Adherence to the Mediterranean Diet and Arterial Blood Pressure in Schoolchildren: The Role of Parental Eating Habits
Abstract
1. Introduction
2. Materials and Methods
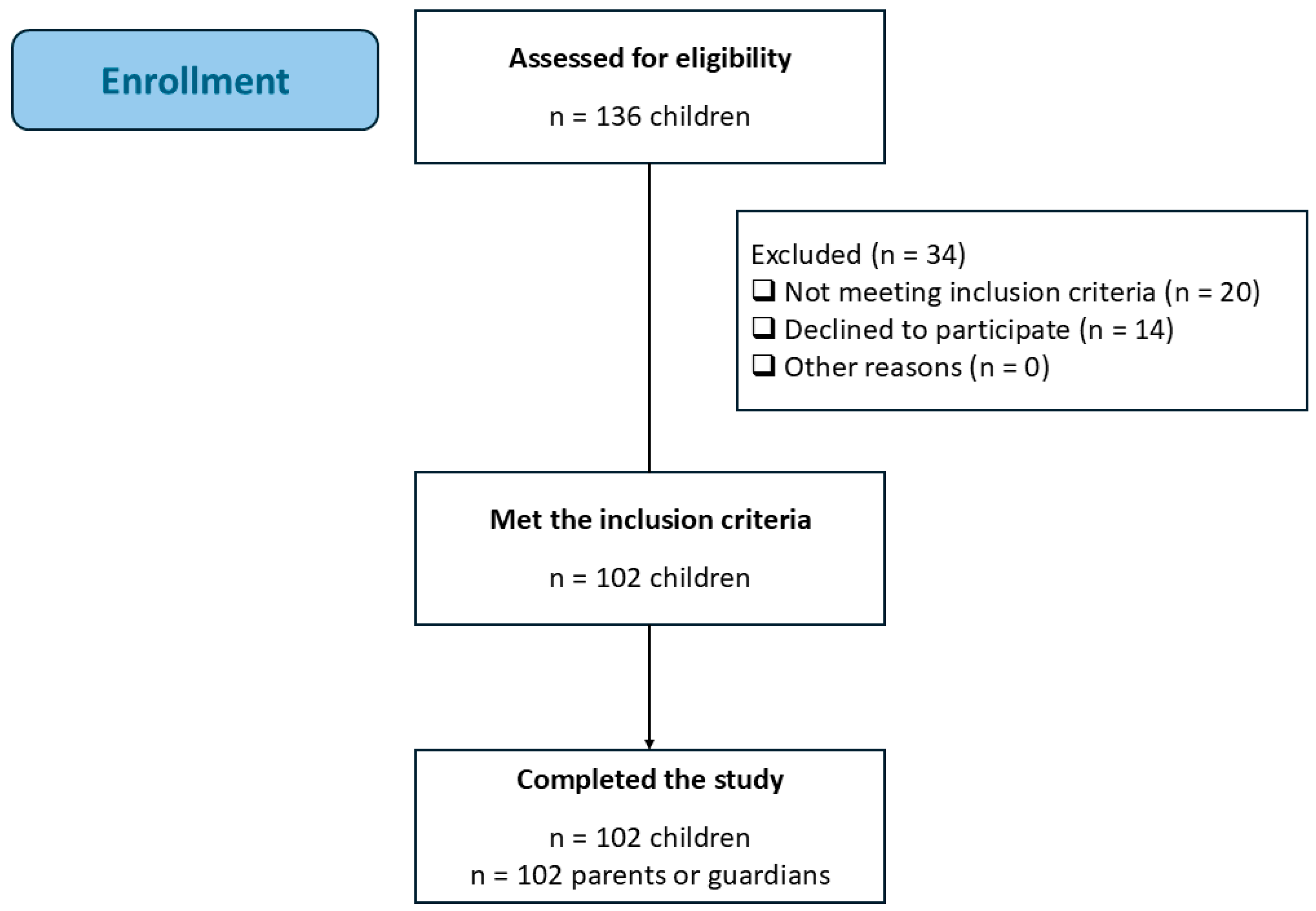
2.1. Study Design and Participants
2.2. Bioethics
2.3. Inclusion and Exclusion Criteria
2.4. Measurements
2.4.1. Children’s Screening
- Sociodemographic characteristics: Age (years) and gender (female/male).
- Anthropometric indices: A flat scale with light clothing was used to measure body weight, while a calibrated stadiometer with an accuracy of 0.1 cm was used to measure height. The z-scores for BMI-for-age, weight-for-age, and height-for-age were calculated according to WHO growth reference data for boys and girls aged 5 to 19 years old [13]. The International Obesity Task Force (IOTF) established age- and sex-specific body mass index cut-off criteria that were used to evaluate the weight status of the participants [14]. Consequently, they were classified into four categories: underweight, normal weight, overweight, and obese. Waist and hip circumferences were measured with a flexible non-stretch tape without clothes. Waist circumference was measured in the middle, between the lowest rib and the iliac crest, using an inelastic measuring tape to the nearest 0.1 cm, while hip circumference was measured between the greater trochanter and the lower buttock level. To define abdominal adiposity, the waist-to-hip ratio was used.
- Eating habits: The KIDMED score (range from −4 to 12), a quality index intended for children and adolescents, was used to evaluate adherence to the Mediterranean Diet [15]. A score of +1 was assigned to dietary behaviors that show a favorable aspect to this dietary pattern, while a score of −1 was assigned to dietary practices that have unfavorable associations. Lower adherence to the Mediterranean diet was indicated by lower scores, while higher devotion was shown by higher scores.
- Clinical parameters: BP was measured in the right arm by using standard procedures [16]. A validated automated oscillometric device (OMRON M3, HEM-7154-E, Omron Corporation (Kyoto, Japan)) suitable for children was used to measure BP. Using a cuff size chosen based on the child’s mid-upper arm circumference, measurements were taken on the child’s right upper arm. Children were told to sit quietly, with their backs supported, feet flat on the ground, and arms at the level of the heart. Following a minimum of five minutes of rest, two consecutive BP measures were obtained. During the procedure, the children were instructed not to move or speak. The mean value of two BP measurements that were obtained at least two minutes apart was used in the present work [17].
2.4.2. Parental Screening
- Sociodemographic characteristics: The sociodemographic data were age (years), gender (female/male), and level of education (secondary/tertiary/postgraduate education).
- Eating habits: A semi-quantitative, validated, and reproducible food frequency questionnaire was used to evaluate dietary habits [18]. The consumption of several food groups (including red meat and meat products, poultry, fish, milk or other dairy products, fruits, vegetables, legumes, olive oil, and beverages, including alcohol), was assessed. Finally, the level of adherence to the Mediterranean Diet was assessed using the MedDietScore (range: 0–55) [19]. Lower values indicated lower adherence, while higher values indicated greater adherence.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| DBP | Diastolic blood pressure |
| SBP | Systolic blood pressure |
| WAz | Weight-to-age z-score |
| HAz | Height-to-age z-score |
References
- Early Childhood Development|UNICEF. Available online: https://www.unicef.org/early-childhood-development (accessed on 12 May 2025).
- Robinson, C.H.; Chanchlani, R. High Blood Pressure in Children and Adolescents: Current Perspectives and Strategies to Improve Future Kidney and Cardiovascular Health. Kidney Int. Rep. 2022, 7, 954–970. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Zhang, Y.; Yu, J.; Zha, M.; Zhu, Y.; Rahimi, K.; Rudan, I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2019, 173, 1154. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Sun, J.; Zhao, M.; Liang, Y.; Bovet, P.; Xi, B. Elevated Blood Pressure in Childhood and Hypertension Risk in Adulthood: A Systematic Review and Meta-Analysis. J. Hypertens. 2020, 38, 2346–2355. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.R.; Pratt, C.A.; Hayman, L.L. Reduction of Risk for Cardiovascular Disease in Children and Adolescents. Circulation 2011, 124, 1673–1686. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health: A Critical Review. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Richardson, L.A.; Izuora, K.; Basu, A. Mediterranean Diet and Its Association with Cardiovascular Disease Risk Factors: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 12762. [Google Scholar] [CrossRef]
- López-Gil, J.F.; García-Hermoso, A.; Martínez-González, M.Á.; Rodríguez-Artalejo, F. Mediterranean Diet and Cardiometabolic Biomarkers in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2024, 7, e2421976. [Google Scholar] [CrossRef]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The Influence of Parental Dietary Behaviors and Practices on Children’s Eating Habits. Nutrients 2021, 13, 1138. [Google Scholar] [CrossRef]
- Vepsäläinen, H.; Nevalainen, J.; Fogelholm, M.; Korkalo, L.; Roos, E.; Ray, C.; Erkkola, M.; DAGIS Consortium Group. Like Parent, like Child? Dietary Resemblance in Families. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 62. [Google Scholar] [CrossRef] [PubMed]
- Growth Reference Data for 5-19 Years—Indicators. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators (accessed on 19 May 2025).
- Cole, T.J. Establishing a Standard Definition for Child Overweight and Obesity Worldwide: International Survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Rehman, S.; Hashmi, M.F. Blood Pressure Measurement. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Araujo-Moura, K.; Souza, L.G.; Mello, G.L.; De Moraes, A.C.F. Blood Pressure Measurement in Pediatric Population: Comparison between Automated Oscillometric Devices and Mercury Sphygmomanometers—A Systematic Review and Meta-Analysis. Eur. J. Pediatr. 2022, 181, 9–22. [Google Scholar] [CrossRef]
- Bountziouka, V.; Bathrellou, E.; Giotopoulou, A.; Katsagoni, C.; Bonou, M.; Vallianou, N.; Barbetseas, J.; Avgerinos, P.C.; Panagiotakos, D.B. Development, Repeatability and Validity Regarding Energy and Macronutrient Intake of a Semi-Quantitative Food Frequency Questionnaire: Methodological Considerations. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 659–667. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary Patterns: A Mediterranean Diet Score and Its Relation to Clinical and Biological Markers of Cardiovascular Disease Risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Fernández-Galván, L.M.; Adelantado-Renau, M.; Beltran-Valls, M.R.; Moliner-Urdiales, D. Relationship Between Dietary Patterns and Blood Pressure During Adolescence: A Longitudinal Analysis from Dados Study. Am. J. Hum. Biol. 2025, 37, e24199. [Google Scholar] [CrossRef]
- Cárdenas-Fuentes, G.; Homs, C.; Ramírez-Contreras, C.; Juton, C.; Casas-Esteve, R.; Grau, M.; Aguilar-Palacio, I.; Fitó, M.; Gomez, S.F.; Schröder, H. Prospective Association of Maternal Educational Level with Child’s Physical Activity, Screen Time, and Diet Quality. Nutrients 2021, 14, 160. [Google Scholar] [CrossRef]
- Bouthoorn, S.H.; Van Lenthe, F.J.; De Jonge, L.L.; Hofman, A.; Van Osch-Gevers, L.; Jaddoe, V.W.V.; Raat, H. Maternal Educational Level and Blood Pressure, Aortic Stiffness, Cardiovascular Structure and Functioning in Childhood: The Generation R Study. Am. J. Hypertens. 2014, 27, 89–98. [Google Scholar] [CrossRef]
- Maia, C.; Braz, D.; Fernandes, H.M.; Sarmento, H.; Machado-Rodrigues, A.M. The Impact of Parental Behaviors on Children’s Lifestyle, Dietary Habits, Screen Time, Sleep Patterns, Mental Health, and BMI: A Scoping Review. Children 2025, 12, 203. [Google Scholar] [CrossRef]
- Hughes, S.O.; Papaioannou, M.A. Maternal Predictors of Child Dietary Behaviors and Weight Status. Curr. Nutr. Rep. 2018, 7, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Luque, V.; Mucarzel, F.; Hertogs, A.; Seed, P.T.; Flynn, A.C.; Poston, L.; Dalrymple, K.V. Associations between Maternal Diet, Family Eating Habits and Preschool Children’s Dietary Patterns: Insights from the UPBEAT Trial. Nutr. J. 2024, 23, 115. [Google Scholar] [CrossRef] [PubMed]
- Pfledderer, C.D.; Gren, L.H.; Metos, J.; Brusseau, T.A.; O’Toole, K.; Buys, S.S.; Daly, M.B.; Frost, C.J. Mothers’ Diet and Family Income Predict Daughters’ Healthy Eating. Prev. Chronic Dis. 2021, 18, 200445. [Google Scholar] [CrossRef]
- Linde, J.A.; Horning Dehmer, M.L.; Lee, J.; Friend, S.; Flattum, C.; Arcan, C.; Fulkerson, J.A. Associations of Parent Dietary Role Modeling with Children’s Diet Quality in a Rural Setting: Baseline Data from the NU-HOME Study. Appetite 2022, 174, 106007. [Google Scholar] [CrossRef]
- Yee, A.Z.H.; Lwin, M.O.; Ho, S.S. The Influence of Parental Practices on Child Promotive and Preventive Food Consumption Behaviors: A Systematic Review and Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef]
- Costa, A.; Oliveira, A. Parental Feeding Practices and Children’s Eating Behaviours: An Overview of Their Complex Relationship. Healthcare 2023, 11, 400. [Google Scholar] [CrossRef]
- De Pergola, G.; D’Alessandro, A. Influence of Mediterranean Diet on Blood Pressure. Nutrients 2018, 10, 1700. [Google Scholar] [CrossRef]
| Children (N = 102) | Age (years) | 12.2 ± 3.2 |
| Female, n (%) | 46 (45) | |
| Weight (kg) | 51.6 ± 19.8 | |
| WAz | 0.63 ± 1.2 | |
| Height (cm) | 152 ± 19.6 | |
| HAz | 0.05 ± 1.3 | |
| Waist circumference (cm) | 71.7 ± 11.7 | |
| Hip circumference (cm) | 84.6 ± 17.5 | |
| Waist-to-hip ratio | 0.89 ± 0.2 | |
| z-BMI | 0.62 ± 1.6 | |
| Normal weight, n (%) | 50 (49) | |
| KIDMED (−4 to 12) | 5.56 ± 2.6 | |
| SBP (mm Hg) | 109 ± 12 | |
| DBP (mm Hg) | 68 ± 9.1 | |
| Parents (N = 102) | Female, n (%) | 86 (84) |
| Secondary education, n (%) | 37 (36.3) | |
| Tertiary education, n (%) | 36 (35.3) | |
| Postgraduate education, n (%) | 29 (28.4) | |
| MedDietScore (0–55) | 32.0 ± 4.1 |
| First Tertiary Low (n = 19) | Second Tertiary Medium (n = 44) | Third Tertiary High (n = 39) | p | ||
|---|---|---|---|---|---|
| Children (N = 102) | Age (years) | 13.4 ± 3.7 | 12.4 ± 3.0 | 11.3 ± 3.3 | 0.08 |
| Female, n (%) | 7 (37) | 24 (55) | 19 (49) | 0.43 | |
| Weight (kg) | 59 ± 19 | 51 ± 18 | 48 ± 22 | 0.12 | |
| WAz | 0.89 ± 0.9 | 0.48 ± 1.1 | 0.67 ± 1.5 | 0.47 | |
| Height (cm) | 159 ± 21 | 152 ± 18 | 147 ± 19 | 0.06 | |
| HAz | 0.28 ± 1.3 | −0.02 ± 1.1 | 0.01 ± 1.53 | 0.70 | |
| Waist circumference (cm) | 77 ± 8.4 | 71 ± 10 | 70 ± 14 | 0.10 | |
| Hip circumference (cm) | 95 ± 12 | 84 ± 16 | 81 ± 19 | 0.01 | |
| Waist-to-hip ratio | 0.83 ± 0.13 | 0.88 ± 0.21 | 0.91 ± 0.22 | 0.39 | |
| z-BMI | 0.81 ± 1.3 | 0.43 ± 1.8 | 0.75 ± 1.5 | 0.57 | |
| Normal weight, n (%) | 8 (42) | 25 (57) | 17 (44) | 0.36 | |
| SBP (mm Hg) | 120 ± 11.7 | 109 ± 8.7 | 106 ± 13.9 | <0.001 | |
| DBP (mm Hg) | 73 ± 9.3 | 66 ± 8.4 | 67 ± 8.9 | 0.009 | |
| Parents (N = 102) | Female, n (%) | 17 (90) | 36 (82) | 33 (85) | 0.74 |
| Secondary education, n (%) | 8 (42) | 14 (31) | 15 (38) | 0.84 | |
| Tertiary education, n (%) | 7 (37) | 17 (39) | 12 (31) | ||
| Postgraduate education, n (%) | 4 (21) | 13 (30) | 12 (31) | ||
| MedDietScore (0–55) | 31 ± 4.7 | 32 ± 4.1 | 32 ± 3.9 | 0.49 |
| First Tertiary Low (n = 31) | Second Tertiary Medium (n = 32) | Third Tertiary High (n = 39) | p | ||
|---|---|---|---|---|---|
| Children (N = 102) | Age (years) | 12.9 ± 3.2 | 12.4 ± 3.4 | 11.4 ± 3.3 | 0.15 |
| Female, n (%) | 12 (39) | 14 (44) | 24 (62) | 0.13 | |
| Weight (kg) | 58 ± 21 | 51 ± 20 | 45 ± 18 | 0.03 | |
| WAz | 0.83 ± 1.4 | 0.71 ± 1.2 | 0.41 ± 1.1 | 0.33 | |
| Height (cm) | 154 ± 20 | 154 ± 18 | 148 ± 20 | 0.40 | |
| HAz | −0.16 ± 1.3 | 0.36 ± 1.37 | −0.03 ± 1.2 | 0.26 | |
| Waist circumference (cm) | 78 ± 13 | 70 ± 13 | 69 ± 8.3 | 0.03 | |
| Hip circumference (cm) | 91 ± 14 | 83 ± 22 | 82 ± 14 | 0.07 | |
| Waist-to-hip ratio | 0.87 ± 0.11 | 0.91 ± 0.31 | 0.88 ± 0.15 | 0.75 | |
| z-BMI | 1.1 ± 1.1 | 0.65 ± 1.2 | 0.26 ± 2.1 | 0.12 | |
| Normal weight, n (%) | 14 (45) | 16 (50) | 20 (51) | 0.81 | |
| SBP (mm Hg) | 115 ± 13 | 109 ± 12 | 105 ± 10 | <0.001 | |
| DBP (mm Hg) | 72 ± 8.4 | 67 ± 8.2 | 65 ± 9.2 | 0.004 | |
| KIDMED score (−4 to 12) | 5.29 ± 2.6 | 6.25 ± 2.5 | 5.21 ± 2.8 | 0.20 | |
| Parents (N = 102) | Female, n (%) | 21 (68) | 31 (97) | 34 (88) | 0.005 |
| Secondary education, n (%) | 14 (45) | 13 (41) | 10 (26) | 0.07 | |
| Tertiary education, n (%) | 11 (35) | 10 (31) | 15 (38) | ||
| Postgraduate education, n (%) | 6 (19) | 9 (28) | 14 (36) |
| (A) b ± SE, for KIDMED | p | (B) b ± SE for MedDietScore | p | ||
|---|---|---|---|---|---|
| SBP | Model 1: KIDMED (A) or MedDietScore (B) | −1.70 ± 0.44 | <0.001 | −1.22 ± 0.28 | <0.001 |
| Model 2: Model 1 + child’s age | −1.22 ± 0.44 | 0.006 | −1.01 ± 0.26 | <0.001 | |
| Model 3: Model 2 + child’s sex | −1.23 ± 0.44 | 0.006 | −1.05 ± 0.27 | <0.001 | |
| Model 4: Model 3 + child’s z-BMI | −1.35 ± 0.41 | 0.001 | −0.89 ± 0.26 | 0.001 | |
| Model 5: Model 4 + parents’ sex | −1.32 ± 0.41 | 0.002 | −1.01 ± 0.27 | <0.001 | |
| Model 6: Model 5 + parents’ education level | −1.34 ± 0.41 | 0.002 | −1.01 ± 0.27 | <0.001 | |
| Model 7: Model 6 + MedDietScore (A) or KIDMED (B) | −1.33 ± 0.39 | <0.001 | −1.01 ± 0.25 | <0.001 | |
| DBP | Model 1: KIDMED (A) or MedDietScore (B) | −0.70 ± 0.34 | 0.04 | −0.78 ± 0.21 | <0.001 |
| Model 2: Model 1 + child’s age | −0.65 ± 0.35 | 0.07 | −0.77 ± 0.21 | <0.001 | |
| Model 3: Model 2 + child’s sex | −0.67 ± 0.36 | 0.06 | −0.78 ± 0.22 | <0.001 | |
| Model 4: Model 3 + child’s z-BMI | −0.71 ± 0.36 | 0.048 | −0.75 ± 0.22 | <0.001 | |
| Model 5: Model 4 + parents’ sex | −0.73 ± 0.36 | 0.044 | −0.77 ± 0.23 | 0.001 | |
| Model 6: Model 5 + parents’ education level | −0.78 ± 0.34 | 0.024 | −0.75 ± 0.21 | <0.001 | |
| Model 7: Model 6 + MedDietScore (A) or KIDMED (B) | −0.77 ± 0.32 | 0.017 | −0.75 ± 0.21 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foscolou, A.; Papandreou, P.; Bikaki, A.; Skouroliakou, M.; Gioxari, A. Adherence to the Mediterranean Diet and Arterial Blood Pressure in Schoolchildren: The Role of Parental Eating Habits. Children 2025, 12, 844. https://doi.org/10.3390/children12070844
Foscolou A, Papandreou P, Bikaki A, Skouroliakou M, Gioxari A. Adherence to the Mediterranean Diet and Arterial Blood Pressure in Schoolchildren: The Role of Parental Eating Habits. Children. 2025; 12(7):844. https://doi.org/10.3390/children12070844
Chicago/Turabian StyleFoscolou, Alexandra, Panos Papandreou, Aikaterini Bikaki, Maria Skouroliakou, and Aristea Gioxari. 2025. "Adherence to the Mediterranean Diet and Arterial Blood Pressure in Schoolchildren: The Role of Parental Eating Habits" Children 12, no. 7: 844. https://doi.org/10.3390/children12070844
APA StyleFoscolou, A., Papandreou, P., Bikaki, A., Skouroliakou, M., & Gioxari, A. (2025). Adherence to the Mediterranean Diet and Arterial Blood Pressure in Schoolchildren: The Role of Parental Eating Habits. Children, 12(7), 844. https://doi.org/10.3390/children12070844






