Surveying the Perspectives of Parents and Professionals on Providing Upright, Hands-Free, Self-Initiated Mobility to Children with Severe Physical and Communication Disabilities
Abstract
1. Introduction
1.1. Upright, Hands-Free, Self-Initiated Mobility
1.2. Upright, Hands-Free, Self-Initiated Mobility and AAC
2. Materials and Methods
2.1. Participants
2.2. Reserch Design
2.3. Materials
2.4. Procedures
2.4.1. Survey Distribution
2.4.2. Data Collection and Analysis
3. Results
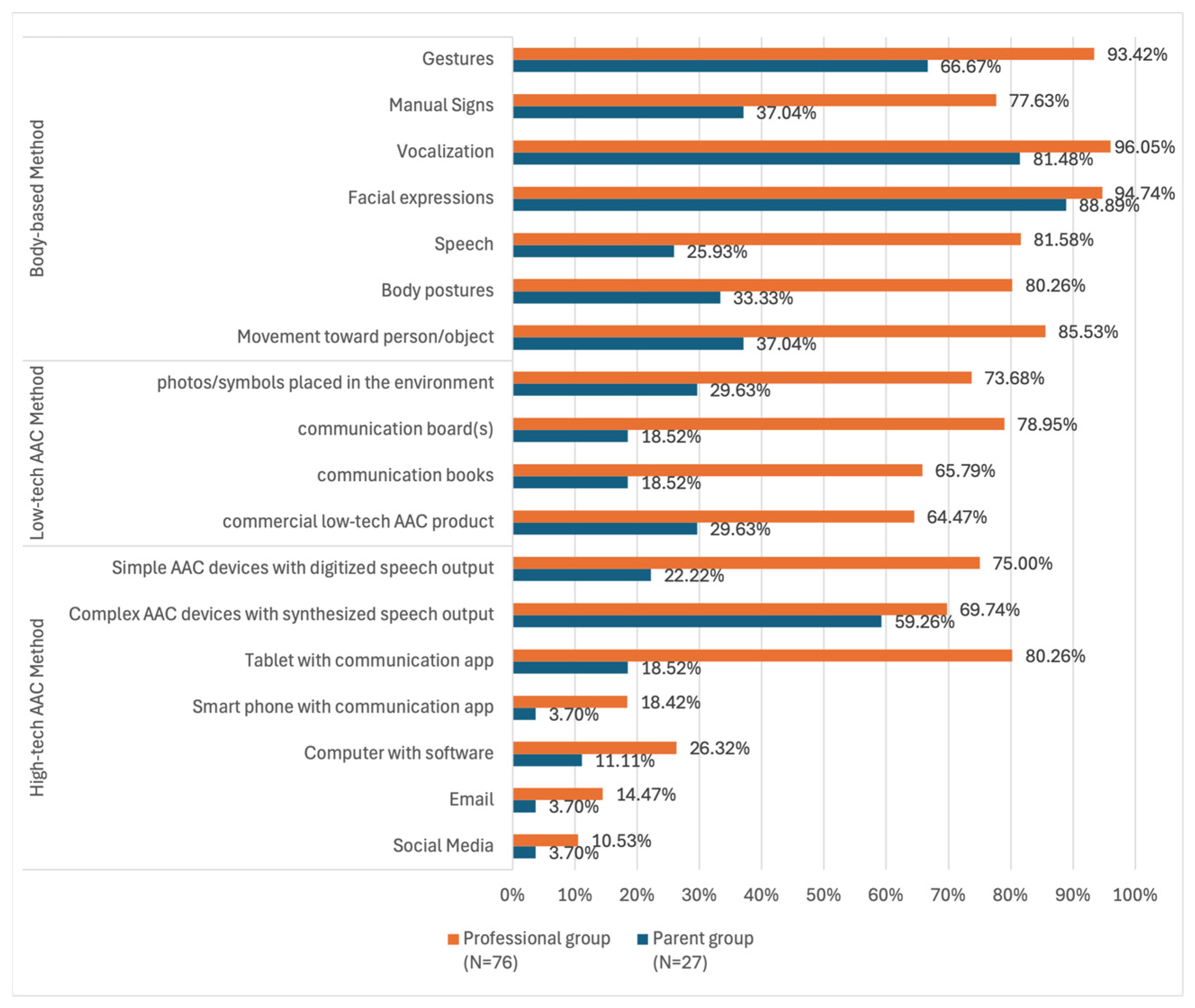
3.1. The Use of AAC
3.2. The Use of the HFSW
3.2.1. Types of the HFSW
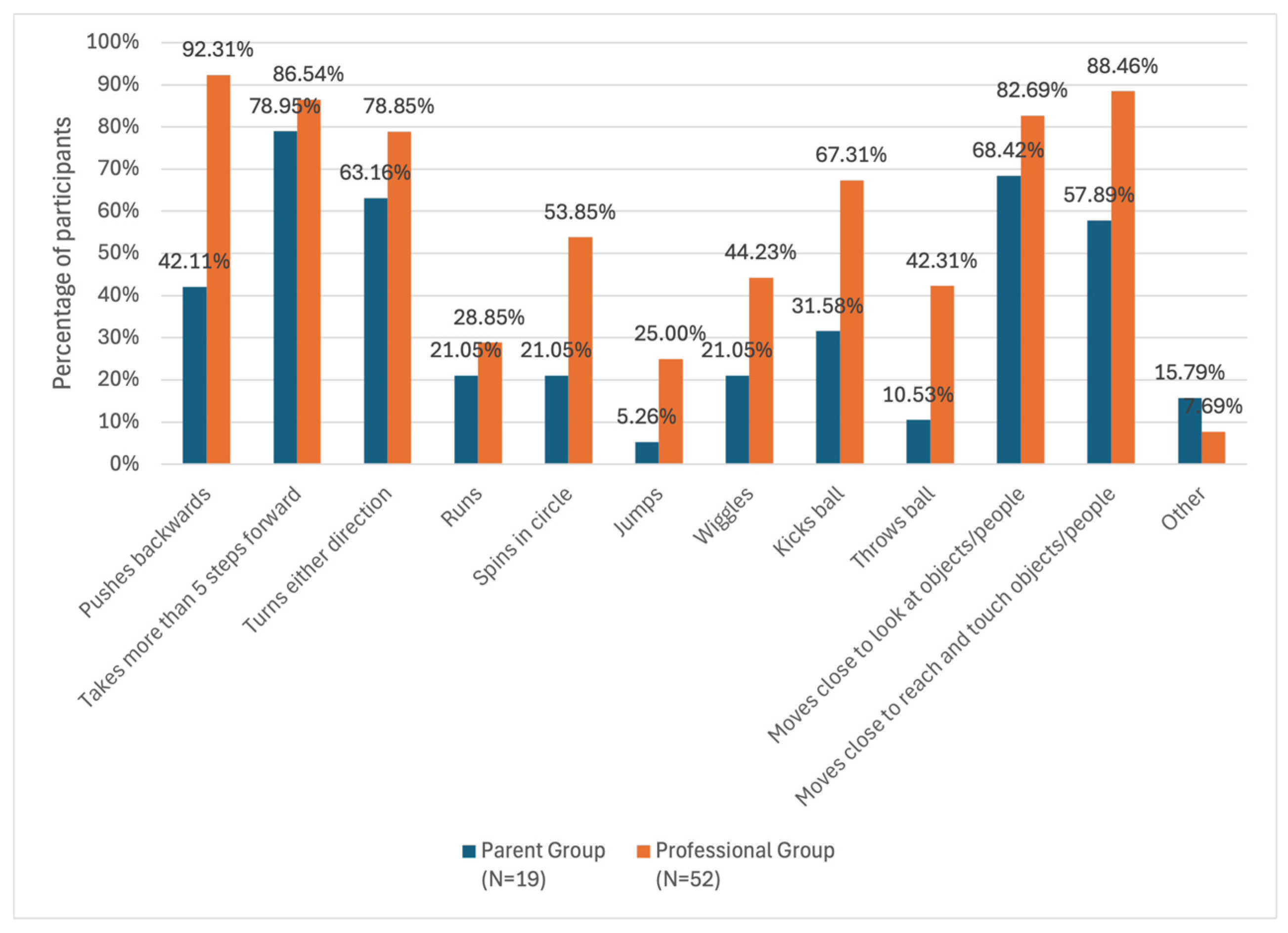
3.2.2. Motor Activities Observed
3.2.3. Purposes for Using the HFSW
3.3. Benefits of Using the HFSW
3.4. Difficulities Encountered
4. Discussion
4.1. Use of AAC
4.2. Use of the HFSW
4.2.1. Types of the HFSW
4.2.2. Motor Activities Observed
4.2.3. Purposes for Using the HFSW
4.3. Benefits of Using the HFSW
4.3.1. Benefits Related to Language and Communication
4.3.2. Benefits Related to Vision
4.4. Challenges of Using the HFSW
4.5. Clinical Implications
4.5.1. Providing More Information and Training to Parents
4.5.2. Adopting Family-Centered Interprofessional Collaborative Practice
4.6. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HFSW | Hands-free support walker |
| AAC | Augmentative and alternative communication |
| CVI | Cortical visual impairment |
References
- Feldner, H. Impacts of early powered mobility provision on disability identity: A case study. Rehabil. Psychol. 2019, 64, 130–145. [Google Scholar] [CrossRef]
- Bolton, T.; Plattner, L. Occupational therapy role in school-based practice: Perspectives from teachers and OTs. J. Occup. Ther. Sch. Early Interv. 2020, 13, 136–146. [Google Scholar] [CrossRef]
- Brandel, J. Speech-language pathology services in the schools: A follow-up 9 years later. Lang. Speech Hear. Serv. Sch. 2020, 51, 1037–1048. [Google Scholar]
- Green, L.; Chance, P.; Stockholm, M. Implementation and perceptions of classroom-based service delivery: A survey of public school clinicians. Lang. Speech Hear. Serv. Sch. 2019, 50, 656–672. [Google Scholar]
- Luo, F.; Blackstone, S.W.; Canchola, J.; Roman-Lantzy, C. Working with children with cortical visual impairment who use augmentative and alternative communication: Implications for improving current practice. Augment. Altern. Commun. 2022, 38, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, D.L.; Pavelko, S.L.; Hahs-Vaughn, D.L.; Dudding, C.C. A national survey of speech-language pathologists’ engagement in interprofessional collaborative practice in schools: Identifying predictive factors and barriers to implementation. Lang. Speech Hear. Serv. Sch. 2019, 50, 639–655. [Google Scholar] [CrossRef]
- Mueller, T.G.; Buckley, P.C. Fathers’ experiences with the special education system: The overlooked voice. Res. Pract. Pers. Sev. Disabil. 2014, 39, 119–135. [Google Scholar] [CrossRef]
- Sousa, A.C. “Crying doesn’t work”: Emotion and parental involvement of working class mothers raising children with developmental disabilities. DSQ 2015, 35, 1–33. [Google Scholar] [CrossRef]
- Blackstone, S.W.; Luo, F.; Canchola, J.; Wilkinson, K.M.; Roman-Lantzy, C. Children with cortical visual impairment and complex communication needs: Identifying gaps between needs and current practice. Lang. Speech Hear. Serv. Sch. 2021, 52, 612–629. [Google Scholar] [CrossRef]
- Cooper-Duffy, K.; Eaker, K. Effective team practices: Interprofessional contributions to communication issues with a parent’s perspective. Am. J. Speech-Lang. Pathol. 2017, 26, 181–192. [Google Scholar] [CrossRef]
- Mandak, K.; Light, J. Family-centered services for children with complex communication needs: The practices and beliefs of school-based speech-language pathologists. Augment. Altern. Commun. 2018, 34, 130–142. [Google Scholar] [CrossRef]
- Ogletree, B.T. Meeting complex communication needs associated with genetic syndromes: A call to interprofessional education and practice. Perspect. Augment. Altern. Commun. 2015, 24, 67–73. [Google Scholar] [CrossRef]
- Ogletree, B.T. Addressing the communication and other needs of persons with severe disabilities through engaged interprofessional teams: Introduction to a clinical forum. Am. J. Speech-Lang. Pathol. 2017, 26, 157–161. [Google Scholar] [CrossRef] [PubMed]
- McCarty, T.V.; Miller, C.A. Reason-based recommendations from a developmental systems approach for students with needs across functional domains. Lang. Speech Hear. Serv. Sch. 2023, 51, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Thelen, E. Development as a dynamic system. Trends Cogn. Sci. 2003, 7, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Gasser, M. The development of embodied cognition: Six lessons from babies. Artif. Life 2005, 11, 13–29. [Google Scholar] [CrossRef]
- Adolf, K.E.; Hoch, J.E. Motor development: Embodied, embedded, enculturated, and enabling. Annu. Rev. Psychol. 2019, 70, 141–164. [Google Scholar] [CrossRef]
- Campos, J.J.; Anderson, D.I.; Barbu-Roth, M.A.; Hubbard, E.M.; Hertenstein, M.J.; Witherington, D. Travel broadens the mind. Infancy 2000, 1, 149–219. [Google Scholar] [CrossRef]
- Gibson, E.J. Exploratory behavior in the development of perceiving, acting, and the acquiring of knowledge. Annu. Rev. Psychol. 1988, 39, 1–42. [Google Scholar] [CrossRef]
- Lobo, M.A.; Harbourne, R.T.; Dusing, S.C.; McCoy, S.W. Grounding early intervention: Physical therapy cannot just be about motor skills anymore. Phys. Ther. 2013, 93, 94–103. [Google Scholar] [CrossRef]
- Iverson, J.M. Developing language in a developing body: The relationship between motor development and language development. J. Child Lang. 2010, 37, 229–261. [Google Scholar] [CrossRef]
- Iverson, J.M. Developmental variability and developmental cascades: Lessons from motor and language development in infancy. Curr. Dir. Psychol. Sci. 2021, 30, 228–235. [Google Scholar] [CrossRef]
- Houwen, S.; Visser, L.; van der Putten, A.; Vlaskamp, C. The interrelationships between motor, cognitive, and language development in children with and without intellectual and developmental disabilities. Res. Dev. Disabil. 2016, 53, 19–31. [Google Scholar] [CrossRef]
- Oudgenoeg-Paz, P.; Volman, M.; Leseman, P. Attainment of sitting and walking predicts development of productive vocabulary between 16 and 28 months. Infant Behav. Dev. 2012, 35, 733–736. [Google Scholar] [CrossRef]
- Bennett, C.R.; Bauer, C.M.; Bailin, E.S.; Merabet, L.B. Neuroplasticity in cerebral visual impairment (CVI): Assessing functional vision and the neurophysiological correlates of dorsal stream dysfunction. Neurosci. Biobehav. Rev. 2020, 108, 171–181. [Google Scholar] [CrossRef]
- Fandakova, Y.; Hartley, C.A. Mechanisms of learning and plasticity in childhood and adolescence. Dev. Cogn. Neurosci. 2020, 42, 100764. [Google Scholar] [CrossRef] [PubMed]
- Mateos-Aparicio, P.; Rodríguez-Moreno, A. The impact of studying brain plasticity. Front. Cell. Neurosci. 2019, 13, 66. [Google Scholar] [CrossRef]
- May, A. Experience-dependent structural plasticity in the adult human brain. Trends Cogn. Sci. 2011, 15, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Brittlebank, S.; Light, J.C.; Pope, L. A scoping review of AAC interventions for children and young adults with simultaneous visual and motor impairments: Clinical and research Implications. Augment. Altern. Commun. 2024, 40, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Adolph, K.; Tamis-LeMonda, C. The costs and benefits of development: The transition from crawling to walking. Child Dev. Perspect. 2014, 8, 187–192. [Google Scholar] [CrossRef]
- He, M.; Walle, E.A.; Campos, J.J. A cross-national investigation of the relation between infant walking and language development. Infancy 2015, 20, 283–305. [Google Scholar] [CrossRef]
- Walle, E.A.; Campos, J.J. Infant language development is related to the acquisition of walking. Dev. Psychol. 2014, 50, 336–348. [Google Scholar] [CrossRef]
- West, K.L.; Iverson, J.M. Communication changes when infants begin to walk. Dev. Sci. 2021, 24, e13102. [Google Scholar] [CrossRef] [PubMed]
- Walle, E.A. Infant social development across the transition from crawling to walking. Front. Psychol. 2016, 7, 960. [Google Scholar] [CrossRef] [PubMed]
- Clearfield, M. Learning to walk changes infants’ social interactions. Infant Behav. Dev. 2011, 34, 15–25. [Google Scholar] [CrossRef]
- Kretch, K.S.; Franchak, J.M.; Adolph, K.E. Crawling and walking infants see the world differently. Child Dev. 2014, 85, 1503–1518. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Sato, A.; Itakura, S. Transition from crawling to walking changes gaze communication space in everyday infant-parent interaction. Front. Psychol. 2020, 10, 2987. [Google Scholar] [CrossRef]
- Karasik, L.B.; Tamis-Lemonda, C.S.; Adolph, K.E. Crawling and walking infants elicit different verbal responses from mothers. Dev. Sci. 2014, 17, 388–395. [Google Scholar] [CrossRef]
- Foreman, N.; Gillett, R.; Jones, S. Choice autonomy and memory for spatial locations in six-year-old children. Br. J. Psychol. 1994, 85, 17–27. [Google Scholar] [CrossRef]
- Feldner, H.A.; Logan, S.W.; Kenyon, L.K. In the driver’s seat: A randomized, crossover clinical trial protocol comparing home and community use of the Permobil Explorer Mini and a modified ride-on car by children with cerebral palsy. Phys. Ther. 2022, 102, pzac062. [Google Scholar] [CrossRef]
- Logan, S.W.; Feldner, H.A.; Galloway, J.C.; Huang, H.H. Modified ride-on car use by children with complex medical needs. Pediatr. Phys. Ther. 2016, 28, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Lynch, A.; Ryu, J.C.; Agrawal, S.; Galloway, J.C. Power mobility training for a 7-month-old infant with spina bifida. Pediatr. Phys. Ther. 2009, 21, 362–368. [Google Scholar] [CrossRef]
- Ragonesi, C.B.; Chen, X.; Agrawal, S.; Galloway, J.C. Power mobility and socialization in preschool: A case study of a child with cerebral palsy. Pediatr. Phys. Ther. 2010, 22, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Blackstone, S. Move to learn: Considerations for providing upright, hands-free, self-initiated mobility to children with severe physical and communication disabilities. Augment. Altern. Commun. 2025, Online ahead of print, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Paleg, G.S.; Livingstone, R.W. Evidence-informed clinical perspectives on selecting gait trainer features for children with cerebral palsy. Int. J. Ther. Rehabil. 2016, 23, 444–454. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child. Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Paleg, G.S. Measuring outcomes for children with cerebral palsy who use gait trainers. Technologies 2016, 4, 22. [Google Scholar] [CrossRef]
- Bradbury, M.; Tierney, S. Perspectives of children with physical disabilities, parents and physiotherapists on use of walkers and their potential to increase physical activity. A qualitative exploration. J. Child Health Care 2022, 28, 256–276. [Google Scholar] [CrossRef]
- Kuenzle, C.; Brunner, R. The effects of the norsk funktion-walking orthosis on the walking ability of children with cerebral palsy and severe gait impairment. J. Prosthet. Orthot. 2009, 21, 138–144. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Paleg, G.S. Use of Overground Supported-Stepping Devices for Non-Ambulant Children, Adolescents, and Adults with Cerebral Palsy: A Scoping Review. Disabilities 2023, 3, 165–195. [Google Scholar] [CrossRef]
- Paleg, G.S.; Livingstone, R.W. Outcomes of gait trainer use in home and school settings for children with motor impairments: A systematic review. Clin. Rehabil. 2015, 29, 1077–1091. [Google Scholar] [CrossRef] [PubMed]
- George, C.; Levin, W.; Ryan, J.M. The use and perception of support walkers for children with disabilities: A United Kingdom survey. BMC Pediatr. 2020, 20, 528. [Google Scholar] [CrossRef] [PubMed]
- Wright-Ott, C. Mobility. In Occupational Therapy for Children and Adolescents, 7th ed.; Case-Smith, J., O’Brien, J.C., Eds.; Mosby: St. Louis, MO, USA, 2015; pp. 560–594. [Google Scholar]
- Wright-Ott, C. Mobility Matters: Imbedding Hands-Free Locomotion Experiences into the Preschool/Elementary Curricula for Students with Severe Speech and Motor Impairment. Available online: https://curriculum.bridgeschool.org/wp-content/uploads/sites/5/2018/06/mobility_matters.pdf (accessed on 11 June 2025).
- McKeever, P.; Rossen, B.E.; Scott, H.; Robinson-Vincent, K.; Wright, V. The significance of uprightness: Parents’ reflections on children’s responses to a hands-free walker for children. Disabil. Soc. 2013, 28, 380–392. [Google Scholar] [CrossRef]
- Low, S.A.; McCoy, S.W.; Beling, J.; Adams, J. Pediatric physical therapists’ use of support walkers for children with disabilities: A nationwide survey. Pediatr. Phys. Ther. 2011, 23, 381–389. [Google Scholar] [CrossRef]
- Eisenberg, S.; Zuk, L.; Carmeli, E.; Katz-Leurer, M. Contribution of stepping while standing to function and secondary conditions among children with cerebral palsy. Pediatr. Phys. Ther. 2009, 21, 79–85. [Google Scholar] [CrossRef]
- Gudjonsdottir, B.; Gudmundsdottir, S.B. Mobility devices for children with physical disabilities: Use, satisfaction and impact on participation. Disabil. Rehabil. Assist. Technol. 2023, 18, 722–729. [Google Scholar] [CrossRef]
- Wright, F.V.; Jutai, J.W. Evaluation of the longer-term use of the David Hart Walker Orthosis by children with cerebral palsy: A 3-year prospective evaluation. Disabil. Rehabil. Assist. Technol. 2006, 1, 155–166. [Google Scholar] [CrossRef]
- Light, J. Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augment. Altern. Commun. 1989, 5, 137–144. [Google Scholar] [CrossRef]
- Light, J.; McNaughton, D. Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication. Augment. Altern. Commun. 2014, 30, 1–18. [Google Scholar] [CrossRef]
- Brown, F.; Cohen, S. Self-determination and young children. J. Assoc. Pers. Sev. Handicap. 1996, 21, 22–30. [Google Scholar] [CrossRef]
- Wright-Ott, C.; Blackstone, S.; Pressman, H. The significance of support walker mobility for children with cortical visual impairment, complex speech, and physical needs: The Bridge School experience. Closing Gap Solut. 2021, 40, 20–33. [Google Scholar]
- Light, J.; McNaughton, D.; Caron, J. New and emerging AAC technology supports for children with complex communication needs and their communication partners: State of the science and future research directions. Augment. Altern. Commun. 2019, 35, 26–41. [Google Scholar] [CrossRef]
- McCarty, T.V.; Light, J.C. “It’s like a guessing game all the time”: Parent insights on barriers, supports, and priorities for children with cortical visual impairment and complex communication needs. Augment. Altern. Commun. 2023, 39, 256–269. [Google Scholar] [CrossRef]
- de Geeter, K.I.; Poppes, P.; Vlaskamp, C. Parents as experts: The position of parents of children with profound multiple disabilities. Child Care Health Dev. 2002, 28, 443–453. [Google Scholar] [CrossRef]
- Etikan, I.; Musa, S.A.; Alkassim, R.S. Comparison of Convenience Sampling and Purposive Sampling. Am. J. Theor. Appl. Stat. 2016, 5, 1–4. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- SAS Institute Inc. SAS/STAT® 15.3 User’s Guide; SAS Institute Inc.: Cary, NC, USA, 2023. [Google Scholar]
- Cramer, H. Mathematical Methods of Statistics; Princeton University Press: Princeton, NJ, USA, 1946. [Google Scholar]
- Berenguer, C.; Martínez, E.R.; De Stasio, S.; Baixauli, I. Parents’ perceptions and experiences with their children’s use of augmentative/alternative communication: A systematic review and qualitative meta-synthesis. Int. J. Environ. Res. Public Health 2022, 19, 8091. [Google Scholar] [CrossRef] [PubMed]
- Doak, L. Rethinking family (dis)engagement with augmentative & alternative communication. J. Res. Spec. Educ. Needs 2021, 21, 198–210. [Google Scholar]
- Yau, S.H.; Choo, K.; Tan, J.; Monson, O.; Bovell, S. Comparing and contrasting barriers in augmentative alternative communication use in nonspeaking autism and complex communication needs: Multi-stakeholder perspectives. Front. Psychiatry 2024, 15, 1385947. [Google Scholar] [CrossRef] [PubMed]
- Boster, J.B.; McCarthy, J.W.; Brown, K.; Spitzley, A.M.; Blackstone, S.W. Creating a path for systematic investigation of children with cortical visual impairment who use augmentative and alternative communication. Am. J. Speech-Lang. Pathol. 2021, 30, 1880–1893. [Google Scholar] [CrossRef]
- Katoch, S.; Devi, A.; Kulkarni, P. Ocular defects in cerebral palsy. Indian J. Ophthalmol. 2007, 55, 154–156. [Google Scholar] [CrossRef]
- Lagunju, I.A.; Oluleye, T.S. Ocular abnormalities in children with cerebral palsy. Afr. J. Med. Med. Sci. 2007, 36, 71–75. [Google Scholar]
- Philip, S.S.; Guzzetta, A.; Chorna, O.; Gole, G.; Boyd, R.N. Relationship between brain structure and cerebral visual impairment in children with cerebral palsy: A systematic review. Res. Dev. Disabil. 2020, 99, 103580. [Google Scholar] [CrossRef]
- Rodríguez-Costa, I.; De la Cruz-López, I.; Fernández-Zárate, I.; Maldonado-Bascón, S.; Lafuente-Arroyo, S.; Nunez-Nagy, S. Benefits of a low-cost walking device in children with cerebral palsy: A qualitative study. Int. J. Environ. Res. Public Health 2021, 18, 2808. [Google Scholar] [CrossRef]
- Mandak, K.; O’Neill, T.; Light, J.; Fosco, G.M. Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augment. Altern. Commun. 2017, 33, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Pappas, N.W.; McLeod, S. Working with Families in Speech-Language Pathology, 1st ed.; Plural Publishing Inc.: San Diego, CA, USA, 2008. [Google Scholar]
- Wilkinson, K.M.; Elko, L.R.; Elko, E.; McCarty, T.V.; Sowers, D.J.; Blackstone, S.; Roman-Lantzy, C. An evidence-based approach to augmentative and alternative communication design for individuals with cortical visual impairment. Am. J. Speech-Lang. Pathol. 2023, 32, 1939–1960. [Google Scholar] [CrossRef] [PubMed]
- Lundeby, H.; Tøssebro, J. Exploring the experiences of “not being listened to” from the perspective of parents with disabled children. Scand. J. Disabil. Res. 2008, 10, 258–274. [Google Scholar] [CrossRef]
- Bundonis, J. Benefits of Early Mobility with an Emphasis on Gait Training. Available online: https://www.rifton.com/education-center/articles/benefits-of-early-mobility-with-an-emphasis-on-gait-training (accessed on 11 June 2025).
- Scheiman, M. Understanding and Managing Vision Deficits: A Guide for Occupational Therapists, 3rd ed.; Routledge: New York, NY, USA, 2024. [Google Scholar]
- Galiano, A.R.; Portalier, S. Language and Visual Impairment: Literature Review. Int. Psychol. Pract. Res. 2011, 2, 1–10. [Google Scholar]
- Bakke, H.A.; Cavalcante, W.A.; Oliveira, I.S.D.; Sarinho, S.W.; Cattuzzo, M.T. Assessment of motor skills in children with visual impairment: A systematic and integrative review. Clin. Med. Insights Pediatr. 2019, 13, 1179556519838287. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, S.; Hopper, C. Individuals with visual impairments: A review of psychomotor behavior. Adapt. Phys. Activ. Q. 1996, 13, 16–26. [Google Scholar] [CrossRef]
- Higginbotham, D.J.; Shane, H.; Russell, S.; Caves, K. Access to AAC: Present, past, and future. Augment. Altern. Commun. 2007, 23, 243–257. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, K.M.; Jagaroo, V. Contributions of principles of visual cognitive science to AAC system display design. Augment. Altern. Commun. 2004, 20, 123–136. [Google Scholar] [CrossRef]
- American Speech-Language-Hearing Association. Preferred Practice Patterns for the Profession of Speech-Language Pathology [Preferred Practice Patterns]. Available online: https://www.asha.org/policy/PP2004-00191 (accessed on 11 June 2025).
- American Speech-Language-Hearing Association. Interprofessional Education/Interprofessional Practice (IPE/IPP). Available online: https://www.asha.org/practice/ipe-ipp/ (accessed on 14 July 2025).
- American Occupational Therapy Association. Joint Statement on Interprofessional Collaborative Goals in School-Based Practice. Available online: https://www.aota.org/-/media/corporate/files/practice/schools/joint-statement-on-interprofessional-collaborative-goals-in-school-based-practice.pdf (accessed on 14 July 2025).
- American Physical Therapy Association. Commitment to Interprofessional Education and Practice. Available online: https://www.apta.org/apta-and-you/leadership-and-governance/policies/commitment-interprofessional-education-practice (accessed on 14 July 2025).


| Disciplines | Number of Participants | Percentage of the Total (N = 90) |
|---|---|---|
| Physical therapists | 22 | 24.44 |
| Speech–language pathologists | 18 | 20.00 |
| Special education teachers | 13 | 14.44 |
| Teachers of the visually impaired and/or orientation and mobility specialists | 14 | 15.56 |
| Assistive technologist | 11 | 12.22 |
| Occupational therapists | 6 | 6.67 |
| Paraprofessionals | 6 | 6.67 |
| Purposes | Parent Group (%) | Professional Group (%) | z | p | Cramér’s V |
|---|---|---|---|---|---|
| (N = 21) | (N = 54) | ||||
| Achieve specific motor/mobility goals | |||||
| Provide independent mobility | 76.19 | 94.44 | −2.3 | 0.078 | 0.266 |
| Improve hip development | 47.62 | 40.74 | 0.54 | 0.677 | 0.062 |
| Maintain bone mineral density | 47.62 | 46.3 | 0.1 | 0.918 | 0.012 |
| Reduce hip/knee ankle contracture | 19.05 | 40.74 | −1.77 | 0.146 | 0.204 |
| Improve muscle strength | 76.19 | 87.04 | −1.15 | 0.411 | 0.133 |
| Achieve cardiopulmonary exercise | 28.57 | 53.7 | −1.96 | 0.115 | 0.226 |
| Reduce spasticity (hypertonus) through movement | 28.57 | 33.33 | −0.4 | 0.723 | 0.046 |
| Achieve specific ADL/functional goals | |||||
| Improve digestive function | 57.14 | 50 | 0.56 | 0.677 | 0.065 |
| Encourage use of upper extremities for reaching/touching | 61.9 | 70.37 | −0.71 | 0.65 | 0.082 |
| Encourage problem solving opportunities | 47.62 | 72.22 | −2.01 | 0.113 | 0.232 |
| Increase independence and participation in daily life | 52.38 | 83.33 | −2.77 | 0.044 * | 0.320 |
| Participate in recess activities | 42.86 | 70.37 | −2.21 | 0.078 | 0.255 |
| Encourage motivating activities | 61.9 | 81.48 | −1.78 | 0.146 | 0.206 |
| Achieve educational goals | |||||
| Increase opportunities to participate with peers | 66.67 | 88.89 | −2.28 | 0.078 | 0.263 |
| Access school environment | 57.14 | 90.74 | −3.35 | 0.013 * | 0.387 |
| Explore surroundings | 85.71 | 90.74 | −0.63 | 0.672 | 0.073 |
| Move to specific location (e.g., retrieve lunch bag) | 38.1 | 77.78 | −3.27 | 0.012 * | 0.378 |
| Move close to see objects and people | 57.14 | 85.19 | −2.6 | 0.053 | 0.300 |
| Access recess activities such as running, jumping, and playground games | 38.1 | 66.67 | −2.26 | 0.078 | 0.261 |
| Participate in inclusive physical education | 57.14 | 62.96 | −0.46 | 0.703 | 0.053 |
| Increase activity level | 71.43 | 85.19 | −1.37 | 0.3 | 0.158 |
| I am not sure | 0 | 5.56 | −1.1 | 0.415 | 0.127 |
| Other | 9.52 | 3.7 | 1.01 | 0.451 | 0.117 |
| Benefits | Parent Group (%) | Professional Group (%) | z | p | Cramér’s V |
|---|---|---|---|---|---|
| (N = 21) | (N = 64) | ||||
| Physical benefits | |||||
| Achieves a means for exercising and being physical active | 71.43 | 85.94 | −1.51 | 0.176 | 0.164 |
| Increase opportunities for self-initiated mobility | 61.9 | 93.75 | −3.64 | 0.007 * | 0.395 |
| Improves motor control (e.g., stepping, reaching, head and trunk) | 66.67 | 76.56 | −0.9 | 0.386 | 0.098 |
| Encourages use of arms/hands for reaching and exploring | 52.38 | 78.13 | −2.27 | 0.053 | 0.246 |
| Enables a child to move close to view and touch objects and people | 52.38 | 81.25 | −2.62 | 0.037 * | 0.284 |
| Enables a child to move towards a desired place or move away from an undesirable place or event | 57.14 | 84.38 | −2.6 | 0.037 * | 0.282 |
| Acquires new motor skills like jumping, wiggling, running, spinning | 19.05 | 50 | −2.49 | 0.037 * | 0.270 |
| Improves muscle strength | 57.14 | 78.13 | −1.88 | 0.099 | 0.204 |
| Improves bone mineral density | 23.81 | 50 | −2.1 | 0.073 | 0.228 |
| Provides a change in position | 71.43 | 85.94 | −1.51 | 0.176 | 0.164 |
| Assists with gastroenterology issues and regularity | 42.86 | 59.38 | −1.32 | 0.216 | 0.143 |
| Social/Emotional/Participation benefits | |||||
| Brings enjoyment: Child smiles, laughs, wants to use the support walker | 85.71 | 85.94 | −0.03 | 0.98 | 0.003 |
| Increases independence and access to surroundings (e.g., opens/closes drawers, reaches for objects, moves to favorite location, plays at peer height) | 71.43 | 84.38 | −1.32 | 0.216 | 0.143 |
| Increases peer/sibling/family interaction | 52.38 | 68.75 | −1.36 | 0.216 | 0.148 |
| Benefits in other key developmental areas | |||||
| Improves communication (e.g., points with arm/hand to a desired location, moves close to a peer to interact, moves away from an undesired event, moves self to seek a needed object like food/drink, moves upon request, answers a question (e.g., “What’s next?”, “Where is the group?”) by moving to that location) | 38.1 | 68.75 | −2.5 | 0.037 * | 0.271 |
| Increases verbalization/vocalizations while standing and moving in a hands-free support walker | 33.33 | 67.19 | −2.74 | 0.037 * | 0.297 |
| Demonstrates more eye contact with people or objects | 33.33 | 62.5 | −2.33 | 0.050 * | 0.253 |
| Uses movement in a hands-free support walker to attain or sustain vision before looking at a visual stimulus (e.g., wiggling, jumping, bouncing) | 33.33 | 53.13 | −1.58 | 0.176 | 0.171 |
| Demonstrates curiosity and problem solving (e.g., interacting with an object to learn how it works, such as turning on a water fountain or opening a door handle, finding and exploring a new place or objects) | 42.86 | 75 | −2.72 | 0.037 * | 0.295 |
| Is more attentive and focused after moving in a hands-free support walker | 33.33 | 45.31 | −0.96 | 0.367 | 0.104 |
| Uses vision to kick a ball, look for feet, reach for a favorite object, move toward/away from a person or an activity, explore the environment | 33.33 | 59.38 | −2.07 | 0.073 | 0.225 |
| Other options | |||||
| No benefits have been observed | 9.52 | 0 | 2.5 | 0.037 * | 0.271 |
| Other | 14.29 | 3.13 | 1.89 | 0.099 | 0.205 |
| Problems | Parent Group (%) | Professional Group (%) | z | p | Cramér’s V |
|---|---|---|---|---|---|
| (N = 21) | (N = 62) | ||||
| Not enough space indoors to use it functionally | 61.9 | 62.9 | −0.08 | 0.956 | 0.009 |
| Difficulty for the child or the client to move over uneven surfaces (e.g., cracks in sidewalk, over carpet, thresholds) | 57.14 | 75.81 | −1.63 | 0.464 | 0.179 |
| Transfers in/out of the walker are difficulty | 57.14 | 56.45 | 0.06 | 0.956 | 0.007 |
| Time (and staff) required to transfer the child or the client in/out of the walker | 38.1 | 62.9 | −1.98 | 0.427 | 0.217 |
| Finding time for the child or the client to use the walker | 42.86 | 32.26 | 0.88 | 0.585 | 0.097 |
| Difficulty adjusting it (for multiple users) | 28.57 | 16.13 | 1.25 | 0.476 | 0.137 |
| Therapist or care provider’s belief that using the walker will not support the child’s or the client’s therapy goals | 14.29 | 9.68 | 0.59 | 0.716 | 0.065 |
| Musculoskeletal issues (e.g., spasticity, muscle tightening, muscle fatigue, etc.) | 23.81 | 33.87 | −0.86 | 0.585 | 0.094 |
| Other | 28.57 | 16.13 | 1.25 | 0.476 | 0.137 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, F.; Blackstone, S.W.; Canchola, J.; Casella, V. Surveying the Perspectives of Parents and Professionals on Providing Upright, Hands-Free, Self-Initiated Mobility to Children with Severe Physical and Communication Disabilities. Children 2025, 12, 1024. https://doi.org/10.3390/children12081024
Luo F, Blackstone SW, Canchola J, Casella V. Surveying the Perspectives of Parents and Professionals on Providing Upright, Hands-Free, Self-Initiated Mobility to Children with Severe Physical and Communication Disabilities. Children. 2025; 12(8):1024. https://doi.org/10.3390/children12081024
Chicago/Turabian StyleLuo, Fei, Sarah W. Blackstone, Jesse Canchola, and Vicki Casella. 2025. "Surveying the Perspectives of Parents and Professionals on Providing Upright, Hands-Free, Self-Initiated Mobility to Children with Severe Physical and Communication Disabilities" Children 12, no. 8: 1024. https://doi.org/10.3390/children12081024
APA StyleLuo, F., Blackstone, S. W., Canchola, J., & Casella, V. (2025). Surveying the Perspectives of Parents and Professionals on Providing Upright, Hands-Free, Self-Initiated Mobility to Children with Severe Physical and Communication Disabilities. Children, 12(8), 1024. https://doi.org/10.3390/children12081024






