Bluish-Green Coloration of the Nipples: A Diagnostic Clue for Retroareolar Cysts
Abstract
Highlights
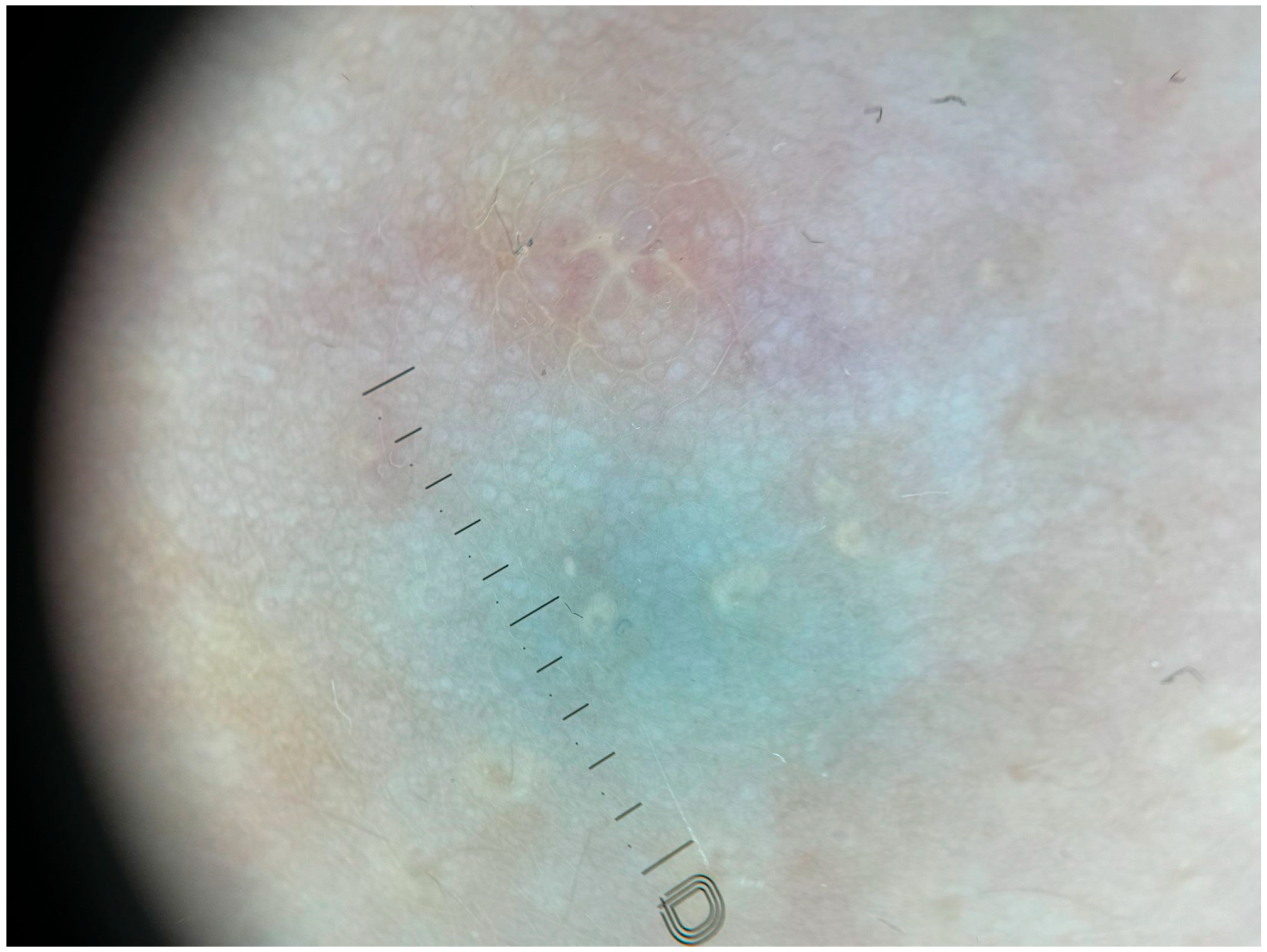
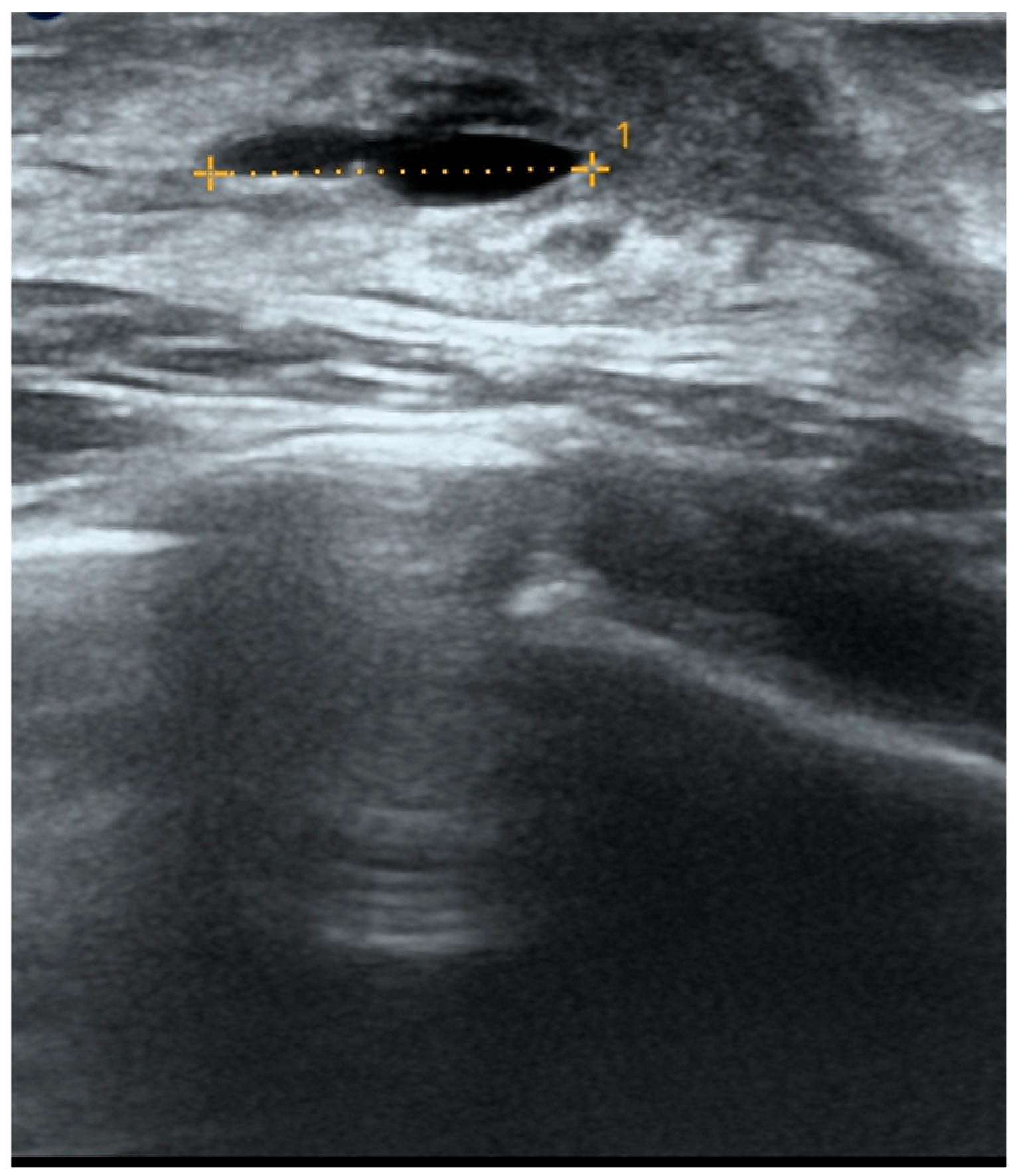
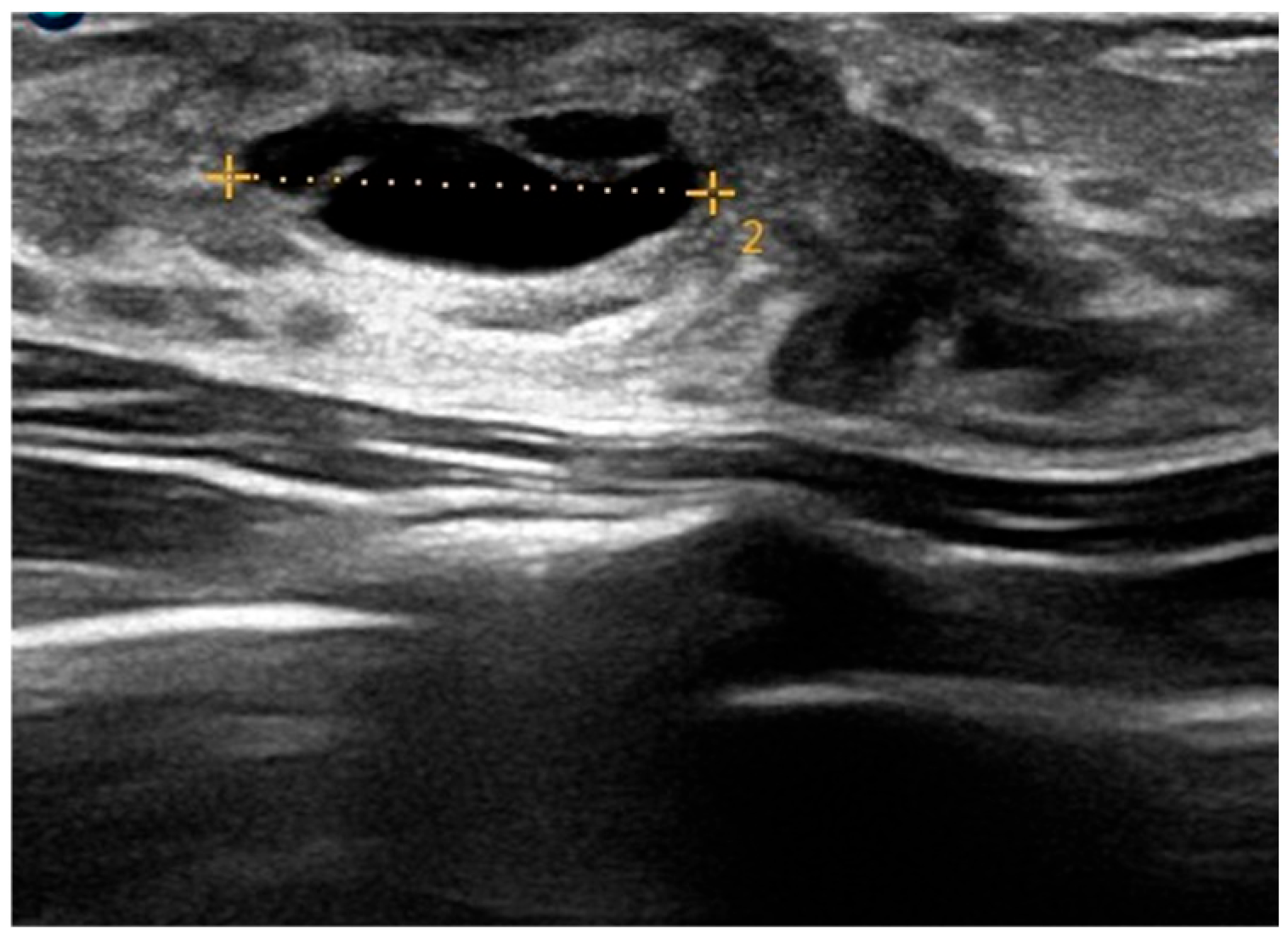
- Bilateral bluish-green retroareolar macules in a pubertal girl were diagnosed as benign retroareolar cysts through dermoscopic and ultrasound evaluation, with stability over one year of conservative management.
- Recognizing this benign presentation can prevent unnecessary diagnostic procedures and support conservative management, preserving normal pubertal breast development.
Abstract
1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Almuhanna, A.F.; Almuhanna, A.F.; Alzuabi, R.S.; Alshamlan, R.A.; Almarhoon, F.H. Cyst of Montgomery: An uncommon adolescent breast lump. J. Fam. Community Med. 2020, 27, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Huneeus, A.; Schilling, A.; Horvath, E.; Pinochet, M.; Carrasco, O. Retroareolar Cysts in the Adolescent. J. Pediatr. Adolesc. Gynecol. 2003, 16, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Mioso, G.; Gnesotto, L.; Cutrone, M.; Parlangeli, A.; Naldi, L.; Sechi, A. Pubertal retroareolar cysts presenting as bluish lumps: New cases and literature review. J. Paediatr. Child Health 2024, 60, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Sechi, A.; Vaccari, S.; Parlangeli, A.; Vara, G.; Patrizi, A. Homogeneous blue lumps of the nipple-areola complex in pubertal girls. Pediatr. Dermatol. 2021, 38, 887–891. [Google Scholar] [CrossRef] [PubMed]
- Rusiñol, L.; Amat-Samaranch, V.; Baselga, E.; Puig, L.; Roé, E. Prepubertal retroareolar cysts. Pediatr. Dermatol. 2021, 38, 1368–1369. [Google Scholar] [CrossRef] [PubMed]
- Oiso, N.; Kawada, A. The Dermoscopic Features in Infantile Hemangioma. Pediatr. Dermatol. 2011, 28, 591–593. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Chang, Y.-W.; Oh, J.H.; Hwang, J.; Hong, S.S.; Kim, H. Breast Lesions in Children and Adolescents: Diagnosis and Management. Korean J. Radiol. 2018, 19, 978. [Google Scholar] [CrossRef] [PubMed]
- Haliasos, E.C.; Kerner, M.; Jaimes, N.; Zalaudek, I.; Malvehy, J.; Hofmann-Wellenhof, R.; Braun, R.P.; Marghoob, A.A. Dermoscopy for the Pediatric Dermatologist Part III: Dermoscopy of Melanocytic Lesions. Pediatr. Dermatol. 2013, 30, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Samimi, M.; Perrinaud, A.; Naouri, M.; Maruani, A.; Perrodeau, E.; Vaillant, L.; Machet, L. High-resolution ultrasonography assists the differential diagnosis of blue naevi and cutaneous metastases of melanoma: Ultrasonography for differential diagnosis of naevi and melanoma metastases. Br. J. Dermatol. 2010, 163, 550–556. [Google Scholar] [CrossRef] [PubMed]


| Patient | References | Age | Clinical Presentation |
|---|---|---|---|
| 1 | Sechi [4] | 10 years 3 months | Two weeks’ history of monolateral blue cyst |
| 2 | Sechi [4] | 10 years 6 months | Three-month history of bilateral blue lumps |
| 3 | Rusiñol [5] | 11 years | Bluish cyst, asymptomatic, 1 year duration |
| 4 | Rusiñol [5] | 12 years | Asymptomatic bluish cyst, 3 years duration |
| 5 | Huneeus [2] | Not reported | Bluish appearance of retroareolar cyst |
| 6 | Huneeus [2] | Not reported | Bluish appearance of retroareolar cyst |
| 7 | Mioso [3] | 10 years 2 months | Monolateral green-blue cyst, 2 weeks duration |
| 8 | Mioso [3] | 11 years 4 months | Bilateral blue lumps, 1 year duration |
| 9 | Mioso [3] | 11 years 7 months | Monolateral blue cyst, 1-year duration |
| 10 | Our case | 11 years | Eight-month history of bilateral symmetrical bluish-green cyst |
| Differential Diagnosis | Clinical Features | Dermoscopic Features | Ultrasound Features | Age/Notes |
|---|---|---|---|---|
| Retroareolar cysts | Superficial, soft, smooth and bluish lesions | Homogeneous, unstructured greenish discoloration with blurred edges | Anechoic, oval, thin-walled mass with posterior enhancement; no Doppler flow | Prepuberal age |
| Deep haemangiomas | Bluish-purplish swelling or mass | Normal or bluish skin, sometimes with a telangiectatic hue | Well-defined, hypoechoic, hypervascular structure with rapid flow (growth phase); more echogenic with reduced vessel size/density (involution phase) | Early in life. Consider presence of superficial hemangioma component. |
| Lymphatic malformations | Multiloculated, translucent vesicles | Yellowish-white lacunae separated by a thin, pale, whitish area | Well-defined, hyperechoic lesion with heterogeneous texture; hypervascular on color Doppler | Early in life |
| Hematomas | Painful lumps or bumps characterized by skin discoloration | Violaceous discoloration with blurred edges; evolves into green/yellowish hues over time | Hyperechoic with ill-defined margins acutely; progresses to complex cystic lesion with internal debris and septations | Resolve spontaneously within 2–3 weeks |
| Common blue nevi | Sharply circumscribed, homogeneously blue lesions | Free from pigment networks, dots, globules, streaks, or vascular patterns | Hypoechoic, dish-shaped pattern | Non-bilateral |
| Surgical dye-related discoloration | Persistent blue discoloration on the nipple surface | Homogeneous bluish discoloration with blurred margins | Negative | Consider surgical history |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Curic, T.; Bellinato, F.; Gisondi, P.; Girolomoni, G. Bluish-Green Coloration of the Nipples: A Diagnostic Clue for Retroareolar Cysts. Children 2025, 12, 1224. https://doi.org/10.3390/children12091224
Curic T, Bellinato F, Gisondi P, Girolomoni G. Bluish-Green Coloration of the Nipples: A Diagnostic Clue for Retroareolar Cysts. Children. 2025; 12(9):1224. https://doi.org/10.3390/children12091224
Chicago/Turabian StyleCuric, Tea, Francesco Bellinato, Paolo Gisondi, and Giampiero Girolomoni. 2025. "Bluish-Green Coloration of the Nipples: A Diagnostic Clue for Retroareolar Cysts" Children 12, no. 9: 1224. https://doi.org/10.3390/children12091224
APA StyleCuric, T., Bellinato, F., Gisondi, P., & Girolomoni, G. (2025). Bluish-Green Coloration of the Nipples: A Diagnostic Clue for Retroareolar Cysts. Children, 12(9), 1224. https://doi.org/10.3390/children12091224







