. Thermal Protection of the Newborn: A Practical Guide; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Knobel, R.B.; Holditch-Davis, D.; Schwartz, T.A. Optimal Body Temperature in Transitional Extremely Low Birth Weight Infants Using Heart Rate and Temperature as Indicators. J. Obstet. Gynecol. Neonatal Nurs. 2010, 39, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Y.; Shah, P.S.; Ye, X.Y.; Warre, R.; Piedboeuf, B.; Deshpandey, A.; Dunn, M.; Lee, S.K.; Harrison, A.; Synnes, A.; et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33weeks’ gestation. JAMA Pediatrics 2015, 169, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Christidis, I.; Zotter, H.; Rosegger, H.; Engele, H.; Kurz, R.; Kerbl, R. Infrared Thermography in Newborns: The First Hour after Birth. Gynakol. Geburtshilfliche. Rundsch. 2003, 43, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Morley, C.J.; Hewson, P.H.; Thornton, A.J.; Cole, T.J. Axillary and rectal temperature measurements in infants. Arch. Dis. Child. 1992, 67, 122–125. [Google Scholar] [CrossRef] [PubMed]
- Takayama, J.I.; Teng, W.; Uyemoto, J.; Newman, T.B.; Pantell, R.H. Body temperature of newborns: What is normal? Clin. Pediatrics 2000, 39, 503–510. [Google Scholar] [CrossRef]
- Miller, S.S.; Lee, H.C.; Gould, J.B. Hypothermia in very low birth weight infants: Distribution, risk factors and outcomes. J. Perinatol. 2011, 31, S49. [Google Scholar] [CrossRef]
- Lunze, K.; Bloom, D.E.; Jamison, D.T.; Hamer, D.H. The global burden of neonatal hypothermia: Systematic review of a major challenge for newborn survival. BMC Med. 2013, 11, 24. [Google Scholar] [CrossRef]
- Wilson, E.; Norman, M.; Wilson, E.; Norman, M.; Wilson, E.; Maier, R.F.; Misselwitz, B.; Howell, E.A.; Zeitlin, J.; Zeitlin, J.; et al. Admission Hypothermia in Very Preterm Infants and Neonatal Mortality and Morbidity. J. Pediatrics 2016, 175, 61–67.e4. [Google Scholar] [CrossRef]
- Baumgart, S. Iatrogenic Hyperthermia and Hypothermia in the Neonate. Clin. Perinatol. 2008, 35, 183–197. [Google Scholar] [CrossRef]
- Pichler, G.; Pocivalnik, M.; Riedl, R.; Pichler-Stachl, E.; Morris, N.; Zotter, H.; Müller, W.; Urlesberger, B. “Multi-associations”: Predisposed to misinterpretation of peripheral tissue oxygenation and circulation in neonates. Physiol. Meas. 2011, 32, 1025–1034. [Google Scholar] [CrossRef]
- Kattwinkel, J.; Perlman, J.M.; Aziz, K.; Colby, C.; Fairchild, K.; Gallagher, J.; Hazinski, M.F.; Halamek, L.P.; Kumar, P.; Little, G.; et al. Part 15: Neonatal Resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122, S909–S919. [Google Scholar] [CrossRef] [PubMed]
- Wyllie, J.; Bruinenberg, J.; Roehr, C.C.; Rüdiger, M.; Trevisanuto, D.; Urlesberger, B. European Resuscitation Council Guidelines for Resuscitation 2015. Section 7. Resuscitation and support of transition of babies at birth. Resuscitation 2015, 95, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Pichler, G.; Binder, C.; Avian, A.; Beckenbach, E.; Schmölzer, G.M.; Urlesberger, B. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J. Pediatrics 2013, 163, 1558–1563. [Google Scholar] [CrossRef] [PubMed]
- Gaasch, M.; Putzer, G.; Schiefecker, A.J.; Martini, J.; Strapazzon, G.; Ianosi, B.; Thome, C.; Paal, P.; Brugger, H.; Mair, P.; et al. Cerebral Autoregulation is Impaired During Deep Hypothermia—A Porcine Multimodal Neuromonitoring Study. Ther. Hypothermia Temp. Manag. 2020, 10, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.J.; da Costa, C.S.; Austin, T.; Brady, K.M.; Czosnyka, M.; Lee, J.K. Neonatal cerebrovascular autoregulation. Pediatric Res. 2018, 84, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Weindling, M.; Paize, F. Peripheral haemodynamics in newborns: Best practice guidelines. Early Hum. Dev. 2010, 86, 159–165. [Google Scholar] [CrossRef]
- Lubkowska, A.; Szymański, S.; Chudecka, M. Surface body temperature of full-term healthy newborns immediately after Birth—Pilot study. Int. J. Environ. Res. Public Health 2019, 16, 1312. [Google Scholar] [CrossRef]
- Knobel, R.B.; Guenther, B.D.; Rice, H.E. Thermoregulation and Thermography in Neonatal Physiology and Disease. Biol. Res. Nurs. 2011, 13, 274–282. [Google Scholar] [CrossRef]
- Anderson, P.A.W.; Kleinman, C.S.; Lister, G.; Talner, N. Cardiovascular Function During Normal Fetal and Neonatal Development and with Hypoxic Stress. In Fetal and Neonatal Physiology; Elsevier: Amsterdam, The Netherlands, 1998. [Google Scholar]
- Davies, P.; Maconochie, I. The relationship between body temperature, heart rate and respiratory rate in children. Emerg. Med. J. 2009, 26, 641–643. [Google Scholar] [CrossRef]
- Mitra, S.; Bale, G.; Meek, J.; Uria-Avellanal, C.; Robertson, N.J.; Tachtsidis, I. Relationship Between Cerebral Oxygenation and Metabolism During Rewarming in Newborn Infants After Therapeutic Hypothermia Following Hypoxic-Ischemic Brain Injury. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2016; pp. 245–251. [Google Scholar]
- Wu, T.W.; Tamrazi, B.; Soleymani, S.; Seri, I.; Noori, S. Hemodynamic Changes During Rewarming Phase of Whole-Body Hypothermia Therapy in Neonates with Hypoxic-Ischemic Encephalopathy. J. Pediatrics 2018, 197, 68–74.e2. [Google Scholar] [CrossRef]
- De Almeida, M.F.B.; Guinsburg, R.; Sancho, G.A.; Rosa, I.R.M.; Lamy, Z.C.; Martinez, F.E.; Da Silva, R.P.G.V.C.; Ferrari, L.S.L.; De Souza Rugolo, L.M.S.; Abdallah, V.O.S.; et al. Hypothermia and early neonatal mortality in preterm infants. J. Pediatrics 2014, 164, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Laptook, A.R.; Salhab, W.; Bhaskar, B. Admission Temperature of Low Birth Weight Infants: Predictors and Associated Morbidities. Pediatrics 2007, 119, e643–e649. [Google Scholar] [CrossRef] [PubMed]
- Finn, D.; Ryan, D.H.; Pavel, A.; O’Toole, J.M.; Livingstone, V.; Boylan, G.B.; Kenny, L.C.; Dempsey, E.M. Clamping the Umbilical Cord in Premature Deliveries (CUPiD): Neuromonitoring in the Immediate Newborn Period in a Randomized, Controlled Trial of Preterm Infants Born at <32 Weeks of Gestation. J. Pediatrics 2019, 208, 121–126.e2. [Google Scholar] [CrossRef] [PubMed]
- Pichler, G.; Baik, N.; Urlesberger, B.; Cheung, P.-Y.; Aziz, K.; Avian, A.; Schmölzer, G.M. Cord clamping time in spontaneously breathing preterm neonates in the first minutes after birth: Impact on cerebral oxygenation—A prospective observational study. J. Matern. Neonatal Med. 2016, 29, 1570–1572. [Google Scholar] [CrossRef] [PubMed]
- Katheria, A.C.; Brown, M.K.; Faksh, A.; Hassen, K.O.; Rich, W.; Lazarus, D.; Steen, J.; Daneshmand, S.S.; Finer, N.N. Delayed Cord Clamping in Newborns Born at Term at Risk for Resuscitation: A Feasibility Randomized Clinical Trial. J. Pediatrics 2017, 187, 313–317.e1. [Google Scholar] [CrossRef]
- Russo, A.; McCready, M.; Torres, L.; Theuriere, C.; Venturini, S.; Spaight, M.; Hemway, R.J.; Handrinos, S.; Perlmutter, D.; Huynh, T.; et al. Reducing Hypothermia in Preterm Infants Following Delivery. Pediatrics 2014, 133, e1055–e1062. [Google Scholar] [CrossRef]
- Pinheiro, J.M.B.; Furdon, S.A.; Boynton, S.; Dugan, R.; Reu-Donlon, C.; Jensen, S. Decreasing Hypothermia During Delivery Room Stabilization of Preterm Neonates. Pediatrics 2014, 133, e218–e226. [Google Scholar] [CrossRef]
- Committee on Accident and Poison Prevention. Hyperthermia from malfunctioning radiant heaters. Pediatrics 1977, 59, 1041. [Google Scholar]
- Vohra, S.; Roberts, R.S.; Zhang, B.; Janes, M.; Schmidt, B. Heat Loss Prevention (HeLP) in the delivery room: A randomized controlled trial of polyethylene occlusive skin wrapping in very preterm infants. J. Pediatrics 2004, 145, 750–753. [Google Scholar] [CrossRef]
- Newton, T. Preventing hypothermia at birth in preterm babies: At a cost of overheating some? Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F256. [Google Scholar] [CrossRef]
- Lenclen, R.; Mazraani, M.; Jugie, M.; Couderc, S.; Hoenn, E.; Carbajal, R.; Blanc, P.; Paupe, A. Use of a polyethylene bag: A way to improve the thermal environment of the premature newborn at the delivery room. Arch. Pediatrie 2002, 9, 238–244. [Google Scholar] [CrossRef]
- Meyer, M.P.; Owen, L.S.; te Pas, A.B. Use of Heated Humidified Gases for Early Stabilization of Preterm Infants: A Meta-Analysis. Front. Pediatrics 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Falzon, A.; Grech, V.; Caruana, B.; Magro, A.; Attard-Montalto, S. How reliable is axillary temperature measurement? Acta Paediatr. 2003, 92, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.V.; Lancaster, G.A.; Williamson, P.R.; Smyth, R.L. Temperature measured at the axilla compared with rectum in children and young people: Systematic review. BMJ 2000, 320, 1174–1178. [Google Scholar] [CrossRef]
| Total (n = 586) | Term (n = 417) | Preterm (n = 169) | p-Value | EPI (n = 10) | VPI (n = 38) | LPI (n = 121) | |
|---|---|---|---|---|---|---|---|
| GA (weeks) | 39 (36–39) | 39 (38–39) | 34 (32–35) | <0.001 | 26 (24–27) | 31 (30–31) | 34 (33–36) |
| Apgar 1 | 9 (8–9) | 9 (9–9) | 8 (8–9) | <0.001 | 8 (8–9) | 8 (7–8) | 8 (8–9) |
| Apgar 5 | 10 (9–10) | 10 (10–10) | 9 (8–10) | <0.001 | 8 (6–8) | 9 (8–9) | 9 (9–10) |
| Apgar 10 | 10 (10–10) | 9 (9–10) | 10 (10–10) | <0.001 | 9 (9–10) | 9 (9–10) | 10 (9–10) |
| BW (grams) | 3088 (2380–3460) | 3290 (2996–3590) | 1830 (1438–2260) | <0.001 | 700 (626–906) | 1330 (1054–1564) | 2040 (1756–2400) |
| pHa | 7.30 (7.28–7.32) | 7.30 (7–28-7.32) | 7.31 (7.28–7.34) | 0.004 | 7.33 (7.31–7.39) | 7.32 (7.29–7.34) | 7.30 (7.27–7.33) |
| MABP (mmHg) | 45 ± 10 | 47 ± 9 | 40 ± 9 | <0.001 | 31 ± 7 | 38 ± 8 | 41 ± 9 |
| SpO2 (%) | 95.1 (91.7–97.7) | 95.7 (92.7–97.9) | 93.5 (88.5–96.8) | <0.001 | 92.6 (72.1–96.1) | 90.4 (86.9–93.8) | 94.5 (91.1–97.3) |
| Heart rate (bpm) | 154 ± 18 | 153 ± 18 | 156 ± 18 | 0.015 | 159 ± 17 | 161 ± 16 | 154 ± 18 |
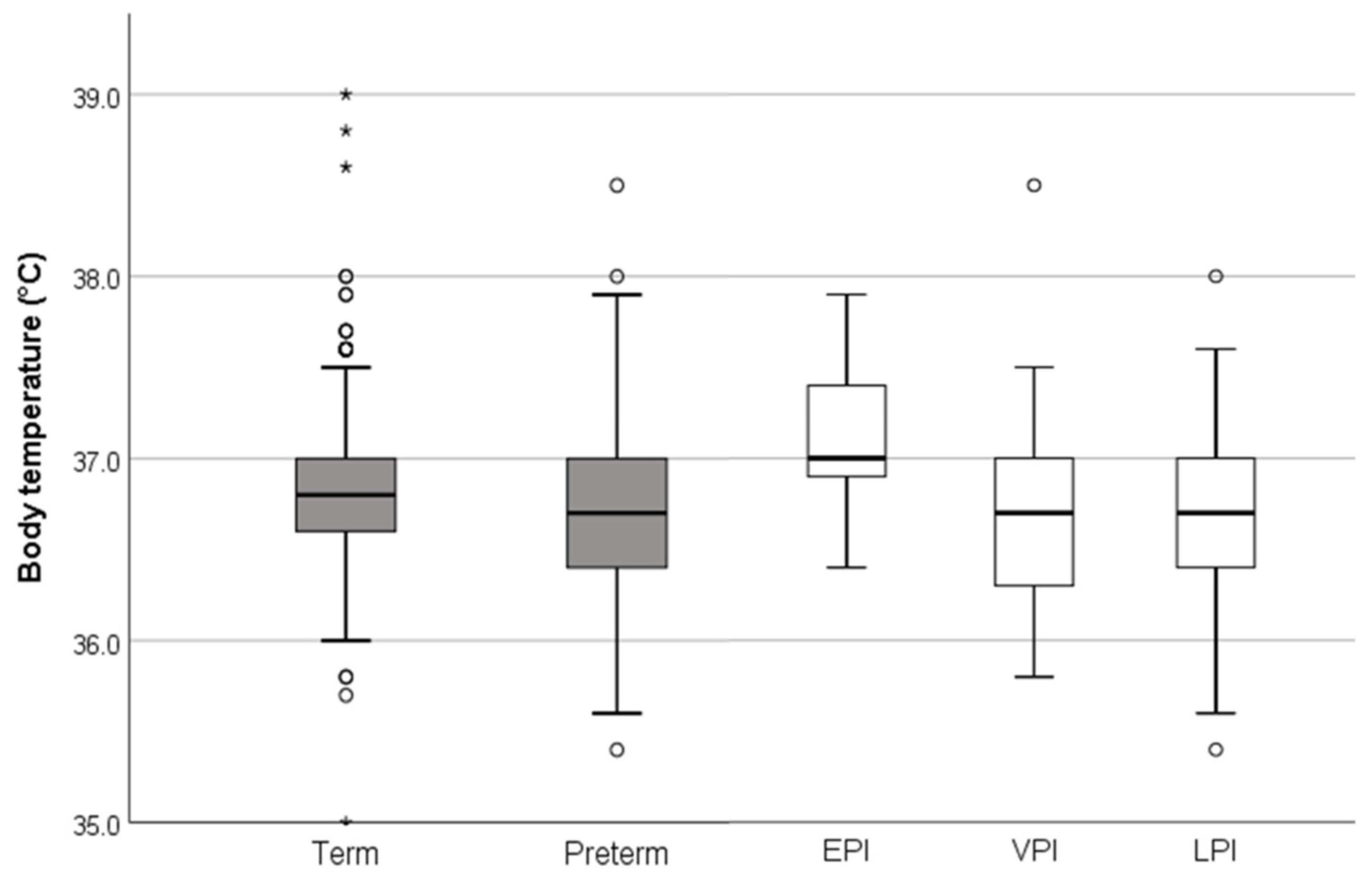
| Body temperature (°C) | 36.8 (36.6–37.0) | 36.8 (36.6–37.0) | 36.7 (36.4–37.0) | 0.001 | 37.0 (36.9–37.4) | 36.7(36.3–37.0) | 36.7 (36.4–37.0) |
| crSO2/cTOI (n) | 458 | 342 | 116 | 5 | 22 | 89 | |
| crSO2/cTOI (%) | 78.9 (71.0–86.0) | 78.4 (71.0–85.0) | 79.0 (68.7–87.5) | 0.853 | 79.6 (75.6–91.1) | 71.7 (62.0–79.0) | 80.0 (72.0–89.0) |
| prSO2 (n) | 355 | 289 | 66 | 1 | 9 | 56 | |
| prSO2 (%) | 74.0 (63.0–85.0) | 74.0 (63.0–85.0) | 73.0 (62.0–87.0) | 0.728 | 69.0 (69.0–69.0) | 65.0 (51.0–75.0) | 76 (63–87.5) |
| pFTOE | 0.23 (0.12–0.34) | 0.22 (0.12–0.34) | 0.23 (0.11–0.30) | 0.596 | 0.28 (0.28–0.28) | 0.24 (0.16–0.40) | 0.23 (0.09–0.29) |
| Total Cohort (n = 586) | Term (n = 417) | Preterm (n = 169) | ||||
|---|---|---|---|---|---|---|
| Body Temperature (°C) | p-Value | Body Temperature (°C) | p-Value | Body Temperature (°C) | p-Value | |
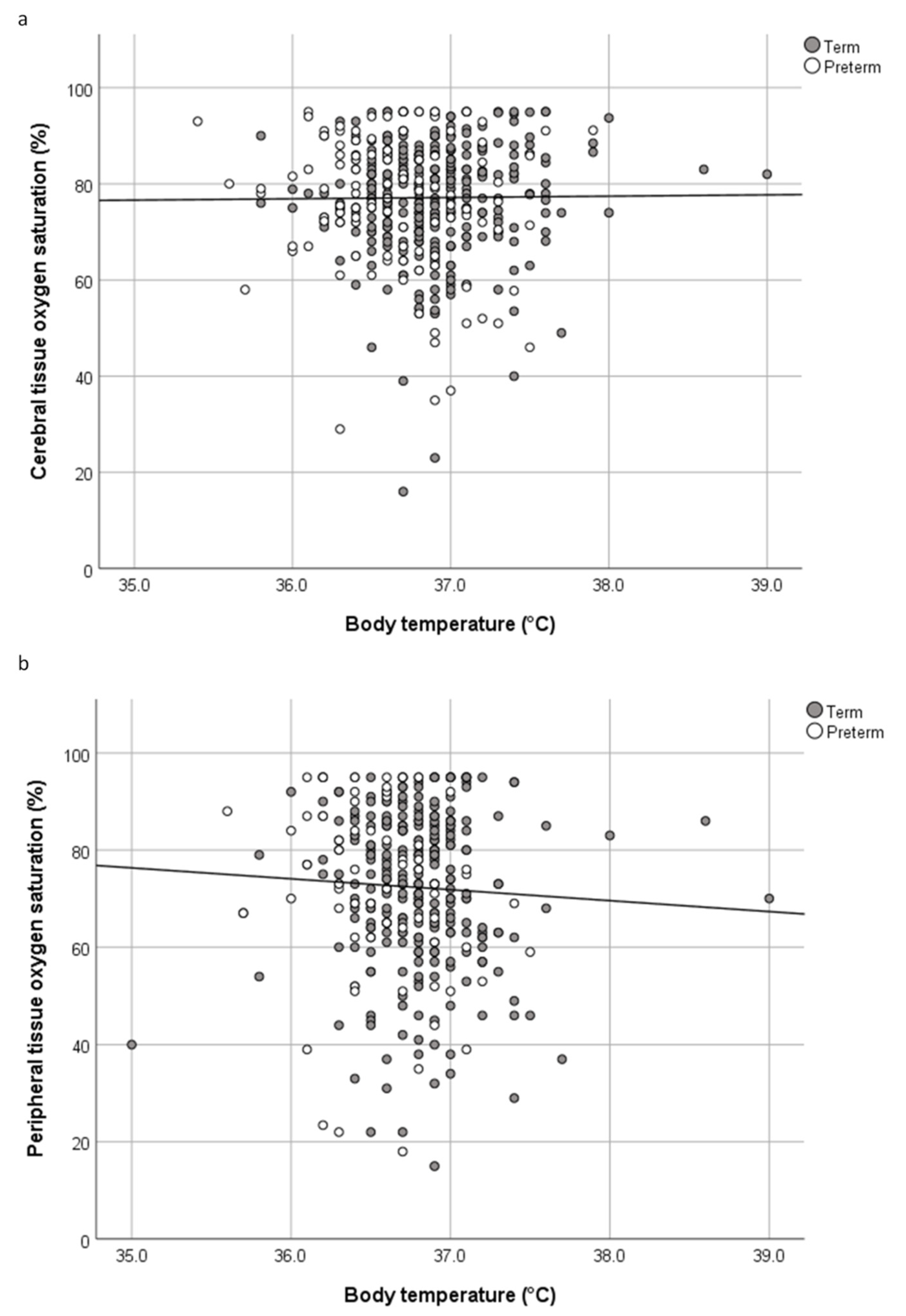
| crSO2/cTOI (%) | ρ = 0.018 | 0.701 | ρ = 0.077 | 0.155 | ρ = −0.102 | 0.275 |
| prSO2 (%) | ρ = −0.092 | 0.084 | ρ = −0.044 | 0.461 | ρ = −0.285 | 0.020 |
| pFTOE | ρ = 0.042 | 0.443 | ρ = 0.011 | 0.852 | ρ = 0.165 | 0.195 |
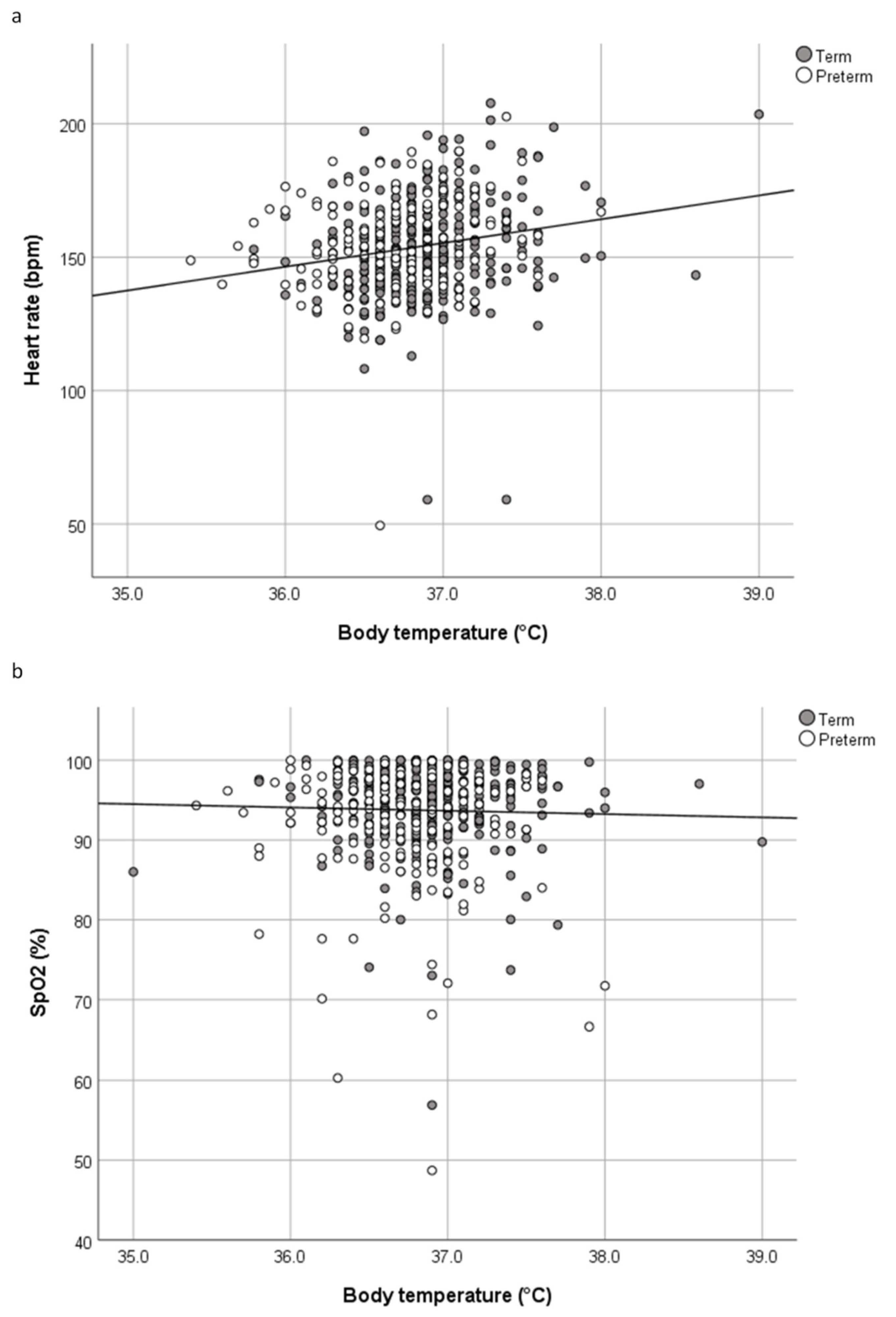
| Heart rate (bpm) | ρ = 0.210 | <0.001 | ρ = 0.236 | <0.001 | ρ = 0.222 | <0.006 |
| SpO2 (%) | ρ = −0.015 | 0.741 | ρ = −0.013 | 0.805 | ρ = −0.125 | 0.111 |
| Total (n = 586) | Term (n = 417) | Preterm (n = 169) | EPI (n = 10) | VPI (n = 38) | LPI (n = 121) | |
|---|---|---|---|---|---|---|
| Normothermia | 461 (78.7) | 347 (83.2) | 114 (67.5) | 7 (70.0) | 23 (60.5) | 84 (69.4) |
| Mild hypothermia | 89 (15.2) | 46 (11.0) | 43 (25.4) | 1 (10.0) | 11 (29.0) | 31 (25.6) |
| Moderate hypothermia | 11 (1.9) | 4 (1.0) | 7 (4.1) | 0 (0.0) | 3 (7.9) | 4 (3.3) |
| Hyperthermia | 25 (4.3) | 20 (4.8) | 5 (3.0) | 2 (20.0) | 1 (2.6) | 2 (1.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruckner, M.; Mileder, L.P.; Richter, A.; Baik-Schneditz, N.; Schwaberger, B.; Binder-Heschl, C.; Urlesberger, B.; Pichler, G. Association between Regional Tissue Oxygenation and Body Temperature in Term and Preterm Infants Born by Caesarean Section. Children 2020, 7, 205. https://doi.org/10.3390/children7110205
Bruckner M, Mileder LP, Richter A, Baik-Schneditz N, Schwaberger B, Binder-Heschl C, Urlesberger B, Pichler G. Association between Regional Tissue Oxygenation and Body Temperature in Term and Preterm Infants Born by Caesarean Section. Children. 2020; 7(11):205. https://doi.org/10.3390/children7110205
Chicago/Turabian StyleBruckner, Marlies, Lukas P. Mileder, Alisa Richter, Nariae Baik-Schneditz, Bernhard Schwaberger, Corinna Binder-Heschl, Berndt Urlesberger, and Gerhard Pichler. 2020. "Association between Regional Tissue Oxygenation and Body Temperature in Term and Preterm Infants Born by Caesarean Section" Children 7, no. 11: 205. https://doi.org/10.3390/children7110205
APA StyleBruckner, M., Mileder, L. P., Richter, A., Baik-Schneditz, N., Schwaberger, B., Binder-Heschl, C., Urlesberger, B., & Pichler, G. (2020). Association between Regional Tissue Oxygenation and Body Temperature in Term and Preterm Infants Born by Caesarean Section. Children, 7(11), 205. https://doi.org/10.3390/children7110205






