Utility of Clinical Signs in the Diagnosis of Testicular Torsion in Pediatric Age: Optimization of Timing in a Time-Sensitive Pathology
Abstract
1. Introduction
2. Materials and Methods
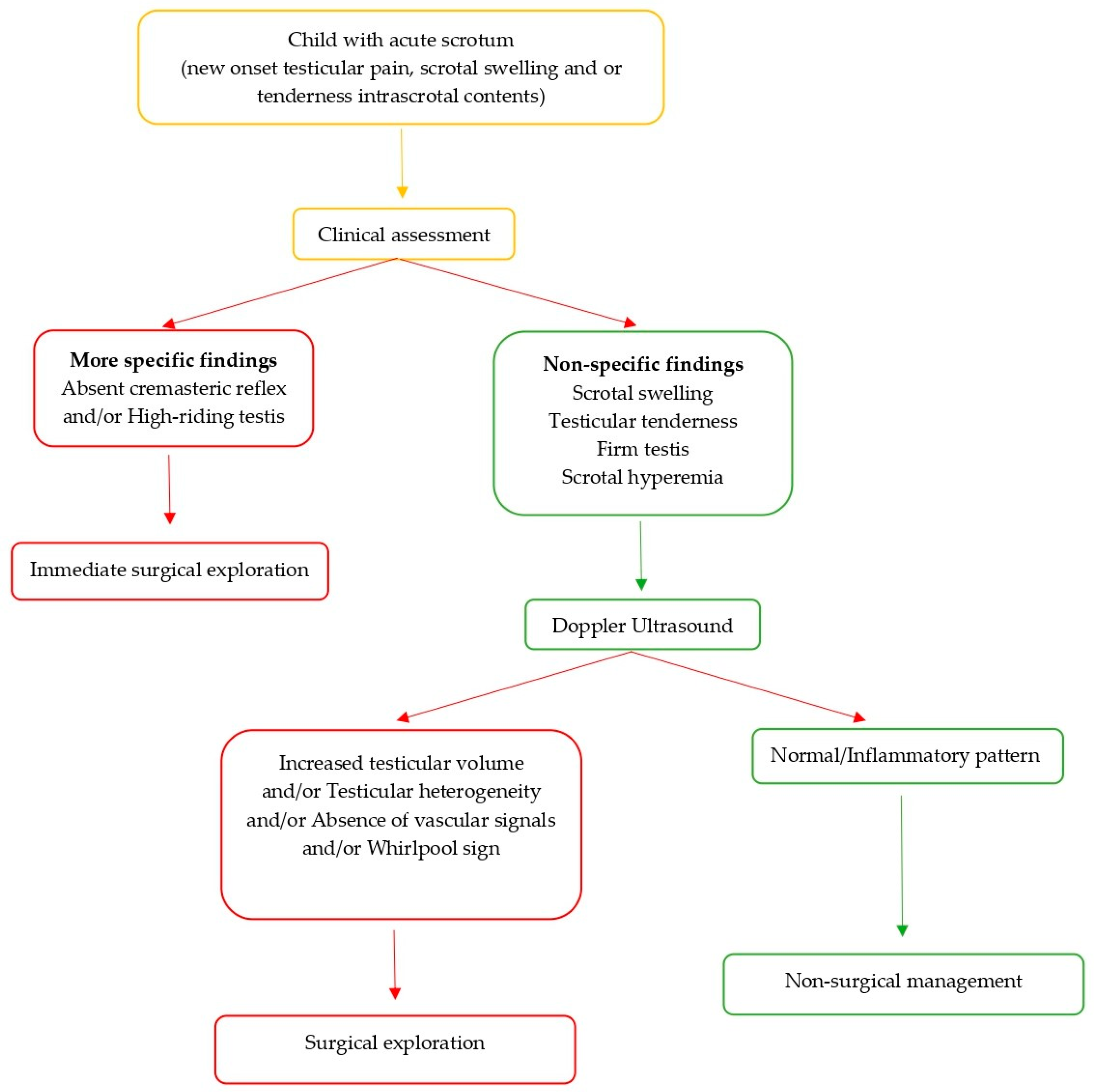
2.1. Diagnostic Evaluation and Management
2.2. Data Collection
2.3. Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qin, K.R.; Qu, L.G. Diagnosing with a TWIST: Systematic review and Meta-analysis of a testicular torsion risk score. J. Urol. 2022, 208, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Gkalonaki, I.; Patoulias, I.; Anastasakis, M.; Panteli, C.; Patoulias, D. The challenging diagnosis of acute scrotum: Remaining difficulties and further insights. Folia Medica Cracoviensia 2023, 62, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Shunmugam, M.; Goldman, R.D. Testicular torsion in children. Can. Fam. Physician. 2021, 67, 669–671. [Google Scholar] [CrossRef] [PubMed]
- Liang, T.; Metcalfe, P.; Sevcik, W.; Noga, M. Retrospective review of diagnosis and treatment in children presenting to the pediatric department with acute scrotum. Am. J. Roentgenol. 2013, 200, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, J.A.; Tiseo, B.C.; Barayan, G.A.; Rosman, B.M.; Torricelli, F.C.M.; Passerotti, C.C.; Srougi, M.; Retik, A.B.; Nguyen, H.T. Development and initial validation of a scoring system to diagnose testicular torsion in children. J. Urol. 2013, 189, 1859–1864. [Google Scholar] [CrossRef] [PubMed]
- Alkhori, N.A.; Barth, R.A. Pediatric scrotal ultrasound: Review and update. Pediatr. Radiol. 2017, 47, 1125–1133. [Google Scholar] [CrossRef] [PubMed]
- Afsarlar, C.E.; Ryan, S.L.; Donel, E.; Baccam, T.H.; Jones, B.; Chandwani, B.; Au, J.; Huang, G.O.; Gonzales, E.T.; Janzen, N.; et al. Standardized process to improve patient flow from the Emergency Room to the Operating Room for pediatric patients with testicular torsion. J. Pediatr. Urol. 2016, 12, 233.e1–233.e4. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Mustapić, K.; Jukić, M.; Todorić, J.; Mrklić, I.; Mešštrović, J.; Jurić, I.; Furlan, D. Management of acute scrotum in children: A 25-year single center experience on 558 pediatric patients. Can. J. Urol. 2016, 23, 8594–8601. [Google Scholar]
- IBM SPSS Statistics for Windows, Version 25.0, IBM Corp.: Armonk, NY, USA, 2017.
- Gupta, A.; Manohar, C.; Keshavamurthy, R.; Shivalingaiah, M.; Sharanbasappa, B.; Singh, V.K. Evaluation of testicular workup for ischemia and suspected torsion score in patients presenting with acute scrotum. Urol. Ann. 2018, 10, 20–23. [Google Scholar] [CrossRef]
- Coles, V.; Elagami, H.; Bhandarker, K.; Awolaran, G.; Murphy, F.; Yardley, I.; Hallows, R.; Davenport, M. The acute scrotum in infancy: A retrospective regional study. J. Pediatr. Urol. 2021, 18, 226–231. [Google Scholar] [CrossRef]
- Bonfiglio, R.; Cassaro, F.; Cambiaso, C.; D’Antoni, S.; Montalto, A.S.; Arena, S.; Romeo, C.; Impellizzeri, P. Clinical score for surgical treatment of acute scrotum in pediatric age. Atti Della Accad. Peloritana Dei Pericolanti-Cl. Di Sci. Med.-Biol. 2023, 111, 1–8. [Google Scholar] [CrossRef]
- Chan, E.; Wang, P.; Myslik, F.; Chen, H.; Dave, S. Identifying systems delays in assessment, diagnosis, and operative management for testicular torsion in a single-payer health-care system. J. Pediatr. Urol. 2019, 15, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lim, X.; Angus, M.I.; Panchalingam, V.; Chng, K.I.; Choo, C.S.; Chen, Y.; Laksmi, N.K. Revisiting testicular torsion scores in an Asian healthcare system. J. Pediatr. Urol. 2020, 16, 821.e1–821.e7. [Google Scholar] [CrossRef] [PubMed]
- Frohlich, L.C.; Paydar-Darian, N.; Cilento, B.G.; Lee, L.K.; Zonfrillo, M.R. Prospective validation of clinical score for males presenting with an acute scrotum. Acad. Emerg. Med. 2017, 24, 1474–1482. [Google Scholar] [CrossRef] [PubMed]
- Pinar, U.; Duquesne, I.; Lannes, F.; Bardet, F.; Kaulanjan, K.; Michiels, C.; de Mazancourt, E.S.; Dominique, I.; Vallee, M.; Felber, M.; et al. The use of doppler ultrasound for suspected testicular torsion: Lessons learned from a 15-year multicentre retrospective study of 2922 patients. Eur. Urol. Focus. 2022, 8, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Wright, H.G.; Wright, H.J. Ultrasound use in suspected testicular torsion: An association with delay to theatre and increased intraoperative finding of non-viable testicle. N. Z. Med. J. 2021, 134, 50–55. [Google Scholar] [PubMed]
- Aquila, I.; Abenavoli, L.; Sacco, M.A.; Ricci, P. The limits of diagnosis of testicular torsion in the child: Medicolegal implications in clinical practice. Clin. Case Rep. 2021, 9, e05180. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Delozier, S.; Lauderdale, C.; Zhao, S.; Clayton, D.; Pope, J.; Tanaka, S.; Adams, M.; Shannon, C.; Brock, J.; et al. Do repeat ultrasounds affect orchiectomy rate in patients with testicular torsion treated at a pediatric institution? J. Pediatr. Urol. 2019, 15, 179.e1–179.e5. [Google Scholar] [CrossRef] [PubMed]
| Clinical Sign | Patients (n) | Percentage (%) |
|---|---|---|
| Scrotal swelling | 95/103 | 92.2 |
| Tenderness on palpation | 100/107 | 93.5 |
| Firm testis | 43/65 | 66.2 |
| Scrotal hyperemia | 65/77 | 84.4 |
| Absence of the cremasteric reflex | 25/38 | 65.8 |
| High riding testis | 13/41 | 31.7 |
| Spermatic Cord Torsion | ||
|---|---|---|
| Percentage | p-Value | |
| Absence of the cremasteric reflex | 65.8% | <0.0001 |
| High riding testis | 31.7% | <0.0001 |
| Time of pain onset > 8 H | 60.4% | 0.200 |
| Scrotal swelling | 92.2% | 0.890 |
| Testicular tenderness | 93.5% | 0.549 |
| Firm testis | 66.2% | 0.105 |
| Scrotal hyperemia | 84.4% | 0.267 |
| Surgical Treatment | ||
|---|---|---|
| Percentage | p-Value | |
| Absence of the cremasteric reflex | 84.6% | <0.01 |
| High riding testis | 58.8% | <0.01 |
| Time of pain onset > 8 H | 50.9% | 0.026 |
| Scrotal swelling | 93% | 0.752 |
| Testicular tenderness | 93.2% | 0.912 |
| Firm testis | 73.7% | 0.128 |
| Scrotal hyperemia | 78.4% | 0.160 |
| Ultrasound Finding | Spermatic Cord Torsion |
|---|---|
| Increased testicular volume | p = 0.037 |
| Testicular heterogeneity | p < 0.001 |
| Absence of vascular signals | p < 0.001 |
| Whirlpool sign | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cassaro, F.; Arena, S.; Bonfiglio, R.; Alibrandi, A.; D’Antoni, S.; Romeo, C.; Impellizzeri, P. Utility of Clinical Signs in the Diagnosis of Testicular Torsion in Pediatric Age: Optimization of Timing in a Time-Sensitive Pathology. Children 2025, 12, 1220. https://doi.org/10.3390/children12091220
Cassaro F, Arena S, Bonfiglio R, Alibrandi A, D’Antoni S, Romeo C, Impellizzeri P. Utility of Clinical Signs in the Diagnosis of Testicular Torsion in Pediatric Age: Optimization of Timing in a Time-Sensitive Pathology. Children. 2025; 12(9):1220. https://doi.org/10.3390/children12091220
Chicago/Turabian StyleCassaro, Fabiola, Salvatore Arena, Roberta Bonfiglio, Angela Alibrandi, Santi D’Antoni, Carmelo Romeo, and Pietro Impellizzeri. 2025. "Utility of Clinical Signs in the Diagnosis of Testicular Torsion in Pediatric Age: Optimization of Timing in a Time-Sensitive Pathology" Children 12, no. 9: 1220. https://doi.org/10.3390/children12091220
APA StyleCassaro, F., Arena, S., Bonfiglio, R., Alibrandi, A., D’Antoni, S., Romeo, C., & Impellizzeri, P. (2025). Utility of Clinical Signs in the Diagnosis of Testicular Torsion in Pediatric Age: Optimization of Timing in a Time-Sensitive Pathology. Children, 12(9), 1220. https://doi.org/10.3390/children12091220








