Postural Fitness Protocol in Children and Adolescents: Descriptive Values from the ISQUIOS Program
Abstract
Highlights
- There are clear sex-related differences in spinal morphology, hip flexibility, and trunk muscle function.
- These results emphasize the need to consider sex as a determining factor when assessing posture and designing physical screening protocols for young people.
- The “Postural Fitness” protocol not only may serve as a valuable and feasible tool for early screening of postural deviations and physical deficits but also offers a foundation for individualized preventive strategies.
- Educators and practitioners should incorporate spine health education, functional mobility work, and muscular endurance challenges into youth physical activity programs, with special attention to pubertal changes and postural evolution.
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
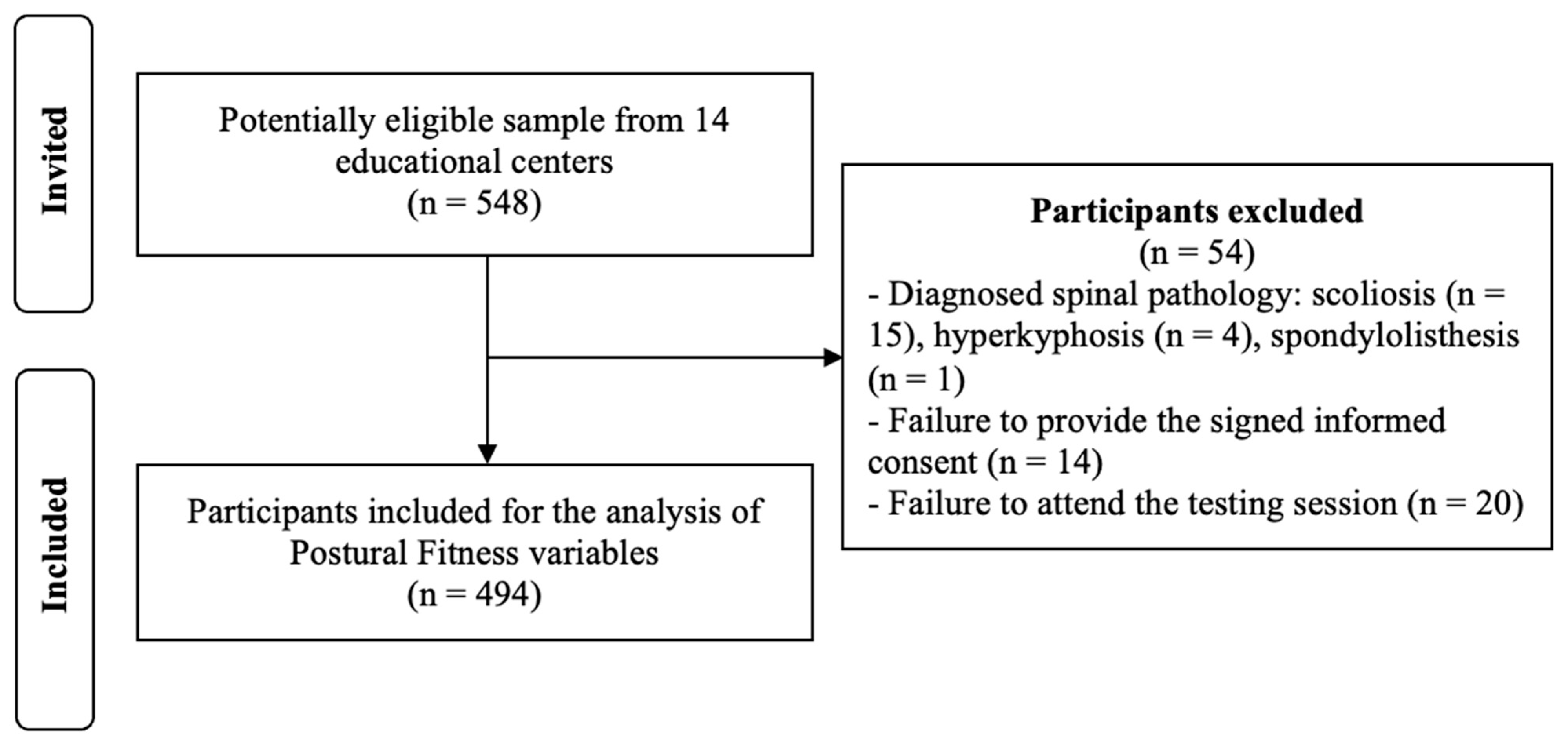
2.2. Participants
2.3. Procedure
2.3.1. Anthropometric Measures
2.3.2. Postural Fitness Protocol
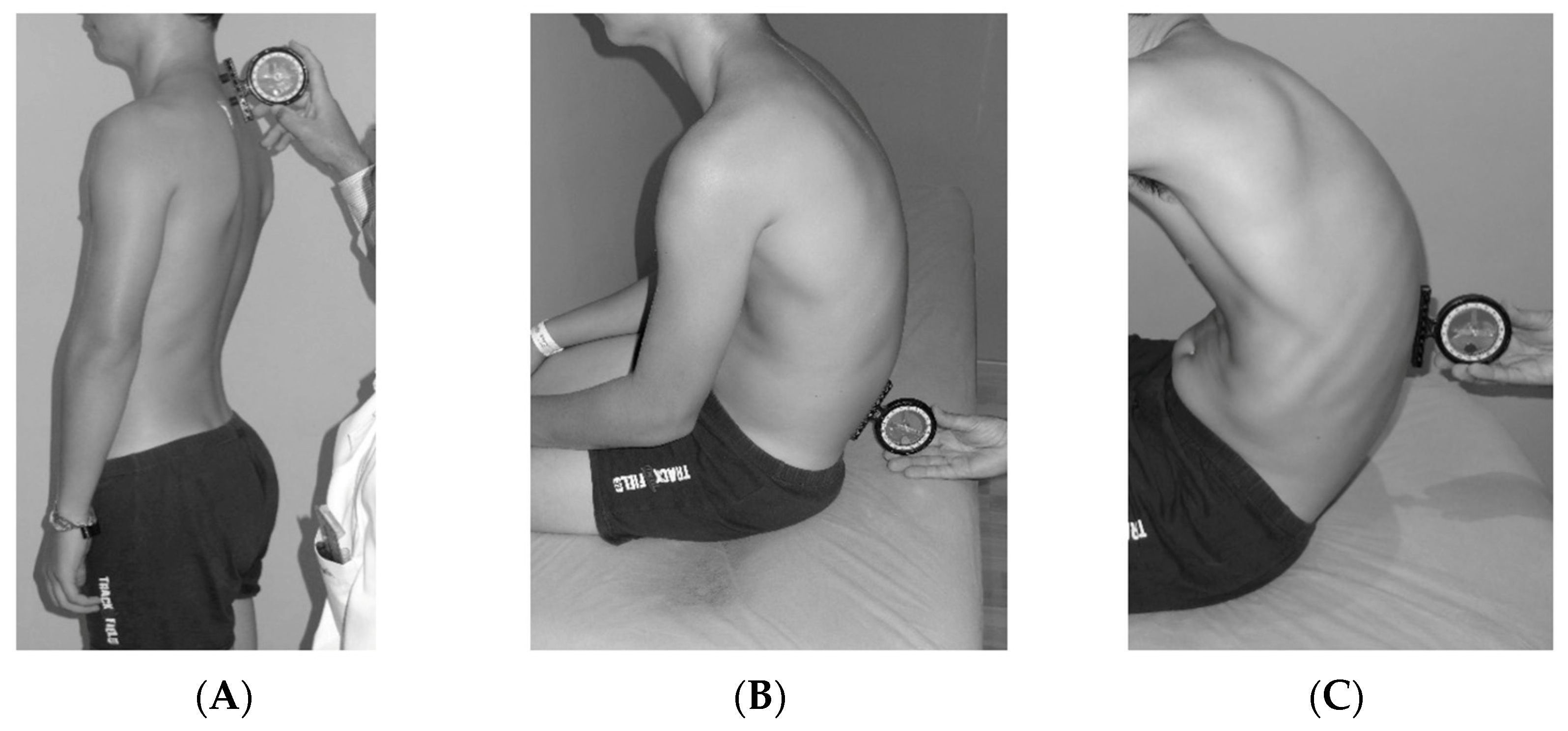
- Sagittal Integral Morphotype (SIM)
- 2.
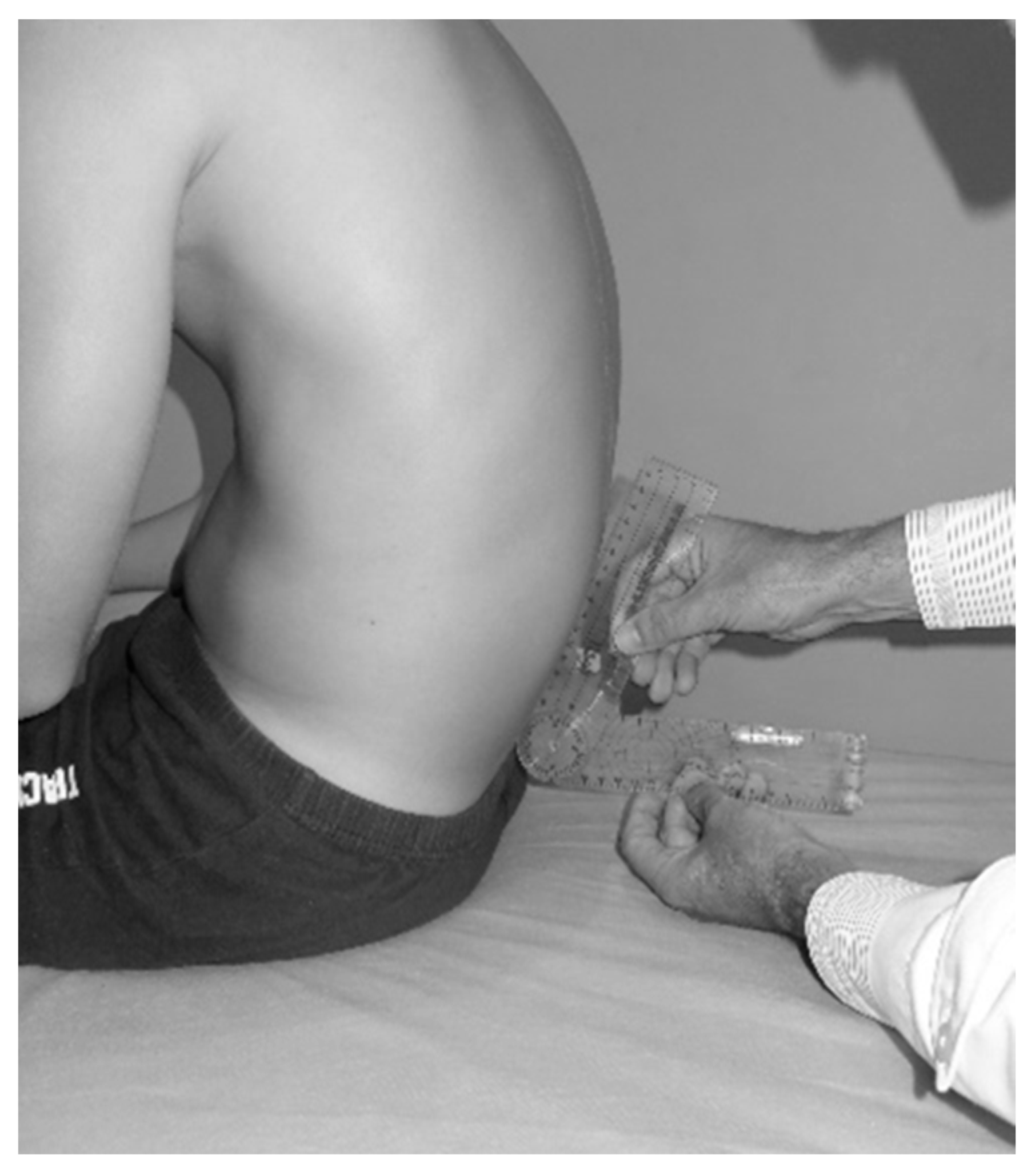
- Pelvic tilt and Toe Touch test
- 3.
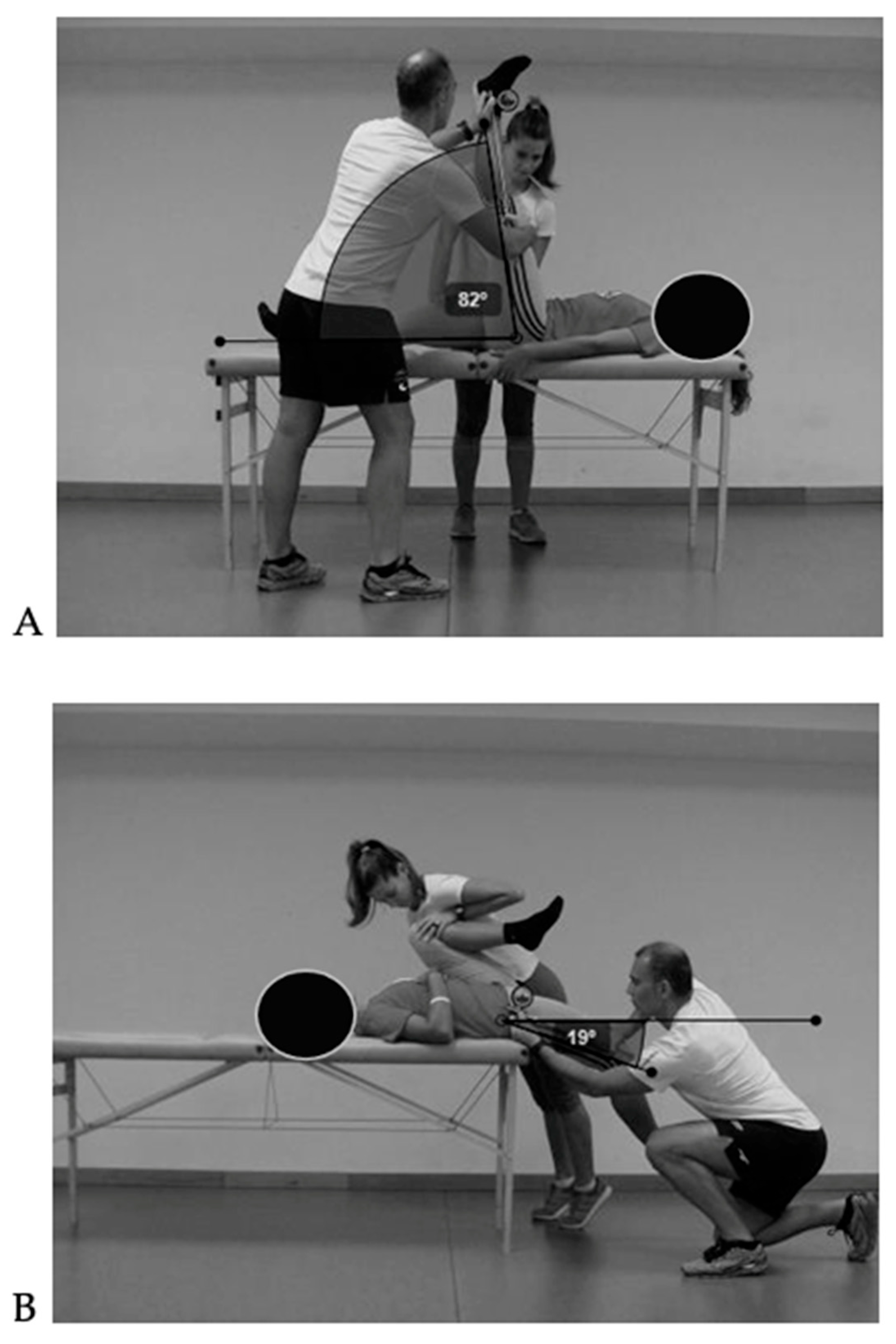
- Range of motion
- 4.
- Trunk muscle endurance
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BP | Back pain |
| BMI | Body mass index |
| ROM | Range of motion |
| PE | Physical education |
| SIM | Sagittal Integral Morphotype |
| SP | Standing position |
| SSP | Slump sitting position |
| FTFP | Forward trunk flexion position |
| TT | Toe Touch test |
| L-H | Lumbo-horizontal angle |
| L-V | Lumbo-vertical angle |
| PHFKE | Passive hip flexion with knee extended |
| PHE | Passive hip extension |
| BS | Biering–Sørensen test |
| SB | Side Bridge test |
References
- Junge, T.; Wedderkopp, N.; Boyle, E.; Kjaer, P. The Natural Course of Low Back Pain from Childhood to Young Adulthood—A Systematic Review. Chiropr. Man. Ther. 2019, 27, 10. [Google Scholar] [CrossRef]
- Ito, T.; Sugiura, H.; Ito, Y.; Narahara, S.; Natsume, K.; Takahashi, D.; Noritake, K.; Yamazaki, K.; Sakai, Y.; Ochi, N. Relationship between Low-Back Pain and Flexibility in Children: A Cross-Sectional Study. PLoS ONE 2023, 18, e0293408. [Google Scholar] [CrossRef] [PubMed]
- da Rosa, B.N.; Noll, M.; Candotti, C.T.; Loss, J.F. Risk Factors for Back Pain among Southern Brazilian School Children: A 6-Year Prospective Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 8322. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Muñoz, I.; Gómez-Conesa, A.; Sánchez-Meca, J. Prevalence of Low Back Pain in Children and Adolescents: A Meta-Analysis. BMC Pediatr. 2013, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Dunn, K.M.; Hestbaek, L.; Cassidy, J.D. Low Back Pain across the Life Course. Best Pract. Res. Clin. Rheumatol. 2013, 27, 591–600. [Google Scholar] [CrossRef]
- Wirth, B.; Potthoff, T.; Rosser, S.; Humphreys, B.K.; De Bruin, E.D. Physical Risk Factors for Adolescent Neck and Mid Back Pain: A Systematic Review. Chiropr. Man. Ther. 2018, 26, 36. [Google Scholar] [CrossRef]
- Potthoff, T.; De Bruin, E.D.; Rosser, S.; Humphreys, B.K.; Wirth, B. A Systematic Review on Quantifiable Physical Risk Factors for Non-Specific Adolescent Low Back Pain. J. Pediatr. Rehabil. Med. 2018, 11, 79–94. [Google Scholar] [CrossRef]
- Calvo-Muñoz, I.; Kovacs, F.M.; Roqué, M.; Gago, I.; Seco, J. Risk Factors for Low Back Pain in Childhood and Adolescence: A Systematic Review. Clin. J. Pain. 2018, 34, 468–484. [Google Scholar] [CrossRef]
- Beynon, A.M.; Hebert, J.J.; Lebouef-Yde, C.; Walker, B.F. Potential Risk Factors and Triggers for Back Pain in Children and Young Adults. A Scoping Review, Part II: Unclear or Mixed Types of Back Pain. Chiropr. Man. Ther. 2019, 27, 61. [Google Scholar] [CrossRef]
- Alhowimel, A.S.; Alfaifi, R.M.; Alluhaybi, A.A.; Alanazi, M.A.; Alanazi, K.M.; Almathami, N.S.; Almedhwah, S.H.; Almuayli, A.A.; Alenazi, A.M.; Alshehri, M.M.; et al. Prevalence of Low Back Pain and Associated Risk Factors among Saudi Arabian Adolescents: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 11217. [Google Scholar] [CrossRef]
- Kato, K.; Otoshi, K.I.; Tominaga, R.; Kaga, T.; Igari, T.; Sato, R.; Konno, S.I. Influences of Limited Flexibility of the Lower Extremities and Occurrence of Low Back Pain in Adolescent Baseball Players: A Prospective Cohort Study. J. Orthop. Sci. 2022, 27, 355–359. [Google Scholar] [CrossRef]
- Endo, S.; Kato, K.; Otoshi, K.; Kaneko, Y.; Tominaga, R.; Kaga, T.; Igari, T.; Sato, R.; Kobayashi, K.; Konno, S.I.; et al. Association between Low Back Pain and Limited Lower-Extremity Flexibility in Elementary School-Aged Softball Players: A Cross-Sectional Study. BMC Sports Sci. Med. Rehabil. 2025, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- González-Gálvez, N.; Carrasco-Poyatos, M.; Vaquero-Cristóbal, R.; Marcos-Pardo, P.J. Gender Mediation in Adolescents’ Back Pain and Physical Fitness: A Cross-Sectional Study. Healthcare 2022, 10, 696. [Google Scholar] [CrossRef] [PubMed]
- Miñana-Signes, V.; Monfort-Pañego, M. The Conditioning of the Trunk Muscles and Back Health in Physical Education. J. Hum. Sport Exerc. 2021, 16, 640–651. [Google Scholar] [CrossRef]
- Dolphens, M.; Vansteelandt, S.; Cagnie, B.; Vleeming, A.; Nijs, J.; Vanderstraeten, G.; Danneels, L. Multivariable Modeling of Factors Associated with Spinal Pain in Young Adolescence. Eur. Spine J. 2016, 25, 2809–2821. [Google Scholar] [CrossRef]
- De Vitta, A.; Noll, M.; Monfort-Pañego, M.; Miñana-Signes, V.; Maciel, N.M. Thoracic Spine Pain in High School Adolescents: A One-Year Longitudinal Study. Healthcare 2023, 11, 196. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Castro-Piñero, J.; España-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.A.M.; Enez-Pavón, D.J.; Chillón, P.; Girela-Rejón, M.J.; Mora, J.; et al. Field-Based Fitness Assessment in Young People: The ALPHA Health-Related Fitness Test Battery for Children and Adolescents. Br. J. Sports Med. 2011, 45, 518–524. [Google Scholar] [CrossRef]
- Plowman, S.A.; Meredith, M.D. Fitnessgram®/Activitygram®. Reference Guide, 4th ed.; The Cooper Institute: Dallas, TX, USA, 2013. [Google Scholar]
- Grabowski, H.; Szopa, J. Eurofit. European Tests of Physical Fitness; Akademia Wychowania Fizycznego: Krakow, Poland, 1991. [Google Scholar]
- Santonja-Medina, F.; Collazo-Diéguez, M.; Martínez-Romero, M.T.; Rodríguez-Ferrán, O.; Aparicio-Sarmiento, A.; Cejudo, A.; Andújar, P.; de Baranda, P.S. Classification System of the Sagittal Integral Morphotype in Children from the Isquios Programme (Spain). Int. J. Environ. Res. Public Health 2020, 17, 2467. [Google Scholar] [CrossRef]
- Cejudo, A. Description of ROM-SPORT I Battery: Keys to Assess Lower Limb Flexibility. Int. J. Environ. Res. Public Health 2022, 19, 747. [Google Scholar] [CrossRef]
- Ito, T.; Shirado, O.; Suzuki, H.; Takahashi, M.; Kaneda, K.; Strax, T.E. Lumbar Trunk Muscle Endurance Testing: An Inexpensive Alternative to a Machine for Evaluation. Arch. Phys. Med. Rehabil. 1996, 77, 75–79. [Google Scholar] [CrossRef]
- McGill, S.M.; Childs, A.; Liebenson, C. Endurance Times for Low Back Stabilization Exercises: Clinical Targets for Testing and Training from a Normal Database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef]
- Biering-Sorensen, F. Physical Measurements as Risk Indicators for Low-Back Trouble over a One-Year Period. Spine 1984, 9, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Romero, M.T.; Ayala, F.; Aparicio-Sarmiento, A.; De Ste Croix, M.; Sainz De Baranda, P. Reliability of Five Trunk Flexion and Extension Endurance Field-Based Tests in High School-Aged Adolescents: ISQUIOS Programme. J. Sports Sci. 2021, 39, 1860–1872. [Google Scholar] [CrossRef] [PubMed]
- Ginés-Díaz, A.; Martínez-Romero, M.T.; Cejudo, A.; Aparicio-Sarmiento, A.; Sainz de Baranda, P. Sagittal Spinal Morphotype Assessment in Dressage and Show Jumping Riders. J. Sport Rehabil. 2019, 29, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Mengibar, J.M.; Sainz de Baranda, P.; Santonja, F. Training Intensity and Sagittal Curvature of the Spine in Male and Female Artistic Gymnasts. J. Sports Med. Phys. Fit. 2018, 58, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Saur, P.M.; Ensink, F.B.; Frese, K.; Seeger, D.; Hildebrandt, J. Lumbar Range of Motion: Reliability and Validity of the Inclinometer Technique in the Clinical Measurement of Trunk Flexibility. Spine 1996, 21, 1332–1338. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz De Baranda, P.; Cejudo, A.; Santonja, F. Pruebas Angulares de Estimación de La Flexibilidad Isquiosural: Descripción de Los Procedimientos Exploratorios y Valores de Referencia. Rev. Andal. Med. Deport. 2013, 6, 120–128. [Google Scholar] [CrossRef][Green Version]
- Sainz De Baranda, P.; Rodríguez-Iniesta, M.; Ayala, F.; Santonja, F.; Cejudo, A. Determination of the Criterion-Related Validity of Hip Joint Angle Test for Estimating Hamstring Flexibility Using a Contemporary Statistical Approach. Clin. J. Sport Med. 2014, 24, 320–325. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Hernández-Martínez, I. Desalineaciones de La Pelvis y Patología Sacroilíaca. In Manual de Exploración Músculo-Esquelética; PANAMERICANA: Madrid, Spain, 2022; pp. 35–48. ISBN 9788491108153. [Google Scholar]
- Ayala, F.; de Baranda, R.S.; De Ste Croix, M.; Santonja, F. Reproducibility and Criterion-Related Validity of the Sit and Reach Test and Toe Touch Test for Estimating Hamstring Flexibility in Recreationally Active Young Adults. Phys. Ther. Sport 2012, 13, 219–226. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Ferrer-López, V.; Santonja-Renedo, S.; Cejudo, A.; Sainz de Baranda, P. Cortedad Isquiosural y Síndrome de Isquiosurales Cortos. In Manual de Exploración Músculo-Esquelética; PANAMERICANA: Madrid, Spain, 2021; pp. 201–210. ISBN 9788491108153. [Google Scholar]
- Cejudo, A.; Sainz de Baranda, P.; Ayala, F.; De Ste Croix, M.; Santonja-Medina, F. Assessment of the Range of Movement of the Lower Limb in Sport: Advantages of the ROM-SPORT I Battery. Int. J. Environ. Res. Public Health 2020, 17, 7606. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Moreno, A.; Cejudo, A.; Santonja, F. Assessment of Hamstring Muscle Extensibility in Children: ISQUIOS Programme. J. Sport Health Res. 2023, 15, 429–440. [Google Scholar] [CrossRef]
- Cejudo, A. Lower-Limb Range of Motion Predicts Sagittal Spinal Misalignments in Children: A Case-Control Study. Int. J. Environ. Res. Public Health 2022, 19, 5193. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Romero, M.T.; Robles-Palazón, F.J.; De Ste Croix, M.; Sainz de Baranda, P. Effects of Age, Maturation, and Sex on Trunk Muscle Performance in Elementary and Secondary School Students: ISQUIOS Program. Appl. Sci. 2025, 15, 2066. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Chi-Squared Test and Fisher’s Exact Test. Restor. Dent. Endod. 2017, 42, 152. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Coorevits, P.; Vleeming, A.; Danneels, L. Classification System of the Normal Variation in Sagittal Standing Plane Alignment: A Study among Young Adolescent Boys. Spine 2013, 38, 1003–1012. [Google Scholar] [CrossRef]
- Araújo, F.A.; Severo, M.; Alegrete, N.; Howe, L.D.; Lucas, R. Defining Patterns of Sagittal Standing Posture in School-Aged Girls and Boys. Phys. Ther. 2017, 97, 258–267. [Google Scholar] [CrossRef][Green Version]
- Schlosser, T.P.C.; Vincken, K.L.; Rogers, K.; Castelein, R.M.; Shah, S.A. Natural Sagittal Spino-Pelvic Alignment in Boys and Girls before, at and after the Adolescent Growth Spurt. Eur. Spine J. 2015, 24, 1158–1167. [Google Scholar] [CrossRef]
- Khalifé, M.; Skalli, W.; Assi, A.; Guigui, P.; Attali, V.; Valentin, R.; Gille, O.; Lafage, V.; Kim, H.J.; Ferrero, E.; et al. Sex-Dependent Evolution of Whole-Body Postural Alignment with Age. Eur. Spine J. 2024, 1–10. [Google Scholar] [CrossRef]
- González-Gálvez, N.; Vaquero-Cristóbal, R.; López-Vivancos, A.; Albaladejo-Saura, M.; Marcos-Pardo, P.J. Back Pain Related with Age, Anthropometric Variables, Sagittal Spinal Curvatures, Hamstring Extensibility, Physical Activity and Health Related Quality of Life in Male and Female High School Students. Int. J. Environ. Res. Public Health 2020, 17, 7293. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Andújar, P.; Collazo-Diéguez, M.; Pastor, A.; Santonja-Renedo, F.; Martínez-Romero, M.T.; Aparicio-Sarmiento, A.; Cejudo, A.; Rodríguez-Ferrán, O.; Santonja-Medina, F. Sagittal Standing Spinal Alignment and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia, Spain: ISQUIOS Programme. J. Back Musculoskelet. Rehabil. 2020, 33, 1003–1014. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Cejudo, A.; Moreno-Alcaraz, V.J.; Martinez-Romero, M.T.; Aparicio-Sarmiento, A.; Santonja-Medina, F. Sagittal Spinal Morphotype Assessment in 8 to 15 Years Old Inline Hockey Players. PeerJ 2020, 8, e8229. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-Structural Misalignments of Body Posture in the Sagittal Plane. Scolisis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef]
- Wirth, B.; Knecht, C.; Humphreys, K. Spine Day 2012: Spinal Pain in Swiss School Children- Epidemiology and Risk Factors. BMC Pediatr. 2013, 13, 159. [Google Scholar] [CrossRef] [PubMed]
- Alricsson, M.; Bjorklund, G.; Cronholm, M.; Olsson, O.; Viklund, P.; Svantesson, U.; Björklund, G.; Cronholm, M.; Olsson, O.; Viklund, P.; et al. Spinal Alignment, Mobility of the Hip and Thoracic Spine and Prevalence of Low Back Pain in Young Elite Cross-Country Skiers. J. Exerc. Rehabil. 2016, 12, 21–28. [Google Scholar] [CrossRef][Green Version]
- Aartun, E.; Hartvigsen, J.; Hestbaek, L. Validity of Commonly Used Clinical Tests to Diagnose and Screen for Spinal Pain in Adolescents: A School-Based Cohort Study in 1300 Danes Aged 11-15 Years. J. Manip. Physiol. Ther. 2016, 39, 76–87. [Google Scholar] [CrossRef]
- Martinez-Garcia, A.C. Efectos de Un Programa de Educación Postural Sobre El Morfotipo Sagital Del Raquis, La Extensibilidad de La Musculatura Isquiosural y Psoas Iliaco y La Resistencia Muscular Abdominal y Lumbar En Escolares de Educación Secundaria; Universidad de Murcia: Murcia, Spain, 2013. [Google Scholar]
- Shultz, S.J.; Nguyen, A.D.; Schmitz, R.J. Differences in Lower Extremity Anatomical and Postural Characteristics in Males and Females between Maturation Groups. J. Orthop. Sports Phys. Ther. 2008, 38, 137–149. [Google Scholar] [CrossRef]
- Wall, J.; Meehan, W.P.; Trompeter, K.; Gissane, C.; Mockler, D.; Van Dyk, N.; Wilson, F. Incidence, Prevalence and Risk Factors for Low Back Pain in Adolescent Athletes: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2022, 56, 1299–1306. [Google Scholar] [CrossRef]
- Costici, E.; De Salvatore, S.; Oggiano, L.; Sessa, S.; Curri, C.; Ruzzini, L.; Costici, P.F. The Impact of Physical Activity on Adolescent Low Back Pain: A Systematic Review. J. Clin. Med. 2024, 13, 5760. [Google Scholar] [CrossRef]
- Ambrosio, L.; Mazzuca, G.; Maguolo, A.; Russo, F.; Cannata, F.; Vadalà, G.; Maffeis, C.; Papalia, R.; Denaro, V. The Burden of Low Back Pain in Children and Adolescents with Overweight and Obesity: From Pathophysiology to Prevention and Treatment Strategies. Ther. Adv. Musculoskelet. Dis. 2023, 15, 1759720X231188831. [Google Scholar] [CrossRef]
- Dejanovic, A.; Cambridge, E.D.J.; McGill, S. Isometric Torso Muscle Endurance Profiles in Adolescents Aged 15–18: Normative Values for Age and Gender Differences. Ann. Hum. Biol. 2014, 41, 153–158. [Google Scholar] [CrossRef]
- Dejanovic, A.; Harvey, E.P.; McGill, S.M. Changes in Torso Muscle Endurance Profiles in Children Aged 7 to 14 Years: Reference Values. Arch. Phys. Med. Rehabil. 2012, 93, 2295–2301. [Google Scholar] [CrossRef]
- Moya-Ramón, M.; Juan-Recio, C.; Lopez-Plaza, D.; Vera-Garcia, F.J. Dynamic Trunk Muscle Endurance Profile in Adolescents Aged 14-18: Normative Values for Age and Gender Differences. J. Back. Musculoskelet. Rehabil. 2018, 31, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Arampatzis, A.; Frank, J.; Laube, G.; Mersmann, F. Trunk Muscle Strength and Lumbo-Pelvic Kinematics in Adolescent Athletes: Effects of Age and Sex. Scand. J. Med. Sci. Sports 2019, 29, 1691–1698. [Google Scholar] [CrossRef]
- Mueller, J.; Mueller, S.; Stoll, J.; Baur, H.; Mayer, F. Trunk Extensor and Flexor Strength Capacity in Healthy Young Elite Athletes Aged 11–15 Years. J. Strength Cond. Res. 2014, 28, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Ervin, R.; Fryar, C.; Wang, C.-Y.; Miller, I.; Ogden, C. Strength and Body Weight in US Children and Adolescents. Pediatrics 2014, 134, e782–e789. [Google Scholar] [CrossRef] [PubMed]
- Dejanovic, A.; Harvey, E.; Andersen, J.; Mcgill, S.M. Do Anthropometric Measures Influence Torso Muscle Endurance Profiles of Children Aged 7 to 14? Adv. Phys. Educ. 2012, 2, 187–196. [Google Scholar] [CrossRef]
- Zurawski, A.L.; Kiebzak, W.P.; Kowalski, I.M.; Sliwinski, G.; Sliwinski, Z. Evaluation of the Association between Postural Control and Sagittal Curvature of the Spine. PLoS ONE 2020, 15, e0241228. [Google Scholar] [CrossRef]
- Wirth, B.; Knecht, C.; Siegenthaler, M.H.; Schweinhardt, P. An Observational Cross-Sectional Study on the Characteristics of Children and Adolescents with Non-Specific Spinal Pain Stratified by Pain Severity. BMC Pediatr. 2024, 24, 757. [Google Scholar] [CrossRef]
- García-Moreno, J.M.; Calvo-Muñoz, I.; Gómez-Conesa, A.; López-López, J.A. Effectiveness of Physiotherapy Interventions for Back Care and the Prevention of Non-Specific Low Back Pain in Children and Adolescents: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2022, 23, 314. [Google Scholar] [CrossRef]
- Azevedo, N.; Ribeiro, J.C.; Machado, L. Back Pain in Children and Adolescents: A Cross-Sectional Study. Eur. Spine J. 2023, 32, 3280–3289. [Google Scholar] [CrossRef]
- Fernández, L.F.; Rodríguez-Gude, C.; de Oliveira, I.M. Effect of Therapeutic Exercise on the Management of Hyperkyphosis in Adolescence and Young Adulthood: A Systematic Review. Physiother. Res. Int. 2025, 30, e70078. [Google Scholar] [CrossRef]
- Wen, L.; Lin, X.; Li, C.; Zhao, Y.; Yu, Z.; Han, X. Sagittal Imbalance of the Spine Is Associated with Poor Sitting Posture among Primary and Secondary School Students in China: A Cross-Sectional Study. BMC Musculoskelet. Disord. 2022, 23, 98. [Google Scholar] [CrossRef]
- Calvo-Muñoz, I.; Kovacs, F.M.; Roqué, M.; Seco-Calvo, J. The Association between the Weight of Schoolbags and Low Back Pain among Schoolchildren: A Systematic Review, Meta-Analysis and Individual Patient Data Meta-Analysis. Eur. J. Pain 2020, 24, 91–109. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Ratamess, N.A.; Kang, J.; Bush, J.A.; Rial Rebullido, T. May the Force Be with Youth: Foundational Strength for Lifelong Development. Curr. Sports Med. Rep. 2023, 22, 414–422. [Google Scholar] [CrossRef]



| Spinal Curve | SP | SSP | FTFP | |||
|---|---|---|---|---|---|---|
| Values | Classification | Values | Classification | Values | Classification | |
| Thoracic | <20° | Hypokyphosis | <20° | Hypokyphosis | <40° | Hypokyphosis |
| 20° to 40° | Normal | 20° to 40° | Normal | 40° to 65° | Normal | |
| >40° | Hyperkyphosis | >40° | Hyperkyphosis | >65° | Hyperkyphosis | |
| Lumbar | <−20° | Hypolordosis | <−15° | Lordosis | <10° | Hypokyphosis |
| −20° to −40° | Normal | −15° to 15° | Normal | 10° to 30° | Normal | |
| >40° | Hyperlordosis | >15° | Hyperkyphosis | >30° | Hyperkyphosis | |
| Classification | Subclassification | SP | SSP | FTFP |
|---|---|---|---|---|
| Normal kyphosis | Normal (20° to 40°) | Normal (20° to 40°) | Normal (40° to 65°) | |
| Functional thoracic hyperkyphosis | Static | Normal (20° to 40°) | Hyperkyphosis (>40°) | Normal (40° to 65°) |
| Dynamic | Normal (20° to 40°) | Normal (20° to 40°) | Hyperkyphosis (>65°) | |
| Total | Normal (20° to 40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) | |
| Hyperkyphosis | Total | Hyperkyphosis (>40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) |
| Standing | Hyperkyphosis (>40°) | Normal (20° to 40°) | Normal (40° to 65°) | |
| Static | Hyperkyphosis (>40°) | Hyperkyphosis (>40°) | Normal (40° to 65°) | |
| Dynamic | Hyperkyphosis (>40°) | Normal (20° to 40°) | Hyperkyphosis (>65°) | |
| Hypokyphosis/Hypokyphotic attitude | Flat-back | Hypokyphosis (<20°) | Hypokyphosis (<20°) | Hypokyphosis (<40°) |
| Standing | Hypokyphosis (<20°) | Normal (20° to 40°) | Normal (40° to 65°) | |
| Static | Hypokyphosis (<20°) | Hypokyphosis (<20°) | Normal (40° to 65°) | |
| Dynamic | Hypokyphosis (<20°) | Normal (20° to 40°) | Hypokyphosis (<40°) | |
| Hypomobile kyphosis | Normal (20° to 40°) | Normal (20° to 40°) | Hypokyphosis (<40°) |
| Classification | Subclassification | SP | SSP | FTFP |
|---|---|---|---|---|
| Normal lordosis | Normal (−20° to −40°) | Normal (−15° to 15°) | Normal (10° to 30°) | |
| Lumbar spine with reduced mobility | Functional lumbar lordosis/Hypomobile lordosis | Normal (−20° to −40°) | Normal (−15° to 15°) | Hypokyphosis or lordosis (<10°) |
| Lumbar hypomobility | Hypolordosis (<−20°) | Normal (−15° to 15°) | Hypokyphosis (<10°) | |
| Hyperlordotic attitude | Hyperlordosis (>−40°) | Normal (−15° to 15°) | Normal (10° to 30°) | |
| Functional lumbar hyperkyphosis | Static | Normal (−20° to −40°) | Hyperkyphosis (>15°) | Normal (10° to 30°) |
| Dynamic | Normal (−20° to −40°) | Normal (−15° to 15°) | Hyperkyphosis (>30°) | |
| Total | Normal (−20° to −40°) | Hyperkyphosis (>15°) | Hyperkyphosis (>30°) | |
| Lumbar hypermobility | Hypermobility 1 | Hyperlordosis (>−40°) | Hyperkyphosis (>15°) | Hyperkyphosis (>30°) |
| Hypermobility 2 | Hyperlordosis (>−40°) | Normal (−15° to 15°) | Hyperkyphosis (> 30°) | |
| Hypermobility 3 | Hyperlordosis (>−40°) | Hyperkyphosis (>15°) | Normal (10° to 30°) | |
| Hypolordosis | Hypolordotic attitude | Hypolordosis (<−20°) | Normal (−15° to 15°) | Normal (10° to 30°) |
| Lumbar kyphosis 1 | Hypolordosis (<−20°) | Hyperkyphosis (>15°) | Hyperkyphosis (>30°) | |
| Lumbar kyphosis 2 | Hypolordosis (<−20°) | Hyperkyphosis (> 15°) | Normal (10° to 30°) | |
| Lumbar kyphosis 3 | Hypolordosis (<−20°) | Normal (−15° to 15°) | Hyperkyphosis (>30°) | |
| Structured Hyperlordosis | Hyperlordosis (>−40°) | Hyperlordosis (<−15°) or normal (−15° to 15°) | Lordosis or Hypokyphosis (<10°) | |
| Structured lumbar kyphosis | Hypolordosis or kyphosis (<−20°) | Hyperkyphosis (>15°) | Hyperkyphosis (>30°) |
| Variables | Total Sample (n = 494) | Male (n = 247) | Female (n = 247) |
|---|---|---|---|
| Anthropometric Characteristics | |||
| Age (y) | 11.03 ± 1.5 (10.9–11.2) | 11 ± 1.5 (10.8–11.2) | 11 ± 1.5 (10.8–11.2) |
| Body mass (kg) | 44.3 ± 11.4 (43.2–45.3) | 44 ± 10.9 (42.6–45.4) | 44.5 ± 11.8 (43–46) |
| Body height (cm) | 146.5 ± 9.7 (145.6–147.3) | 146.9 ± 10.1 (145.7–148.2) | 145.9 ± 9.3 (144.8–147.1) |
| BMI (kg/m2) | 20.4 ± 3.8 (20.1–20.8) | 20.2 ± 3.6 (19.7–20.6) | 20.6 ± 4 (20.1–21.1) |
| Fitness Postural Protocol | |||
| SIM | |||
| SP thoracic (°) | 38.5 ± 9.5 (37.7–39.4) | 40.3 ± 9.6 (39.1–41.5) | 36.7 ± 9.2 (35.5–37.8) * |
| SP lumbar (°) | 33.6 ± 8.8 (32.8–34.5) | 31.5 ± 8.5 (30.4–32.5) | 35.7 ± 8.6 (34.6–36.8) * |
| SSP thoracic (°) | 35.5 ± 10.3 (34.6–36.4) | 37.2 ± 10.2 (35.9–38.5) | 33.8 ± 10.2 (32.5–35.1) * |
| SSP lumbar (°) | 11.1 ± 10.9 (10.1–12.1) | 13.4 ± 11.4 (12–14.9) | 8.7 ± 10 (7.5–10) * |
| FTFP thoracic (°) | 49.3 ± 11.9 (48.3–50.4) | 51.3 ± 11.1 (49.9–52.7) | 47.4 ± 12.3 (45.9–48.9) * |
| FTFP lumbar (°) | 26 ± 8.7 (25.2–26.8) | 27.7 ± 8.4 (26.6–28.7) | 24.3 ± 8.7 (23.2–25.4) * |
| Pelvic tilt and Toe Touch test | |||
| L-H angle in SSP (°) | 102.3 ± 8.6 (101.6–103.1) | 104.9 ± 8.4 (103.8–105.9) | 99.7 ± 8.1 (98.6–100.7) * |
| L-V angle in FTFP (°) | 114.5 ± 14.9 (113.1–115.9) | 120.6 ± 12 (119–122.2) | 108.3 ± 15 (106.2–110.3) * |
| TT test (cm) | −7.3 ± 8.6 (−8.1–(−6.6)) | −10.2 ± 7.5 (−11.1-(−9.3)) | −4.5 ± 8.7 (−5.6–(−3.4)) * |
| ROM | |||
| PHE-R (°) | 17.7 ± 8.6 (16.9–18.4) | 16.8 ± 8.1 (15.8–17.8) | 18.5 ± 9 (17.4–19.7) * |
| PHE-L (°) | 17.6 ± 8.2 (16.9–18.4) | 16.8 ± 7.6 (15.9–17.8) | 18.5 ± 8.7 (17.4–19.6) * |
| PHFKE-R (°) | 74.6 ± 29 (72–77.2) | 68.9 ± 8.6 (67.4–69.6) | 77.9 ± 13 (75.5–78.7) * |
| PHFKE-L (°) | 72.8 ± 11.8 (71.7–73.8) | 68.5 ± 8.9 (67.9–70.1) | 77.1 ± 12.7 (75.3–85.1) * |
| Trunk Muscle Endurance | |||
| Ito test (s) | 95.8 ± 72 (85.9–105.6) | 106.9 ± 82.1 (89.6–124.2) | 84.7 ± 61.9 (75.4–94) |
| BS test (s) | 114.7 ± 72.7 (107.9–121.4) | 106.2 ± 69.8 (97–115.4) | 123.2 ± 74.7 (113.3–133.1) * |
| SB-R test (s) | 45 ± 28.3 (42.5–47.6) | 48.7 ± 31 (44.7–52.6) | 41.4 ± 24.9 (38.2–44.5) * |
| SB-L test (s) | 45.9 ± 29.3 (43.3–48.6) | 50.9 ± 32.5 (46.8–55.1) | 40.9 ± 24.7 (37.8–44.1) * |
| Classification | Total Sample (n = 494) | Male (n = 247) | Female (n = 247) | Chi-Square | |
|---|---|---|---|---|---|
| Thoracic curvature | |||||
| SP | Hypokyphosis | 0.8% (4) | 0% (0) | 1.6% (4) | χ2(2) = 9.45, p = 0.01 |
| Normal | 58.2% (289) | 53.8% (133) | 63.1% (156) | ||
| Hyperkyphosis | 40.6% (201) | 46.1% (114) | 35.2% (87) | ||
| SSP | Hypokyphosis | 1.7% (4) | 0% (0) | 1.7% (4) | χ2(2) = 8.43, p = 0.01 |
| Normal | 71.2% (352) | 67.6% (167) | 74.9% (185) | ||
| Hyperkyphosis | 27.9% (138) | 32.4% (80) | 23.5% (58) | ||
| FTFP | Hypokyphosis | 0.4% (1) | 0% (0) | 0.4% (1) | χ2(2) = 7.577, p = 0.02 |
| Normal | 26.9% (133) | 21.8% (54) | 31.9% (79) | ||
| Hyperkyphosis | 72.9% (360) | 78.2% (193) | 67.6% (167) | ||
| SIM | Normal kyphosis | 16.2% (80) | 12.1% (30) | 20.2% (50) | χ2(9) = 21.774, p = 0.01 |
| Functional static hyperkyphosis | 2% (10) | 1.2% (3) | 2.8% (7) | ||
| Functional dynamic hyperkyphosis | 32% (158) | 30.8% (76) | 33.2% (82) | ||
| Total functional hyperkyphosis | 8.1% (40) | 9.7% (24) | 6.5% (16) | ||
| Hyperkyphosis standing | 6.3% (31) | 5.7% (14) | 6.9% (17) | ||
| Hyperkyphosis static | 1.6% (8) | 2.8% (7) | 0.4% (1) | ||
| Hyperkyphosis dynamic | 16.6% (82) | 19% (47) | 174.2% (35) | ||
| Total hyperkyphosis | 16.2% (80) | 18.6% (46) | 13.8% (34) | ||
| Hypokyphosis | 0.8% (4) | 0% (0) | 1.6% (4) | ||
| Hypomobile kyphosis | 0.2% (1) | 0% (0) | 0.4% (1) | ||
| Lumbar curvature | |||||
| SP | Hypolordosis | 4.8% (24) | 6.47% (16) | 3.2% (8) | χ2(2) = 11.989, p = 0.002 |
| Normal | 77.5% (383) | 81.4% (201) | 73.7% (182) | ||
| Hyperlordosis | 17.6% (87) | 12.1% (30) | 23.1% (57) | ||
| SSP | Lordosis | 0% (0) | 0% (0) | 0% (0) | χ2(1) = 17.386, p < 0.001 |
| Normal | 64.3% (317) | 55.3% (136) | 73.3% (181) | ||
| Hyperkyphosis | 35.7% (176) | 44.7% (110) | 26.7% (66) | ||
| FTFP | Hypokyphosis | 2.2% (11) | 1.6% (4) | 2.8% (7) | χ2(2) = 3.64, p = 0.16 |
| Normal | 72.1% (356) | 69.2% (171) | 74.9% (185) | ||
| Hyperkyphosis | 25.7% (127) | 29.1% (72) | 22.2% (55) | ||
| SIM | Normal lordosis | 38.9% (192) | 35.2% (87) | 42.5% (105) | χ2(10) = 25.536, p = 0.004 |
| Functional lumbar lordosis | 1.6% (8) | 1.2% (3) | 2% (5) | ||
| Hyperlordotic attitude | 14.4% (71) | 9.7% (24) | 19% (47) | ||
| Functional static hyperkyphosis | 15% (74) | 19.8% (49) | 10.1% (25) | ||
| Functional dynamic hyperkyphosis | 7.1% (35) | 6.9% (17) | 7.3% (18) | ||
| Total Functional hyperkyphosis | 15% (74) | 18.2% (45) | 11.7% (29) | ||
| Lumbar hypermobility | 2.6% (13) | 2% (5) | 3.2% (8) | ||
| Hypolordotic attitude | 1.2% (6) | 1.2% (3) | 1.2% (3) | ||
| Lumbar kyphosis | 2% (10) | 2.8% (7) | 1.2% (3) | ||
| Structured hyperlordosis | 0.6% (3) | 0.4% (1) | 0.8% (2) | ||
| Structured lumbar kyphosis | 1.6% (8) | 2.4% (6) | 0.8% (2) | ||
| Classification | Total Sample (n = 494) | Male (n = 247) | Female (n = 247) | Chi-Square | |
|---|---|---|---|---|---|
| Pelvic tilt | |||||
| L-H angle | Neutral | 43.9% (212) | 31.7% (78) | 56.5% (134) | χ2(1) = 30.226, p < 0.001 |
| Posterior PT | 56.1% (271) | 68.3% (168) | 43.4% (103) | ||
| L-V angle | Neutral | 20.1% (85) | 5.6% (12) | 35.1% (73) | χ2(1) = 57.69, p < 0.001 |
| Posterior PT | 79.9% (339) | 94.4% (204) | 64.9% (135) | ||
| ROM | |||||
| PHE-R | Normal | 70.6% (349) | 67.2% (166) | 74.1% (183) | χ2(1) = 2.82, p = 0.08 |
| Reduced | 29.4% (145) | 32.8% (81) | 25.9% (64) | ||
| PHE-L | Normal | 71.6% (354) | 69.2% (171) | 74.1% (183) | χ2(1) = 1.43, p = 0.23 |
| Reduced | 28.4% (140) | 30.8% (76) | 25.9% (64) | ||
| PHFKE-R | Normal | 37.9% (187) | 22.7% (56) | 53.1% (131) | χ2(1) = 48.403, p < 0.001 |
| Reduced | 62.1% (307) | 77.3% (191) | 46.9% (116) | ||
| PHFKE-L | Normal | 38.9% (192) | 25.1% (62) | 52.6% (130) | χ2(1) = 39.39, p = 0.001 |
| Reduced | 61.1% (302) | 74.9% (185) | 47.4% (117) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Romero, M.T.; De Ste Croix, M.; Sainz de Baranda, P. Postural Fitness Protocol in Children and Adolescents: Descriptive Values from the ISQUIOS Program. Children 2025, 12, 1253. https://doi.org/10.3390/children12091253
Martínez-Romero MT, De Ste Croix M, Sainz de Baranda P. Postural Fitness Protocol in Children and Adolescents: Descriptive Values from the ISQUIOS Program. Children. 2025; 12(9):1253. https://doi.org/10.3390/children12091253
Chicago/Turabian StyleMartínez-Romero, María Teresa, Mark De Ste Croix, and Pilar Sainz de Baranda. 2025. "Postural Fitness Protocol in Children and Adolescents: Descriptive Values from the ISQUIOS Program" Children 12, no. 9: 1253. https://doi.org/10.3390/children12091253
APA StyleMartínez-Romero, M. T., De Ste Croix, M., & Sainz de Baranda, P. (2025). Postural Fitness Protocol in Children and Adolescents: Descriptive Values from the ISQUIOS Program. Children, 12(9), 1253. https://doi.org/10.3390/children12091253






