Mothers’ Use of Social Media to Inform Their Practices for Pumping and Providing Pumped Human Milk to Their Infants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Longitudinal Design
2.2. Cross-Sectional Design
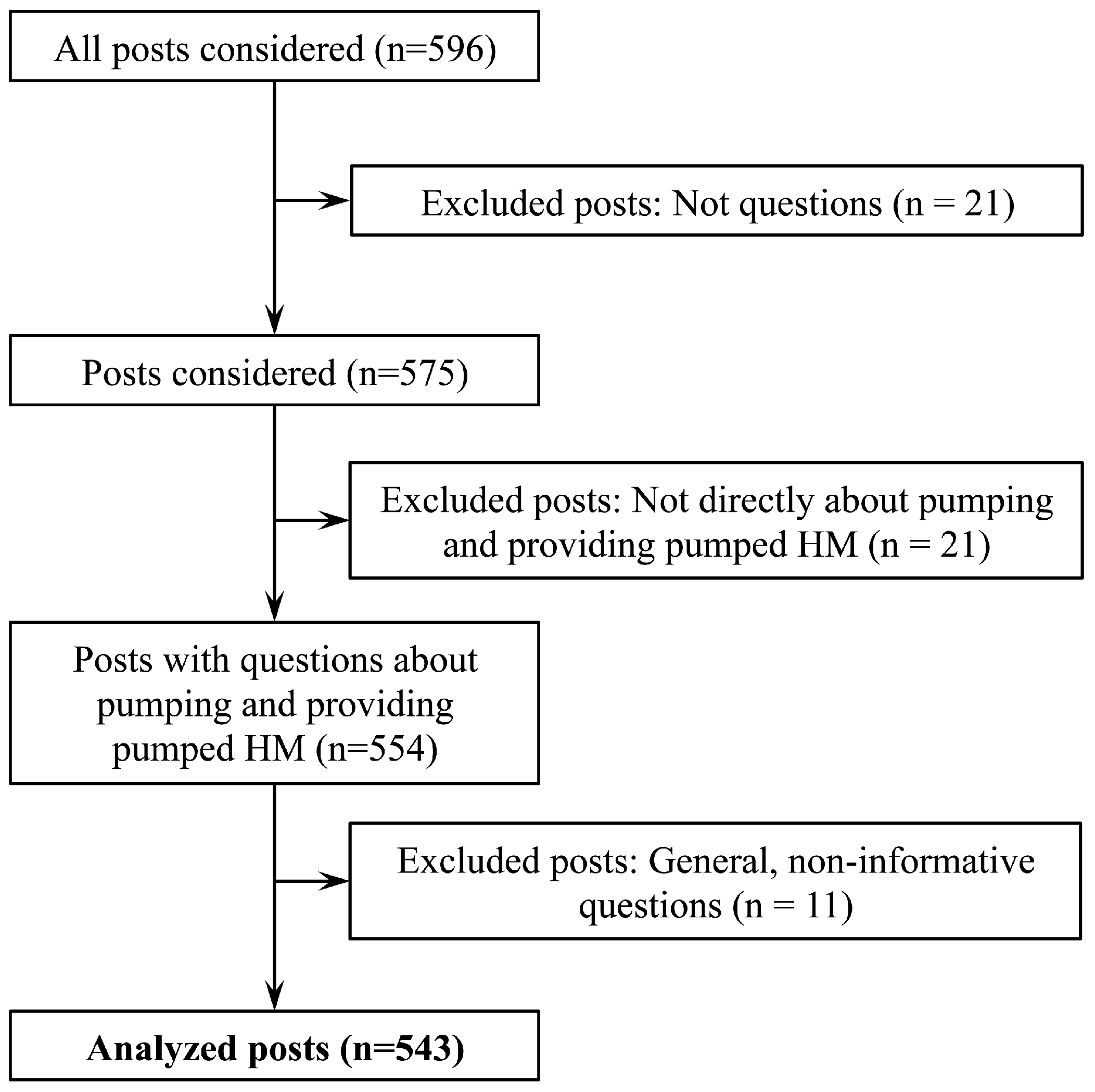
2.3. Study Sample
2.4. Data Collection and Cleaning
2.5. Data Analysis
3. Results
3.1. Choosing and Purchasing Pumps
3.1.1. Longitudinal Results
3.1.2. Cross-Sectional Results
I really want to get a breast pump but there just so expensive i’ve looked online and my [husband] is just like no thats to much but ive really want to get one until i seen the prices! Any one know of a good cheaper place to get them? Cus 200+ is just to much!—prenatal
[Insurance provider] told me insurance would cover a breast pump. Well fast forward & I’m just a couple of days away from delivery & need to get mine ASAP. Has anyone with the same plan been able to pick up the pump from a med supply store? Are they shipped only? And did you need to get a prescription first?—prenatal
3.2. Storing and Preparing Pumped HM
3.2.1. Longitudinal Results
3.2.2. Cross-Sectional Results
I usually store the milk in the fridge for a couple of days and then freeze it if its not consumed…I noticed/tasted milk freshly expressed – it has a sweet taste. Milk stored in fridge, then in the freezer, when unfrozen, it seems slight acidic. Is this normal? [sic]—postpartum (1.5–4.5 months)
3.3. Strategies for and Difficulties with Pumping and Integrating Pumping into Work
3.3.1. Longitudinal Results
3.3.2. Cross-Sectional Results
It seems like everyday my breasts get fuller, and never empty…I’ve tried heating pads, but only helped for a few pumps. Today my breasts are so sore, my nipples are cracked even though I use lanolin before and after pumping. Any suggestions?—postpartum (0–1.5 months)
3.4. Stopping Pumping
3.4.1. Longitudinal Results
3.4.2. Cross-Sectional Results
When will you stop pumping? …I guess I’m not sure what my end goal should be. A certain age? A certain amount frozen? What is your situation, how long will you pump for? Maybe hearing others situations will help me decide what I want to do.—postpartum (0–1.5 months)
I have been exclusively pumping since day 1 and [my baby] is now 16 weeks old. For various reasons I am ready to give up on pumping and put him on formula. However, how do I deal with the guilt of now doing something that feels right for me instead of what’s obviously best for him?! Pumping is tiresome, I find it very hard to do other things like make healthy lunches for myself for example, and I’m going nuts with constantly washing and storing the paraphernalia.—postpartum (4 months, as reported by mother)
I am mentally and physically exhausted from the strenuous schedule of pumping and taking care of a newborn. I return to work in one week and don’t want to stress about pumping there. Not to mention physically I am fed up [with] having boobs that weigh a million pounds, sweat, and hurt when I don’t pump every 2 to 3 h, specifically if I try to sleep longer. [My husband] wants me to continue to pump [because] he feels like the benefits outweigh all the physical, mental and emotional stresses I’m going thru. What would You do?—postpartum (1.5 months, as reported by mother)
4. Discussion
4.1. Guidelines for Safe Handling of Pumped HM
4.2. Guidelines for Obtaining Pumps and Earlier Access to Pumps
4.3. Additional Support from Family Members
4.4. Additional Support from Employers and Coworkers
4.5. Limitations
4.6. Strengths
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Labiner-Wolfe, J.; Fein, S.B.; Shealy, K.R.; and Wang, C. Prevalence of breast milk expression and associated factors. Pediatrics 2008, 122, S63–S68. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- Taveras, E.M.; Scanlon, K.S.; Birch, L.; Rifas-Shiman, S.L.; Rich-Edwards, J.W.; Gillman, M.W. Association of breastfeeding with maternal control of infant feeding at age 1 year. Pediatrics 2004, 114, e577–e583. [Google Scholar] [CrossRef] [PubMed]
- Wright, P.; Fawcett, J.; Crow, R. The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behav. Process. 1980, 5, 1–20. [Google Scholar] [CrossRef]
- Li, R.; Fein, S.B.; Grummer-Strawn, L.M. Do infants fed from bottles lack self-regulation of milk intake compared with directly breastfed infants? Pediatrics 2010, 125, e1386–e1393. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Fein, S.B.; Chen, J.; Grummer-Strawn, L.M. Why mothers stop breastfeeding: Mothers’ self-reported reasons for stopping during the first year. Pediatrics 2008, 122, S69–S76. [Google Scholar] [CrossRef] [PubMed]
- Keim, S.A.; Hogan, J.S.; McNamara, K.A.; Gudimetla, V.; Dillon, C.E.; Kwiek, J.J.; Geraghty, S.R. Microbial contamination of human milk purchased via the internet. Pediatrics 2013, 132, e1227–e1235. [Google Scholar] [CrossRef] [PubMed]
- Boo, N.Y.; Nordiah, A.J.; Alfizah, H.; Nor-Rohaini, A.H.; Lim, V.K. Contamination of breast milk obtained by manual expression and breast pumps in mothers of very low birthweight infants. J. Hosp. Infect. 2001, 49, 274–281. [Google Scholar] [CrossRef] [PubMed]
- García-Lara, N.R.; Escuder-Vieco, D.; García-Algar, O.; De la Cruz, J.; Lora, D.; Pallás-Alonso, C. Effect of freezing time on macronutrients and energy content of breastmilk. Breastfeed. Med. 2011, 7, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Soto-Ramírez, N.; Karmaus, W.; Zhang, H.; Davis, S.; Agarwal, S.; Albergottie, A. Modes of infant feeding and the occurrence of coughing/wheezing in the first year of life. J. Hum. Lact. 2013, 29, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, K.M.; Geraghty, S.R. The Quiet Revolution: Breastfeeding transformed with the use of breast pumps. Am. J. Public Health 2011, 101, 1356–1359. [Google Scholar] [CrossRef] [PubMed]
- Boone, K.M.; Geraghty, S.R.; Keim, S.A. Feeding at the breast and expressed milk feeding: Associations with otitis media and diarrhea in infants. J. Pediatr. 2016, 174, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Felice, J.P. A Mixed-Methods Investigation of Pumping Human Milk and Feeding Pumped Milk to Infants. Ph.D. Thesis, Cornell University, Ithaca, NY, USA, 2015. [Google Scholar]
- Ogbuanu, C.; Glover, S.; Probst, J.; Liu, J.; Hussey, J. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics 2011, 127, e1414–e1427. [Google Scholar] [CrossRef] [PubMed]
- Rojjanasrirat, W.; Sousa, V.D. Perceptions of breastfeeding and planned return to work or school among low-income pregnant women in the USA. J. Clin. Nurs. 2010, 13–14, 2014–2022. [Google Scholar] [CrossRef] [PubMed]
- Kimbro, R.T. On-the-job moms: Work and breastfeeding initiation and duration for a sample of low-income women. Matern. Child Health J. 2006, 10, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.S.; Zhou, W.; Arensberg, M.B. The effect of employment status on breastfeeding in the United States. Womens Health Issues 2006, 16, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Angeletti, M.A. Breastfeeding mothers returning to work: Possibilities for information, anticipatory guidance and support from US health care professionals. J. Hum. Lact. 2009, 25, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Fein, S.B.; Mandal, B.; Roe, B.E. Success of strategies for combining employment and breastfeeding. Pediatrics 2008, 122, S56–S62. [Google Scholar] [CrossRef] [PubMed]
- Negin, J.; Coffman, J.; Vizintin, P.; Raynes-Greenow, C. The influence of grandmothers on breastfeeding rates: A systematic review. BMC Pregnancy Childbirth. 2016, 16, 91. [Google Scholar] [CrossRef] [PubMed]
- Valente, T. Social Networks and Health: Models, Methods, and Applications, 1st ed.; Oxford University Press: New York, NY, USA, 2010. [Google Scholar]
- April 2014 Birth Club. Available online: http://community.babycenter.com/groups/a6737770/ april_2014_birth_club (accessed on 1 January 2014).
- Fein, S.B.; Labiner-Wolfe, J.; Shealy, K.R.; Li, R.; Chen, J.; Grummer-Strawn, L.M. Infant Feeding Practices Study II: Study methods. Pediatrics 2008, 122, S28–S35. [Google Scholar] [CrossRef] [PubMed]
- Jukic, A.M.; Baird, D.D.; Weinberg, C.R.; McConnaughey, D.R.; Wilcox, A.J. Length of human pregnancy and contributors to its natural variation. Hum. Reprod. 2013, 28, 2848–2855. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, S.R. Photo album of expressed breastmilk. Breastfeed. Med. 2011, 6, 433–434. [Google Scholar] [CrossRef] [PubMed]
- Parker, L.A.; Sullivan, S.; Krueger, C.; Mueller, M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed. Med. 2015, 10, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Parker, L.A.; Sullivan, S.; Krueger, C.; Kelechi, T.; Mueller, M. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: A pilot study. J. Perinatol. 2012, 32, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.G.; Johnson, L.W.; Rosenthal, M.S. Sources of education about breastfeeding and breast pump use: What effect do they have on breastfeeding duration? An analysis of the Infant Feeding Practices Survey II. Matern. Child Health J. 2012, 16, 1421–1430. [Google Scholar] [CrossRef] [PubMed]
- The Patient Protection and Affordable Care Act, H.R. 3590, 111th Congress, 2nd Sess. Available online: http://www.dol.gov/whd/regs/compliance/whdfs73.htm (accessed on 1 March 2015).
| Main Theme | Infant Age (Months) | |||
|---|---|---|---|---|
| Prenatal | 0–1.5 Months | 1.5–4.5 Months | Total | |
| Choosing and purchasing pumps | 37 | 10 | 12 | 59 |
| Storing and preparing pumped HM * | 14 | 48 | 106 | 168 |
| Strategies for and difficulties with pumping | 12 | 118 | 103 | 233 |
| Integrating pumping into work | 5 | 10 | 37 | 52 |
| Stopping pumping | 0 | 4 | 27 | 31 |
| Total | 68 | 190 | 285 | 543 |
| Main Theme | Examples of Topics Raised by Women |
|---|---|
| Choosing and purchasing pumps | Options available through insurance policy; length and logistics of insurance process; pump affordability vs. quality; when, where, and how to get a pump out-of-pocket |
| Storing and preparing pumped HM | Bag and bottle quality and desired traits (e.g., maintenance required to keep supplies clean and cost); length of storage time at room temperature, in refrigerator, and in freezer; thawing and warming; mixing from different pumping sessions; effects of alcohol, caffeine, and medications on pumped HM; smell, taste, and appearance of fresh, refrigerated, or frozen pumped HM |
| Strategies for and difficulties with pumping and integrating pumping into work | Pump features and malfunctions; managing physical discomfort; other experienced and anticipated barriers to pumping (e.g., heavy workload and a lack of designated place to pump) |
| Stopping pumping | Appropriate time to stop pumping and/or providing pumped HM; acceptable reasons to stop pumping; guilt; painful engorgement; drying up HM supply |
| Main Theme | Common Questions Asked by Women |
|---|---|
| Choosing and purchasing pumps |
|
| Storing and preparing pumped HM |
|
| Strategies for and difficulties with pumping and integrating pumping into work |
|
| Stopping pumping |
|
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, R.; Rasmussen, K.M.; Felice, J.P. Mothers’ Use of Social Media to Inform Their Practices for Pumping and Providing Pumped Human Milk to Their Infants. Children 2016, 3, 22. https://doi.org/10.3390/children3040022
Yamada R, Rasmussen KM, Felice JP. Mothers’ Use of Social Media to Inform Their Practices for Pumping and Providing Pumped Human Milk to Their Infants. Children. 2016; 3(4):22. https://doi.org/10.3390/children3040022
Chicago/Turabian StyleYamada, Rei, Kathleen M. Rasmussen, and Julia P. Felice. 2016. "Mothers’ Use of Social Media to Inform Their Practices for Pumping and Providing Pumped Human Milk to Their Infants" Children 3, no. 4: 22. https://doi.org/10.3390/children3040022
APA StyleYamada, R., Rasmussen, K. M., & Felice, J. P. (2016). Mothers’ Use of Social Media to Inform Their Practices for Pumping and Providing Pumped Human Milk to Their Infants. Children, 3(4), 22. https://doi.org/10.3390/children3040022






