Stability and Change in Longitudinal Associations between Child Behavior Problems and Maternal Stress in Families with Preterm Born Children, Follow-Up after a RCT-Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Design of the Intervention
2.2. Data Collection
2.3. Plan of Analysis
2.4. Ethical Approval
3. Results
3.1. Initial Exploration of Correlations
3.2. Longitudinal Associations between Children’s Internalizing Behavior and Parenting Stress
3.3. Longitudinal Associations between Children’s Social Problems and Parenting Stress
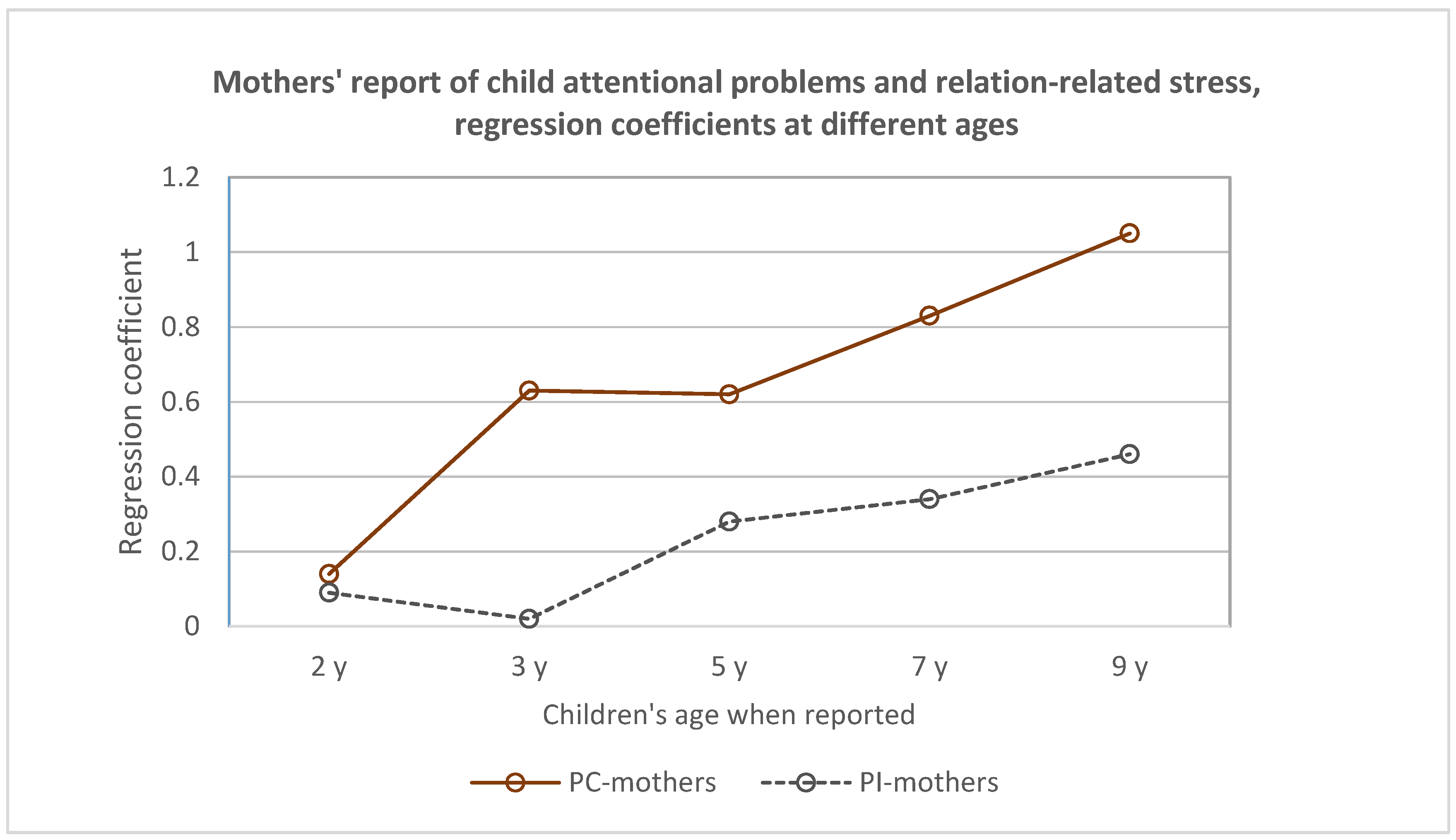
3.4. Longitudinal Associations between Children’s Attentional Problems and Three Dimensions of Parenting Stress
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BW | Birthweight |
| CBCL | Child Behavior Checklist |
| GA | Gestational age |
| MITP | Mother-Infant Transaction Program |
| MITP-m | Mother-Infant Transaction Program, modified version |
| NICU | Neonatal intensive care unit |
| PC | Preterm control group |
| PI | Preterm intervention group |
| PSI | Parenting Stress Index |
| P-CDI | PSI dimension, Parent–child difficult interaction |
| TISP | Tromsø Intervention Study on Preterms |
Appendix A
| Fixed Effect Variables | Child-Related Stress (DC) as Independent Predictor | Parent-Related Stress (PD) as Independent Predictor | Relation-Related Stress (P-CDI) as Independent Predictor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | |
| Intercept | 19.7 | 4.8 | <0.0005 | 25.5 | 5.9 | <0.0005 | 35.6 | 12.7 | <0.0005 |
| Group | 5.6 | 1.0 | 0.32 | 4.9 | 0.8 | 0.45 | −0.9 | −0.2 | 0.84 |
| Time | 2.8 | 2.7 | 0.01 | 1.7 | 1.5 | 0.13 | 0.9 | 0.1 | 0.12 |
| Group*Time | −2.1 | −1.4 | 0.16 | −2.5 | −1.5 | 0.13 | −0.3 | 0.7 | 0.78 |
| Stress | 0.3 | 6.4 | <0.0005 | 0.2 | 4.7 | <0.0005 | 0.5 | 3.7 | <0.0005 |
| Time*Stress | −0.1 | −2.4 | 0.02 | -0.1 | −1.3 | 0.21 | −0.1 | −1.1 | 0.29 |
| Group*Stress | −0.1 | −2.4 | 0.24 | −0.1 | −0.6 | 0.52 | 0.1 | 0.4 | 0.71 |
| Group*Stress*Time | 0.1 | 1.4 | 0.17 | 0.1 | 1.3 | 0.18 | <0.1 | 0.2 | 0.87 |
| Fixed Effect Variables | Child-Related Stress (DC) as Independent Predictor | Parent-Related Stress (PD) as Independent Predictor | Relation-Related Stress (P-CDI) as Independent Predictor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | |
| Intercept | 46.5 | 34.5 | <0.0005 | 50.9 | 47.4 | <0.0005 | 50.2 | 55.2 | <0.0005 |
| Group | 0.4 | 0.2 | 0.86 | 0.3 | 0.2 | 0.86 | 0.9 | 0.6 | 0.56 |
| Time | 0.8 | 2.7 | 0.01 | 0.4 | 1.6 | 0.10 | 0.4 | 1.5 | 0.14 |
| Group*Time | 0.1 | 0.1 | 0.92 | −0.3 | 0.7 | 0.51 | −0.1 | −0.3 | 0.77 |
| Stress | 0.4 | 4.8 | <0.0005 | 0.2 | 1.9 | 0.06 | 0.3 | 3.3 | <0.0005 |
| Time*Stress | −0.1 | −1.2 | 0.22 | <−0.2 | −1.0 | 0.33 | −0.1 | −0.5 | 0.63 |
| Group*Stress | −0.1 | −0.4 | 0.68 | <0.1 | 0.4 | 0.67 | −0.1 | −0.3 | 0.73 |
| Group*Stress*Time | −0.1 | −0.2 | 0.81 | <0.1 | 0.6 | 0.57 | −0.1 | −0.2 | 0.84 |
References
- Deater-Deckard, K.; Bulkley, J. Parent concerns in long-term follow-up. Semin. Neonatol. 2000, 5, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Spittle, A.; Treyvaud, K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin. Perinatol. 2016, 40, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Howell, C.T.; Aoki, M.; Rauh, V.A. Nine-year outcome of the Vermont Intervention Program for low birth-weight infants. Pediatrics 1993, 93, 45–55. [Google Scholar]
- Kaaresen, P.I.; Rønning, J.A.; Ulvund, S.E.; Dahl, L.B. A randomized controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics 2006, 118, e9-19. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, J.; Newnham, C.; Martin, P.R.; Anderson, P.J.; Doyle, L.W.; Hunt, R.W.; Achenbach, T.M.; Ferretti, C.; Holt, C.J.; Inder, T.E.; et al. Early communication in preterm infants following intervention in the NICU. Early Hum. Dev. 2013, 89, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Landsem, I.P.; Handegård, B.H.; Ulvund, S.E.; Tunby, J.; Kaaresen, P.I.; Rønning, J.A. Does an early intervention influence behavioral development until age nine of children born prematurely? Child Dev. 2015, 86, 1063–1079. [Google Scholar] [CrossRef]
- Putthussery, S.; Chutiyami, M.; Tseng, P.-C.; Kilby, L.; Kapadia, J. Effectiveness of early intervention programs for parents of preterm infants: A meta-review of systematic reviews. BMC Pediatr. 2018, 18, 223. [Google Scholar] [CrossRef]
- Deater-Deckard, K. Parenting Stress; Yale University Press: New Haven, CT, USA; London, UK, 2004. [Google Scholar]
- Treyvaud, K.; Doyle, L.W.; Lee, K.; Roberts, G.; Cheong, J.L.Y.; Inder, T.E.; Anderson, P.J. Family functioning, burden and parenting stress 2 years after very preterm birth. Early Hum. Dev. 2011, 87, 427–431. [Google Scholar] [CrossRef]
- Deater-Deckard, K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clin. Psychol. Sci. Pract. 1998, 3, 314–332. [Google Scholar] [CrossRef]
- Crnic, K.A.; Gaze, C.; Hoffman, C. Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behavior at age 5. Inf. Child Dev. 2005, 14, 117–132. [Google Scholar] [CrossRef]
- Abidin, R.R. Parenting Stress Index, Professional Manual, 3rd ed.; PAR Psychological Assessment Resources, Inc.: Odessa, TX, USA, 1995. [Google Scholar]
- Pedersen, A.L.; Crnic, K.A.; Baker, B.L.; Blacher, J. Reconceptualizing family adaptation to developmental delay. Am. J. Intellect. Dev. Disabil. 2015, 120, 346–370. [Google Scholar] [CrossRef] [PubMed]
- Sameroff, A.J.; Fiese, B. Transactional regulation: The developmental ecology of early intervention. In Handbook of Early Childhood Intervention; Shonkoff, J., Meisel, S., Eds.; Cambridge University Press: Cambridge, UK, 2000; pp. 135–159. [Google Scholar]
- Tu, M.T.; Grunau, R.E.; Petrie-Thomas, J.; Haley, D.W.; Weinberg, J.; Whitfield, M.F. Maternal stress and behavior modulate relationships between neonatal stress, attention, and basal cortisol at 8 months in preterm infants. Dev. Psychobiol. 2007, 49, 150–164. [Google Scholar] [CrossRef] [PubMed]
- Hall, R.A.S.; Hoffenkamp, H.N.; Tooten, A.; Braeken, J.; Vingerhoets, A.J.; van Bakel, H.J.A. The quality of parent-infant interaction in the first 2 years after full-term and preterm birth. Parent Sci. Pract. 2015, 15, 247–268. [Google Scholar] [CrossRef]
- Als, H. Toward a synactive theory of development: Promise for the assessment and the support of infant individuality. Infant Ment. Health 1982, 3, 229–243. [Google Scholar] [CrossRef]
- Feldman, R. Intervention programs for premature infants: Considering potential mechanisms for change. Signal World ASS Infant Ment. Health 2002, 10, 1–11. [Google Scholar]
- Feldman, R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev. Psychol. 2006, 42, 175–188. [Google Scholar] [CrossRef] [PubMed]
- Singer, L.T.; Fulton, S.; Davillier, M.; Koshy, D.; Salvator, A.; Baley, J.E. Effects of infant risk status and maternal psychological distress on maternal-infant interactions during the first years of life. J. Dev. Behav. Pediatr. 2003, 24, 233–241. [Google Scholar] [CrossRef]
- Forcada-Guex, M.; Pierrehumbert, B.; Borghini, A.; Moessinger, A.; Muller-Nix, C. Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics 2006, 118, e107–e114. [Google Scholar] [CrossRef]
- Gerstein, E.D.; Poehlmann-Tynan, J. Transactional processes in children born preterm: Influences of mother-child interactions and parenting stress. J. Fam. Psychol. 2015, 29, 777–787. [Google Scholar] [CrossRef]
- Gueron-Sela, N.; Atzaba-Poria, N.; Meiri, G.; Marks, K. The care-giving environment and developmental outcomes of preterm infants: Diathesis stress or differential susceptibility effects? Child Dev. 2015, 86, 1014–1030. [Google Scholar] [CrossRef]
- Achenbach, T. Manual for the Child Behavior Checklist/4-18 and 1991 Profile; University of Vermont: Burlington, VT, USA, 1991. [Google Scholar]
- Achenbach, T.M. Manual for the Child Behavior Checklist/2-3 and 1992 Profile; University of Vermont: Burlington, VT, USA, 1992. [Google Scholar]
- Landsem, I.P.; Handegård, B.H.; Ulvund, S.E.; Tunby, J.; Rønning, J.A. Early intervention program reduces stress in parents of preterms during childhood, a randomized controlled trial. Trials 2014, 15, 387. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.S.; Kopin, I.J. Evolution of concepts of stress. Stress 2007, 10, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Aarnoudse-Moens, C.S.H.; Weisglas-Kuperus, N.; van Goudoever, J.B.; Oosterlaan, J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low-birth-weight children. Pediatrics 2009, 124, 717–728. [Google Scholar] [CrossRef] [PubMed]
- Nordhov, S.M.; Rønning, J.A.; Ulvund, S.E.; Dahl, L.B.; Kaaresen, P.I. Early intervention improves behavioral outcomes for preterm infants: Randomized controlled trial. Pediatrics 2012, 129, e9–e16. [Google Scholar] [CrossRef] [PubMed]
- Rauh, V.A.; Nurcombe, B.; Achenbach, T.; Howell, C. The Mother-Infant Transaction Program. The content and implications of an intervention for the mothers of low- birthweight infants. Clin. Perinatol. 1990, 17, 31–45. [Google Scholar] [CrossRef]
- PAR. Assessment of Parenting Stress and the PSI-4 SF. Creating Connections, Changing Lives. Presentation from Psychological Assessment Resources Inc. 2017, Downloaded to UiT The Arctic University of Norway 01.02.2017. Available online: https://en.uit.no/startsida (accessed on 31 January 2019).
- Singer, J.D.; Willett, J.B. Applied Longitudinal Data Analysis, Modeling Change and Event Occurrence; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Peugh, J.L.; Enders, C.K. Using the SPSS mixed procedure to fit cross-sectional and longitudinal multilevel models. Educ. Psychol. Meas. 2005, 65, 717–741. [Google Scholar] [CrossRef]
- Nugent, J.K.; Keefer, C.H.; Minear, S.; Johnson, L.C.; Blanchard, Y. Understanding Newborn Behavior & Early Relationships. In The Newborn Behavioral Observations (NBO) System Handbook; Brookes Publishing: Baltimore, MD, USA; London, UK; Sidney, Australia, 2007. [Google Scholar]
- Landry, S.H.; Smith, K.E.; Swank, P.R. Responsive parenting: Establishing early foundations for social, communication, and independent problem-solving skills. Dev. Psychol. 2006, 42, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Poehlmann, J.; Fiese, B.H. The interaction of maternal and infant vulnerabilities on developing attachment relationships. Dev. Psychopathol. 2001, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Olafsen, K.S.; Rønning, J.A.; Kaaresen, P.I.; Ulvund, S.E.; Handegård, B.H.; Dahl, L.B. Joint attention in term and preterm infants at 12 months corrected age: The significance of gender and intervention based on a randomized controlled trial. Infant Behav. Dev. 2006, 29, 554–563. [Google Scholar] [CrossRef]
- Guralnick, M.J.; Hammond, M.A.; Neville, B.; Connor, R.T. The relationship between sources and functions of social support and dimensions of child- and parent-related stress. J. Intellect. Disabil. Res. 2008, 52, 1138–1154. [Google Scholar] [CrossRef]
- Downey, L.C.; O’Shea, T.M.; Allred, E.N.; Kuban, K.; McElrath, T.F.; Warner, D.D.; Ware, J.; Hecht, J.L.; Onderdonk, A.; Leviton, A. Antenatal and early postnatal antecedents of parent-reported attention problems at 2 years of age. J. Pediatr. 2015, 166, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Morales, M.R.; Polizzi, C.; Sulliotti, G.; Perricone, G. Early precursors of low attention and hyperactivity in moderately and very preterm children at preschool age. Pediatr. Rep. 2013, 5, e18. [Google Scholar] [CrossRef] [PubMed]
- Polderman, T.J.; de Geus, E.J.; Hoekstra, R.A.; Bartels, M.; van Leeuwen, M.; Verhulst, F.C.; Posthuma, D.; Boomsma, D.I. Attention problems, inhibitory control, and intelligence index overlapping genetic factors: A study in 9, 12, and 18-year-old twins. Neuropsychology 2009, 23, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Groen-Blokhuis, M.M.; Middeldorp, C.M.; van Beijsterveldt, C.E.M.; Boomsma, D.I. Evidence for a causal association of low-birth-weight and attention problems. J. Am. Acad. Child Adolescent. Psychiat. 2011, 50, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Leijten, P.; Raaijmakers, M.A.J.; de Castro, B.O.; Matthys, W. Does socioeconomic status matter? A meta-analysis on parent training effectiveness for disruptive child behavior. J. Clin. Child Adolescent. Psychol. 2013, 42, 384–392. [Google Scholar] [CrossRef] [PubMed]
| PI Group n = 72 | PC Group n = 74 | |
|---|---|---|
| Infant characteristics | ||
| BW, mean ± SD, grams | 1396 ± 429 | 1381 ± 436 |
| 400–1000 grams, n (%) | 20 (28) | 20 (27) |
| 1001–1500 grams, n (%) | 15 (21) | 20 (27) |
| 1501–2000 grams, n (%) | 37 (51) | 34 (46) |
| GA, mean ± SD, week | 30.2 ± 3.1 | 29.9 ± 3.5 |
| <28-week, n (%) | 17 (24) | 19 (27) |
| 28–32-week, n (%) | 36 (50) | 37 (50) |
| >33-week, n (%) | 19 (26) | 18 (24) |
| Boy, n (%) | 38 (53) | 39 (53) |
| Twin, n (%) | 16 (22) | 16 (21) |
| Received ventilation, n (%) Duration of ventilation, n (%) Postnatal steroid use, n (%) Oxygen therapy at 38-week GA, n (%) | 29 (40) 7.0 ± 18.6 9 (13) 11 (15) | 37 (50) 7.1 ± 17.3 10 (14) 14 (19) |
| Abnormal cerebral ultrasound, n (%) | ||
| IVH grade 1 or 2 | 7 (10) | 8 (11) |
| IVH grade 3 or 4 | 3 (4) | 5 (7) |
| Periventricular leukomalacia | 4 (6) | 8 (11) |
| Maternal and social characteristics | ||
| Mother’s age a, mean ± SD | 30.8 ± 6.1 | 29.1 ± 6.4 |
| First-born child, n (%) | 40 (56) | 37 (54) |
| Mother’s education a, mean ± SD, n = 131 | 14.6 ± 2.8 | 13.5 ± 3.2 |
| Father’s education a, mean ± SD, n = 131 | 13.8 ± 3.1 | 13.5 ± 3.2 |
| Mother’s monthly income b, mean ± SD, n = 131 | 15.8 ± 7.7 | 14.6 ± 6.7 |
| Father’s monthly income b, mean ± SD, n = 131 | 21.1 ± 8.7 | 19.9 ± 8.1 |
| Internalizing behavior | ||||||
| Group | Stress dimension | 2 y | 3 y | 5 y | 7 y | 9 y |
| PC mothers | Child-related | 0.44 ** | 0.48 ** | 0.54 ** | 0.62 ** | 0.71 ** |
| Parent-related | 0.32 * | 0.37 ** | 0.44 ** | 0.48 ** | 0.55 ** | |
| Interaction-related | 0.28 | 0.34 ** | 0.37 ** | 0.37 ** | 0.48 ** | |
| PI mothers | Child-related | 0.41 ** | 0.37 ** | 0.55 ** | 0.41 ** | 0.60 ** |
| Parent-related | 0.23 | 0.30 * | 0.43 ** | 0.31 * | 0.37 ** | |
| Interaction-related | 0.34 * | 0.27 * | 0.41 ** | 0.20 | 0.36 ** | |
| Attentional behavior problems | ||||||
| Group | Stress dimension | 2 y | 3 y | 5 y | 7 y | 9 y |
| PC mothers | Child-related | 0.09 | 0.50 ** | 0.44 ** | 0.58 ** | 0.59 ** |
| Parent-related | 0.25 | 0.49 ** | 0.23 | 0.45 ** | 0.50 ** | |
| Interaction-related | 0.17 | 0.54 ** | 0.45 ** | 0.48 ** | 0.68 ** | |
| PI mothers | Child-related | 0.25 | 0.17 | 0.37 ** | 0.49 ** | 0.58 ** |
| Parent-related | −0.01 | 0.01 | 0.41 ** | 0.37 ** | 0.12 | |
| Interaction-related | 0.11 | −0.02 | 0.38 ** | 0.35 ** | 0.39 ** | |
| Social behavior problems | ||||||
| Group | Stress dimension | 5 y | 7 y | 9 y | ||
| PC mothers | Child-related | 0.55 ** | 0.52 ** | 0.58 ** | ||
| Parent-related | 0.25 | 0.41 ** | 0.34 ** | |||
| Interaction-related | 0.50 ** | 0.43 ** | 0.49 ** | |||
| PI mothers | Child-related | 0.57 ** | 0.39 ** | 0.69 ** | ||
| Parent-related | 0.30 * | 0.35 ** | 0.23 | |||
| Interaction-related | 0.49 ** | 0.40 ** | 0.44 ** | |||
| Fixed Effect Variables | Child-Related Stress (DC) as Independent Predictor | Parent-Related Stress (PD) as Independent Predictor | Relation-Related Stress (P-CDI) as Independent Predictor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | Estimate | t-Value | p-Value | |
| Intercept | 50.01 | 43.77 | <0.0005 | 51.96 | 58.13 | <0.0005 | 52.19 | 68.06 | <0.0005 |
| Group | −0.96 | −0.71 | 0.50 | −1.54 | −1.32 | 0.19 | −2.05 | −1.97 | 0.04 |
| Time | −1.34 | −2.28 | 0.02 | −0.41 | −0.85 | 0.39 | −0.28 | −0.71 | 0.49 |
| Quadratic time | 0.22 | 3.05 | 0.003 | 0.08 | 1.38 | 0.17 | 0.06 | 1.13 | 0.28 |
| Group*Time | 0.13 | 0.29 | 0.78 | 0.65 | −1.45 | 0.15 | 0.36 | 0.78 | 0.42 |
| Group* Quadratic time | 0.02 | 0.31 | 0.75 | −0.04 | −0.70 | 0.49 | −0.02 | −0.29 | 0.78 |
| Stress | 0.16 | 2.17 | 0.03 | 0.02 | 0.28 | 0.78 | −0.08 | −0.10 | 0.83 |
| Time*Stress | 0.08 | 2.32 | 0.02 | 0.43 | 1.12 | 0.26 | 0.05 | 1.13 | 0.27 |
| Quadratic time *Stress | −0.01 | −2.29 | 0.02 | -0.004 | -0.91 | 0.36 | −0.004 | −0.67 | 0.51 |
| Group*Stress | 0.07 | 1.04 | 0.33 | 0.18 | 2.29 | 0.02 | 0.34 | 3.69 | <0.0005 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landsem, I.P.; Handegård, B.H.; Kaaresen, P.I.; Tunby, J.; Ulvund, S.E.; Rønning, J.A. Stability and Change in Longitudinal Associations between Child Behavior Problems and Maternal Stress in Families with Preterm Born Children, Follow-Up after a RCT-Study. Children 2019, 6, 19. https://doi.org/10.3390/children6020019
Landsem IP, Handegård BH, Kaaresen PI, Tunby J, Ulvund SE, Rønning JA. Stability and Change in Longitudinal Associations between Child Behavior Problems and Maternal Stress in Families with Preterm Born Children, Follow-Up after a RCT-Study. Children. 2019; 6(2):19. https://doi.org/10.3390/children6020019
Chicago/Turabian StyleLandsem, Inger P., Bjørn H. Handegård, Per I. Kaaresen, Jorunn Tunby, Stein E. Ulvund, and John A. Rønning. 2019. "Stability and Change in Longitudinal Associations between Child Behavior Problems and Maternal Stress in Families with Preterm Born Children, Follow-Up after a RCT-Study" Children 6, no. 2: 19. https://doi.org/10.3390/children6020019
APA StyleLandsem, I. P., Handegård, B. H., Kaaresen, P. I., Tunby, J., Ulvund, S. E., & Rønning, J. A. (2019). Stability and Change in Longitudinal Associations between Child Behavior Problems and Maternal Stress in Families with Preterm Born Children, Follow-Up after a RCT-Study. Children, 6(2), 19. https://doi.org/10.3390/children6020019





