Evaluation of Oral Health and Oral Health-Related Quality of Life in Children with Adenoid Hypertrophy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Sample Size and Criteria
2.3. Data Collection
2.3.1. ECOHIS-T
2.3.2. DMFT Index
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mnatsakanian, A.; Heil, J.R.; Sharma, S. Anatomy, head and neck: Adenoids. In StatPearls [Internet]; StatPearls Publishing: Saint Petersburg, FL, USA, 2023. [Google Scholar]
- Niedzielski, A.; Chmielik, L.P.; Mielnik-Niedzielska, G.; Kasprzyk, A.; Bogusławska, J. Adenoid hypertrophy in children: A narrative review of pathogenesis and clinical relevance. BMJ Paediatr. Open 2023, 7, e001710. [Google Scholar] [CrossRef]
- Kara, A.; Elden, H.; Okur, E.; Yilmaz, M.S.; Mutlu, F.; Guven, M.; Demir, D. Impact of tonsillectomy on COVID–19 pandemic: An observational study of the incidence and prognosis. Acta Oto-Laryngol. 2021, 141, 857–859. [Google Scholar] [CrossRef]
- Regauer, S. Nasopharynx and Waldeyer’s ring. In Pathology of the Head and Neck; Springer: Berlin/Heidelberg, Germany, 2006; pp. 171–196. [Google Scholar]
- Shen, Y.; Li, X.; Liang, X.; Xu, H.; Li, C.; Yu, Y.; Qiu, B. A deep-learning-based approach for adenoid hypertrophy diagnosis. Med. Phys. 2020, 47, 2171–2181. [Google Scholar] [CrossRef]
- Baroni, M.; Ballanti, F.; Franchi, L.; Cozza, P. Craniofacial features of subjects with adenoid, tonsillar, or adenotonsillar hypertrophy. Prog. Orthod. 2011, 12, 38–44. [Google Scholar] [CrossRef]
- İnönü-Sakallı, N.; Sakallı, C.; Tosun, Ö.; Akşit-Bıçak, D. Comparative evaluation of the effects of adenotonsillar hypertrophy on oral health in children. BioMed Res. Int. 2021, 2021, 5550267. [Google Scholar] [CrossRef]
- Jácomo, A.; Akamatsu, F.; Andrade, M.; NF, M. Pharyngeal lymphatic ring: Anatomical review. J. Morphol. Sci. 2017, 27, 47–49. [Google Scholar]
- Pereira, L.; Monyror, J.; Almeida, F.T.; Almeida, F.R.; Guerra, E.; Flores-Mir, C.; Pachêco-Pereira, C. Prevalence of adenoid hypertrophy: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 38, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Qiao, X.; Qi, S.; Zhang, X.; Li, S. Effect of adenoid hypertrophy on the upper airway and craniomaxillofacial region. Transl. Pediatr. 2021, 10, 2563. [Google Scholar] [CrossRef] [PubMed]
- Evcimik, M.F.; Dogru, M.; Cirik, A.A.; Nepesov, M.I. Adenoid hypertrophy in children with allergic disease and influential factors. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 694–697. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Dhong, H.-J.; Lee, J.-K.; Chung, S.-K.; Jung, S.-C. Sleep quality and effects of position on sleep apnea in East Asian children. Auris Nasus Larynx 2011, 38, 228–232. [Google Scholar] [CrossRef]
- Chervin, R.D.; Archbold, K.H.; Dillon, J.E.; Panahi, P.; Pituch, K.J.; Dahl, R.E.; Guilleminault, C. Inattention, hyperactivity, and symptoms of sleep-disordered breathing. Pediatrics 2002, 109, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Türkoğlu, S.; Tahsin Somuk, B.; Sapmaz, E.; Bilgiç, A. Effect of adenotonsillectomy on sleep problems, attention deficit hyperactivity disorder symptoms, and quality of life of children with adenotonsillar hypertrophy and sleep-disordered breathing. Int. J. Psychiatry Med. 2019, 54, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Erdamar, B.; Suoglu, Y.; Cuhadaroglu, C.; Katircioglu, S.; Guven, M. Evaluation of clinical parameters in patients with obstructive sleep apnea and possible correlation with the severity of the disease. Eur. Arch. Oto-Rhino-Laryngol. 2001, 258, 492–495. [Google Scholar]
- Yıldırım, A.; Tekeşin, A.K. Obstrüktif Uyku Apne Sendromu Olan Hastalarda Klinik ve Demografik Verilerinin Değerlendirilmesi. Sak. Tıp Derg. 2021, 11, 103–108. [Google Scholar]
- De Serres, L.M.; Derkay, C.; Sie, K.; Biavati, M.; Jones, J.; Tunkel, D.; Manning, S.; Inglis, A.F.; Haddad Jr, J.; Tampakopoulou, D. Impact of adenotonsillectomy on quality of life in children with obstructive sleep disorders. Arch. Otolaryngol.–Head Neck Surg. 2002, 128, 489–496. [Google Scholar] [CrossRef]
- Carneiro, L.E.P.; Neto, G.C.R.; Camera, M.G. Adenotonsillectomy effect on the life quality of children with adenotonsillar hyperplasia. Intl. Arch. Otorhinolaryngol. 2009, 13, 270–276. [Google Scholar]
- Kim, D.-K.; Rhee, C.S.; Yun, P.-Y.; Kim, J.-W. Adenotonsillar hypertrophy as a risk factor of dentofacial abnormality in Korean children. Eur. Arch. Oto-Rhino-Laryngol. 2015, 272, 3311–3316. [Google Scholar] [CrossRef]
- Poddębniak, J.; Zielnik-Jurkiewicz, B. Impact of adenoid hypertrophy on the open bite in childrena. Pol. J. Otolaryngol. 2019, 73, 8–13. [Google Scholar]
- Lin, L.; Zhao, T.; Qin, D.; Hua, F.; He, H. The impact of mouth breathing on dentofacial development: A concise review. Front. Public Health 2022, 10, 929165. [Google Scholar] [CrossRef]
- Galeotti, A.; Festa, P.; Viarani, V.; D’Antò, V.; Sitzia, E.; Piga, S.; Pavone, M. Prevalence of malocclusion in children with obstructive sleep apnoea. Orthod. Craniofacial Res. 2018, 21, 242–247. [Google Scholar] [CrossRef] [PubMed]
- El Aouame, A.; Daoui, A.; El Quars, F. Nasal breathing and the vertical dimension: A cephalometric study. Int. Orthod. 2016, 14, 491–502. [Google Scholar] [CrossRef]
- Souki, B.Q.; Lopes, P.B.; Veloso, N.C.; Avelino, R.A.; Pereira, T.B.; Souza, P.E.; Franco, L.P.; Becker, H.M. Facial soft tissues of mouth-breathing children: Do expectations meet reality? Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 1074–1079. [Google Scholar] [CrossRef]
- Nogami, Y.; Saitoh, I.; Inada, E.; Murakami, D.; Iwase, Y.; Kubota, N.; Nakamura, Y.; Kimi, M.; Hayasaki, H.; Yamasaki, Y. Prevalence of an incompetent lip seal during growth periods throughout Japan: A large-scale, survey-based, cross-sectional study. Environ. Health Prev. Med. 2021, 26, 11. [Google Scholar] [CrossRef]
- Ballikaya, E.; Dogan, B.G.; Onay, O.; Tekcicek, M.U. Oral health status of children with mouth breathing due to adenotonsillar hypertrophy. Int. J. Pediatr. Otorhinolaryngol. 2018, 113, 11–15. [Google Scholar] [CrossRef]
- Kaskova, L.; Ulasevych, L. Oral hygienic state and pH value in children with adenoid hypertrophy. Ukr. Dent. Alm. 2016, 2, 64–66. [Google Scholar]
- Cantekin, K.; Yildirim, M.D.; Cantekin, I. Assessing change in quality of life and dental anxiety in young children following dental rehabilitation under general anesthesia. Pediatr. Dent. 2014, 36, 12E–17E. [Google Scholar] [PubMed]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Sengul, F.; Kilic, M.; Gurbuz, T.; Tasdemir, S. Carbonic anhydrase VI gene polymorphism rs2274327 relationship between salivary parameters and dental-oral health status in children. Biochem. Genet. 2016, 54, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Jazi, S.M.H.; Barati, B.; Kheradmand, A. Treatment of adenotonsillar hypertrophy: A prospective randomized trial comparing azithromycin vs. fluticasone. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2011, 16, 1590. [Google Scholar]
- Abreu, R.R.; Rocha, R.L.; Lamounier, J.A.; Guerra, Â.F.M. Etiology, clinical manifestations and concurrent findings in mouth-breathing children. J. Pediatr. 2008, 84, 529–535. [Google Scholar] [CrossRef]
- Eliasson, L.; Carlén, A.; Almståhl, A.; Wikström, M.; Lingström, P. Dental plaque pH and micro-organisms during hyposalivation. J. Dent. Res. 2006, 85, 334–338. [Google Scholar] [CrossRef]
- Motta, L.J.; Bachiega, J.C.; Guedes, C.C.; Laranja, L.T.; Bussadori, S.K. Association between halitosis and mouth breathing in children. Clinics 2011, 66, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, Ö. Allergic rhinitis and dental caries. Allergol. Immunopathol. 2023, 51, 19–20. [Google Scholar] [CrossRef] [PubMed]
- Manuelli, M.; Marcolina, M.; Nardi, N.; Bertossi, D.; De Santis, D.; Ricciardi, G.; Luciano, U.; Nocini, R.; Mainardi, A.; Lissoni, A. Oral mucosal complications in orthodontic treatment. Minerva Stomatol. 2019, 68, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Farahzadi, Z.; Khodadadi, E.; Abesi, F.; Gholinia, H. Assessment of the relationship between oral health and adenoid hypertrophy in children aged 8 to 15 years. J. Oral Health Oral Epidemiol. 2024, 13, 6–12. [Google Scholar] [CrossRef]
- Ma, Y.; Xie, L.; Wu, W. The effects of adenoid hypertrophy and oral breathing on maxillofacial development: A review of the literature. J. Clin. Pediatr. Dent. 2024, 48, 1–6. [Google Scholar] [CrossRef]
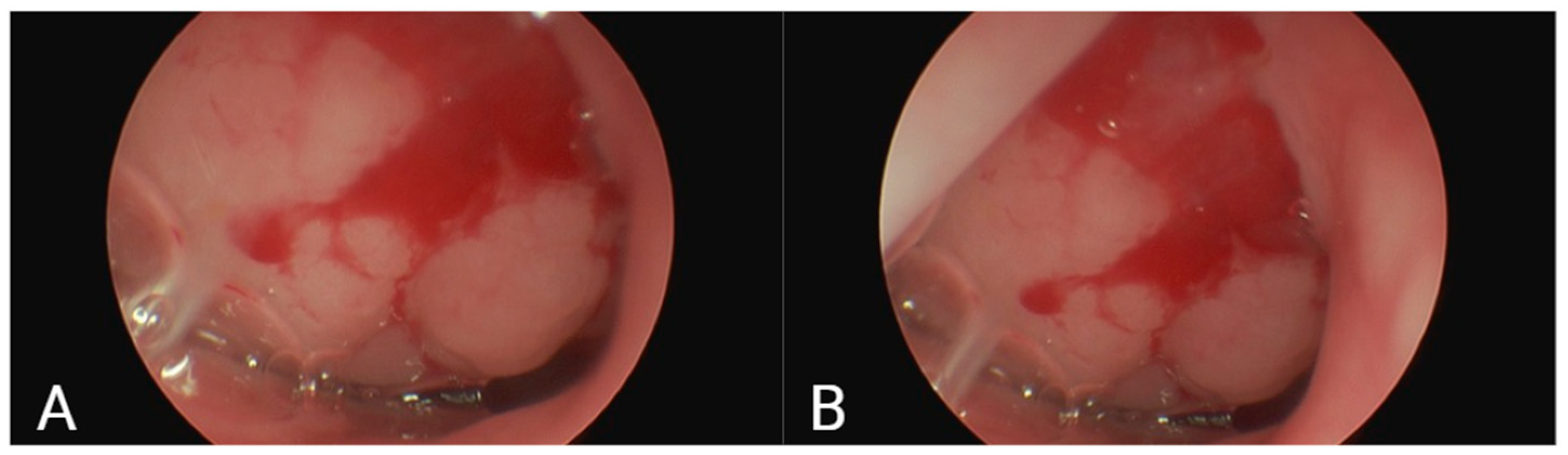
- Zwierz, A.; Domagalski, K.; Masna, K.; Burduk, P. Effectiveness of evaluation of adenoid hypertrophy in children by flexible nasopharyngoscopy examination (FNE), proposed schema of frequency of examination: Cohort study. Diagnostics 2022, 12, 1734. [Google Scholar] [CrossRef]
- Nugroho, P.S.; Falerina, R.; Rakhma, H.K.; Nurfaizi, A. Correlation of Clinical Score, Radiological Examination, and Nasopharyngeal Endoscopy in Adenoid Hypertrophy Patients as a Consideration of Adenoidectomy. Korean J. Otorhinolaryngol.-Head Neck Surg. 2023, 66, 315–321. [Google Scholar] [CrossRef]
- Agarwal, L.; Tandon, R.; Kulshrestha, R.; Gupta, A. Adenoid facies and its management: An orthodontic perspective. Indıan J. Orthod. Dentofac. Res. 2016, 2, 50–55. [Google Scholar]
| Response Options: 0 = Never; 1 = Almost Never; 2 = Occasionally; 3 = Frequently; 4 = Very Frequently; 5 = I Don’t Know |
|---|
| Child Impact Section |
| 1. Has your child ever had pain in the teeth, mouth, or jaws (bones of the mouth)? |
| 2. Has your child ever had difficulty drinking hot or cold drinks due to problems with teeth or dental treatments? |
| 3. Has your child ever had trouble eating certain foods due to problems with teeth or dental treatments? |
| 4. Has your child ever had difficulty pronouncing any words due to problems with teeth or dental treatments? |
| 5. Has your child ever missed daycare, kindergarten, or school due to problems with teeth or dental treatments? |
| 6. Has your child ever had trouble sleeping due to problems with teeth or dental treatments? |
| 7. Has your child ever been irritated by problems with teeth or dental treatments? |
| 8. Has your child ever avoided smiling or laughing due to problems with teeth or dental treatments? |
| 9. Has your child ever avoided talking due to problems with teeth or dental treatments? |
| Family Impact Section |
| 10. Have you or someone else in the family ever been upset because of problems with your child’s teeth or dental treatments? |
| 11. Have you or someone else in the family ever felt guilty because of problems with your child’s teeth or dental treatments? |
| 12. Have you or someone else in the family missed work due to problems with your child’s teeth or dental treatments? |
| 13. Has your child ever had problems with his teeth or had dental treatments that have had a financial impact on your family? |
| Gender (Girls–Boys) | Age (Avg. ± SS) | DMFT (Avg. ± SS) | N, DP% D-K-S | N, DO% Class 1 | |
|---|---|---|---|---|---|
| Control Group | 30 (14–16) | 7.35 ± 4.85 | 3.86 ± 5.21 | 6-9-0 40%, 60%, 0 | 8, 53%, 3 |
| Adenoid Hypertrophy Grade (2,3,4) | 30 (12–18) | 8.71 ± 3.50 | 8.39 ± 4.58 | 5-7-3 33.3%, 46.6%, 20% | 5, 33%, 3 |
| Total | 60 (26–34) | 7.53 ± 2.641 | 6.27 ± 5.21 | 11-16-3 36.6%, 53.3%, 10% | 13, 43%, 3 |
| p | 0.177 | 0.08 | 0.010 * | 0.25 | 0.49 |
| Group | (Avg. ± SS) | p Value | |
|---|---|---|---|
| Child Impact Domain | |||
| Symptoms in Children | AHG | 0.97 ± 1.32 | 0.948 |
| CG | 1.08 ± 1.24 | ||
| Total | 1.03 ± 1.42 | ||
| Child Functional Status | AHG | 2.07 ± 3.23 | 0.789 |
| CG | 2.46 ± 3.64 | ||
| Total | 2.42 ± 3.55 | ||
| Child Psychology | AHG | 0.52 ± 1.27 | 0.807 |
| CG | 0.65 ± 1.57 | ||
| Total | 0.57 ± 1.45 | ||
| Child’s Self-Perception and Social Interaction | AHG | 1.93 ± 1.78 | 0.048 * |
| CG | 0.98 ± 1.47 | ||
| Total | 1.43 ± 1.67 | ||
| Total Child Score | AHG | 5.37 ± 6.72 5.0 ± 6.87 | 0.520 |
| CG | |||
| Total | |||
| Family Impact Section | |||
| Parental Distress | AHG | 0.68 ± 1.54 | 0.348 |
| CG | 1.24 ± 2.12 | ||
| Total | 1.00 ± 1.82 | ||
| Family Function | AHG | 0.50 ± 0.92 | 0.134 |
| CG | 0.76 ± 1.52 | ||
| Total | 0.55 ± 1.62 | ||
| Total Parent Score | AHG | 0.89 ± 2.23 | 0.560 |
| CG | 1.93 ± 3.49 | ||
| Total | 1.53 ± 3.09 | ||
| Total ECOHIS Score | AHG | 6.57 ± 8.62 | 0.690 |
| CG | 6.81 ± 9.94 | ||
| Total | 6.59 ± 9.63 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kılıç, M.Ç.; Cantekin, K.; Haylaz, E.; Kalabalık, F.; Kılıç, K.; Bircan, H.B.; Güner, M. Evaluation of Oral Health and Oral Health-Related Quality of Life in Children with Adenoid Hypertrophy. Children 2025, 12, 1206. https://doi.org/10.3390/children12091206
Kılıç MÇ, Cantekin K, Haylaz E, Kalabalık F, Kılıç K, Bircan HB, Güner M. Evaluation of Oral Health and Oral Health-Related Quality of Life in Children with Adenoid Hypertrophy. Children. 2025; 12(9):1206. https://doi.org/10.3390/children12091206
Chicago/Turabian StyleKılıç, Münevver Çoruh, Kenan Cantekin, Emre Haylaz, Fahrettin Kalabalık, Korhan Kılıç, Hasan Basri Bircan, and Mihriban Güner. 2025. "Evaluation of Oral Health and Oral Health-Related Quality of Life in Children with Adenoid Hypertrophy" Children 12, no. 9: 1206. https://doi.org/10.3390/children12091206
APA StyleKılıç, M. Ç., Cantekin, K., Haylaz, E., Kalabalık, F., Kılıç, K., Bircan, H. B., & Güner, M. (2025). Evaluation of Oral Health and Oral Health-Related Quality of Life in Children with Adenoid Hypertrophy. Children, 12(9), 1206. https://doi.org/10.3390/children12091206







