Motor Development Scales Validated in Spanish Populations of Children Aged 0–18 Months: Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
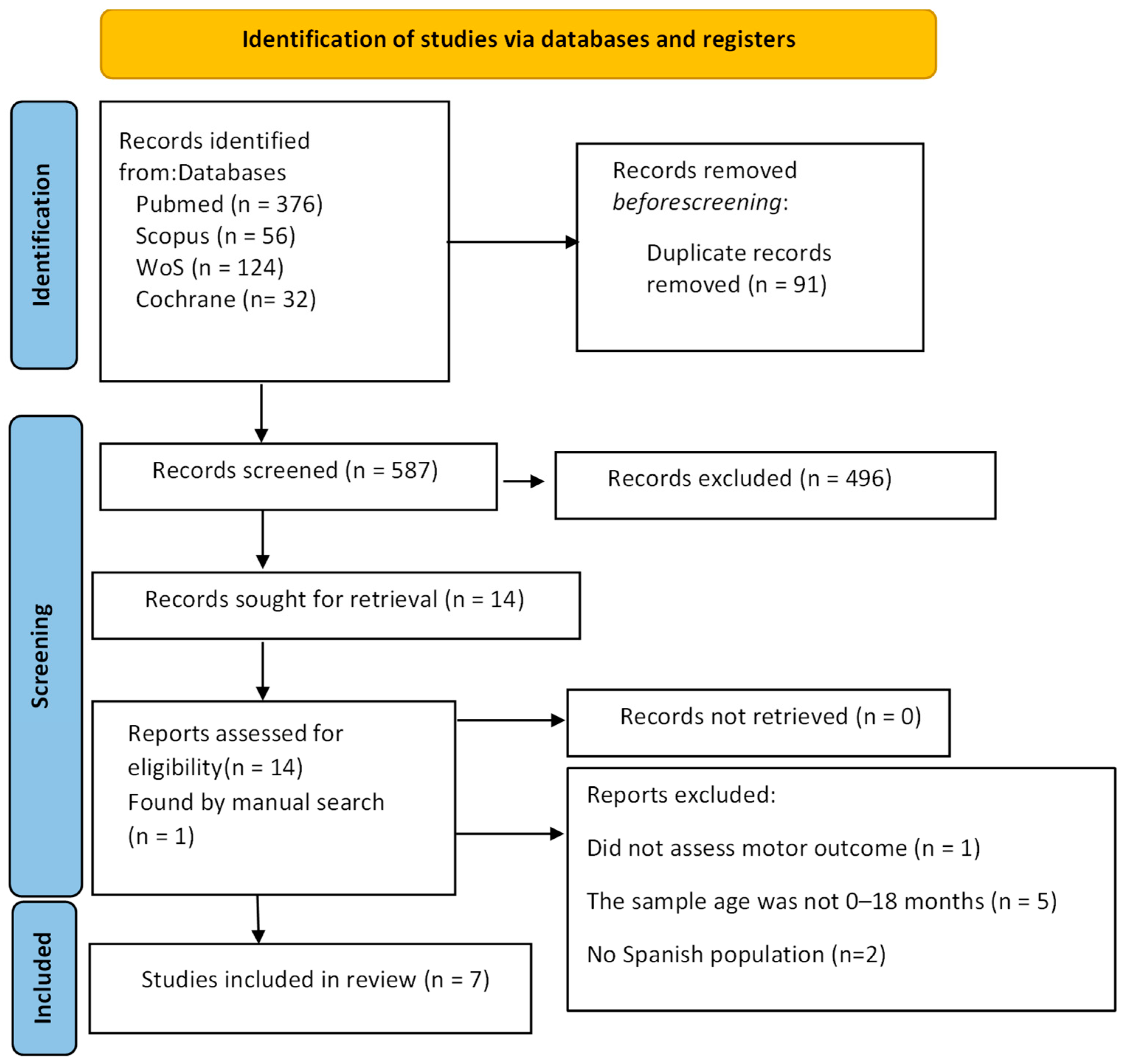
2.3. Selection Process
2.4. Data Synthesis
2.5. Article Quality Evaluation
3. Results
3.1. Characteristics of the Included Studies
3.2. Study Quality Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Wang, X.; Zhou, B. Motor development-focused exercise training enhances gross motor skills more effectively than ordinary physical activity in healthy preschool children: An updated meta-analysis. Front. Public Health 2024, 12, 1414152. [Google Scholar] [CrossRef]
- Hadders-Algra, M. The developing brain: Challenges and opportunities to promote school readiness in young children at risk of neurodevelopmental disorders in low- and middle-income countries. Front. Pediatr. 2022, 10, 989518. [Google Scholar] [CrossRef]
- Wu, Y.; Heineman, K.R.; Gemert, S.L.B.; Kuiper, D.; Olivares, M.D.; Hadders-Algra, M. Motor behaviour in infancy is associated with neurological, cognitive, and behavioural function of children born to parents with reduced fertility. Dev. Med. Child Neurol. 2020, 62, 1089–1095. [Google Scholar] [CrossRef]
- Elhakeem, A.; Hardy, R.; Bann, D.; Kuh, D.; Cooper, R. Motor performance in early life and participation in leisure-time physical activity up to age 68 years. Paediatr. Périnat. Epidemiol. 2018, 32, 327–334. [Google Scholar] [CrossRef]
- Uller, T.; Milocco, L.; Isanta-Navarro, J.; Cornwallis, C.K.; Feiner, N.; Wright, P.A.; Gilmour, K.M. Twenty years on from Developmental Plasticity and Evolution: Middle-range theories and how to test them. J. Exp. Biol. 2024, 227, jeb246375. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.H. Developmental theories: Past, present, and future. Dev. Rev. 2022, 66, 101049. [Google Scholar] [CrossRef]
- Raichle, M.E. The restless brain: How intrinsic activity organizes brain function. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140172. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Robles, Á.; Merino-Andrés, J.; Rodríguez-Fernández, Á.L.; Gutiérrez-Ortega, M.; León-Estrada, I.; Ródenas-Martínez, M. Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination. Healthcare 2024, 12, 380. [Google Scholar] [CrossRef]
- Burton, V.J.; Kannan, S.; Jayakumar, S.; Gerner, G.; West, S.; Yenokyan, G.; Duncan, A.F. Longitudinal Hammersmith Infant Neurological Examination (HINE) Trajectories in Children with Cerebral Palsy Identified in High-Risk Follow-Up. J. Clin. Med. 2025, 14, 1572. [Google Scholar] [CrossRef]
- Fujihira, R.; Taga, G. Dynamical systems model of development of the action differentiation in early infancy: A requisite of physical agency. Biol. Cybern. 2023, 117, 81–93. [Google Scholar] [CrossRef]
- Hadders-Algra, M. Early human motor development: From variation to the ability to vary and adapt. Neurosci. Biobehav. Rev. 2018, 90, 411–427. [Google Scholar] [CrossRef]
- Sangkarit, N.; Tapanya, W. Factors influencing on gross motor skills in infants: Implications for walking development. Early Hum. Dev. 2024, 195, 106076. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Huang, M.; Yuan, X.; Zhong, X.; Dai, S.; Wang, Y.; Zhang, Q.; Wongwitwichote, K.; Jiang, C. Lifespan trajectories of motor control and neural oscillations: A systematic review of magnetoencephalography insights. Dev. Cogn. Neurosci. 2025, 72, 101529. [Google Scholar] [CrossRef] [PubMed]
- Gooijers, J.; Pauwels, L.; Hehl, M.; Seer, C.; Cuypers, K.; Swinnen, S.P. Aging, brain plasticity, and motor learning. Ageing Res. Rev. 2024, 102, 102569. [Google Scholar] [CrossRef] [PubMed]
- Hadders-Algra, M. Early Diagnostics and early intervention in neurodevelopmental disorders—Age-dependent challenges and opportunities. J. Clin. Med. 2021, 10, 861. [Google Scholar] [CrossRef]
- Merlo, L.M.; Mata, J.F. Fisioterapia en Pediatría, 2nd ed.; Panamericana: Madrid, Spain, 2018. [Google Scholar]
- Moriyama, C.H.; Massetti, T.; Crocetta, T.B.; Da Silva, T.D.; Mustacchi, Z.; Guarnieri, R.; De Abreu, L.C.; De Araújo, A.V.L.; Menezes, L.D.C.D.; Monteiro, C.B.D.M.; et al. Systematic Review of the Main Motor Scales for Clinical Assessment of Individuals with down Syndrome. Dev. Neurorehabilit. 2019, 23, 39–49. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Mourad, O.; Hossam, H.; Zbys, F.; Ahmed, E. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Mokkink, L.B.; de Vet, H.C.W.; Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; Terwee, C.B. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018, 27, 1171–1179. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. QUADAS-2: A Revised Tool for the Quality As-sessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536. Available online: https://annals.org (accessed on 15 May 2025). [CrossRef]
- Morales-Monforte, E.; Bagur-Calafat, C.; Suc-Lerin, N.; Fornaguera-Martí, M.; Cazorla-Sánchez, E.; Girabent-Farrés, M. The Spanish version of the Alberta Infant Motor Scale: Validity and reliability analysis. Dev. Neurorehabilit. 2015, 20, 76–82. [Google Scholar] [CrossRef]
- Álvarez-Gonzalo, V.; Pandiella-Dominique, A.; Kürlander-Arigón, G.; Simó-Segovia, R.; Caballero, F.F.; Miret, M. Validation of the PDMS-2 scale in the Spanish population. Evaluation of physiotherapy intervention and parental involvement in the treatment of children with neurodevelopmental disorders. Rev. Neurol. 2021, 73, 81–88. [Google Scholar]
- Ferre-Fernández, M.P.; Murcia-González, M.A.; Ríos-Díaz, J.P. Intra- and Interrater Reliability of the Spanish Version of the Gross Motor Function Measure (GMFM-SP-88). Pediatr. Phys. Ther. 2022, 34, 193–200. [Google Scholar] [CrossRef]
- Fernández, M.F.; González, M.A.M.; Díaz, J.R. Traducción y Adaptación Transcultural del Gross Motor Function Measure a la Población Española de Niños con Parálisis Cerebral. Rev. Neurol. 2020, 71, 177–185. Available online: https://www.imrpress.com/journal/RN/71/5/10.33588/rn.7105.2020087 (accessed on 9 August 2025). [CrossRef] [PubMed]
- Costas Moragas, C.; Fornieles Deu, A.; Botet Mussons, F.; Boatella Costa, E.; Cáceres Zurita, M.L. Evaluación psicométrica de la Escala de Brazelton en una muestra de recién nacidos españoles. Psicothema 2007, 19, 140–149. [Google Scholar] [PubMed]
- Fernández, D.; Alvarez, M.J.; Rodríguez, D.; Rodríguez, M.; Fernández, E.; Urdiales, P. Spanish Validation of the Premie-Neuro Scale in Premature Infants. J. Pediatr. Nurs. 2015, 30, 560–567. [Google Scholar] [CrossRef] [PubMed]
- De Medicina, F.; Ulloa, M.E.; Ma, D.; Arroyo, O.; Antonio, R.; Badillo, Á. Adaptación Transcultural y Versión Española de la Prueba de Rendimiento Motor Infantil (TIMP). Ph.D. Thesis, Universidad Complutense de Madrid, Madrid, Spain, 2017. [Google Scholar]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.-C.; et al. Early, accurate diagnosis and early inter-vention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Heineman, K.R.; Hadders-Algra, M. Evaluation of Neuromotor Function in Infancy–A Systematic Review of Available Methods. J. Dev. Behav. Pediatr. 2008, 29, 315–323. [Google Scholar] [CrossRef]
- Hadders-Algra, M.; Tacke, U.; Pietz, J.; Rupp, A.; Philippi, H. Predictive value of the General Movements Assessment and Standardized Infant NeuroDevelopmental Assessment in infants at high risk of neurodevelopmental disorders. Dev. Med. Child Neurol. 2024, 66, 1361–1368. [Google Scholar] [CrossRef]
- Rosalind Sacrey, L.A.; Karl, J.; Reid, K.; Raza, S.; Eliks, M.; Gajewska, E.; Eliks, M.; Gajewska, E. The Alberta Infant Motor Scale: A tool for the assessment of motor aspects of neurodevelopment in infancy and early childhood. Front. Neurol. 2022, 13, 927502. [Google Scholar] [CrossRef]
- Valentini, N.C.; Zanella, L.W. Peabody Developmental Motor Scales-2: The Use of Rasch Analysis to Examine the Model Unidi-mensionality, Motor Function, and Item Difficulty. Front Pediatr. 2022, 10, 852732. [Google Scholar] [CrossRef]
- Gagnon, K.; Cannon, S.; Weatherstone, K.B. Predictive Validity of the Premie-Neuro at 3 Months’ Adjusted Age and 2 Years’ Chronological Age. Adv. Neonatal Care 2016, 16, 151–157. [Google Scholar] [CrossRef]
- Campbell, S.K. Functional movement assessment with the Test of Infant Motor Performance. J. Perinatol. 2021, 41, 2385–2394. [Google Scholar] [CrossRef]
- Griffiths, A.; Toovey, R.; Morgan, P.E.; Spittle, A.J. Psychometric properties of gross motor assessment tools for children: A systematic review. BMJ Open 2018, 8, e021734. [Google Scholar] [CrossRef]
| Scale, Author, Year | Country of Origin | Scale Description (Definition and Number Items) | Population | Age Range | Administration Time | Instructions of Use | Outcome Measure | Psychometric Properties | Proportion of Children Aged 0–18 Months Included in the Study Population |
|---|---|---|---|---|---|---|---|---|---|
| AIMS, Martha C. Piper and Johanna Darra, 1994 [22] | Canada | Observational scale (spontaneous motor skills). 58 items (21 PP, 9 SP, 12 Si, 16 St). | Children with TD, risk, motor delay. | 0–18 months | 10–30 min | Direct observation. Mark the motor window of the child and write down the observed items, giving a score of 1 point. | Percentile. | IC (α TS-0.99, P-0.97, Sp-0.88, St-0.97, S-0.96) Intra-R (ICCs 0.94–1.00 CI 95%) Inter-R (ICCs 0.95–1.00 CI 95%) CoV (0.973) | 100% |
| HINE, Lilly Dubowitz, 1981 [8] | UK | Neurological evaluation. 37 items (26 neurological evaluation, 8 MD and 3 behaviour). | Preterm and full-term | 2–24 months CA | 5–15 min | Direct observation. 0–3 pts each item. Write down asymmetries. | TS, optimal or non-optimal, and motor prognosis. | Intra-R (ICCs 0.98 CI 95%) Inter-R (ICCs 0.98 CI 95%) | 94.4% |
| PDMS-2, M. Rhonda Folio and Rebecca R. Fewell, 2000 [23] | USA | Observational evaluation (gross and fine MD). 249 items (8 MR, 30 postural control, 89 locomotion, 24 object handling, 26 grip and 72 VC). | Children with MD delay | 0–5 years | 45–60 min | Direct observation. It is initiated at any age between 0 and 5 years. 0–2 pts. It is terminated when three consecutive zeros are obtained. | SS, percentile and DQ. Risk of motor delay. | Inter-R (ICCs 0.758–0.999 CI 95%) IC (α 0.991–0.999) | 100% |
| GMFM-88. Dianne J. Russell, Peter L. Rosenbaum, Marilyn Wright, and Lisa M. Avery, 1989 [24,25] | UK | Observational scale. 88 items (17 lying down and turning over, 20 St, 14 crawling and kneeling, 13 S, 24 walking, running and jumping). | Children with CP | 5 months- 16 years | 45–60 min | Direct observation. 0–3 pts. Write down the use of walking devices. | Total percentage of MD and each dimension. | Inter-R (ICCs 0.99–1.00, CI 95%) Intra-R (ICCs 0.99–1.00, CI 95%) | 77.8% |
| NBAS, T. Berry Brazelton, 1973 [26] | USA | Neonatal behaviour scale. 53 items (18 autonomous behaviour, 18 MD, 7 self-regulation, 10 social behaviour). | TD or preterm babies | 0–2 months | 30–45 min | Direct observation in Sp or semi-seated. 0–9 pts. | TS (profile) expected behaviour or risk. | IC (α 0.65) | 16.7% |
| Premie-Neuro, Diane K. Daily and Patricia H. Ellison, 2005 [27] | USA | Neuromotor assessment. 24 items (8 neurological, 8 movement and 8 response capacity). | Preterm children (23–37 GW) | 0–6 months CA | 4–8 min | Direct observation (monitoring device). Hands in the incubator, movements/handling are triggered. | TS: neurologically normal, doubtful, lower than normal. | IC (α 0.72) Inter-R (ICCs 0.524–0.901 CI 95%) | 38.9% |
| TIMP, Suzann K. Campbell, Gay L. Girolami y Thubi HA Kolobe, Elizabeth T. Osten and Maureen C. Lenke, 1900 [28] | USA | Early MD scale. 42 items (13 MB, 29 MR). | Premature and full-term babies | 34 GW–4 months CA | 20–30 min | Direct observation and triggered responses. 0–6 pts (MB) and 0–3 pts (MR). | TS: risk of neuromotor alteration. | IC (α > 0.95) Intra-R (ICCs 0.994 CI 95%). | 27.8% |
| Scales | Gross Motor Development | Reflexes | Postural Control | Balance | Coordination | Locomotion | Object Handling | Grip | Muscle tone | Body Alignment: Asymmetries | Social Behaviour and Reactions to Stimuli | Movements (Quality, Fluidity, Symmetry) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PP | SP | Si | St | W | Static | Dynamic | Body | Eye-hand | ||||||||||
| 1. AIMS [22] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||||
| 2. HINE [8] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||
| 3. PDMS-2 [23] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||
| 4. GMFM-88 [24,25] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||||
| 5. NBAS [26] | ✔ | ✔ | ✔ | ✔ | ✔quality | |||||||||||||
| 6. Premie-Neuro [27] | ✔ | ✔ | ✔ | ✔ | ✔ | ✔symmetry | ||||||||||||
| 7. TIMP [28] | ✔ | ✔ | ✔ | ✔ | ✔symmetry | |||||||||||||
| Studies | Risk of Bias | Applicability Results | ||||||
|---|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Test | Flow and Times | Patient Selection | Index Test | |||
| AIMS, Martha C. Piper and Johanna Darra, 1994 [22] | ? | ☺ | ? | ? | ☺ | ☺ | ? | |
| HINE, Lilly Dubowitz, 1981 [8] | ? | ☺ | ? | ☺ | ☺ | ☺ | ? | |
| PDMS-2, M. Rhonda Folio and Rebecca R. Fewell, 2000 [23] | ? | ☺ | ☹ | ☺ | ☺ | ☺ | ? | |
| GMFM-88. Dianne J. Russell, Peter L. Rosenbaum, Marilyn Wright, and Lisa M. Avery, 1989 [24,25] | ? | ☺ | ? | ☺ | ☹ | ☺ | ? | |
| NBAS, T. Berry Brazelton, 1973 [26] | ☺ | ☹ | ? | ☹ | ☺ | ? | ? | |
| Premie-Neuro, Diane K. Daily and Patricia H. Ellison, 2005 [27] | ? | ☺ | ? | ☺ | ☹ | ☺ | ? | |
| TIMP, Suzann K. Campbell, Gay L. Girolami y Thubi HA Kolobe, Elizabeth T. Osten and Maureen C. Lenke, 1900 [28] | ? | ☺ | ? | ? | ☺ | ☺ | ? | |
| Studies | Internal Consistency | Reliability | Content Validity | Structural Validity | Criterion Validity | Sensitivity | Transcultural Validity |
|---|---|---|---|---|---|---|---|
| AIMS, Martha C. Piper and Johanna Darra, 1994 [22] | +++ | +++ | +++ | +++ | ++ | ++ | |
| HINE, Lilly Dubowitz, 1981 [8] | ++ | ++ | +++ | +++ | ++ | +++ | |
| PDMS-2, M. Rhonda Folio and Rebecca R. Fewell, 2000 [23] | +++ | +++ | ++ | +++ | ++ | +++ | |
| GMFM-88. Dianne J. Russell, Peter L. Rosenbaum, Marilyn Wright, and Lisa M. Avery, 1989 [24,25] | ++ | +++ | +++ | ++ | ++ | ++ | +++ |
| NBAS, T. Berry Brazelton, 1973 [26] | ++ | + | +++ | ++ | + | ++ | |
| Premie-Neuro, Diane K. Daily and Patricia H. Ellison, 2005 [27] | ++ | ++ | ++ | ++ | ++ | ++ | |
| TIMP, Suzann K. Campbell, Gay L. Girolami y Thubi HA Kolobe, Elizabeth T. Osten and Maureen C. Lenke, 1900 [28] | +++ | +++ | +++ | +++ | ++ | +++ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cala de la Torre, E.; Pinero-Pinto, E. Motor Development Scales Validated in Spanish Populations of Children Aged 0–18 Months: Systematic Review. Children 2025, 12, 1106. https://doi.org/10.3390/children12091106
Cala de la Torre E, Pinero-Pinto E. Motor Development Scales Validated in Spanish Populations of Children Aged 0–18 Months: Systematic Review. Children. 2025; 12(9):1106. https://doi.org/10.3390/children12091106
Chicago/Turabian StyleCala de la Torre, Elena, and Elena Pinero-Pinto. 2025. "Motor Development Scales Validated in Spanish Populations of Children Aged 0–18 Months: Systematic Review" Children 12, no. 9: 1106. https://doi.org/10.3390/children12091106
APA StyleCala de la Torre, E., & Pinero-Pinto, E. (2025). Motor Development Scales Validated in Spanish Populations of Children Aged 0–18 Months: Systematic Review. Children, 12(9), 1106. https://doi.org/10.3390/children12091106








