Comorbid Insomnia and Sleep Apnea Across the Pediatric Age: A Polysomnographic Study
Abstract
Highlights
- Comorbid insomnia and sleep apnea (COMISA) is less common in children than in adults.
- Among patients with obstructive sleep apnea (OSA), those with comorbid insomnia demonstrated a lower OSA severity but higher anxiety levels.
- The mechanisms underlying COMISA may differ between children and adults, highlighting the need for age-specific approaches to diagnosis and treatment.
- Anxiety should systematically be assessed in children with OSA, as it may be a risk factor for COMISA.
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Ethical Considerations
2.3. Demographic Characteristics
2.4. Polysomnography
2.4.1. Sleep Architecture
2.4.2. Respiratory Parameters
2.5. Questionnaires
2.6. Definition of Obstructive Sleep Apnea and Insomnia
2.7. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.1.1. Demographic Characteristics
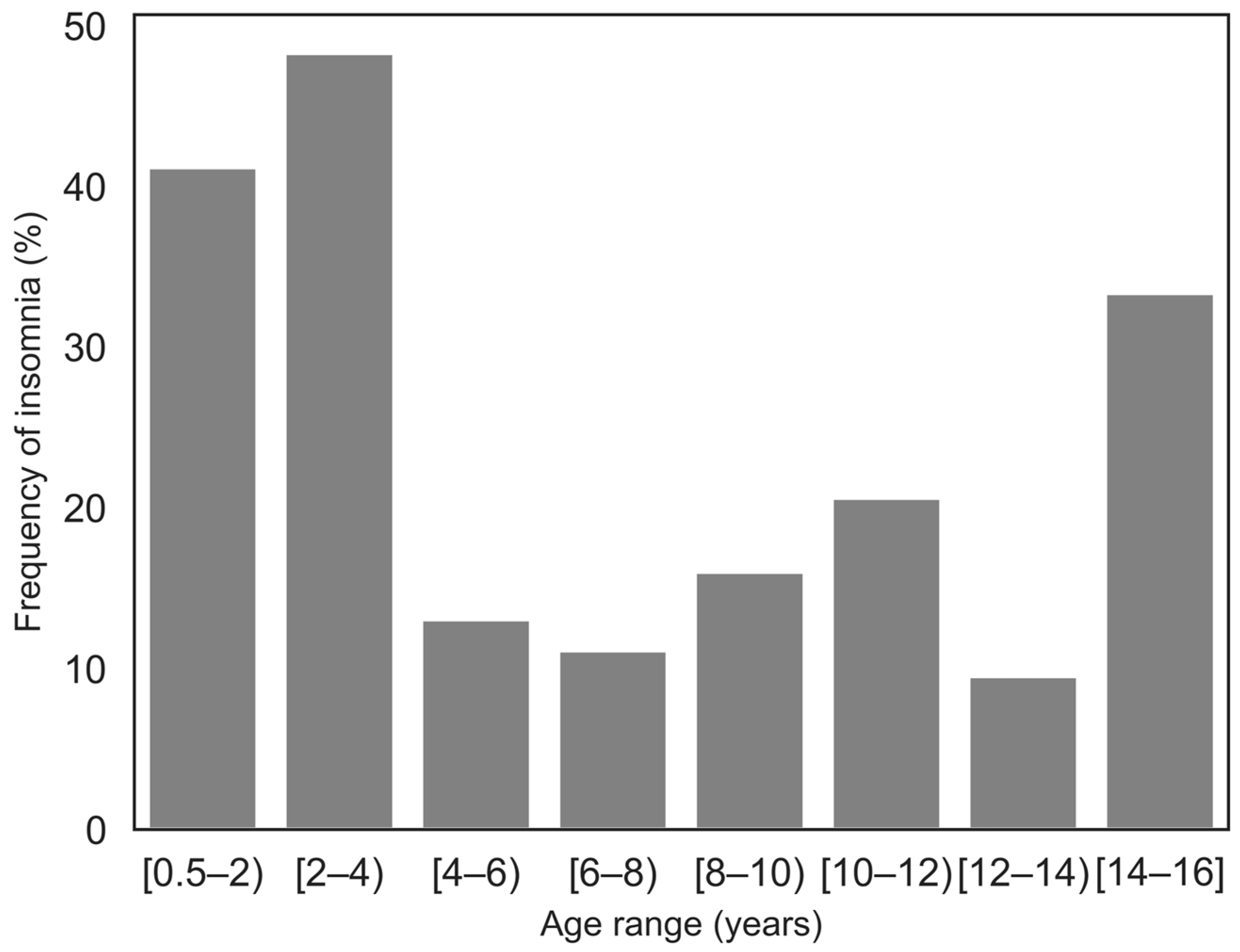
3.1.2. OSA and Insomnia
3.2. Characteristics Associated with COMISA
3.2.1. Demographic Characteristics
3.2.2. Polysomnographic Characteristics
Sleep Architecture
Respiratory Parameters
3.2.3. Questionnaires
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AASM | American Academy of Sleep Medicine |
| ADHD | Attention Deficit Hyperactivity Disorder |
| BMI | Body Mass Index |
| CAHI | Central Apnea-Hypopnea Index |
| CBCL | Child Behavior Checklist |
| CDI | Children’s Depression Inventory |
| COMISA | COMorbid Insomnia and Sleep Apnea |
| CPAP | Continuous Positive Airway Pressure |
| DIMS | Disorders of Initiating and Maintaining Sleep |
| EEG | Electroencephalogram |
| FDR | False Discovery Rate |
| FSSA | French Sleepiness Scale for Adolescents |
| GA | Gestational Age |
| OAHI | Obstructive Apnea-Hypopnea Index |
| ODI > 3 | Oxygen Desaturation Index >3% |
| OSA | Obstructive Sleep Apnea |
| PLMI | Periodic Leg Movement Index |
| PSG | Polysomnography |
| REM | Rapid Eye Movement |
| RERA | Respiratory Effort-Related Arousal |
| SDB | Sleep Disordered Breathing |
| SDSC | Sleep Disturbance Scale for Children |
| SE | Sleep Efficacy |
| SOL | Sleep Onset Latency |
| SpO2 | Oxygen Saturation |
| TST | Total Sleep Time |
| WASO | Wake After Sleep Onset |
References
- Marcus, C.L.; Brooks, L.J.B.; Davidson Ward, S.; Draper, K.A.; Gozal, D.; Halbower, A.C.; Jones, J.; Lehmann, C.; Schechter, M.S.; Sheldon, S.; et al. Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome. Pediatrics 2012, 130, e714–e755. [Google Scholar] [CrossRef]
- Nunes, M.L.; Bruni, O. Insomnia in childhood and adolescence: Clinical aspects, diagnosis, and therapeutic approach. J. Pediatr. 2015, 91, S26–S35. [Google Scholar] [CrossRef][Green Version]
- Owens, J.A.; Mindell, J.A. Pediatric Insomnia. Pediatr. Clin. N. Am. 2011, 58, 555–569. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.M.; Malow, B.A. Pediatric Insomnia. Chest 2016, 149, 1332–1339. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.K.; Kim, S.S. Behavioral insomnia in infants and young children. Clin. Exp. Pediatr. 2021, 64, 111–116. [Google Scholar] [CrossRef]
- Sweetman, A.; Lack, L.; McEvoy, R.D.; Smith, S.; Eckert, D.J.; Osman, A.; Carberry, J.C.; Wallace, D.; Nguyen, P.D.; Catcheside, P. Bi-directional relationships between co-morbid insomnia and sleep apnea (COMISA). Sleep Med. Rev. 2021, 60, 101519. [Google Scholar] [CrossRef] [PubMed]
- Luyster, F.S.; Buysse, D.J.; Strollo, P.J. Comorbid Insomnia and Obstructive Sleep Apnea: Challenges for Clinical Practice and Research. J. Clin. Sleep Med. 2010, 06, 196–204. [Google Scholar] [CrossRef]
- Ragnoli, B.; Pochetti, P.; Raie, A.; Malerba, M. Comorbid Insomnia and Obstructive Sleep Apnea (COMISA): Current Concepts of Patient Management. Int. J. Environ. Res. Public Health 2021, 18, 9248. [Google Scholar] [CrossRef]
- Meira ECruz, M.; Salles, C.; Seixas, L.; D’Elia, C.; Rocha, I.; Gozal, D. Comorbid insomnia and sleep apnea in children: A preliminary explorative study. J. Sleep Res. 2023, 32, e13705. [Google Scholar] [CrossRef]
- Yelov, L.; Reiter, J.; Cruz, M.M.E.; Gileles-Hillel, A. The association of obstructive sleep apnea and behavioral insomnia in children aged 10 and under. J. Clin. Sleep Med. 2023, 20, 245–251. [Google Scholar] [CrossRef]
- Cole, T.J. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L.; Quan, S. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Westchester, IL, USA, 2007; Volume 1. [Google Scholar]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for Scoring Respiratory Events in Sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef] [PubMed]
- Lecuelle, F.; Gustin, M.-P.; Leslie, W.; Mindell, J.A.; Franco, P.; Putois, B. French validation of the sleep disturbance scale for children (SDSC) in young children (aged 6 months to 4 years). Sleep Med. 2020, 67, 56–65. [Google Scholar] [CrossRef]
- Putois, B.; Leslie, W.; Gustin, M.P.; Challamel, M.-J.; Raoux, A.; Guignard-Perret, A.; Weick, D.; Sauzeau, J.-B.; Herbillon, V.; Zourou, F.; et al. The French Sleep Disturbance Scale for Children. Sleep Med. 2017, 32, 56–65. [Google Scholar] [CrossRef]
- Snow, A.; Gozal, E.; Malhotra, A.; Tiosano, D.; Perlman, R.; Vega, C.; Shahar, E.; Gozal, D.; Hochberg, Z.; Pillar, G. Severe hypersomnolence after pituitary/hypothalamic surgery in adolescents: Clinical characteristics and potential mechanisms. Pediatrics 2002, 110, e74. [Google Scholar] [CrossRef]
- Gustin, M.-P.; Putois, B.; Guyon, A.; Lecendreux, M.; Challamel, M.-J.; Plancoulaine, S.; Bioulac-Rogier, S.; Schroder, C.; Royant-Parola, S.; Huguelet, S.; et al. French Sleepiness Scale for Adolescents-8 items: A discriminant and diagnostic validation. L’Encéphale 2023, 49, 109–116. [Google Scholar] [CrossRef]
- Achenbach, T.M. Program Manual for the 1991 Child Behavior Checklist/4-18 Profile; University Associates in Psychiatry: Burlington, VT, USA, 1991. [Google Scholar]
- Achenbach, T.M.; Ruffle, T.M. The Child Behavior Checklist and Related Forms for Assessing Behavioral/Emotional Problems and Competencies. Pediatr. Rev. 2000, 21, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Fombonne, E.; Chehdan, F.; Carradec, A.M.; Achard, S.; Navarro, N.; Reis, S. Le Child Behavioral Checklist: Un instrument pour la recherche en psychiatrie de l’enfant. Psychiatry Psychobiol. 1988, 3, 409–418. [Google Scholar] [CrossRef]
- Sun, S.; Wang, S. The Children’s Depression Inventory in Worldwide Child Development Research: A Reliability Generalization Study. J. Child. Fam. Stud. 2015, 24, 2352–2363. [Google Scholar] [CrossRef]
- Conners, C.K. Symposium: Behaviour modification by drugs 11. Psychological effects of stimulan drugs in children with minimal brain dysfunction. Pediatrics 1972, 49, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Kaditis, A.G.; Alonso Alvarez, M.L.; Boudewyns, A.; Abel, F.; Alexopoulos, E.I.; Ersu, R.; Joosten, K.; Larramona, H.; Miano, S.; Narang, I.; et al. ERS statement on obstructive sleep disordered breathing in 1- to 23-month-old children. Eur. Respir. J. 2017, 50, 1700985. [Google Scholar] [CrossRef] [PubMed]
- Kaditis, A.G.; Alonso Alvarez, M.L.; Boudewyns, A.; Alexopoulos, E.I.; Ersu, R.; Joosten, K.; Larramona, H.; Miano, S.; Narang, I.; Trang, H.; et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: Diagnosis and management. Eur. Respir. J. 2016, 47, 69–94. [Google Scholar] [CrossRef]
- Capdevila, O.S.; Kheirandish-Gozal, L.; Dayyat, E.; Gozal, D. Pediatric Obstructive Sleep Apnea: Complications, Management, and Long-term Outcomes. Proc. Am. Thorac. Soc. 2008, 5, 274–282. [Google Scholar] [CrossRef]
- Python Software Foundation. Python, Version 3.11.7; Python Software Foundation: Wilmington, DE, USA, 2023.
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental algorithms for scientific computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef]
- Vallat, R. Pingouin: Statistics in Python. J. Open Source Softw. 2018, 3, 1026. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Ong, J.C.; Crawford, M.R.; Wallace, D.M. Sleep Apnea and Insomnia: Emerging Evidence for Effective Clinical Management. Chest 2021, 159, 2020–2028. [Google Scholar] [CrossRef]
- Calhoun, S.L.; Fernandez-Mendoza, J.; Vgontzas, A.N.; Liao, D.; Bixler, E.O. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: Gender effects. Sleep Med. 2014, 15, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Björnsdóttir, E.; Janson, C.; Sigurdsson, J.F.; Gehrman, P.; Perlis, M.; Juliusson, S.; Arnardottir, E.S.; Kuna, S.T.; Pack, A.I.; Gislason, T.; et al. Symptoms of Insomnia among Patients with Obstructive Sleep Apnea Before and After Two Years of Positive Airway Pressure Treatment. Sleep 2013, 36, 1901–1909. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ren, R.; Lei, F.; Zhou, J.; Zhang, J.; Wing, Y.-K.; Sanford, L.D.; Tang, X. Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 45, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Krakow, B.; Melendrez, D.; Ferreira, E.; Clark, J.; Warner, T.D.; Sisley, B.; Sklar, D. Prevalence of Insomnia Symptoms in Patients With Sleep-Disordered Breathing. Chest 2001, 120, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Sweetman, A.M.; Lack, L.C.; Catcheside, P.G.; Antic, N.A.; Chai-Coetzer, C.L.; Smith, S.S.; Douglas, J.A.; McEvoy, R.D. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med. Rev. 2017, 33, 28–38. [Google Scholar] [CrossRef]
- Sweetman, A.; Lack, L.; Bastien, C. Co-Morbid Insomnia and Sleep Apnea (COMISA): Prevalence, Consequences, Methodological Considerations, and Recent Randomized Controlled Trials. Brain Sci. 2019, 9, 371. [Google Scholar] [CrossRef]
- Niedzielski, A.; Chmielik, L.P.; Mielnik-Niedzielska, G.; Kasprzyk, A.; Bogusławska, J. Adenoid hypertrophy in children: A narrative review of pathogenesis and clinical relevance. BMJ Paediatr. Open 2023, 7, e001710. [Google Scholar] [CrossRef]
- Viveros, N. Adenoid and Tonsil Hypertrophy in Children and Facial Malformations. J. Otolaryngol.-ENT Res. 2016, 4, 18–20. [Google Scholar] [CrossRef]
- Alsubie, H.S.; BaHammam, A.S. Obstructive Sleep Apnoea: Children are not little Adults. Paediatr. Respir. Rev. 2017, 21, 72–79. [Google Scholar] [CrossRef]
- Choi, J.H.; Kim, E.J.; Choi, J.; Kwon, S.Y.; Kim, T.H.; Lee, S.H.; Lee, H.M.; Shin, C.; Lee, S.H. Obstructive Sleep Apnea Syndrome: A Child is not Just a Small Adult. Ann. Otol. Rhinol. Laryngol. 2010, 119, 656–661. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
| <4 Years Old (n = 46) | 4–16 Years Old (n = 154) | p | Effect Size | |
|---|---|---|---|---|
| General characteristics | ||||
| Age (years) | 2.5 [0.6–3.9] | 10.9 [4.1–16.7] | - | - |
| Sex | ||||
| Females | 21 (45.7) | 74 (48.1) | 0.9 | 0.02 |
| BMI z-score | 0.4 [−2.7–5.5] | 0.5 [−2.1–18.3], n = 153 | 0.2 | 0.1 |
| Obesity | 3 (10.3), n = 29 | 18 (11.8), n = 153 | 1 | 0.02 |
| Pre-term | 7 (15.2) | 15 (10.6), n = 142 | 0.4 | 0.06 |
| Neurodevelopmental disorder | 9 (19.6) | 65 (42.2) | 0.005 | 0.2 |
| ADHD | - | 19 (12.3) | - | |
| Epilepsy | 1 (2.2) | 15 (9.7) | 0.1 | 0.1 |
| Treatments | ||||
| Wake-promoting only | 0 (0.0) | 15 (9.7) | 0.03 | 0.2 |
| Sleep-inducing only | 2 (4.3) | 17 (11.0) | 0.3 | 0.1 |
| Both | 0 (0.0) | 21 (13.6) | 0.005 | 0.2 |
| Reason for PSG | ||||
| SDB | 41 (89.1) | 88 (57.1) | 0.003 | 0.3 |
| Insomnia | 2 (4.3) | 39 (25.3) | ||
| Hypersomnia | 1 (2.2) | 24 (15.6) | ||
| Parasomnia | 2 (4.3) | 3 (1.9) | ||
| OSA | ||||
| OAHI (/h) | 5.0 [0.0–43.9] | 1.6 [0.0–64.9] | <0.001 | 0.3 |
| Pathological OAHI (≥2/h) | 36 (78.3) | 66 (42.9) | <0.001 | 0.5 |
| Mild OSA [2–5)/h | 13 (36.1) | 36 (54.5) | 0.1 | 0.2 |
| Moderate OSA [5–10)/h | 6 (16.7) | 11 (16.7) | ||
| Severe OSA ≥ 10/h | 17 (47.2) | 19 (28.8) | ||
| Type I | 17 (47.2) | 26 (39.4) | 0.2 | 0.2 |
| Type II | 0 (0) | 5 (7.6) | ||
| Type III | 19 (52.8) | 35 (53.0) | ||
| Insomnia | ||||
| SDSC-DIMS | 15.2 [8.0–34.0] | 15.0 [7.0–31.0] | - | |
| Pathological insomnia | 21 (45.7) | 29 (18.8) | <0.001 | 0.3 |
| SDSC-initiation/20 | 7.0 [4–19] | 8.0 [4–19] | 0.05 | 0.1 |
| SDSC-maintaining/5 | 2.0 [1–5] | 2.0 [1–5] | 0.2 | 0.1 |
| COMISA | ||||
| In all patients | 18 (39.1) | 9 (5.8) | <0.001 | 0.4 |
| In OSA subgroup | 18 (50.0) | 9 (13.6) | <0.001 | 0.4 |
| OSA-Only (n = 18) | COMISA (n = 18) | p | Effect Size | |
|---|---|---|---|---|
| General characteristics | ||||
| Age (years) | 2.5 [0.7–3.8] | 2.4 [0.6–3.9] | 0.9 | 0.02 |
| Sex | ||||
| Females | 10 (55.6) | 7 (38.9) | 0.5 | 0.2 |
| BMI z-score | 1.0 [−2.4–5.5] | 0.7 [−2.2–2.5] | 0.6 | 0.1 |
| Obesity | 3.0 (27.3), n = 11 | 0 (0), n = 11 | 0.2 | 0.4 |
| Neurodevelopmental disorder | 5 (27.8) | 4 (22.2) | 1 | 0.06 |
| Epilepsy | 0 (0) | 1 (5.6) | 1 | 0.2 |
| Sleep-inducing treatment | 1 (5.6) | 1 (5.6) | 1 | 0 |
| OSA type | ||||
| Type I | 4 (22.2) | 13 (72.2) | 0.008 | 0.5 |
| Type III | 14 (77.8) | 5 (27.8) | ||
| PSG sleep architecture | ||||
| TST (min) | 497.5 [396.0–667.0] | 526.0 [366.0–644.0] | 0.3 | 0.2 |
| SOL (min) | 11.4 [1.3–405.5], n = 17 | 9.4 [2.4–194.0], n = 17 | 0.8 | 0.06 |
| SE (%) | 81.2 [63.4–96.8] | 86.8 [68.1–96.0] | 0.4 | 0.2 |
| WASO (min) | 107.2 [21.0–239.0] | 83.0 [24.0–205.0] | 0.4 | 0.2 |
| N1 sleep (%TST) | 11.6 [4.2–30.3] | 15.3 [7.5–20.3] | 0.4 | 0.2 |
| N2 sleep (%TST) | 0.4 [0.3–71.1] | 0.4 [0.1–61.6] | 0.9 | 0.02 |
| N3 sleep (%TST) | 25.4 [0.0–39.3] | 27.3 [7.3–43.3] | 1 | 0.01 |
| REM sleep (%TST) | 27.8 [18.9–35.6] | 24.4 [16.5–35.1] | 0.4 | 0.2 |
| Arousal index (/h) | 28.8 [6.2–72.0] | 31.8 [8.7–44.5] | 0.8 | 0.04 |
| Arousal-and-awakening index (/h) | 32.7 [12.5–86.5] | 37.2 [12.0–52.5] | 0.8 | 0.05 |
| PLMI(/h) | 6.1 [0.0–11.3], n = 9 | 3.3 [0.0–12.9], n = 11 | 0.2 | 0.3 |
| PSG respiratory parameters | ||||
| OAHI (/h) | 5.4 [2.0–29.4] | 11.7 [2.7–43.9] | 0.2 | 0.2 |
| Mild OSA [2–5)/h | 9 (50.0) | 4 (22.2) | 0.2 | 0.3 |
| Moderate OSA [5–10)/h | 3 (16.7) | 3 (16.7) | ||
| Severe OSA ≥ 10/h | 6 (33.3) | 11 (61.1) | ||
| RERA (/h) | 9.6 [0.2–20.2] | 12.2 [2.6–18.3] | 0.6 | 0.09 |
| Mean SpO2 (%) | 96.5 [94.6–98.3] | 96.9 [92.1–98.5] | 0.9 | 0.02 |
| SpO2 < 90% (min) | 0.6 [0.0–35.8] | 0.6 [0.0–94.9] | 1 | 0 |
| ODI > 3 (/h) | 7.5 [0.8–25.1] | 7.8 [0.3–74.8] | 0.4 | 0.1 |
| Mean CO2 (mmHg) | 40.1 [37.0–52.1], n = 17 | 42.1 [33.5–49.0] | 0.9 | 0.02 |
| CO2 > 50 mmHg (%) | 0.0 [0.0–69.5], n = 17 | 0.0 [0.0–10.0], n = 17 | 0.8 | 0.04 |
| Insomnia | ||||
| SDSC-DIMS/40 | 11.0 [9.0–16.0] | 23.5 [17.0–34.0] | <0.001 | 0.9 |
| SDSC-initiation/20 | 6.0 [4–8] | 11.5 [5–19] | <0.001 | 0.7 |
| SDSC-maintaining/5 | 1.0 [1–3] | 3.8 [1–5] | <0.001 | 0.7 |
| no-OSA no-INS (n = 68) | INS-Only (n = 20) | OSA-Only (n = 57) | COMISA (n = 9) | p | |
|---|---|---|---|---|---|
| General characteristics | |||||
| Age (years) | 10.5 [4.6–16.1] | 11.5 [5.5–16.7] | 10.7 [4.1–16.6] | 9.3 [4.1–16.7] | 0.3 |
| Sex | |||||
| Females | 34 (50.0) | 9 (45.0) | 27 (47.4) | 4 (44.4) | 0.9 |
| BMI z-score | 0.0 [−1.9–9.0] | 0.9 [−1.6–8.2] | 1.2 [−2.1–18.3], n = 56 | 0.2 [−1.3–9.3] | 0.4 |
| Obesity | 7 (10.3) | 2 (10.0) | 8 (14.3), n = 56 | 1 (11.1) | 0.9 |
| Neurodevelopmental disorder | 30 (44.1) | 9 (45.0) | 22 (38.6) | 4 (44.4) | 0.9 |
| ADHD | 11 (16.2) | 5 (25.0) | 2 (3.5) | 1 (11.1) | 0.05 c+ |
| Epilepsy | 7 (10.3) | 1 (5.0) | 6 (10.5) | 1 (11.1) | 0.9 |
| Treatments | |||||
| Wake-promoting only | 7 (10.3) | 2 (10.0) | 6 (10.5) | 0 (0) | 0.8 |
| Sleep-inducing only | 9 (13.2) | 0 (0) | 6 (10.5) | 2 (22.2) | 0.3 |
| Both | 10 (14.7) | 4 (20.0) | 5 (8.8) | 2 (22.2) | 0.5 |
| OSA type | |||||
| Type I | - | - | 21 (36.8) | 5 (55.6) | 0.4 |
| Type II | - | - | 4 (7.0) | 1 (11.1) | |
| Type III | - | - | 32 (56.1) | 3 (33.3) | |
| PSG sleep architecture | |||||
| TST (min) | 536.0 [273.0–665.0] | 499.0 [395.0–610.0] | 502.0 [264.0–684.0] | 499.0 [411.0–548.0] | 0.1 |
| SOL (min) | 19.8 [0.8–190.9] | 26.8 [5.4–299.0] | 14.8 [1.3–293.5], n = 56 | 21.9 [3.7–80.6] | 0.1 |
| SE (%) | 89.9 [62.9–97.6] | 91.2 [71.6–96.9] | 86.7 [52.4–97.7] | 88.6 [73.4–95.1] | 0.1 |
| WASO (min) | 57.8 [14.0–217.0] | 46.8 [16.5–193.0] | 75.5 [13.5–256.5] | 62.0 [28.5–180.5] | 0.06 |
| N1 sleep (%TST) | 9.7 [2.3–23.3] | 8.6 [0.9–15.6] | 11.6 [2.0–32.8] | 8.4 [4.7–14.7] | 0.02 c+ |
| N2 sleep (%TST) | 40.0 [0.3–56.7] | 41.3 [0.3–60.0] | 37.7 [0.3–69.8] | 47.3 [0.4–60.4] | 0.2 |
| N3 sleep (%TST) | 24.2 [1.0–40.6] | 24.7 [9.7–41.1] | 23.0 [0.6–37.1] | 23.2 [7.1–34.0] | 0.5 |
| REM sleep (%TST) | 22.8 [11.9–35.4] | 21.0 [10.2–31.4] | 22.2 [7.4–30.9] | 22.5 [19.5–31.7] | 0.7 |
| Arousal index (/h) | 15.0 [2.7–39.5] | 9.9 [4.3–18.5] | 22.4 [4.9–75.3] | 16.8 [8.3–27.5] | <0.001 a#,c# |
| Arousal-and-awakening index (/h) | 21.3 [4.0–43.0], n = 39 | 17.8 [6.0–24.9], n = 8 | 27.2 [8.2–90.8], n = 50 | 22.0 [12.5–33.7], n = 6 | 0.006 c+ |
| PLMI (/h) | 1.6 [0.0–22.5], n = 65 | 2.5 [0.0–15.8] | 1.8 [0.0–27.8], n = 55 | 4.3 [0.0–12.5], n = 8 | 0.5 |
| PSG respiratory parameters | |||||
| OAHI (/h) | 0.7 [0.0–1.9] | 0.4 [0.0–1.5] | 4.7 [2.1–64.9] | 3.3 [2.1–5.8] | <0.001 a#, b+, c# |
| Mild OSA [2–5)/h | - | - | 29 (50.9) | 7 (77.8) | 0.1 |
| Moderate OSA [5–10)/h | - | - | 9 (15.8) | 2 (22.2) | |
| Severe OSA ≥ 10/h | - | - | 19.0 (33.3) | 0 (0) | |
| RERA (/h) | 1.9 [0.2–9.5] | 1.1 [0.1–6.7] | 8.1 [0.7–45.4] | 6.0 [1.6–8.9] | <0.001 a#,c# |
| Mean SpO2 (%) | 96.8 [94.7–98.3], n = 67 | 96.6 [92.4–97.7] | 96.3 [91.9–98.7], n = 56 | 97.3 [93.1–97.8] | 0.04 |
| SpO2 < 90% (min) | 0.0 [0.0–9.7], n = 67 | 0.0 [0.0–9.2] | 0.0 [0.0–54.4], n = 56 | 0.0 [0.0–0.0] | 0.09 |
| ODI > 3 (/h) | 2.1 [0.0–11.2], n = 67 | 1.4 [0.0–8.0] | 4.2 [0.2–62.7], n = 56 | 2.4 [0.4–9.2] | <0.001 c+ |
| Mean CO2 (mmHg) | 42.8 [36.4–48.8], n = 66 | 42.6 [34.6–49.2] | 42.7 [33.2–49.1], n = 56 | 42.4 [38.7–50.4] | 0.7 |
| CO2 > 50 mmHg (%) | 0.0 [0.0–35.4], n = 66 | 0.0 [0.0–47.7] | 0.0 [0.0–45.1], n = 56 | 0.0 [0.0–67.8] | 0.5 |
| Questionnaires | |||||
| SDSC-DIMS/35 | 13.0 [7–21] | 25.5 [22–31] | 13.0 [2–21] | 26.0 [22–31] | <0.001 b#,c# |
| SDSC-initiation/20 | - | 15.5 [12–19] | - | 17.0 [13–18] | 0.9 |
| SDSC-maintaining/5 | - | 3.0 [2–5] | - | 4.0 [2–5] | 0.3 |
| FSSA/24 | 6.0 [0–24], n = 61 | 3.5 [0–10], n = 18 | 6.0 [0–21], n = 46 | 6.5 [1–11] | 0.06 |
| FSSA > 10 | 11 (18.0), n = 61 | 0 (0), n = 18 | 16 (37.2), n = 46 | 1 (12.5), n = 8 | 0.007 c+ |
| CDI/54 | 10.0 [2–23], n = 34 | 13.5 [6–39], n = 12 | 14.5 [4–28], n = 10 | 17.0 [8–24], n = 3 | 0.1 |
| CDI ≥ 16 | 9 (26.5), n = 34 | 5 (41.7), n = 12 | 5 (50.0), n = 10 | 2 (66.7), n = 3 | 0.3 |
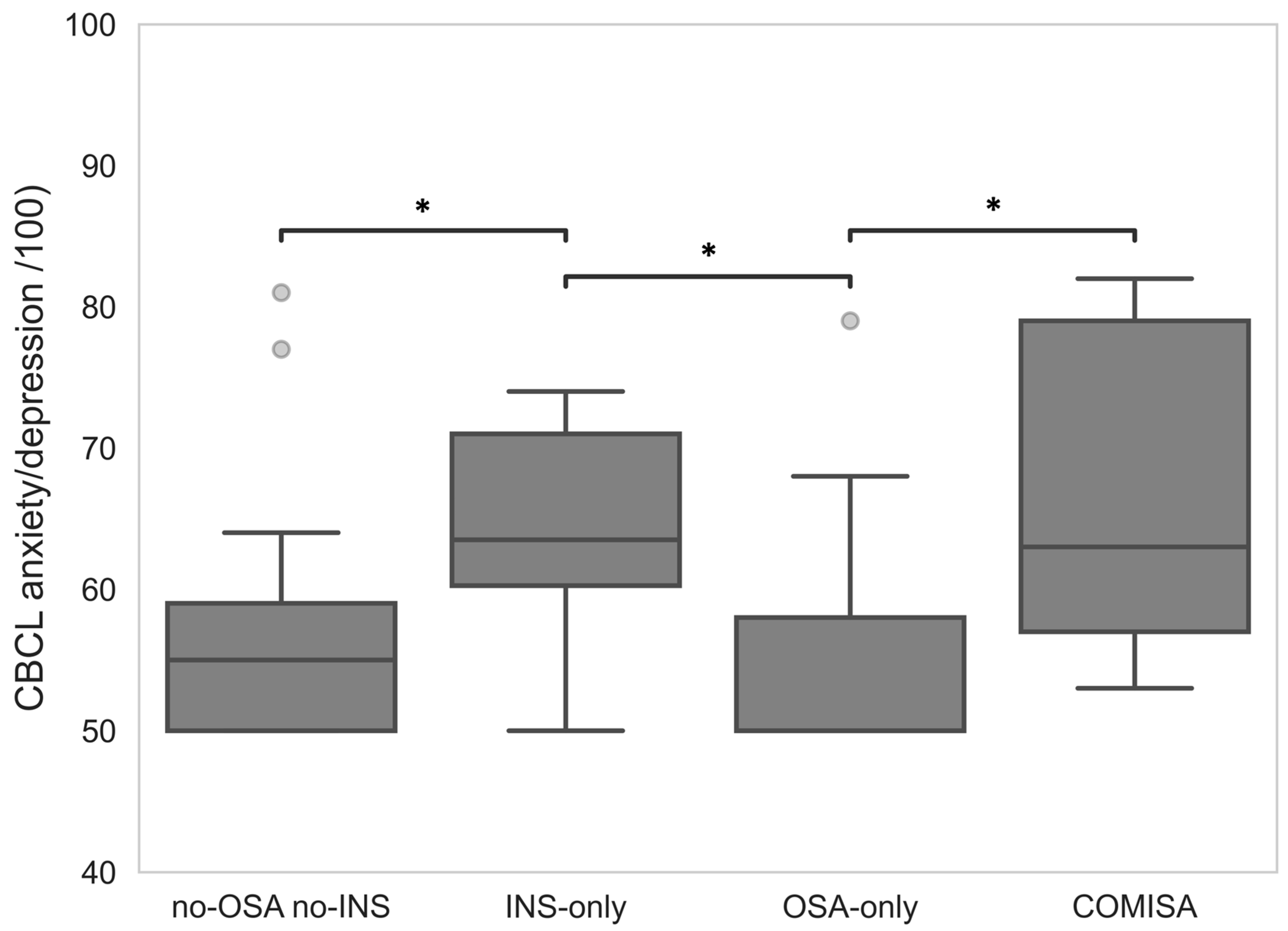
| CBCL anxiety/depression/100 | 55.0 [50–81], n = 29 | 63.5 [50–74], n = 8 | 50.0 [50–79], n = 29 | 63.0 [53–82], n = 5 | 0.008 b+,c+ |
| CBCL ≥ 70 | 2 (6.9), n = 29 | 3 (37.5), n = 8 | 1 (3.4), n = 29 | 2 (40.0), n = 5 | 0.008 |
| Conners/30 | 10.0 [0–26], n = 57 | 14.0 [2–27], n = 16 | 11.0 [0–27], n = 38 | 14.0 [4–22] | 0.5 |
| Conners > 15 | 13 (22.8), n = 57 | 7 (43.8), n = 16 | 11 (28.9), n = 38 | 4 (50.0) | 0.2 |
| School difficulties | 25 (41.0), n = 61 | 4 (23.5), n = 17 | 21 (45.7), n = 46 | 3 (33.3) | 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunel, L.; Comajuan, M.; Plancoulaine, S.; Putois, B.; Lioret, J.; Thieux, M.; Coutier, L.; Franco, P.; Guyon, A. Comorbid Insomnia and Sleep Apnea Across the Pediatric Age: A Polysomnographic Study. Children 2025, 12, 1250. https://doi.org/10.3390/children12091250
Brunel L, Comajuan M, Plancoulaine S, Putois B, Lioret J, Thieux M, Coutier L, Franco P, Guyon A. Comorbid Insomnia and Sleep Apnea Across the Pediatric Age: A Polysomnographic Study. Children. 2025; 12(9):1250. https://doi.org/10.3390/children12091250
Chicago/Turabian StyleBrunel, Lisa, Marion Comajuan, Sabine Plancoulaine, Benjamin Putois, Julien Lioret, Marine Thieux, Laurianne Coutier, Patricia Franco, and Aurore Guyon. 2025. "Comorbid Insomnia and Sleep Apnea Across the Pediatric Age: A Polysomnographic Study" Children 12, no. 9: 1250. https://doi.org/10.3390/children12091250
APA StyleBrunel, L., Comajuan, M., Plancoulaine, S., Putois, B., Lioret, J., Thieux, M., Coutier, L., Franco, P., & Guyon, A. (2025). Comorbid Insomnia and Sleep Apnea Across the Pediatric Age: A Polysomnographic Study. Children, 12(9), 1250. https://doi.org/10.3390/children12091250





